Introduction
Lymphomas are a group of malignancies that occur in
the lymph nodes, extranodal lymphoid tissues and the
monocyte-macrophage cell system (1). Lymphomas can be divided into Hodgkin
lymphomas and non-Hodgkin lymphoma (NHLs), according to the
structure and composition of the tissue pathology. In addition,
according to the cell source, NHLs are divided into B-cell and
natural killer/T-cell types, while B-cell NHLs can be divided into
further subtypes, including diffuse large B-cell, mantle cell and
follicular lymphomas (2). In
recent years, the incidence of lymphomas has increased gradually
and significantly, particularly NHLs (3). The peritoneum, omentum and mesentery
are the most complex serosas, and are commonly involved in ovarian,
stomach, colon and colorectal cancers, serving as important
indicators in prognostic assessment (4). Enlarged lymph nodes are the
predominant imaging features of NHL, which indicates that enlarged
lymph nodes are the most common imaging manifestation (5), while involvement of the peritoneum,
omentum or mesentery is a rare phenomenon. Furthermore, NHLs
involving the omentum are not commonly observed in autopsies, but
are more common in diffuse large B-cell, mantle cell, follicular
cell and T-cell lymphomas (6).
Clinically, it is rare that NHL invades the peritoneum, omentum or
mesentery, however, lymphoma is considered in the differential
diagnosis of extensive peritoneal tumor lesions in computed
tomography (CT) images, as the treatment and prognosis differs
compared with other types of tumor and the method can improve
current understanding of CT signs of the disease. Therefore, the
aim of the present study was to investigate the correlation between
CT images and pathological observations of NHLs with omental,
peritoneal or mesenteric involvement.
Materials and methods
General materials
In total, 26 cases of NHLs with peritoneal, omental
or mesenteric involvement were admitted to the Shandong Tumor
Hospital (Jinan, China) between January 2003 and September 2010. An
NHL was pathologically confirmed in all the patients (male, 16;
female, 10; age range, 7–70 years; mean age, 46 years). The
clinical symptoms included abdominal pain, bloating, an abdominal
mass and changes in stool. The study was conducted in accordance
with the Declaration of Helsinki and with approval from the Ethics
Committee of the Affiliated Hospital of Shandong University of
Traditional Chinese Medicine (Jinan, China). Written informed
consent was obtained from all the participants.
Inspection methods
A 64-slice CT scanner (SOMATOM Sensation; Siemens,
Erlangen, Germany) was used to scan each patient between the
xiphoid process and the pubic symphysis plane, in a conventional
supine position (tube voltage, 120 kV; tube current, 240–330 mA;
layer thickness, 5 mm; pitch, 5 mm). The patients were administered
500 ml diatrizoate (1%) orally to fill the gastrointestinal tract
30 min prior to scanning. An intravenous bolus injection of the
nonionic contrast medium, iohexol (350 mg/ml; dose, 80–100 ml;
injection rate, 3 ml/sec), was applied to the elbow for enhanced
scanning (Hokuriku Pharmaceutical Co., Ltd., Beijing, China).
Image analysis
CT images were retrospectively analyzed by two
experienced radiologists who were unfamiliar with the pathological
situation of the patients. Features observed in the CT scans
included cord-like and tumor-like thickening of the peritoneum,
abdominal omental nodules, cake-like thickening of the omentum,
increased density of the mesenteric fat and a large number of
nodules. The CT values of the lymph nodes were significantly more
marked following the injection of intravenous contrast medium.
Statistical analysis
SPSS 11.5 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. Fisher’s exact test for
four-fold table was used for the exact test and P<0.05 was
considered to indicate a statistically significant difference. The
distribution of the NHL subtypes found in the patients was
statistically analyzed and the CT scan characteristics of the NHL
subtypes were compared.
