Introduction
Sepsis is a serious condition associated with great
mortality, characterized by an infectious process that induces a
severe systemic inflammatory response. The physiopathology of
sepsis is well understood, and mediators such as pro-inflammatory
cytokines, reactive oxygen species, nitric oxide, toll-like
receptors and transcription factors such as nuclear factor κB
(NF-κB) play central roles in regulating the immune response
responsible for tissue injury and circulatory collapse (1,2).
These events lead to hypotension, increased capillary permeability,
multiple organ failure and mortality.
Although various therapeutic strategies have been
implemented with the aim of reducing sepsis-associated morbidity
and mortality, the cornerstone of treatment remains prompt
antibiotic use and hemodynamic management (3). The use of immunomodulators, such as
activated protein C, has been evaluated and early results were
promising (4). However, a recent
trial did not find any clinical benefit with the use of this drug
(5), thus questioning the use of
drugs that attempt to modulate the inflammatory response. Various
drugs with pleiotropic immunomodulatory properties are currently
being studied, and this remains an active field of research
(6).
Fibrates such as gemfibrozil (GFZ) and fenofibrate
are drugs commonly used in the management of dyslipidemia. They are
ligands for peroxisome proliferator-activated receptor α (PPAR-α),
receptors that belong to the steroid nuclear receptor family and
that participate in lipid peroxidation, the cell cycle and fatty
acid synthesis. Potent immunomodulatory effects have been
associated with fibrates (7).
Fibrates have shown the ability to reduce the expression of
inflammatory genes in endothelial cells, the release of
pro-inflammatory cytokine such as interleukins (ILs) and
tumor-necrosis factor-α (TNF-α), and the transcription of NF-κB in
experimental studies (8,9). Fibrates have also been shown to
reduce IL-1 and C-reactive protein in humans (10). Fibrates also possess antioxidant
effects, and regulate the activation and function of inflammatory
cells (11,12). These effects are independent of the
lipid-lowering properties of fibrates.
The anti-inflammatory effects of fibrates have been
tested in various experimental models of tissue and organ injury,
showing beneficial results (reduced injury and inflammation) in
models of autoimmune encephalomyelitis (13), ischemia-reperfusion injury
(14) and alcohol-induced
hepatotoxicity (15), among
others. Considering the wide ranging immunomodulatory effects of
fibrates, some of which overlap with the physiopathology of sepsis,
the use of fibrates emerges as an interesting option.
Materials and methods
Animals
Animal procedures were performed in accordance with
the proper use and care of laboratory animals, approved by the
ethics committee of the University Hospital ‘José Eleuterio
González’ (Monterrey, Mexico). Experiments were performed on 45
male Wistar rats weighing 200–250 g (Vivarium of the Department of
Physiology, Autonomous University of Nuevo León, Monterrey,
Mexico). Animals were maintained under standard conditions,
including a stable room temperature (24±3°C), a 12 h light/12 h
dark cycle, and had access to commercial rat pellets and water
ad libitum.
Cecal ligation and puncture model (CLP)
(16)
After fasting for 12 h, the rats underwent
ketamine/xylazine anesthesia (Anesket; Pfizer Inc., Mexico City,
Mexico) at a dose of 50/10 mg/kg, intraperitoneally (i.p). Animals
were placed under a heating lamp in order to preserve a core body
temperature of 37°C. A midline incision exposed the intestines and
the cecum was ligated (using 2-0 silk sutures) immediately proximal
to the ileocecal valve causing a 50% obstruction and allowing for
permeability. Two through-and-through punctures using a 18-gauge
needle were performed at the anti-mesenteric side of the cecum.
Light pressure was applied to confirm that fecal matter could
emerge into the peritoneal cavity. The cecum was returned to its
site, the wound was closed and 3 ml/100 g saline was administered
subcutaneously.
The rats were randomly divided into three groups
(n=15 per group): i) Sham-operated group (sham), where laparotomy
was performed, the intestines were only manipulated and the cecum
was ligated but not punctured. ii) Control group, subjected to CLP
as described above. iii) GFZ group that received GFZ (Pfizer Inc.)
prior to undergoing CLP. A dose of 100 mg/kg GFZ was chosen based
on dose-response experiments and was administered 24 h and
immediately prior to surgery. This dose has been shown to decrease
oxidative stress in rodent models (11). The groups were then subdivided into
three different time-points: 2, 4 and 24 h. These time-points
indicated the time after CLP when samples were obtained for
analysis.
