Introduction
Type 2 diabetes mellitus has become a worldwide
epidemic with a prevalence that has tripled in the last 30 years,
and is predicted to affect >350 million individuals by 2025
(1). Despite lifestyle and
pharmacological interventions, patients with type 2 diabetes
mellitus continue to experience increases in glucose levels over
time, which is likely to be as a consequence of declining β-cell
function. One study found that approximately two-thirds of patients
with type 2 diabetes mellitus in developed countries do not
effectively control their glucose levels and that an even greater
proportion does not do so in developing countries, particularly in
China (2). A major reason for this
failure is the progressive nature of type 2 diabetes mellitus,
which makes it difficult for patients to maintain target levels of
glycated hemoglobin (hemoglobin A1c; HbA1c) using traditional
glucose-lowering agents, and usually requires them to take multiple
antihyperglycemic agents (AHAs) to attain or maintain glycemic
control.
Metformin, a commonly used oral antihyperglycemic
agent used as a monotherapy and in combination with other
antihyperglycemic agents, was introduced in the 1950s for the
treatment of type 2 diabetes mellitus. Metformin has many
advantages, including that it neither promotes weight gain nor
causes hypoglycemia, it exerts beneficial effects on cardiovascular
risk (3) and is well tolerated and
inexpensive (4). Due to these
advantages, clinical practice guidelines (5–8)
recommend metformin as the first-line oral antihyperglycemic drug
for treating most patients with type 2 diabetes mellitus when
glycemic control cannot be achieved by lifestyle interventions
alone. Sulfonylureas are frequently used as a second-line therapy
if the use of metformin alone does not achieve acceptable glycemic
control (9); however, an increased
risk of hypoglycemia and weight gain can result from sulfonylurea
treatment (10). Newer treatment
options and combination therapies that sustain glycemic control
with fewer such adverse effects are, therefore, being evaluated.
Sitagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor, is an
incretin-based therapy that is effective and well tolerated when
used in addition to metformin therapy (11,12).
Furthermore, when added to metformin the risk of hypoglycemia with
sitagliptin is similar to that observed using metformin with
placebo (13). Several combination
trials (14–19) have compared the efficacy and safety
of sitagliptin with sulfonylurea therapy in patients with type 2
diabetes mellitus who are experiencing inadequate glycemic control
(HbA1c >6.5 mmol/l and <10%) on metformin monotherapy;
however, the trials reported conflicting results and used modest
sample sizes (15–18). To clarify these findings, in the
current study a meta-analysis was conducted of all the published
RCTs to compare the efficacy and safety of combined metformin and
sitagliptin therapy with combined metformin and sulfonylurea
therapy in patients with type 2 diabetes mellitus who had been
experiencing inadequate glycemic control when treated with
metformin monotherapy.
Materials and methods
Literature search
The Medline, Embase, Cochrane Library, Chinese
National Knowledge Infrastructure and Chinese Biomedical Literature
databases were systematically searched to identify studies
published in English between January 2000 and December 2012 or
published in Chinese between January 1996 and December 2012 using
the following search terms: Type 2 diabetes mellitus, type II
diabetes mellitus, diabetes mellitus type 2, metformin,
sitagliptin, sulfonylurea, glibenclamide, gliclazide, glipizide
controlled-release tablets, gliquidone, glimepiride, dipeptidyl
peptidase-4 and clinical trial. Following retrieval of the relevant
articles, a manual search of the references was performed to
identify the relevant trials. Attempts were also made to contact
investigators for unpublished data and the full text of articles
when deemed necessary for clarification or for more information.
Two investigators reviewed all potentially relevant articles
independently to determine whether they met all the inclusion
criteria and none of the exclusion criteria.
Study selection
Studies were included in the analysis if they met
all the following inclusion criteria: i) Use of a prospective RCT;
ii) comparison of combined metformin and sitagliptin therapy with
combined metformin and sulfonylurea therapy in the treatment
groups; iii) treatment of patients for ≥12 weeks; iv) inclusion of
patients who had not been achieving their glycemic targets with
metformin monotherapy; and iv) reporting of outcomes in terms of
HbA1c values. Trials were excluded if they met one or both of the
following exclusion criteria: i) Evaluation of the addition of more
than one drug to metformin monotherapy and/or ii) inclusion of
participants using background therapies other than metformin
monotherapy. Methodological quality assessment was conducted using
the Cochrane Collaboration’s tool for assessing the risk of bias in
randomized trials. The RCTs were assessed for quality according to
the criteria of i) method of randomization; ii) allocation
concealment; iii) blinding of participants; iv) addressing of
incomplete data; v) freedom of selective reporting; vi)
comparability of groups at baseline; and vii) sample size
calculation. The trials were independently reviewed and graded by
two investigators who resolved any disagreements through
discussion.
Outcome measures
The primary outcome measure was the mean change in
HbA1c values from baseline to study endpoint. Secondary outcomes
included the proportion of participants achieving <7% HbA1c body
weight, and the occurrence of hypoglycemia.
Data extraction
Two investigators independently reviewed the titles,
abstracts and full texts of articles for inclusion using
standardized data extraction forms. Validity assessment was
performed using the Jadad scale (20). Disagreements were discussed between
investigators until agreement had been achieved. The following data
were extracted from each trial: i) An individual reference
identifier which indicated author and publication year; ii)
fundamental study data, including indication, treatment duration,
number of patients randomized, treatment aims and background
medication; iii) patient characteristics at baseline, including
mean age, gender, ethnicity, duration of type 2 diabetes mellitus,
body mass index and HbA1c values; iv) quality measures, including
the means of random sequence generation, allocation concealment,
blinding and efficacy analysis; the dropout rate; and the funding
source(s); and v) endpoint values, including the mean change in
HbA1c values; the number of patients achieving <7% HbA1c; the
change in body weight and the incidence of hypoglycemia.
