Introduction
The prognosis of patients with lung cancer
metastasis to the spine is poor, and the option of surgery is
questionable based on the aggressiveness of the disease. Between 5
and 10% of patients with systemic cancer develop vertebral
metastases (1–4). The thoracic spine is the most common
region involved in spinal metastases (70%) (5). The five-year survival rate for
patients with lung cancer is 10 to 20%, as reported by Sundaresan
et al (2) Stanley (6) and Freise et al (7) indicating a poor prognosis. In a
retrospective study of 118 patients with bone metastasis from lung
cancer, treatment with an epidermal growth factor receptor (EGFR)
inhibitor indicated improved prognosis for patients with
adenocarcinoma. The mean survival time was longer in the group
treated with the EGFR inhibitor (17.8 months; range, 8.4–30.1
months) than that in the group without the EGFR inhibitor (10.8
months; range, 0.6–54.0 months) among 52 patients with
adenocarcinoma metastases (8). It
is therefore possible that the survival time for certain patients
could be extended following appropriate surgical treatment combined
with radiation and EGFR inhibitor therapy.
Case report
The present study describes the case of a
56-year-old male who seeked consultation due to back pain [Visual
Analog Scale (VAS) of 7/10], numbness below the umbilicus and
weakness of the bilateral lower limbs. The patient had no other
signs or symptoms, no significant past medical history and no
history of smoking. The patient was immediately referred to the
Department of Orthopedic Oncology of the General Hospital of Ji’nan
Military Region (Ji’nan, China). The laboratory findings were
unremarkable. Upon arrival to the inpatient department, a computed
tomography (CT) scan and X-ray of the spine were taken. An abnormal
mass was noted at the level of T9 and the left upper lobe of the
lung. Further investigation with magnetic resonance imaging (MRI),
positron emission tomography (PET)-CT and biopsies of the vertebral
and pulmonary lesions confirmed the diagnosis of a single
metastatic lesion at the level of T9. The primary site was the lung
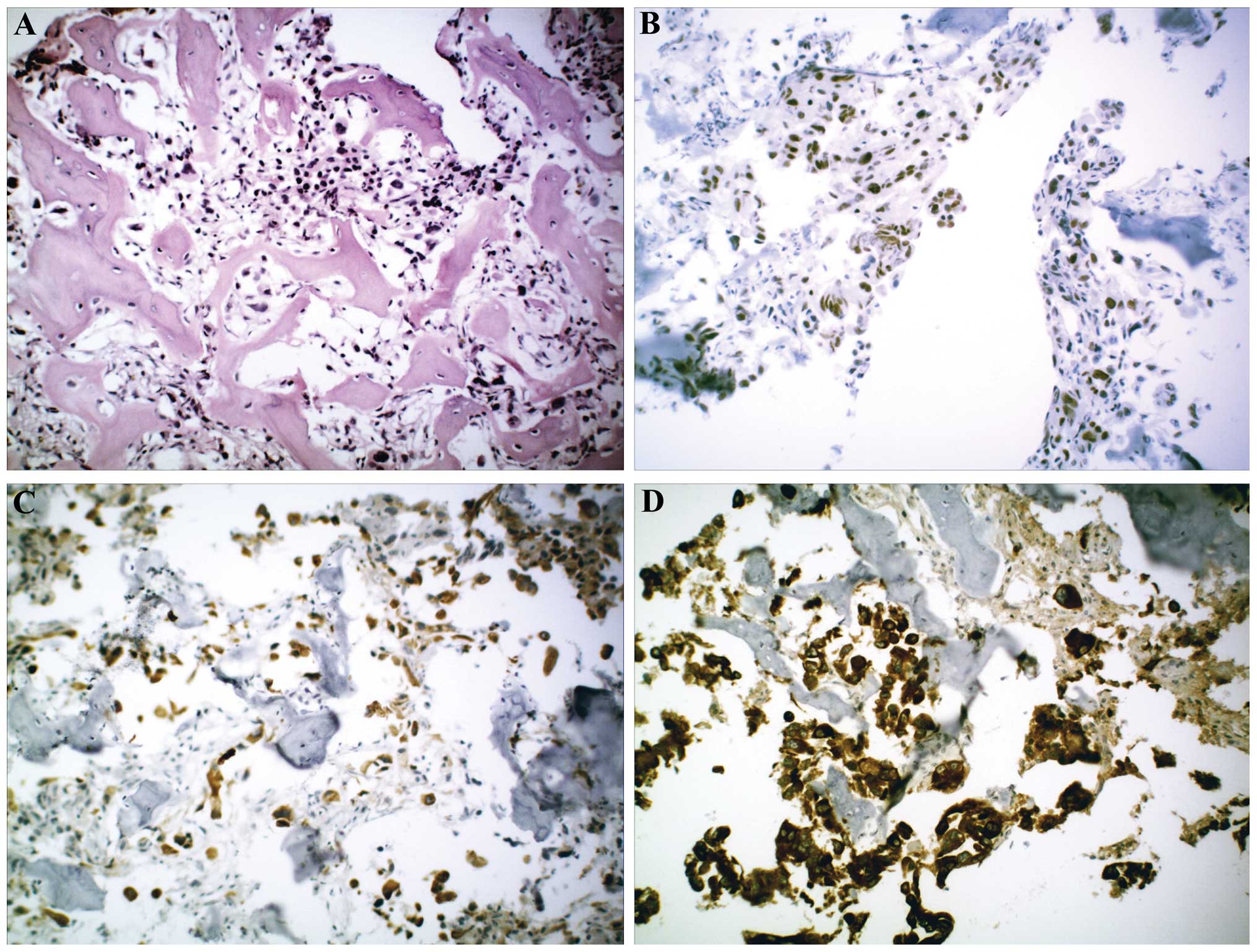
with staging of T1N0M1. The lesion was confirmed to be non-small