Results
Quantitative distribution of patients
with peritoneal, omentalor mesenteric invasion by NHL subtypes
Diffuse large B-cell lymphomas were most commonly
diagnosed in NHL patients with peritoneal, omental or mesenteric
involvement, while the number of these patients diagnosed with the
other three subtypes was significantly lower (Table I).
 | Table IDistribution of non-Hodgkin lymphoma
subtypes in patients. |
Table I
Distribution of non-Hodgkin lymphoma
subtypes in patients.
| Item | Diffuse large
B-cell | Mantle cell | Follicular cell | T-cell |
|---|
| Cases, n | 18 | 2 | 2 | 4 |
| Distribution, % | 69.2 | 7.7 | 7.7 | 15.4 |
Distribution of CT scan characteristics
for NHL subtypes
As shown in Table
II, 18 patients were diagnosed with diffuse large B-cell
lymphoma, of which 15 (83.3%), 13 (86.7%) and 12 patients (66.7%)
were found to have cord-like thickening of the peritoneum, omental
nodular thickening of the abdomen and abdominal tumor-like
thickening, respectively. In addition, of the eight cases with a
different NHL subtype, one (12.5%), two (25.0%) and one (12.5%)
cases, respectively, were found to exhibit the aforementioned CT
scan characteristics. The number of diffuse large B-cell lymphoma
cases identified to exhibit the various CT scan characteristics was
significantly higher compared with the other NHL subtypes
(P<0.05). In total, nine (50.0%) and eight cases (44.4%) with
diffuse large B-cell lymphoma were found to exhibit omental
cake-like thickening and mesenteric root nodules, respectively,
while for the other NHL subtypes, five (62.5%) and six (75.0%)
patients exhibited these characteristics, respectively. However,
the probability of two or more CT scan characteristics occurring
was not found to be statistically significant when comparing the
NHL subtypes (P>0.05).
 | Table IIComparisons of various computed
tomography characteristics observed in patients with different
histological subtypes. |
Table II
Comparisons of various computed
tomography characteristics observed in patients with different
histological subtypes.
| Histological
subtypes | Peritoneal cord-like
thickening | Peritoneal nodular
thickening | Peritoneal tumor-like
thickening | Omental cake-like
thickening | Mesenteric root
nodules |
|---|
| Diffuse large |
| B-cell, % (n) | 83.3 (15/18) | 86.7 (13/18) | 66.7 (12/18) | 50.0 (9/18) | 44.4 (8/18) |
| Other, % (n) | 12.5 (1/8) | 25.0 (2/8) | 12.5 (1/8) | 62.5 (5/8) | 75.0 (6/8) |