Statistical analysis
The analyses were performed using Review Manager
(version 5.0; The Cochrane Collaboration, Copenhagen, Denmark) and
Stata (version 10; Stata Corp, College Station, TX, USA) software.
The heterogeneity of treatment effects among the studies was
formally tested with Cochrane’s test at a significance level of
P<0.1 and determination of the I2 statistic, with
I2>50% considered an indication of significant
heterogeneity between two trials. A random-effects model was used
in the presence of heterogeneity and a fixed-effects model in the
absence of heterogeneity. The weighted mean difference (WMD) or
odds ratio and its 95% confidence interval (CI) for each outcome
relative to the control were calculated for continuous and
dichotomous variables, respectively. Studies were excluded from the
meta-analysis if insufficient information was provided to enable
standard error calculation.
Results
Study selection
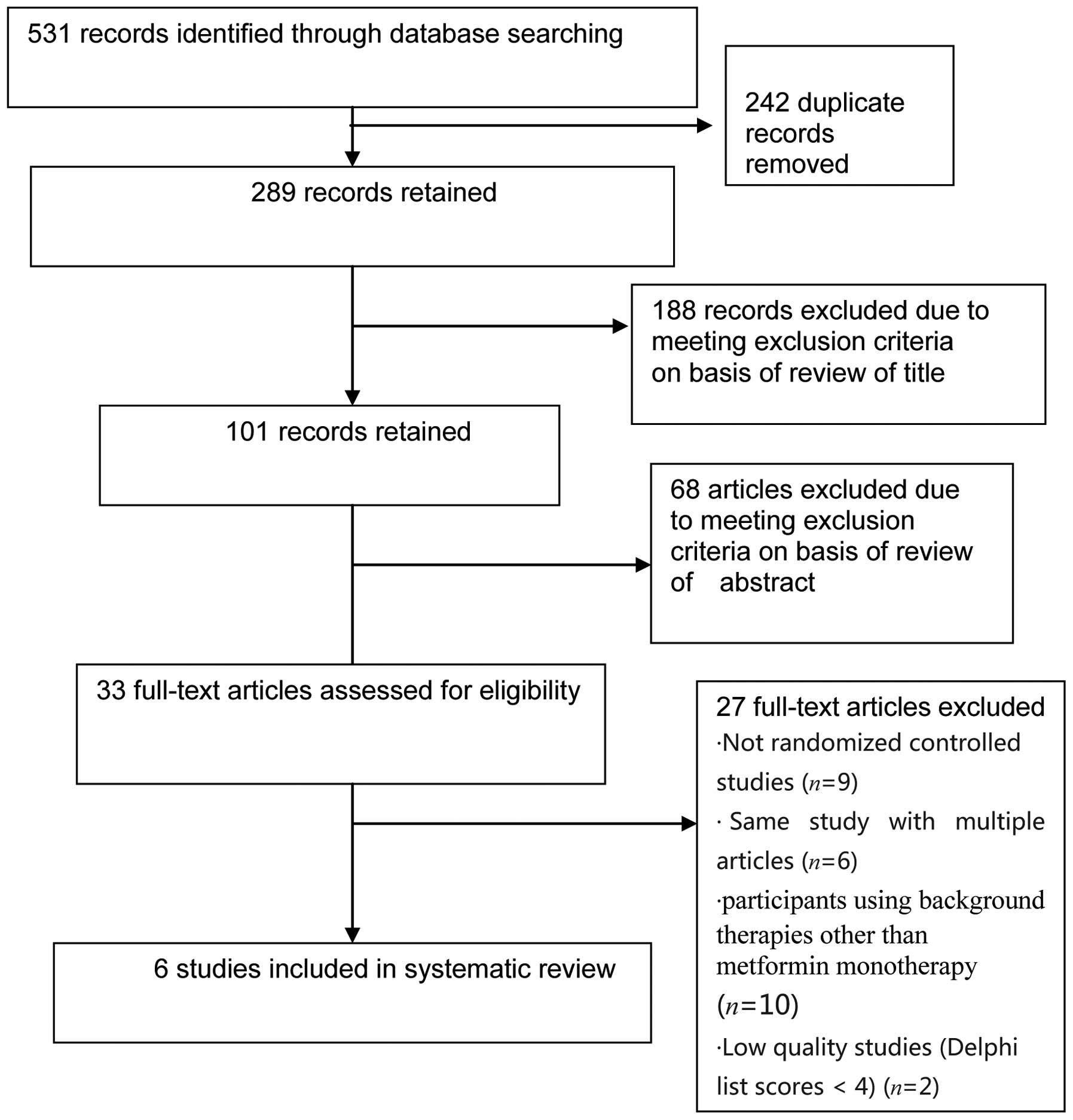
The database search results are summarized in
Fig. 1. Among the 33 full-text
articles that were assessed for eligibility, six reported the
results of six RCTs (14–17,19,20)
that fulfilled all the inclusion criteria and none of the exclusion
criteria. The main reasons for the exclusion of six potential RCTs
were the evaluation of the addition of more than one drug with
metformin monotherapy, the inclusion of participants undergoing
background therapies other than metformin, trial durations of
<12 weeks, and a lack of participant randomization.
