Introduction
B-cell chronic lymphocytic leukemia (B-CLL) is the
most common form of leukemia and occurs with a male predominance
(1), with majority of patients
being over the age of 45 years. Medical literature describing the
appearance of cutaneous involvement in patients with B-CLL is
limited. In the majority of cases, the cutaneous lesions are
nonspecific manifestations associated with an impaired immune
system (2). The reported specific
skin lesions include nodules, papules, infiltrates, plaques,
ulcerations and exfoliative erythroderma (2–5),
presenting predominantly in the head and neck areas. In the present
study, a 57-year-old man with B-CLL who presented with plaque skin
infiltrates affecting the limbs, buttocks and prominent parts of
the face is described.
Case report
A 57-year-old male presented with a one-week history
of non-pitting edema in the hands and feet in addition to
erythematous skin on both buttocks. The patient had a 10-year
history of untreated B-CLL and self-reported concurrent gradual
hypertrophic changes of the ears, eyebrows, nose and toes. Informed
consent was obtained from the patient.
Blood tests showed a percentage of blood lymphocytes
of 65.4% (normal, 20–45%), a lymphocyte count of
5.7×109/l (normal, 1.5–3×109/l) and no
significant abnormalities in erythrocyte sedimentation rate, tumor
markers and biochemistry. A 24-h electrocardiogram showed atrial
flutter and atrial fibrillation. The patient was admitted to Sir
Run Run Shaw Hospital, School of Medicine, Zhejiang University
(Hangzhou, China) for further diagnosis and treatment.
On examination, the vital signs were stable. The
patient was observed to have plum-colored swelling involving the
prominent parts of the ears (helix, tragus and ear lobe), the
eyebrows, nose and toes and non-pitting edema on the dorsal
surfaces of the hands and fingers (Fig. 1). The lymph nodes in the right
submandibular, left subclavian, left axilla and groin areas were
enlarged. Non-blanching erythematous plaques were present on the
patient’s buttocks.
Laboratory findings when the patient was first
admitted were as follows: The leukocyte count was
14.0×109/l (normal range, 4.0–10.0×109/l),
the lymphocyte count was 10.6×109/l (normal range,
1.5–3.0×109/l), the percentage of lymphocytes was 65.4%
(normal range, 20–45%), the neutrophil count was
2.9×109/l (normal range, 1.5–3.0×109/l) and
the percentage of neutrophils was 20.5% (normal range, 55–75%).
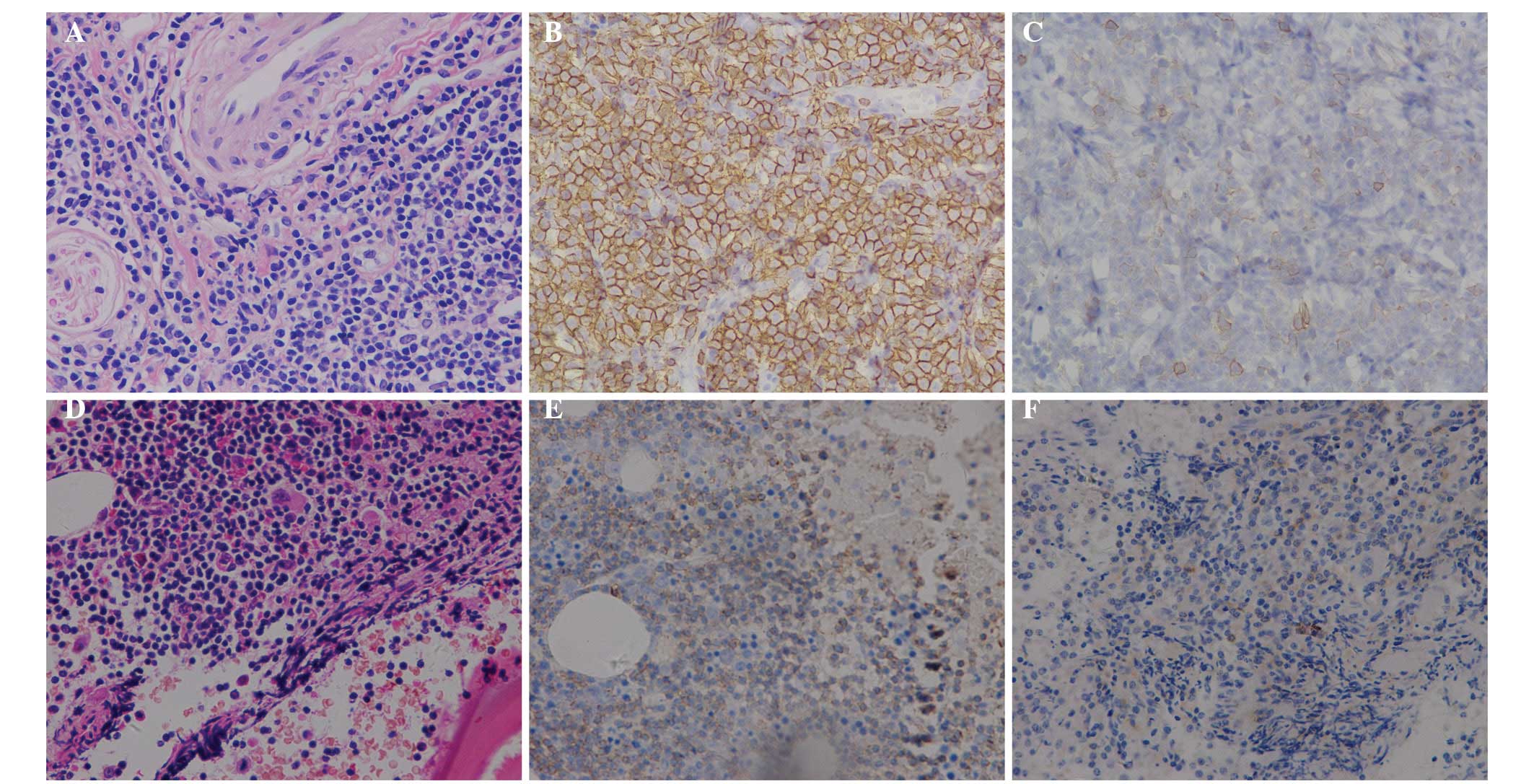
Histopathology of a biopsy from the right auricular lobule showed
atypical hyperplasia of lymphoid tissue. Immunohistochemical
investigation revealed that the right auricular lobule co-expressed
CD20 and CD5, which is consistent with CLL/small lymphocytic
lymphoma. Hematoxylin and eosin staining of bone marrow revealed
the diffuse infiltration of small lymphocytic cells.
