Introduction
In recent years, with the improvement of imaging
techniques and prenatal care systems, a growing number of cases of
pediatric hydronephrosis have been detected in the early prenatal
period and followed up (1,2). In addition, an increasing number of
cases of pediatric ampullary renal pelvis (ARP), which is
challenging to distinguish from hydronephrosis, have been diagnosed
in postnatal follow-up observations (3). To improve the diagnostic accuracy of
this type of pelvis and to reduce misdiagnosis, the present study
reports the findings in the clinical follow-up of 65 cases of ARP
from 1,167 pediatric patients who were prenatally suspected to have
hydronephrosis.
Patients and methods
Patient characteristics
This study retrospectively analyzed 1,167 cases of
prenatally suspected hydronephrosis, who were referred to
comprehensive pediatric surgery, obstetrics, ultrasound and other
related departments in the Qilu Hospital of Shandong University
(Jinan, China) between January 2003 and December 2011. For the
purpose of this study, different levels of postnatal follow-up
program were performed for these cases according to the grade of
hydronephrosis. A total of 65 cases were diagnosed with pediatric
ARP by complete physical examination by ultrasound, computed
tomography urography (CTU) and magnetic resonance imaging of the
urinary system (MRU). Of these cases of ARP, 37 were males and 28
were females. The average age of the cases ranged from 2 to 8 years
(mean age, 3.9 years). Unilateral and bilateral ARP were diagnosed
in 54 (left in 31 and right in 23 cases) and 11 cases,
respectively.
Follow-up surveillance
In the large-scale prenatal screening and follow-up
of postnatal hydronephrosis, ARP initially did not show any
difference from hydronephrosis by sonographic examination.
Ultrasonic examination reported a volatile separation of the renal
pelvis collection system by 2–3 cm, with or without mild renal
calyx dilatation. Such cases were closely followed up according to
the grade of hydronephrosis and ultrasound tests were performed
once every one to three months. Compared with cases of ordinary
uteropelvic junction (UPJ) obstruction hydronephrosis and
pyelonephritis, the separation of the collection system in such
cases was always volatile (sometimes large and sometimes small) as
the number of follow-up observations increased. Moreover, the calyx
in these cases did not show clear dilatation or exhibited no
dilatation, and did not tend to increase in the follow-up
observation. As the follow-up observations continued, and the
in-depth understanding of the disease increased, the cases were
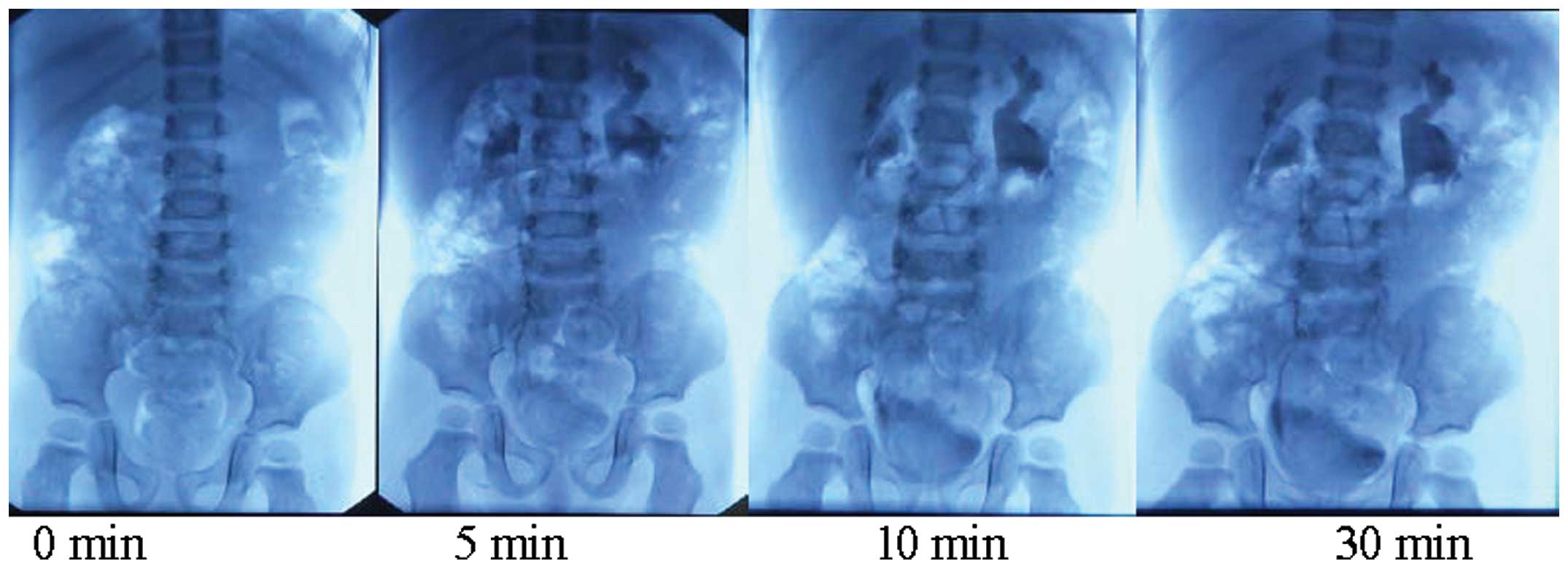
identified and summarized. Further imaging studies, such as CTU and
MRU, documented the morphology of the renal pelvis in these cases,
which were grouped separately from other hydronephrosis cases
(Figs. 1 and 2). This group of cases continued to be
followed up by ultrasound test every three months and the
separation of the renal pelvis collection system was recorded. All