| P-value | 0.001 | 0.038 | 0.030 | 0.683 | 0.216 |
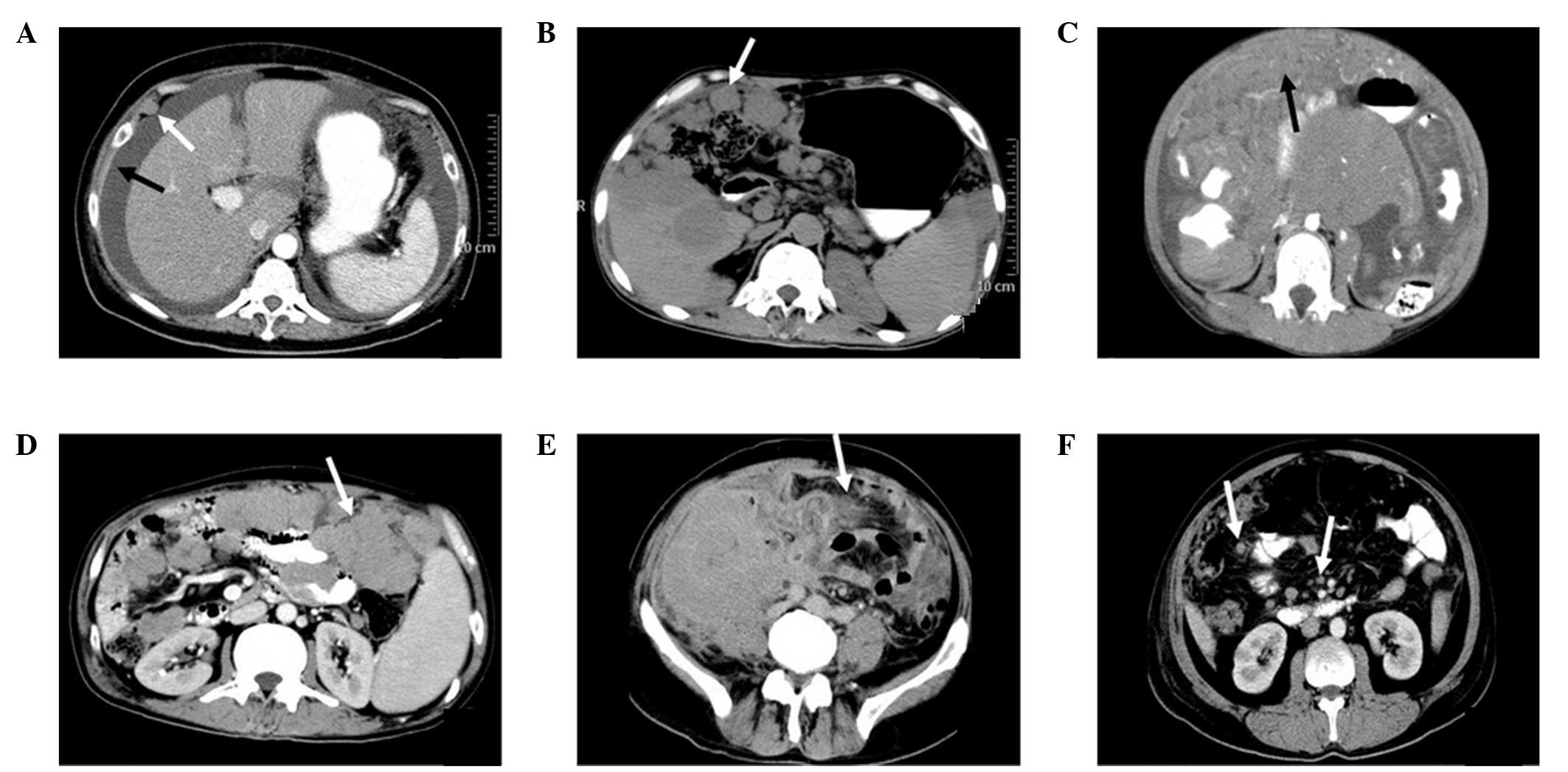
CT scans of NHL cases with peritoneal,
omental and mesenteric involvement
In total, eight cases were found to have peritoneal
thickening with significant enhancement, including nodular,
cord-like and tumor-like thickening (Fig. 1A). In addition, two cases exhibited
omental nodular thickening (Fig.
1B), seven cases showed omental cake-like thickening (Fig. 1C) and one case exhibited tumor-like
thickening (Fig. 1D). The fat
density of the intestinal interval increased (Fig. 1E) and numerous nodules were
observed in the mesenteric root (Fig.
1F).
Discussion
The peritoneum comprises serosal tissues with a wide
scope and complicated structure. Peritoneal primary tumors are less
common (peritoneal mesothelioma), while peritoneal secondary tumors
are commonly observed in ovarian, stomach, colon, colorectal,
pancreatic, endometrial and bladder cancers (7,8).
NHLs are a common lymphoid malignancy, identified as the isolation
or fusion of lymph nodes through imaging methods. However, NHLs
with peritoneal, omental or mesenteric involvement are rare
(9), but have been found to
exhibit similar CT scan characteristics to peritoneal metastasis.
Since NHLs require a completely distinct treatment method from
peritoneal carcinomatosis, the correct diagnosis of an NHL with
peritoneal, omental or mesenteric involvement is essential.
Lymphomas with peritoneal, omental or mesenteric
involvement have been identified to have a lower incidence in
females (10–12). In total, 26 patients diagnosed with
NHL participated in the present study, including 18 cases (69.2%)
of diffuse large B-cell NHL, two cases (7.7%) of mantle cell NHL,
two cases (7.7%) of follicular cell NHL and four cases (15.4%) of
T-cell NHL. Thus, diffuse large B-cell lymphoma was the most common
subtype in NHL patients with peritoneal, omental or mesenteric
involvement, which is consistent with the results of a previous
study (10).
The omentum consists of a fibrous tissue structure
without lymphoid tissues (10);
therefore, NHL with omental involvement is rare. At present, the
mechanisms underlying lymphoma invasion into omental pathways
remain unclear, but have been hypothesized to be similar to
gastrointestinal cancer metastasis and the spreading through the
transverse mesocolon and stomach mesocolon surface (13). Only 64 cases with peritoneal
involvement were identified in the autopsy of 322 NHL cases
(6).