Study and patient characteristics
Table I summarizes
the characteristics of the six RCTs and the 3,585 participants that
they included. As can be observed, the mean patient age ranged from
53 to 59 years, the percentage of male patients from 48.3 to 62.9%,
and the baseline HbA1c level from 7.3 to 8.8%.
 | Table ICharacteristics of studies and
patients in six randomized controlled trials. |
Table I
Characteristics of studies and
patients in six randomized controlled trials.
| First author, year,
country (ref) | Interventions | Patient
characteristics | Duration (weeks) | Outcomes
measured |
|---|
| Seck, 2010, USA
(17) |
-
Sitagliptin 100 mg qd + metformin ≥1500 mg qd
-
Glipizide 5–20 mg qd + metformin ≥1500 mg qd
| N=1172
Sitagliptin + metformin, n=588; glipizide + metformin,
n=584
Mean age (years): Sitagliptin + metformin, 57.6; glipizide +
metformin, 57.0
Sex ratio (%): Sitagliptin + metformin, 57.3M/42.7 F glipizide +
metformin, 62.9 M/37.1 F
HbA1c (%): Sitagliptin + metformin, 7.3; glipizide + metformin,
7.3
BMI (kg/m2): Sitagliptin + metformin, 30.9; glipizide +
metformin, 31.3
Ethnicity: Caucasian, Black, Hispanic, Asian, other
T2DM duration (years): 6.2–6.5 | 104 | Primary: HbA1c
level
Other: FPG level, insulin level, proinsulin level, lipid profiles,
β-cell function, (HOMA-β value) PR/IR, HOMA-IR quantitative insulin
percentage with HbA1c <7%, incidence of adverse events,
safety |
| Li, 2012, China
(19) |
-
Sitagliptin 100 mg qd + metformin ≥1500 mg qd
-
Glimepiride 1–4 mg qd + metformin ≥1500 mg qd
| N=116
Sitagliptin + metformin, n=58; glimepiride + metformin,
n=58
Mean age (years): Sitagliptin + metformin, 53.7; glimepiride +
metformin, 54.0
Sex ratio (%): Sitagliptin + metformin, 48.3 M/50 F; glimepiride +
metformin, 50 M/50 F
HbA1c (%): Sitagliptin + metformin, 8.8; glimepiride + metformin,
8.6
BMI (kg/m2): Sitagliptin + metformin, 26.7; glimepiride
+ metformin, 26.5
Ethnicity: Chinese
Diabetes duration: NR | 24 | Primary: HbA1c
level
Other: percentage with HbA1c <7%, FPG level, 2HPPG level,
incidence of adverse events |
| Koren, 2012, Israel
(15) |
-
Sitagliptin 100 mg qd + metformin ≥1500 mg qd
-
Glibenclamide 5 mg qd + metformin ≥1500 mg qd
| All patients:
N=40
Mean age (years): 59
Gender ratio (%): 62.5 M/37.5 F
HbA1c: 8.3%
BMI (kg/m2): 31
Ethnicity: NR
Diabetes duration: NR | 12 | Primary: arterial
stiffness
Other: HbA1c level, FPG level, blood pressure, lipid profiles,
hsCRP level, BMI, STAT-8-isoprostane level, incidence of adverse
events |
| Nauck, 2007, USA
(16) |
-
Sitagliptin 100 mg qd + metformin ≥1500 mg qd
-
Glipizide 5–20 mg qd + metformin ≥1500 mg qd
| N=1172
Sitagliptin + metformin, n=588; glipizide + metformin,
n=584
Mean age (years): Sitagliptin + metformin, 56.8; glipizide +
metformin, 56.6
Sex ratio (%): Sitagliptin + metformin, 57.1 M/42.9 F; glipizide +
metformin, 61.3 M/38.7 F
HbA1c (%): Sitagliptin + metformin, 7.7; glipizide + metformin,
7.6
BMI (kg/m2): Sitagliptin + metformin, 31.2; glipizide +
metformin, 31.3
Ethnicity: Caucasian, Black, Hispanic, Asian, other
Diabetes duration (years): 6.2–6.5 | 52 | Primary: HbA1c
level
Other: FPG level, insulin level, percentage with HbA1c <7.0%,
proinsulin lipid profiles, β-cell function (HOMA-β value, PI/IR
HOMA-IR value, quantitative insulin index (QUICKI), incidence of
adverse events, safety |
| Arechavaleta, 2011,
USA (14) |
-
Sitagliptin 100 mg qd + metformin ≥1500 mg qd
-
Glimepiride 1–6 mg qd + metformin ≥1500 mg qd
| N=1035
Sitagliptin + metformin, n=516; glimepiride + metformin,
n=519
Mean age (years): Sitagliptin + metformin, 56.3; glimepiride +
metformin, 56.2
Sex ratio (%): Sitagliptin + metformin, 55.0 M/46.2 F; glimepiride
+ metformin, 53.8 M/46.2 F
HbA1c (%): Sitagliptin + metformin, 7.5; glimepiride + metformin,
7.5
BMI (kg/m2): Sitagliptin + metformin, 29.7; glimepiride
+ metformin, 30.2
Ethnicity: 37.8–38.0% Hispanic or Latino, 62–62.2% other
Diabetes duration (years): 6.8–6.7 | 30 | Primary: HbA1c
level
Other: FPG level, percentages with HbA1c <7.0 and <6.5%,
lipid profiles, incidence of adverse events, safety |
| Srivastava, 2012,
India (18) |
-
Sitagliptin 50/100 mg qd + metformin ≥1500 mg qd
-
Glimepiride 0.5 mg qd + metformin ≥1500 mg qd
| N=50
sitagliptin + metformin, n=25; glimepiride + metformin,
n=25
Mean age (years): NR
Gender ratio (%): NR
HbA1c (%): Sitagliptin + metformin, 8.28; glimepiride + metformin,
8.25
BMI (kg/m2): Sitagliptin + metformin, 25.27; glimepiride
+ metformin, 26.48
Ethnicity: NR
Diabetes duration: NR | 18 | Primary: HbA1c
level
Other: percentage with HbA1c <7%, FPG level, 2HPPG level, BMI,
incidence of adverse events |
Methodological quality and risk of
bias
Table II shows the
results of the assessment of risk of bias. As can be observed, the
studies were found to be of moderate to high quality, with the
majority fulfilling five to seven of the seven quality criteria.