Serum analysis
Blood samples obtained following CLP were used to
determine the serum levels of aspartate aminotransferase (AST),
alanine aminotransferase (ALT) and lactate dehydrogenase (LDH) by
standard biochemical automated methods (Vitros Chemical Products;
Johnson & Johnson, New Brunswick, NJ, USA), using commercially
available kits and DT6011 and DTSC11 analyzers (Vitros Chemical
System; Johnson & Johnson). The serum concentrations of TNF-α
and IL-1 were determined using a rat ELISA kit (PeproTech, Mexico
City, Mexico). Lipid peroxidation, expressed as the malondialdehyde
(MDA) level, was assessed by the thiobarbituric acid reactive
substances (TBARS) method using a TBARS colorimetric assay kit
(Cayman Chemical Company, Ann Arbor, MI, USA). The level of LDH was
only evaluated at the 24-h time-point after CLP.
Survival
To assess survival, additional groups of rats (n=10
per group) underwent the same study protocol as those in the
control and GFZ groups, and the rats were left to recover following
the surgery. The animals were observed for a period of five days
and the mortality rate was recorded.
Statistical analysis
SPSS statistical software, version 11.0 (SPSS Inc.,
Chicago, IL, USA) was used to analyze data using one-way analysis
of variance (ANOVA) and with LSD post-hoc test (when data were
found to be normally distributed) and Kruskal-Wallis test (when
data were not normally distributed) so as to evaluate comparisons
between groups, and differences between groups, respectively. The
survival curves were determined using the Kaplan-Meier method and
the log-rank test was used to compare the curves. All values are
expressed as mean ± standard deviation (SD) and P<0.05 was
considered to indicate a statistically significant result.
Results
ALT and AST
AST and ALT values were significantly elevated
following CLP compared with those in the sham group, peaking at 4 h
for AST and 24 h for ALT (Table
I). GFZ treatment was able to reduce the elevations in AST and
ALT, with its effects reaching statistical significance at 2 and 4
h in the case of AST and at 4 h in the case of ALT. At 24 h after
CLP, LDH levels were significantly elevated, and GFZ treatment was
also able to attenuate this increase.
 | Table ISerum levels of ALT, AST and LDH. |
Table I
Serum levels of ALT, AST and LDH.
| Group | AST (UI) | ALT (UI) | LDH (UI) |
|---|
| Sham | 109.0±10.6 | 15.8±5.2 | 537.0±141.4 |
| CLP 2 h | 271.4±58.7a | 27.4±10.2 | |
| CLP 4 h | 293.8±113.9a | 39.8±16.3 | |
| CLP 24 h | 200.8±16.6a | 44.0±2.7a | 1983.4±530.7a |
| GFZ 2 h | 175.8±69.9b | 19.0±11.6 | |
| GFZ 4 h | 204.6±28.8b | 19.4±5.1b | |
| GFZ 24 h | 172.2±33.9 | 37.4±8.3 |
1057.4±403.2b |
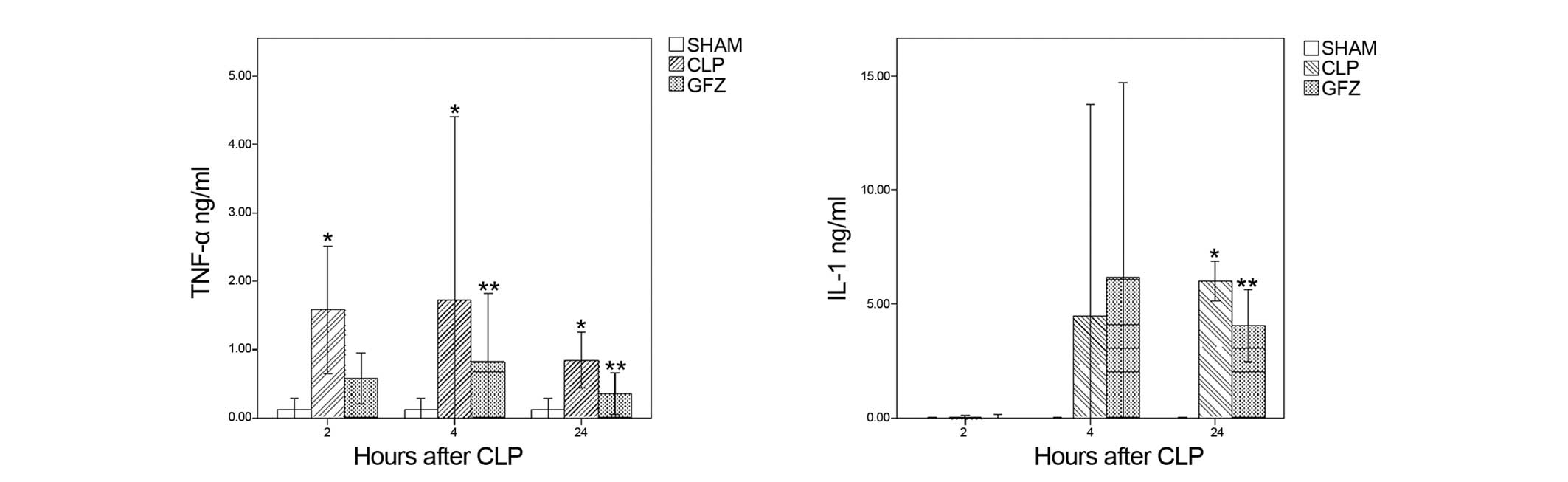
Serum cytokine levels
Levels of TNF-α were significantly elevated in all