CT manifestations of peritoneal lymphoma invasion
include diffuse peritoneal cord-like thickening, a smooth surface
and significant strengthening, as well as nodular thickening or
tumor-like thickening in a number of cases (9,10).
CT is the most effective method for the detection of peritoneal
thickening, and may even reveal submillimeter nodules. Among the
NHL cases, the CT scan results revealed 16 patients with peritoneal
cord-like thickening, nine patients with nodular thickening and six
patients with tumor-like thickening. All the cases exhibited
peritoneal involvement, accompanied by omental thickening or
mesangial nodules, with 16 cases also accompanied by a small or
moderate number of ascites.
NHLs with omental and mesenteric involvement are
commonly accompanied by intestinal lesions, with CT scans revealing
the presence of a cake-like soft tissue, nodule or mass (9). In the present study, 18 patients with
diffuse large B-cell lymphoma were diagnosed with omentum
involvement, including nine cases with omental cake-like
thickening, 13 cases with nodular thickening and 12 cases of
tumor-like thickening. Peritoneal and omental thickening are not
unusual characteristics of NHLs, but are more commonly a feature of
peritoneal metastases. The CT scans of the patients were similar,
and the diagnostic characteristics were difficult to identify.
Changes were identified in the omentum and peritoneum that were
reminiscent of tumor samples, which have been rarely reported in
patients with metastatic cancer. However, further confirmation is
required to clarify whether the observed CT features were due to
NHL.
Mesenteric root nodules and increased diffuse
mesenteric fat density were also common features of NHLs in the CT
scans. The nodules varied in size, had a high occurrence and often
oppressed the bowel; however, the nodules were not found in the
intestinal canal and obstruction was rarely observed. NHL can
invade the mesentry, and their CT signs include obscure gut
clearance, increased density and a fixed intestinal canal position.
Among the 26 patients, 14 cases were found to have mesenteric root
nodules and 12 cases were found to have increased fat density
around the bowel. However, mesenteric root nodules and increased
diffuse mesenteric fat density are not unique characteristics of
NHLs, and are commonly observed in peritoneal carcinomatosis and
tuberculosis. Therefore, the CT images obtained showed similar
characteristics to these diseases and providing a definitive
diagnosis was difficult.
The occurrence of peritoneal cord-like, abdominal
omental nodular and abdominal omental tumor-like thickening was
higher in diffuse large B-cell lymphoma cases compared with other
subtypes (P<0.05). However, the occurrence of omental cake-like
thickening and mesenteric root nodules in the NHL subtypes was not
found to be statistically significant (P>0.05). Thus, diffuse
large B-cell lymphoma is likely to cause peritoneal thickening,
nodular thickening of the abdominal omentum and abdominal omental
tumor-like thickening. The cake-like omental thickening and
mesenteric root nodules between the various NHL subtypes exhibited
no characteristic distribution and, due to increased omentum, no
significant differences were detected between the mesenteric root
nodules between each NHL subtype.
To identify between NHLs with peritoneal, omental
and mesenteric involvement and peritoneal metastases, tumor markers
can be used. Peritoneal metastases are malignant and exhibit
elevated levels of tumor markers. In addition, the peritoneum and
omentum exhibit cake-like or nodular thickening, abdominal or
retroperitoneal tumors, smaller lymph nodes, limited bowel
involvement and obstruction is a common feature. By contrast, the
NHL invasion of the peritoneum and omentum may exhibit omental
tumor-like thickening, with a wide range of bowel involvement and
visible ‘aneurysmal dilatation’ (14), often accompanied by liver or spleen
involvement.
Epstein et al (16) hypothesized that high-density
ascites, along with other CT features, were characteristic of
tuberculosis. Intestine, liver and spleen involvement is less
common in peritoneal tuberculosis; thus, the conditions may be
differentiated and diagnosed by clinical investigation.