Specifically, one study fulfilled three criteria, one study
fulfilled five criteria and the remaining three studies fulfilled
seven criteria. The use of blinding was not deemed practical in
several RCTs.
 | Table IIResults of quality assessment of six
randomized controlled trials. |
Table II
Results of quality assessment of six
randomized controlled trials.
| First author, year
(ref) | Allocation
concealment | Blinding | Randomization | Percentage that
completed the trial | Intention- to-treat
analysis | Free of selective
reporting | Groups comparable at
baseline |
|---|
| Nauck, 2007 (16) | Yes | Yes, double
blind | Computer-generated
allocation schedule | 68 | Yes | Yes | Yes |
| Arechavaleta, 2011
(14) | Yes | Yes, double
blind | Computer-generated
allocation schedule | 90 | Yes | Yes | Yes |
| Srivastava, 2012
(18) | Unclear | Unclear | Computer-generated
random number | 100 | No | Yes | Yes |
| Seck, 2010
(17) | Yes | Yes, double
blind | Computer-generated
allocation schedule | 43 | Yes | Yes | Yes |
| Li, 2012 (20) | Unclear | Unclear | Random number
table | 100 | No | Yes | Yes |
| Koren, 2012
(19) | No | Open-label
crossover trial | Recruitment
order | 85 | Yes | Yes | Yes |
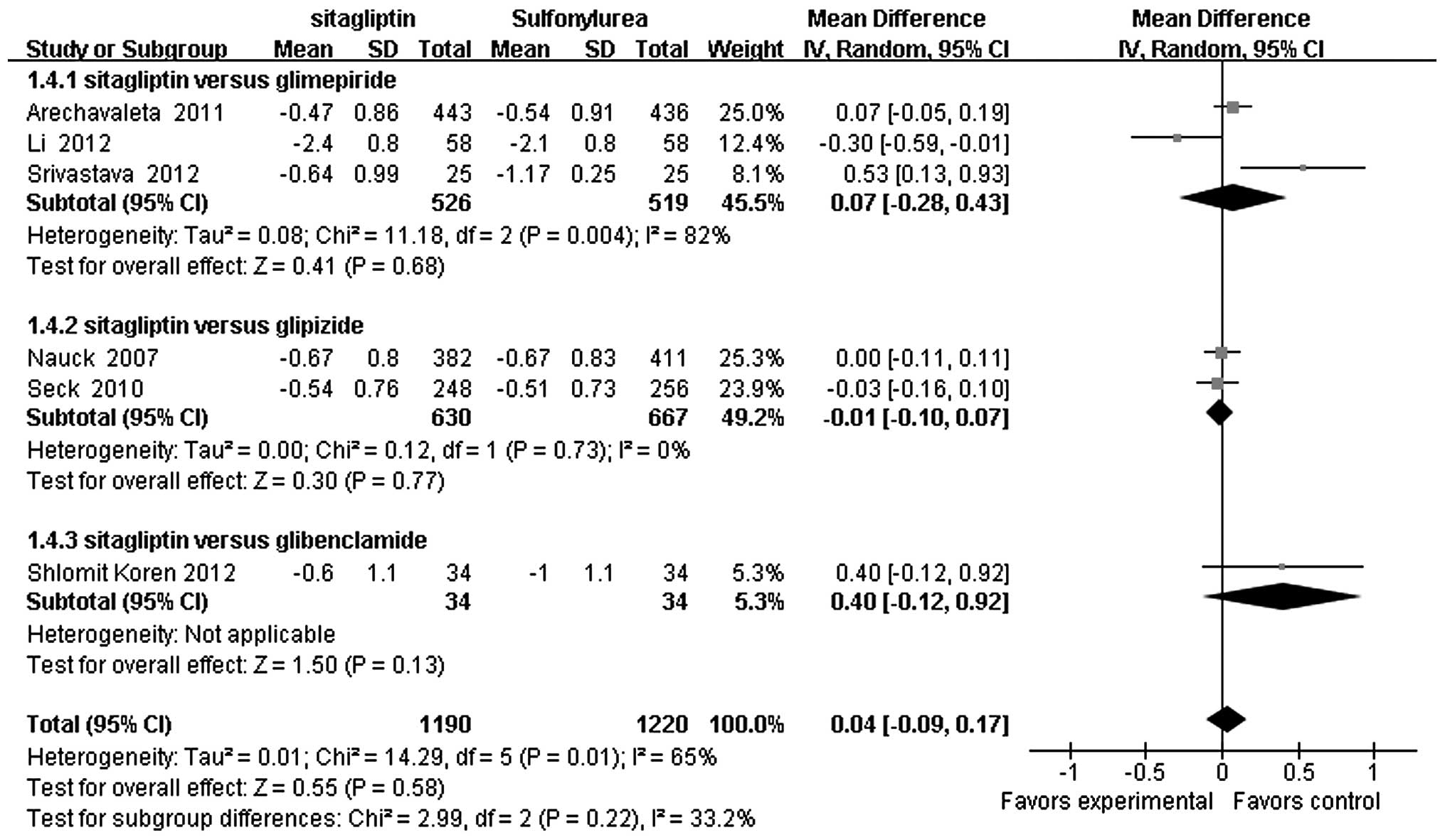
Change in HbA1c values and HbA1c
goal
Fig. 2 shows the
results of the meta-analysis of the change in HbA1c from baseline
(i.e., the effect estimate), the primary outcome of the six RCTs
that reported a change in HbA1c for 2,410 subjects. As can be
observed, no significant differences were found between the
metformin plus sitagliptin and the metformin plus sulfonylurea
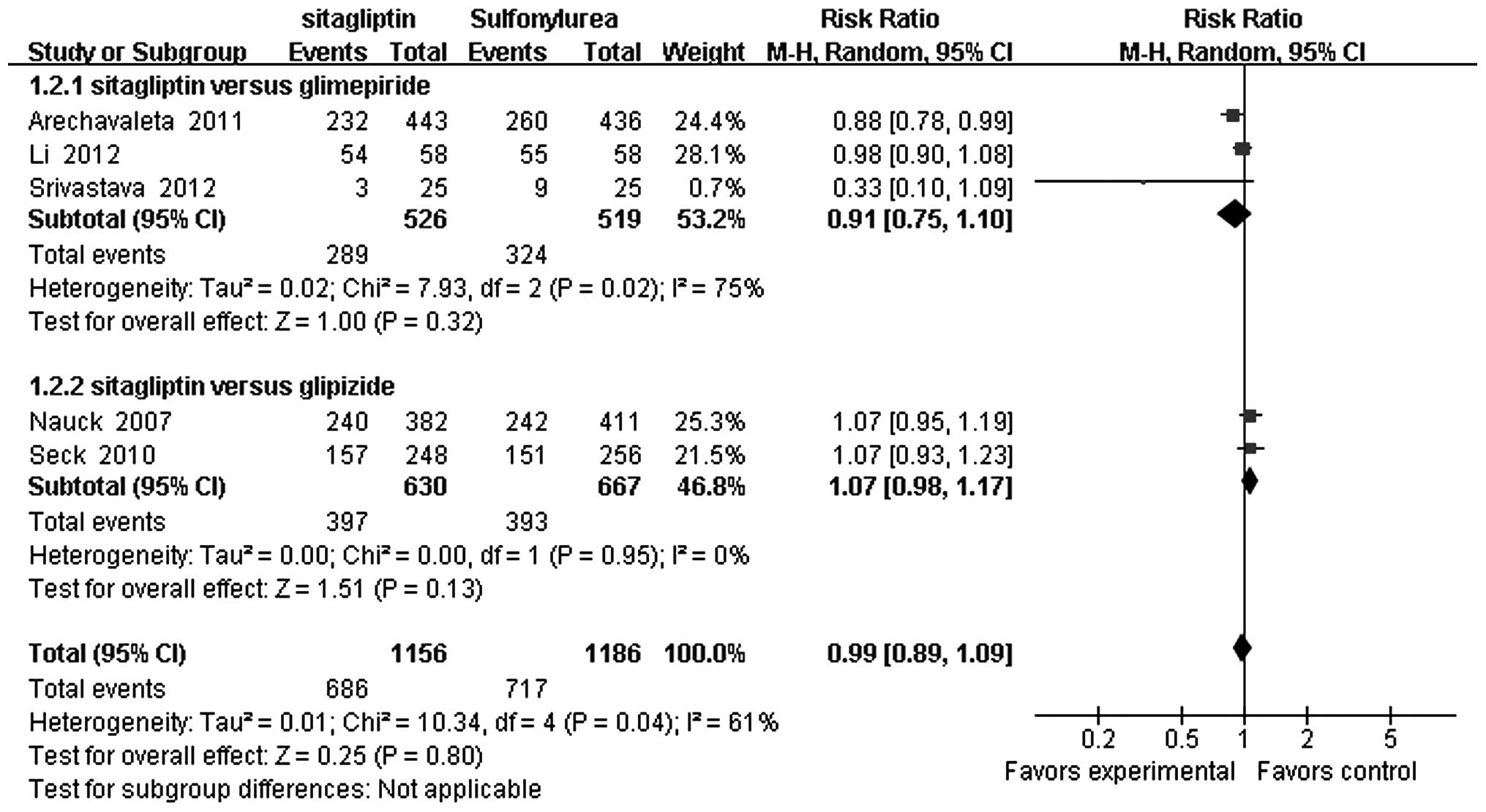
groups (WMD=0.04, 95% CI −0.09 to 0.17, P=0.58). Fig. 3 shows the results of the
meta-analysis of the risk ratio for achieving <7% HbA1c for the
five RCTs that reported the achievement of this goal for 2,342
subjects. As can be observed, no significant differences were found
between the metformin plus sitagliptin and the metformin plus
sulfonylurea groups in the attainment of this goal [risk ratio
(RR)=0.99, 95% CI 0.89–1.09, P=0.80].