cell lung cancer (adenocarcinoma) with immunological pathology
(Fig. 1). A mutation to the EGFR
gene was identified (deletion of exon 21). The MRI showed pedicle
involvement and spinal canal stenosis. The vertebral lesion spanned
the entire T9 vertebra. The Tokuhashi score (9) was nine, which indicated survival of
>6 months, and palliative surgery was recommended.
The surgery consisted of a posterior decompression
with partial resection of the T9 tumor followed by the installation
of a posterior pedicle screw system between T7 and T11. The patient
fully recovered and had no complications due to surgery. His
postoperative VAS was reduced to 2/10 and the numbness and weakness
disappeared immediately subsequent to the surgery. The patient
received follow-ups at 1, 3, 6, 12 and 24 months without recurrence
of the numbness or weakness or any other complication. The patient
was also treated with three cycles of three-dimensional (3D)
conformal radiotherapy (RT) (30 cGy/day for 10 days) localized to
the spine and lung subsequent to surgery. The RT was completed
without any associated complications. Erlotinib therapy (150 mg
daily) was initiated from February 2012, and continues to date, and
the patient experienced significant symptom improvement. After 24
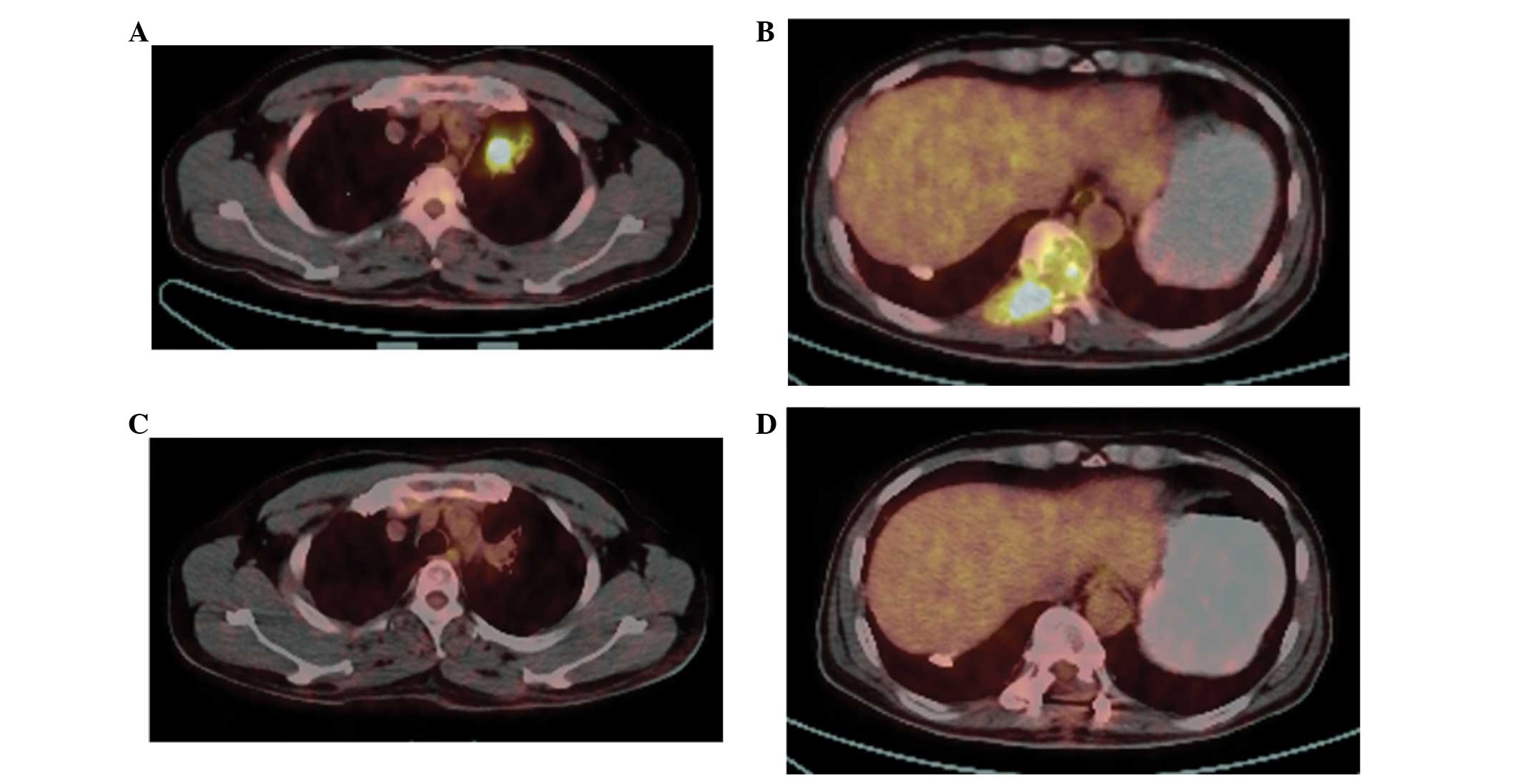
months, PET-CT scan showed a decrease in the left upper lobe mass
in the short axis and inactivation of the neoplasm in the left
upper lobe and T9 vertebra (Fig.
2). This patient continues to be monitored through follow-up
appointments. Informed consent was obtained from either the patient
or the patient’s family prior to inclusion in the present
study.
Discussion
As well as chronic and increasing pain, spinal
metastases cause neurological deficits due to destruction of the
vertebral body and subsequent epidural growth expansion (10). The primary aim of surgery in the
treatment of spinal metastases is the reduction of pain and the
maintenance of neurological function and spinal stability. The
decision to proceed with surgery should be determined individually
in an interdisciplinary consultation. In a previous retrospective
cohort study of 2,321 consecutive patients with acute symptoms of
metastatic spinal cord compression (MSCC) admitted to a single