CT scans of NHLs with peritoneal, omental and
mesenteric involvement revealed peritoneal cord-like, abdominal
omental nodular, abdominal omental tumor-like and omental cake-like
thickening, as well as increased fat density of the bowel interval
and mesenteric gap roots nodules with no specificity. NHLs with
peritoneal, omental and mesenteric involvement were more common in
diffuse large B-cell lymphoma cases. Therefore, diffuse large
B-cell lymphoma is more likely to cause peritoneal cord-like,
abdominal omental nodular, abdominal omental tumor-like and omental
cake-like thickening, as well as mesenteric root nodules, in
various pathological subtypes with no specificity. These CT
characteristics are not specific signs of peritoneal and omental
invasion by NHL, and other diseases may exhibit the same
characteristics. In cases with no typical CT scan characteristics,
the CT images of NHLs with peritoneal, omental and mesenteric
involvement were difficult to distinguish from CT images of
peritoneal metastasis and tuberculosis. In these cases, an
aspiration biopsy is required to confirm the diagnosis.
References
|
1
|
Zhou K, Yan F and Zhou L: Lymphatic
System. CT of the Abdomen. 1st Edition. Shanghai Medical University
Press; Shanghai: pp. 2741993
|
|
2
|
Terzidis IP, Christodoulou AG, Ploumis AL,
Metsovitis SR, Koimtzis M and Givissis P: The appearance of kissing
contusion in the acutely injured knee in the athletes. Br J Sports
Med. 38:592–596. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weng Y, Zhang F and Zhou L: Extranodal
Lymphoma of the abdomen: CT imaging manifestations with pathologic
correlation. Zhongguo Yi Xue Ji Suan Ji Cheng Xiang Za. 18:35–38.
2012.(In Chinese).
|
|
4
|
Sharifah MI, Zamzami NA and Rafeah TN:
Diffuse peritoneal lymphomatosis simulating peritoneal
carcinomatosis. Med J Malaysia. 66:270–272. 2011.PubMed/NCBI
|
|
5
|
Yang ZG, Zuo P, Yu J and Chen Z: Helical
CT features of abdominal malignant lymphoma. Lin Chuang Fang She
Xue Za Zhi. 22:680–683. 2003.(In Chinese).
|
|
6
|
Gadage V, Kembhavi S, Kumar P and Shet T:
Primary cardiac diffuse large B-cell lymphoma with activated
B-cell-like phenotype. Indian J Pathol Microbiol. 54:591–593. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kobayashi Y, Sugitani S, Oseki K and Iiri
T: A case of meningeal carcinomatosis due to gastric cancer treated
with intrathecal chemotherapy. Nihon Shokakibyo Gakkai Zasshi.
108:1696–1704. 2011.(In Japanese). PubMed/NCBI
|
|
8
|
Tombesi P, Di Vece F, Ermili F, Fabbian F
and Sartori S: Role of ultrasonography and contrast-enhanced
ultrasonography in a case of Krukenberg tumor. World J Radiol.
5:321–324. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sia DS, Kapur J and Thian YL: Peritoneal
lymphomatosis mimicking peritoneal carcinomatosis: important
imaging clues for correct diagnosis. Singapore Med J. 54:e93–e96.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Karaosmanoglu D, Karcaaltincaba M, Oguz B,
Akata D, Ozmen M and Akhan O: CT findings of lymphoma with
peritoneal, omental and mesenteric involvement: peritoneal
lymphomatosis. Eur J Radiol. 71:313–317. 2009. View Article : Google Scholar
|
|
11
|
Kim Y, Cho O, Song S, Lee H, Rhim H and
Koh B: Peritoneal lymphomatosis: CT findings. Abdom Imaging.
23:87–90. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lynch MA, Cho KC, Jeffrey RB Jr, Alterman
DD and Federle MP: CT of peritoneal lymphomatosis. AJR Am J
Roentgenol. 151:713–715. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jin H and Min PQ: Computed tomography of
gastrocolic ligament: involvement in malignant tumors of the
stomach. Abdom Imaging. 32:59–65. 2007. View Article : Google Scholar
|
|
14
|
Fan Z, Li ZP, Meng ZF, Zhong YG and Xu DS:
The CT findings of non-Hodgkin’s lymphoma in the abdominal cavity
of children. Zhonghua Fang She Xian Yi Xue Za Zhi. 38:273–276.
2004.(In Chinese).
|
|
15
|
Marshall JB: Tuberculosis of the
gastrointestinal tract and peritoneum. Am J Gastroenterol.
88:989–999. 1993.PubMed/NCBI
|
|
16
|
Epstein BM and Mann JH: CT of abdominal
tuberculosis. AJR Am J Roentgenol. 139:861–866. 1982. View Article : Google Scholar : PubMed/NCBI
|