these experiments were conducted after informed consent was given
by the parents and under the approval by the ethics committee of
the Qilu Hospital of Shandong University (Shandong, China).
Results
The diagnosis of pediatric ARP was made on the basis
of imaging examination in the postnatal follow-up observation.
Ultrasonic diagnosis showed that the separation of the collection
system was mostly volatile by 2–3 cm with only small changes in the
next two or three follow-up observations. Even though the
hydronephrosis in these cases was mainly Society for Fetal Urology
(SFU) classification 2 or 3 (4),
CTU or MRU examination showed dilatation of the renal pelvis
collection system, but mild renal caliectasis and complete
cup-shaped calyx morphology. In total, 37 cases were followed up
and diagnosed with ARP by ultrasonic examination (Table I).
 | Table ISeparation of the renal pelvis and
renal cortical thickness as evaluated by ultrasound (mm, mean ±
standard deviation). |
Table I
Separation of the renal pelvis and
renal cortical thickness as evaluated by ultrasound (mm, mean ±
standard deviation).
| Age |
|---|
|
|
|---|
| Variable | 6 days | 42 days | 3 months | 6 months | 1 year |
|---|
| Pelvis collection
system | 22.3±5.60 | 24.4±6.03 | 25.5±6.22 | 23.2±6.3 | 24.4±5.23 |
| Renal cortical
thickness | 0.76±0.13 | 0.69±0.16 | 0.75±0.17 | 0.85±0.18 | 0.75±0.16 |
Discussion
In the past, pediatric hydronephrosis was identified
when patients received abdominal ultrasound screening due to
abdominal mass and abdominal pain. Now, pediatric hydronephrosis
can be diagnosed prenatally (5)
and closely followed up in postnatal examination (1,6,7).
Follow-up program development is based on the hydronephrosis
classification (8). With an
increase in the follow-up observation and in-depth understanding of
pediatric hydronephrosis, pediatric ARP may be detected and
verified.
The morphology of the renal pelvis does not have
uniform standards in anatomy and imaging. Anatomically, the renal
pelvis is situated in the renal sinus and comprises two or three
major renal calyces formed from two or three renal calyces. Renal
angiography intuitively displays the morphology and type of renal
pelvis. The renal pelvis can be divided into intrarenal and renal
pelvis according to the location of the pelvis, while the shape of
the renal pelvis can be divided into horn, branching, ampullary and
transitional types. X-ray angiographic observation demonstrates
that ARP is large and round and may be connected with renal calyces
instead of major renal calyces.
To the best of our knowledge, this is the first
detailed report on the diagnosis of pediatric ARP. With
improvements of imaging techniques and prenatal care systems,
pediatric UPJ hydronephrosis can be diagnosed and closely followed
up in the early fetal period. Therefore, pediatric ARP can be
observed in the early postnatal follow-up examination and diagnosed
in the continuous follow-up observations. Pediatric hydronephrosis
is divided into physiological and pathological pediatric
hydronephrosis, which can be diagnosed during postnatal follow-ups.