time-points in the CLP group as compared with those in the sham
controls (Fig. 1). TNF-α levels
peaked at 4 h and remained elevated even at 24 h. GFZ treatment
resulted in significantly lower levels of TNF-α at 4 and 24 h after
CLP. In the case of IL-1, there was no difference between the
groups at 2 h, where levels were undetectable by the assay. At 4
and 24 h, the IL-1 levels were elevated; however, statistical
significance was reached only at 24 h. At this time-point, GFZ
reduced IL-1 levels significantly (Fig. 1).
MDA
There were two identifiable time-points of increased
MDA levels in the CLP group, at 2 and 24 h. However, no difference
was found between the CLP and GFZ groups (data not shown).
Survival
By 48 h, five rats in the CLP group and three in the
GFZ group had died. At 5 days, seven rats in the CLP group and five
rats in the GFZ group had died. The difference in survival between
groups did not reach statistical significance (P=0.1).
Discussion
PPARs have been studied in models of sepsis, and
PPAR-γ agonists have been found to be effective in reducing the
severity of endotoxic shock (17).
A recent study showed that PPAR-α expression was decreased in
patients with septic shock and that the values correlated with the
severity of disease; in addition, in the CLP model, knockout mice
lacking PPAR-α had decreased survival rates compared with wild-type
animals (18). Fenofibrate
treatment has been shown to reduce endothelial dysfunction and
endothelial cell injury in a rabbit model of endotoxemia by
lipopolysaccharide (LPS) injection (19). Improved endothelial-dependent
relaxation and decreased monocyte tissue factor expression were
observed. Another model of LPS-induced endotoxemia in rats also
demonstrated reductions in myocardial contractility depression and
in TNF-α levels after fenofibrate treatment (20). These results are in contrast to
those in another study where dietary fenofibrate caused increased
levels of TNF-α and mortality in endotoxemic wild-type mice, while
showing lower TNF-α levels in PPAR-α knockout mice (21). Using a physiologically relevant
model of abdominal sepsis, in the present study it was demonstrated
that GFZ pretreatment reduced the inflammatory response associated
with abdominal sepsis. GFZ had immunomodulatory effects, reducing
the circulating levels of TNF-α, IL-1 and MDA, as well as markers
of tissue injury such as AST and ALT. Differences between the LPS
injection and CLP models could be relevant in explaining these
inconsistent results, although the present study would support
those showing a beneficial effect of PPAR-α ligands such as
fibrates, despite only a trend towards a survival benefit being
observed.
Inflammatory cytokines play an important but complex
role in sepsis (1,2,22).