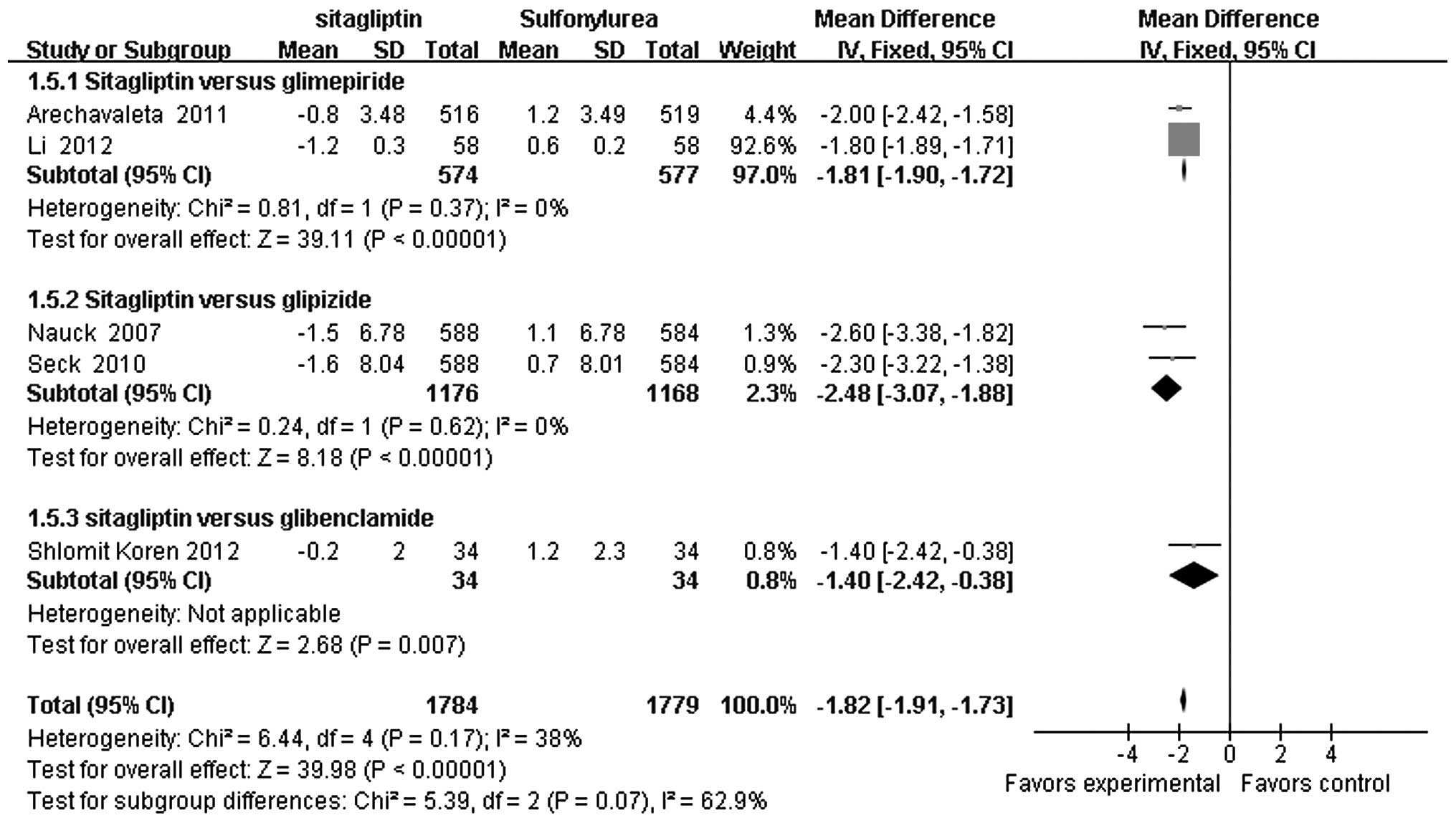
Body weight
Fig. 4 shows the
results of the meta-analysis of the change in body weight for the
five trials that reported a change for 3,563 subjects. As can be
observed, the metformin plus sitagliptin group was found to
experience a significantly greater loss in body weight compared
with the metformin plus sulfonylurea group (WMD=−1.82; 95% CI,
−1.91 to −1.73; P<0.00001).