Pediatric ARP can be distinguished from hydronephrosis since in ARP
the separation of the renal pelvis collection system does not tend
to increase during the postnatal follow-up observation. Wang et
al reported that by ultrasonic examination, the morphology of
the pediatric ampullary pelvis exhibits four shapes, specifically
obtuse triangle, shuttle type, oval and dendritic (9). Ultra-sonography reveals that the
obtuse triangle and oval ampullary types are mainly characterized
by a mild separation of the pelvis collection system with <2 cm
width, in the shape of an obtuse triangle or oval. Moreover, the
calyx echo is indistinguishable and without a sense of tension;
also, no clear changes in the non-echo range are detected in
several reviews following urination. The morphology of the
shuttle-type pediatric ampullary pelvis is very similar to the
physiological separation of the renal sinus, whereas the dendritic
ampullary pelvis has a branch-like shape.
Although the ampullary pelvis has previously been
described, the clinical manifestations and diagnosis of pediatric
ampullary pelvis have not been reported. With the large-scale
screening of cases of fetal hydronephrosis and follow-up
observation, cases of pediatric ampullary pelvis may be
distinguished from those of fetal hydronephrosis. The diagnosis of
pediatric ampullary pelvis not only relies on comprehensive
analysis of ultrasonography, CTU, MRU and other imaging
examinations, but also on long-term dynamic follow-up observation.
A full understanding of the pediatric ampullary pelvis is
significant to the differential diagnosis of this normal
physiological pelvis morphology from pediatric hydronephrosis. To
reduce misdiagnosis, it is recommended that renal ultrasound tests
in each postnatal follow-up observation are combined with history
and previous follow-up test results. It is also recommended that
clinicians highly regard complete follow-up observation data to
distinguish pediatric ampullary pelvis from pediatric
hydronephrosis and make a correct diagnosis and use the correct
treatment protocols.
In conclusion, an increasing number of cases of
hydronephrosis may be detected ante partum, and patients should be
closely followed up until the infant and juvenile periods. The
cases may be distinguished by ultrasonography. Thus, the diagnosis
methods and timing of the surgical treatment that should be adopted
differ from those previously. In addition, it is necessary to
distinguish between physiological and pathological hydronephrosis.
Hydronephrosis requires close follow-up and appropriate treatment.
Finally, selecting an appropriate opportunity for surgical
treatment is dependent on the grade of severity, results of
follow-up and renal function.
References
|
1
|
Barbosa JA, Chow JS, Benson CB, Yorioka
MA, Bull AS, Retik AB and Nguyen HT: Postnatal longitudinal
evaluation of children diagnosed with prenatal hydronephrosis:
insights in natural history and referral pattern. Prenat Diagn.
32:1242–1249. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chu L, Jacobs BL, Schwen Z and Schneck FX:
Hydronephrosis in pediatric kidney transplant: clinical relevance
to graft outcome. J Pediatr Urol. 9:217–222. 2013. View Article : Google Scholar
|
|
3
|
Wieczorkiewicz-Płaza A, Zajaczkowska M,
Radzikowska E and Maciejewski R: Diagnostic difficulties in the
differentiation of urine retention and developmental anomalies in
the pelvicalyceal system in the ultrasound examination of children.
Folia Morphol (Warsz). 63:245–247. 2004.
|
|
4
|
Fembach SK, Maizels M and Conway JJ:
Ultrasound grading of hydronephrosis: introduction to the system
used by the society for fetal urology. Pediatr Radio. 23:478–480.
1993. View Article : Google Scholar
|
|
5
|
Pates JA and Dashe JS: Prenatal diagnosis
and management of hydronephrosis. Early Hum Dev. 82:3–8. 2006.
View Article : Google Scholar
|
|
6
|
Mouriquand PD, Whitten M and Pracros JP:
Pathophysiology, diagnosis and management of prenatal upper tract
dilatation. Prenat Diagn. 21:942–951. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mure PY and Mouriquand P: Upper urinary
tract dilatation: prenatal diagnosis, management and outcome. Semin
Fetal Neonatal Med. 13:152–163. 2008. View Article : Google Scholar
|
|
8
|
Timberlake MD and Herndon CD: Mild to
moderate postnatal hydronephrosis-grading systems and management.
Nat Rev Urol. 10:649–656. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang Z, Zhang D, Gui M, et al: Extrarenal
pelvis a normal shape of pelvis. J Med Imaging. 13:410–411.
2003.
|