center, the patients with MSCC deriving from pulmonary and renal
cancer experienced an improved one-year survival compared with
other oncologic diagnoses (11).
The selection of surgical treatment for MSCC has increased due to
positive results from clinical studies, improved surgical
techniques and an increasing number of patients being treated for
an oncological condition. In the present case, the patient had
incomplete paralysis and was treated with posterior decompression
with internal fixation, which not only cured the MSCC but also gave
a strong support for his spine.
RT is important in palliating the symptoms of
patients with metastatic disease. The response to RT has been
quantified and qualified with numerous criteria and instruments
over the past decades (12).
Studies have shown that 70–90% of patients achieve a beneficial
response with analgesic-directed RT, with complete responses
observed in up to 40% of patients (13,14).
As the majority of spinal tumors are metastases, spinal RT is
typically delivered using conventional two-dimensional or 3D
conformal techniques, as demonstrated in the present case.
EGFR inhibitors comprise a novel, molecule-targeting
treatment for lung cancer. These inhibitors have been reported to
exert promising effects in females and nonsmokers, particularly
those with adenocarcinoma (15–17).
Treatment with an EGFR inhibitor may prolong survival following
bone metastasis (8); however,
interstitial pneumonia remains a serious side effect (18), and it has been reported EGFR
inhibitors are less effective in patients without the EGFR gene
(15). The indications for EGFR
inhibitor therapy should therefore be considered carefully prior to
expecting an improvement in survival. To the best of our knowledge,
few reports have focused on EGFR mutations as effective prognosis
indicators for patients with lung cancer adenocarcinoma
metastasized to the spine (11,19,20).
EGFR mutations should be verified for this patient group. In the
present case, the combination treatment regimen of radiation and
EGFR inhibitor therapy following surgical treatment was proved to
be fully effective for the patient, as shown in the PET-CT images
and by the good quality of life during follow-up.