Some of the mechanisms by which fibrates might suppress
inflammatory cytokines are beginning to be uncovered. In a study
with LPS-activated cells, PPAR-α ligands, including fibrates, were
able to inhibit NF-κB DNA binding activity in astrocytes, leading
to a modulation of the expression of inflammatory genes responsible
for the production of cytokines such as IL-1 and TNF-α (23). Similar results were obtained in
LPS-stimulated cardiac myocytes (24), and in injured endothelial cells
(9). Clinical studies have shown
that GFZ reduces TNF-α production in human peripheral blood
mononuclear cells (25), and
fibrates reduce IL-1 in human whole blood stimulated by endotoxin
(26). Fibrates dose-dependently
inhibit cytokine production (ILs, TNF-α and interferons) in
activated T cells, probably via the inhibition of transcription
factors associated with the inflammatory response, such as
activator protein-1, c-Jun NH2-terminal protein kinase and P38
mitogen-activated protein kinase (27). The expression of IL-1 receptor
antagonist, which is acutely stimulated by LPS treatment in the
liver, can also be induced by PPARα (28). The switching of T cells from Th1 to
Th2 profiles by GFZ is responsible for the tissue protection
afforded against experimental encephalomyelitis in rats (12). Interestingly, the majority of
studies use LPS, a key mediator of the sepsis inflammatory cascade,
as a stimulant for cytokine production. In one study, using
LPS-stimulated airway inflammation, PPAR-α−/− mice
exhibited increased neutrophil infiltration and TNF-α production
compared with that in PPAR-α+/+ mice, and fenofibrate
was able to reduce TNF-α production in wild-type mice (8).
NF-κB is a key mediator of the sepsis inflammatory
cascade. NF-κB activity is markedly increased in every organ
studied, both in human and experimental models of septic shock, and
greater levels of NF-κB activity are associated with a higher rate
of mortality and worse clinical outcome in septic patients
(29). The inhibition of NF-κB,
and of the subsequent overproduction of inflammatory cytokines such
as TNF-α, appears to be a crucial step in the immunomodulatory
effects of PPAR-α activators. Cultured injured endothelial cells
show activation of NF-κB that can be inhibited by incubation with
fenofibrate (9). Fibrates were
able to induce the expression of the inhibitory protein IκBα in
human aortic smooth muscle cells as well as in primary human
hepatocytes, providing a possible mechanism for NF-κB inhibition
(30). Another study has also
linked TLR to PPAR-α signaling. The PPARα agonist fenofibrate was
found to reduce inflammatory cytokines and inflammation by
antagonizing LPS-mediated inflammatory responses in vascular smooth
muscle cells through a mechanism involving TLR-4 (31).
Marked oxidative stress results from the initiation
of the inflammatory response in sepsis, and it initiates changes in
mitochondrial function that may result in organ damage (32). Sepsis suppresses free fatty acid
oxidation with the result of increased circulating fatty acids,
through LPS-induced suppression of PPAR-α (33). Additionally, LPS induces the
production of MDA and depletes catalase and superoxide dismutase in
inflammatory cells (34). A
previous study found elevations in MDA and glutathione depletion
following CLP in rats (35).
Fibrates are known to diminish MDA production in diabetic rats
(36), and following severe liver
ischemia-reperfusion injury in rats, fibrate pretreatment is able
to reduce elevations in MDA and depletion of endogenous
antioxidants (37). Elevations in
MDA after CLP were observed in the present study, but only in
untreated animals. No difference in MDA levels was identified
between the CLP and GFZ group.
Although the inhibition of single cytokines or the
addition of antioxidants has not shown value in the treatment of
sepsis (38,39), the use of immunomodulators with
pleiotropic effects has been continuously studied (6). Lipid-lowering drugs such as statins
are currently thought to be prime candidates as adjunct treatments
in sepsis (40), and clinical
trials are underway. In this study it was found that another class
of lipid-lowering drugs, fibrates, also have immunomodulating
properties and could also be of value. The use of these drugs,
alone or in combination, warrants further study.
Acknowledgements
The authors would like to thank the staff at their
laboratories for invaluable assistance.
References
|
1
|
Nduka OO and Parrillo JE: The
pathophysiology of septic shock. Crit Care Clin. 25:677–702. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cinel I and Opal SM: Molecular biology of
inflammation and sepsis: a primer. Crit Care Med. 37:291–304. 2009.
View Article : Google Scholar
|
|
3
|
Dellinger RP, Levy MM, Carlet JM, et al:
Surviving sepsis campaign: international guidelines for management
of severe sepsis and septic shock: 2008. Intensive Care Med.