Immunohistochemical staining revealed that the bone marrow was
positive for the B-cell marker CD20 and also partly positive for
CD23 and CD5, which is consistent with an infiltrate of CLL
(Fig. 2).
The patient was recommended to receive chemotherapy
but declined it due to a poor financial situation and fear of the
side-effects of chemotherapy. Following a three-year follow-up in
the clinic, the patient remained alive with mildly aggravated
symptoms.
Discussion
B-CLL is a low-grade, B-cell lymphoproliferative
monoclonal disorder in which functionally immunoincompetent
lymphocytes are progressive accumulated, and thereby affect immune
function and normal hematopoiesis. It is associated with an
increased incidence of other malignancies, including squamous cell
carcinoma, basal cell carcinoma, malignant melanoma and Merkel cell
carcinoma (6). B-CLL patients are
prone to cutaneous infections, particularly viral infections, and
have exaggerated reactions to insect bites (6,7).
From a broader point of view, the incidence of
lymphomas, in particular that of B-CLL, is increasing worldwide
(8,9). The majority of patients with CLL
manifest atypical clinical features. The most common symptoms and
signs of this condition include fatigue, fever, easy bruising and
generalized lymphadenopathy (10).
Although skin infiltration occurs in 3–50% of
patients with leukemias or lymphomas overall, it is rare in
patients with CLL (11,12). When evident skin involvement is
observed in CLL, it usually is seen in Richter syndrome or T-cell
CLL (13,14), which generally indicates a poor
prognosis (3,15,16).
Medical literature reports that CLL can cause skin infiltrates,
chronic and relapsing pruritic skin lesions (17) and indurated plaques of the eyebrows
(18). Reports of cutaneous
symptoms being the primary manifestation of B-CLL are unusual
(3,19,20).
The case described in the present study presented as a skin
infiltrate involving prominent parts of the head, such as the nose,
ears and eyebrows, and other parts of the body, including the
fingers and toes, a rare combination which might shed light on the
mechanism involved in attracting leukemic cells of CLL patients to
the skin. In the present case, this process was not investigated
further and the possibilities can only be speculated on. The
mechanism of cutaneous infiltration has not been fully elucidated.
It has been postulated that skin invasiveness may be caused by the
upregulation of intercellular adhesion molecule 1 (ICAM-1) and
lymphocyte function-associated antigen 1 (LFA-1) (21). It is important to be aware of the
possibility of these unusual presentations of cutaneous B-CLL,
although skin involvement in B-CLL may be consistent with prolonged
survival (15). Additional
investigations into the behavior of B-CLL in the skin may further
elucidate how this condition develops.