In conclusion, the present study describes a case in
which favorable results and a good recovery were achieved based on
the selection of surgical treatment combined with radiation and
EGFR inhibitor therapy, an option that is recommended for patients
with lung cancer metastasized to the spine. We suggest that EGFR
mutation be verified for patients with lung cancer metastasized to
the spine. Furthermore, we encourage orthopedic oncologists to
consider radiation and EGFR inhibitor therapy with surgery, based
on the promising results observed in the present study.
References
|
1
|
Sciubba DM and Gokaslan ZL: Diagnosis and
management of metastatic spine disease. Surg Oncol. 15:141–151.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sundaresan N, Boriani S, Rothman A and
Holtzman R: Tumors of the osseous spine. J Neurooncol. 69:273–290.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
White AP, Kwon BK, Lindskog DM, et al:
Metastatic disease of the spine. J Am Acad Orthop Surg. 14:587–598.
2006.PubMed/NCBI
|
|
4
|
Witham TF, Khavkin YA, Gallia GL, et al:
Surgery insight: current management of epidural spinal cord
compression from metastatic spine disease. Nat Clin Pract Neurol.
2:87–94. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Black P: Spinal metastasis: current status
and recommended guidelines for management. Neurosurgery. 5:726–746.
1979. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stanley KE: Prognostic factors for
survival in patients with inoperable lung cancer. J Natl Cancer
Inst. 65:25–32. 1980.PubMed/NCBI
|
|
7
|
Freise G, Gabler A and Liebig S: Bronchial
carcinoma and long-term survival. Retrospective study of 433
patients who underwent resection. Thorax. 33:228–234. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sugiura H, Yamada K, Sugiura T, et al:
Predictors of survival in patients with bone metastasis of lung
cancer. Clin Orthop Relat Res. 466:729–736. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tokuhashi Y, Matsuzaki H, Oda H, et al: A
revised scoring system for preoperative evaluation of metastatic
spine tumor prognosis. Spine (Phila Pa 1976). 30:2186–2191. 2005.
View Article : Google Scholar
|
|
10
|
Klimo P Jr and Schmidt MH: Surgical
management of spinal metastases. Oncologist. 9:188–196. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Morgen SS, Lund-Andersen C, Larsen CF, et
al: Prognosis in patients with symptomatic metastatic spinal cord
compression: survival in different cancer diagnosis in a cohort of
2321 patients. Spine (Phila Pa 1976). 38:1362–1367. 2013.
View Article : Google Scholar
|
|
12
|
Komatsu T, Kunieda E, et al: An analysis
of the survival rate after radiotherapy in lung cancer patients
with bone metastasis: is there an optimal subgroup to be treated
with high-dose radiation therapy? Neoplasma. 59:650–657. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jacobs WB and Perrin RG: Evaluation and
treatment of spinal metastases: an overview. Neurosurg Focus.
11:e102001. View Article : Google Scholar
|
|
14
|
Agarawal JP, Swangsilpa T, van der Linden
Y, et al: The role of external beam radiotherapy in the management
of bone metastases. Clin Oncol (R Coll Radiol). 18:747–760. 2006.
View Article : Google Scholar
|
|
15
|
Mitsudomi T, Kosaka T, Endoh H, et al:
Mutations of the epidermal growth factor receptor gene predict
prolonged survival after gefitinib treatment in patients with
non-small-cell lung cancer with postoperative recurrence. J Clin
Oncol. 23:2513–2520. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yokouchi H, Yamazaki K, Kinoshita I, et
al: Clinical benefit of readministration of gefitinib for initial
gefitinib-responders with non-small cell lung cancer. BMC Cancer.
7:512007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Herbst RS, Maddox AM, Rothenberg ML, et
al: Selective oral epidermal growth factor receptor tyrosine kinase
inhibitor ZD1839 is generally well-tolerated and has activity in
non-small-cell lung cancer and other solid tumors: results of a
phase I trial. J Clin Oncol. 20:3815–3825. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Inoue A, Saijo Y, Maemondo M, et al:
Severe acute interstitial pneumonia and gefitinib. Lancet.
361:137–139. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ni X, Wu P, Wu C, et al: Treatment of
cervical vertebral (C1) metastasis of lung cancer with
radiotherapy: A case report. Oncol Lett. 5:1129–1132.
2013.PubMed/NCBI
|
|
20
|
Aoude AA and Amiot LP: Surgical treatment
of a patient with lung cancer metastasized to the spine with EGFR
mutation: A case report. Int J Surg Case Rep. 3:510–512. 2012.
View Article : Google Scholar : PubMed/NCBI
|