34:17–60. 2008. View Article : Google Scholar :
|
|
4
|
Neyrinck AP, Liu KD, Howard JP and Matthay
MA: Protective mechanisms of activated protein C in severe
inflammatory disorders. Br J Pharmacol. 158:1034–1047. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ranieri VM, Thompson BT, Barie PS, et al:
PROWESS-SHOCK Study Group: Drotrecogin alfa (activated) in adults
with septic shock. N Engl J Med. 366:2055–2064. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Parrish WR, Gallowitsch-Puerta M, Czura CJ
and Tracey KJ: Experimental therapeutic strategies for severe
sepsis: mediators and mechanisms. Ann NY Acad Sci. 1144:210–236.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Michalik L and Wahli W: Involvement of
PPAR nuclear receptors in tissue injury and wound repair. J Clin
Invest. 116:598–606. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Delayre-Orthez C, Becker J, Guenon I,
Lagente V, Auwerx J, Frossard N and Pons F: PPARalpha downregulates
airway inflammation induced by lipopolysaccharide in the mouse.
Respir Res. 6:912005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang TL, Chen MF, Luo BL, Xie QY, Jiang JL
and Li YJ: Fenofibrate decreases asymmetric dimethylarginine level
in cultured endothelial cells by inhibiting NF-kappaB activity.
Naunyn Schmiedebergs Arch Pharmacol. 371:401–407. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zambon A, Gervois P, Pauletto P, Fruchart
JC and Staels B: Modulation of hepatic inflammatory risk markers of
cardiovascular diseases by PPAR-alpha activators: clinical and
experimental evidence. Arterioscler Thromb Vasc Biol. 26:977–986.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ozansoy G, Akin B, Aktan F and Karasu C:
Short-term gemfibrozil treatment reverses lipid profile and
peroxidation but does not alter blood glucose and tissue
antioxidant enzymes in chronically diabetic rats. Mol Cell Biochem.
216:59–63. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roy A and Pahan K: Gemfibrozil, stretching
arms beyond lipid lowering. Immunopharmacol Immunotoxicol.
31:339–351. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dasgupta S, Roy A, Jana M, Hartley DM and
Pahan K: Gemfibrozil ameliorates relapsing-remitting experimental
autoimmune encephalomyelitis independent of peroxisome
proliferator-activated receptor-alpha. Mol Pharmacol. 72:934–946.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sivarajah A, Chatterjee PK, Hattori Y, et
al: Agonists of peroxisome-proliferator activated receptor-alpha
(clofibrate and WY14643) reduce renal ischemia/reperfusion injury
in the rat. Med Sci Monit. 8:BR532–BR539. 2002.PubMed/NCBI
|
|
15
|
Nanji AA, Dannenberg AJ, Jokelainen K and
Bass NM: Alcoholic liver injury in the rat is associated with
reduced expression of peroxisome proliferator-alpha
(PPARalpha)-regulated genes and is ameliorated by PPARalpha
activation. J Pharmacol Exp Ther. 310:417–424. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hubbard WJ, Choudhry M, Schwacha MG, Kerby
JD, Rue LW III, Bland KI and Chaudry IH: Cecal ligation and
puncture. Shock. 24(Suppl 1): 52–57. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wu WT, Lee CC, Lee CJ, Subeq YM, Lee RP
and Hsu BG: Rosiglitazone ameliorates endotoxin-induced organ
damage in conscious rats. Biol Res Nurs. 13:38–43. 2011. View Article : Google Scholar
|
|
18
|
Standage SW, Caldwell CC, Zingarelli B and
Wong HR: Reduced peroxisome proliferator-activated receptor α
expression is associated with decreased survival and increased
tissue bacterial load in sepsis. Shock. 37:164–169. 2012.
View Article : Google Scholar :
|
|
19
|
Wiel E, Lebuffe G, Robin E, et al:
Pretreatment with peroxysome proliferator-activated receptor alpha
agonist fenofibrate protects endothelium in rabbit Escherichia coli
endotoxin-induced shock. Intensive Care Med. 31:1269–1279. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jozefowicz E, Brisson H, Rozenberg S, et
al: Activation of peroxisome proliferator-activated receptor-alpha
by fenofibrate prevents myocardial dysfunction during endotoxemia
in rats. Crit Care Med. 35:856–863. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hill MR, Clarke S, Rodgers K, Thornhill B,
Peters JM, Gonzalez FJ and Gimble JM: Effect of peroxisome
proliferator-activated receptor alpha activators on tumor necrosis
factor expression in mice during endotoxemia. Infect Immun.