References
|
1
|
Chiorazzi N, Rai KR and Ferrarini M:
Chronic lymphocytic leukemia. N Engl J Med. 352:804–815. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
di Meo N, Stinco G and Trevisan G:
Cutaneous B-cell chronic lymphocytic leukaemia resembling a
granulomatous rosacea. Dermatol Online J. 19:200332013.PubMed/NCBI
|
|
3
|
Cerroni L, Zenahlik P, Höfler G, Kaddu S,
Smolle J and Kerl H: Specific cutaneous infiltrates of B-cell
chronic lymphocytic leukemia: a clinicopathologic and prognostic
study of 42 patients. Am J Surg Pathol. 20:1000–1010. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Robak E and Robak T: Skin lesions in
chronic lymphocytic leukemia. Leuk Lymphoma. 48:855–865. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dhir R: Chronic lymphocytic leukaemia
manifestating as exfoliative dermatitis. Indian J Dermatol Venereol
Leprol. 61:102–103. 1995.PubMed/NCBI
|
|
6
|
Agnew KL, Ruchlemer R, Catovsky D, Matutes
E and Bunker CB: Cutaneous findings in chronic lymphocytic
leukaemia. Br J Dermatol. 150:1129–1135. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Walker P, Long D, James C and Marshman G:
Exaggerated insect bite reaction exacerbated by a pyogenic
infection in a patient with chronic lymphocytic leukaemia.
Australas J Dermatol. 48:165–169. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sng I: Malignant lymphoma - a changing
spectrum. Ann Acad Med Singapore. 38:837–839. 2009.PubMed/NCBI
|
|
9
|
Wu SJ, Huang SY, Lin CT, Lin YJ, Chang CJ
and Tien HF: The incidence of chronic lymphocytic leukemia in
Taiwan, 1986–2005: a distinct increasing trend with birth-cohort
effect. Blood. 116:4430–4435. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hallek M, Cheson BD, Catovsky D, et al;
International Workshop on Chronic Lymphocytic Leukemia. Guidelines
for the diagnosis and treatment of chronic lymphocytic leukemia: a
report from the International Workshop on Chronic Lymphocytic
Leukemia updating the National Cancer Institute-Working Group 1996
guidelines. Blood. 111:5446–5456. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jasim ZF, Cooke N, Somerville JE and Hay
RJ: Chronic lymphocytic leukaemia skin infiltrates affecting
prominent parts of the face and the scalp. Br J Dermatol.
154:981–982. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chang HY, Wong KM, Bosenberg M, McKee PH
and Haynes HA: Myelogenous leukemia cutis resembling stasis
dermatitis. J Am Acad Dermatol. 49:128–129. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Giles FJ, O’Brien SM and Keating MJ:
Chronic lymphocytic leukemia in (Richter’s) transformation. Semin
Oncol. 25:117–125. 1998.PubMed/NCBI
|
|
14
|
Hoyer JD, Ross CW, Li CY, Witzig TE,
Gascoyne RD, Dewald GW and Hanson CA: True T-cell chronic
lymphocytic leukemia: a morphologic and immunophenotypic study of
25 cases. Blood. 86:1163–1169. 1995.PubMed/NCBI
|
|
15
|
Colburn DE, Welch MA and Giles FJ: Skin
infiltration with chronic lymphocytic leukemia is consistent with a
good prognosis. Hematology. 7:187–188. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Watson KM, Mufti G, Salisbury JR, du
Vivier AW and Creamer D: Spectrum of clinical presentation,
treatment and prognosis in a series of eight patients with
leukaemia cutis. Clin Exp Dermatol. 31:218–221. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Neuber K, Berg-Drewniock B, Volkenandt M,
et al: B-cell chronic lymphocytic leukemia associated with high
serum IGE levels and pruriginous skin lesions: successful therapy
with IFN-alpha 2b after failure on IFN-gamma. Dermatology.
192:110–115. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schmid-Wendtner MH, Sander C, Volkenandt M
and Wendtner CM: Unusual manifestations of B-cell disorders. Case
2: chronic lymphocytic leukemia presenting with cutaneous lesions.
J Clin Oncol. 17:1084–1085. 1999.PubMed/NCBI
|
|
19
|
Padgett JK, Parlette HL III and English JC
III: A diagnosis of chronic lymphocytic leukemia prompted by
cutaneous lymphocytic infiltrates present in Mohs micrographic
surgery frozen sections. Dermatol Surg. 29:769–771. 2003.PubMed/NCBI
|
|
20
|
Khandelwal A, Seilstad KH and Magro CM:
Subclinical chronic lymphocytic leukaemia associated with a 13q
deletion presenting initially in the skin: apropos of a case. J
Cutan Pathol. 33:256–259. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Uccini S, Ruco LP, Monardo F, La Parola
IL, Cerimele D and Baroni CD: Molecular mechanisms involved in
intraepithelial lymphocyte migration: a comparative study in skin
and tonsil. J Pathol. 169:413–419. 1993. View Article : Google Scholar : PubMed/NCBI
|