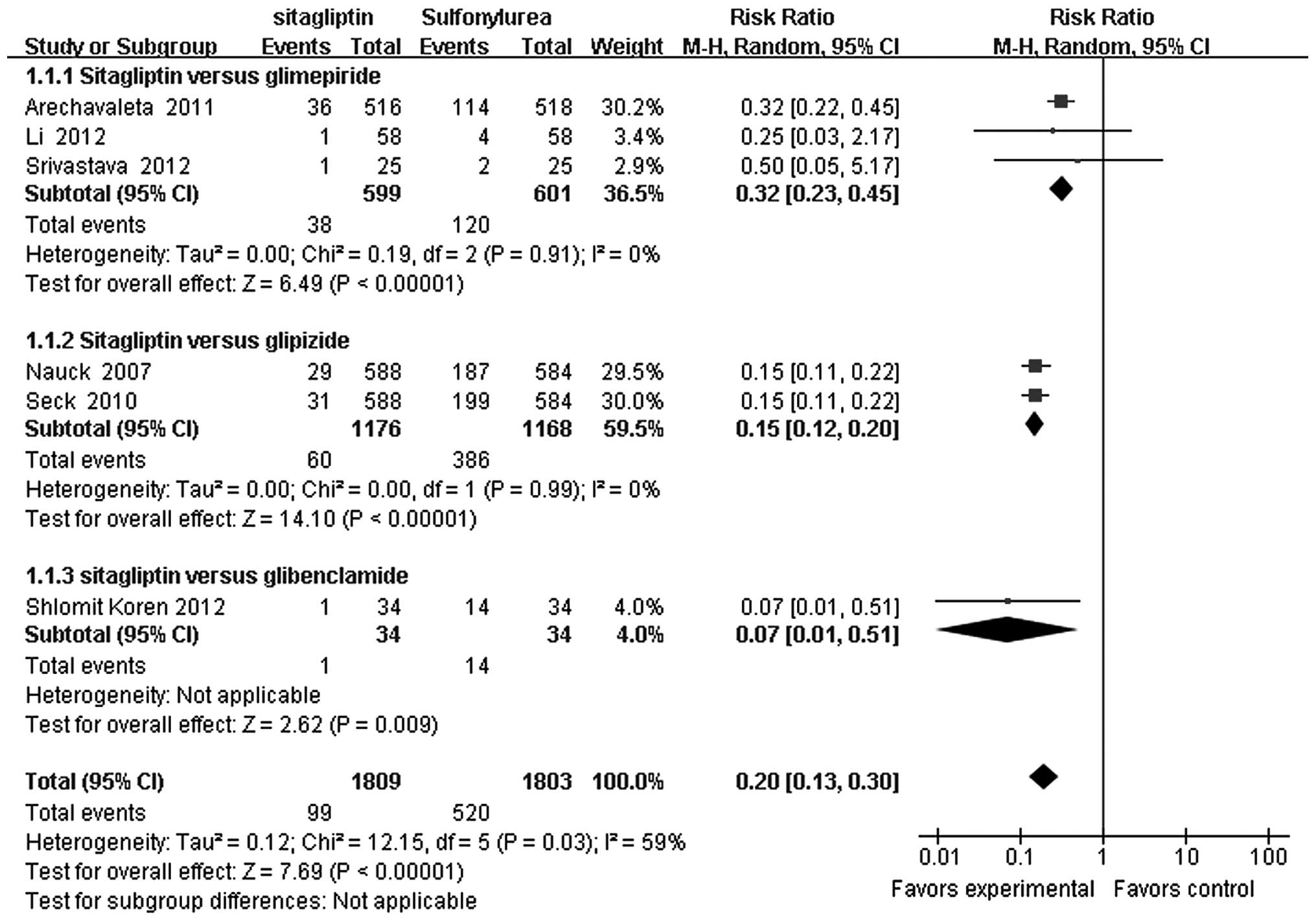
Hypoglycemic events
Fig. 5 shows the
results of the meta-analysis of the six RCTs that reported that
3,612 patients had experienced at least one hypoglycemic event. As
can be observed, the metformin plus sitagliptin group was found to
experience significantly fewer hypoglycemic events compared with
the metformin plus sulfonylurea group (RR=0.20; 95% CI, 0.13–0.30;
P<0.00001).
Discussion
The results of the meta-analyses conducted in this
study strongly indicate that the addition of sitagliptin therapy to
the regimen of patients with type 2 diabetes mellitus who are
currently undergoing metformin monotherapy but failing to achieve
their glycemic targets can result in a reduction in HbA1c values
similar to that resulting from the addition of sulfonylurea therapy
to metformin monotherapy. Metformin plus sulfonylurea therapy,
however, was not found to lower the risk of hypoglycemia to the
same extent as metformin plus sitagliptin therapy. Since
sulfonylurea stimulation of insulin secretion is not strictly
glucose dependent (21),
sulfonylurea agents continue to stimulate insulin secretion even
with falling glucose concentrations (22). By contrast, sitagliptin inhibits
the enzymatic degradation and inactivation of glucagon-like
peptide-1 (GLP-1), thus increasing endogenous GLP-1 and gastric
inhibitory polypeptide levels (23,24).
GLP-1 then potentially stimulates insulin secretion and inhibits
glucagon release effects that disappear when glucose levels
approach normal concentrations (25). Sitagliptin also induces stimulation
of insulin release and the suppression of glucagon release in a
glucose-dependent fashion.
The results also suggest that metformin plus
sitagliptin therapy results in greater weight loss compared with
metformin plus sulfonylurea therapy. Regarding the underlying
mechanism, sitagliptin can increase endogenous GLP-1, which, by
delaying gastric-emptying, increases satiety, resulting in
significant weight loss (26).
This beneficial effect is important, as weight gain is a common
side effect of sulfonylurea treatment that may be related to a
sulfonylurea-induced increase in insulin concentrations (27).