67:3488–3493. 1999.PubMed/NCBI
|
|
22
|
van der Poll T and van Deventer SJ:
Cytokines and anticytokines in the pathogenesis of sepsis. Infect
Dis Clin North Am. 13:413–426. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xu J, Chavis JA, Racke MK and Drew PD:
Peroxisome proliferator-activated receptor-alpha and retinoid X
receptor agonists inhibit inflammatory responses of astrocytes. J
Neuroimmunol. 176:95–105. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Takano H, Nagai T, Asakawa M, et al:
Peroxisome proliferator-activated receptor activators inhibit
lipopolysaccharide-induced tumor necrosis factor-alpha expression
in neonatal rat cardiac myocytes. Circ Res. 87:596–602. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rosenson RS: Effect of fenofibrate on
adiponectin and inflammatory biomarkers in metabolic syndrome
patients. Obesity (Silver Spring). 17:504–509. 2009. View Article : Google Scholar
|
|
26
|
Zhao SP, Ye HJ, Zhou HN, Nie S and Li QZ:
Gemfibrozil reduces release of tumor necrosis factor-alpha in
peripheral blood mononuclear cells from healthy subjects and
patients with coronary heart disease. Clin Chim Acta. 332:61–67.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cheng SM, Chu KM and Lai JH: The
modulatory mechanisms of fenofibrate on human primary T cells. Eur
J Pharm Sci. 40:316–324. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Stienstra R, Mandard S, Tan NS, et al: The
interleukin-1 receptor antagonist is a direct target gene of
PPARalpha in liver. J Hepatol. 46:869–877. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu SF and Malik AB: NF-kappaB activation
as a pathological mechanism of septic shock and inflammation. Am J
Physiol Lung Cell Mol Physiol. 290:L622–L645. 2006. View Article : Google Scholar
|
|
30
|
Delerive P, Gervois P, Fruchart JC and
Staels B: Induction of IkappaB alpha expression as a mechanism
contributing to the anti-inflammatory activities of peroxisome
proliferator-activated receptor-alpha activators. J Biol Chem.
275:36703–36707. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ji Y, Wang Z, Li Z and Liu J: Modulation
of LPS-mediated inflammation by fenofibrate via the TRIF-dependent
TLR4 signaling pathway in vascular smooth muscle cells. Cell
Physiol Biochem. 25:631–640. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Galley HF: Oxidative stress and
mitochondrial dysfunction in sepsis. Br J Anaesth. 107:57–64. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Maitra U, Chang S, Singh N and Li L:
Molecular mechanism underlying the suppression of lipid oxidation
during endotoxemia. Mol Immunol. 47:420–425. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Victor VM and De la Fuente M: Immune cells
redox state from mice with endotoxin-induced oxidative stress.
Involvement of NF-kappaB. Free Radic Res. 37:19–27. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Koksal GM, Sayilgan C, Aydin S, Oz H and
Uzun H: Correlation of plasma and tissue oxidative stresses in
intra-abdominal sepsis. J Surg Res. 122:180–183. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Olukman M, Sezer ED, Ulker S, Sözmen EY
and Cınar GM: Fenofibrate treatment enhances antioxidant status and
attenuates endothelial dysfunction in streptozotocin-induced
diabetic rats. Exp Diabetes Res. 2010:8285312010. View Article : Google Scholar
|
|
37
|
Boshra V and Moustafa AM: Effect of
preischemic treatment with fenofibrate, a peroxisome
proliferator-activated receptor-α ligand, on hepatic
ischemia-reperfusion injury in rats. J Mol Histol. 42:113–122.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lorente JA and Marshall JC: Neutralization
of tumor necrosis factor in preclinical models of sepsis. Shock.
24(Suppl 1): 107–119. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Szakmany T, Hauser B and Radermacher P:
N-acetylcysteine for sepsis and systemic inflammatory response in
adults. Cochrane Database Syst Rev. 9:CD0066162012.PubMed/NCBI
|
|
40
|
Mermis JD and Simpson SQ: HMG-CoA
reductase inhibitors for prevention and treatment of severe sepsis.
Curr Infect Dis Rep. 14:484–492. 2012. View Article : Google Scholar : PubMed/NCBI
|