The present study had two primary strengths and
three major limitations that should be considered when reviewing
the results. Regarding its strengths, the study authors ensured
that only high-quality evidence was examined by limiting the
inclusion of studies to only double-blind RCTs. Furthermore, as the
first systematic review, to the best of our knowledge, to compare
the efficacy and safety of sitagliptin and sulfonylurea therapies
in the treatment of patients with type 2 diabetes mellitus
experiencing inadequate glycemic control with metformin
monotherapy, this study filled an important research gap. Regarding
its limitations, the study examined RCTs that were conducted for
varying lengths of time (range, 12–104 weeks), which may affect the
extent to which the results can be compared. In addition, as the
RCTs did not report economic indicators, the present study was not
able conduct the relevant economic analysis. Such analysis is
important, as cost is a significant consideration in therapeutic
decision making in order to support the allocation of sufficient
healthcare resources for the treatment of type 2 diabetes mellitus
and its complications, particularly in light of its increasing
global prevalence. Finally, as none of the RCTs were designed to
compare the cardiovascular endpoints of the two study groups, any
conclusions regarding outcomes, such as cardiovascular morbidity or
mortality, should be considered with caution and only be accepted
following confirmation by additional investigation by more
RCTs.
In conclusion, the addition of sitagliptin therapy
to the regimen of patients with type 2 diabetes mellitus who are
not achieving their glycemic targets with metformin monotherapy may
result in a reduction in HbA1c values in a manner similar to the
addition of sulfonylurea therapy to metformin monotherapy while
posing a lower risk of hypoglycemia and resulting in a greater loss
of weight.
Acknowledgements
This study was supported by the Department of
Endocrinology and Metabolism, West China Hospital of Sichuan
University, which offered a grant for a literature review.
References
|
1
|
Stulc T and Sedo A: Inhibition of
multifunctional dipeptidyl peptidase-IV: is there a risk of
oncological and immunological adverse effects? Diabetes Res Clin
Pract. 88:125–131. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Choudhury SR, Datta A, Chanda S, et al:
Overview of current and upcoming strategies implied for the therapy
of type 2 diabetes mellitus. Curr Diabetes Rev. 10:275–282. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Eurich DT, McAlister FA, Blackburn DF, et
al: Benefits and harms of antidiabetic agents in patients with
diabetes and heart failure: systematic review. BMJ. 335:4972007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Saenz A, Fernandez-Esteban I, Mataix A, et
al: Metformin monotherapy for type 2 diabetes mellitus. Cochrane
Database Syst Rev. 3:CD0029662005.PubMed/NCBI
|
|
5
|
IDF Clinical Guidelines Task Force. Global
Guideline for Type 2 Diabetes: recommendations for standard,
comprehensive, and minimal care. Diabet Med. 23:579–593. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
National Collaborating Centre for Chronic
Conditions (UK). Type 2 Diabetes: National Clinical Guideline for
Management in Primary and Secondary Care (Update). National
Institute for Health and Clinical Excellence: Guidance. Royal
College of Physicians; London: 2008
|
|
7
|
American Diabetes Association. Standards
of medical care in diabetes - 2009. Diabetes Care. 32(Suppl 1):
S13–S61. 2009. View Article : Google Scholar
|
|
8
|
American Diabetes Association. Standards
of medical care in diabetes - 2010. Diabetes Care. 33(Suppl 1):
S11–S61. 2010. View Article : Google Scholar
|
|
9
|
Nathan DM, Buse JB, Davidson MB, et al;
American Diabetes Association and the European Association for
Study of Diabetes. Medical management of hyperglycemia in type 2
diabetes: a consensus algorithm for the initiation and adjustment
of therapy: a consensus statement of the American Diabetes
Association and the European Association for the Study of Diabetes.
Diabetes Care. 32:193–203. 2009. View Article : Google Scholar :
|
|
10
|
Inzucchi SE: Oral antihyperglycemic
therapy for type 2 diabetes: scientific review. JAMA. 287:360–372.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goldstein BJ, Feinglos MN, Lunceford JK,
et al; Sitagliptin 036 Study Group. Effect of initial combination
therapy with sitagliptin, a dipeptidyl peptidase-4 inhibitor, and
metformin on glycemic control in patients with type 2 diabetes.
Diabetes Care. 30:1979–1987. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Charbonnel B, Karasik A, Liu J, et al;
Sitagliptin Study 020 Group. Efficacy and safety of the dipeptidyl
peptidase-4 inhibitor sitagliptin added to ongoing metformin
therapy in patients with type 2 diabetes inadequately controlled
with metformin alone. Diabetes Care. 29:2638–2643. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Williams-Herman D, Johnson J, Teng R, et
al: Efficacy and safety of initial combination therapy with
sitagliptin and metformin in patients with type 2 diabetes: a
54-week study. Curr Med Res Opin. 25:569–583. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Arechavaleta R, Seck T, Chen Y, et al:
Efficacy and safety of treatment with sitagliptin or glimepiride in
patients with type 2 diabetes inadequately controlled on metformin
monotherapy: a randomized, double-blind, non-inferiority trial.
Diabetes Obes Metab. 13:160–168. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Koren S, Shemesh-Bar L, Tirosh A, et al:
The effect of sitagliptin versus glibenclamide on arterial
stiffness, blood pressure, lipids, and inflammation in type 2
diabetes mellitus patients. Diabetes Technol Ther. 14:561–567.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nauck MA, Meininger G, Sheng D, et al;
Sitagliptin Study 024 Group. Efficacy and safety of the dipeptidyl
peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea,
glipizide, in patients with type 2 diabetes inadequately controlled
on metformin alone: a randomized, double-blind, non-inferiority
trial. Diabetes Obes Metab. 9:194–205. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Seck T, Nauck M, Sheng D, et al;
Sitagliptin Study 024 Group. Safety and efficacy of treatment with
sitagliptin or glipizide in patients with type 2 diabetes
inadequately controlled on metformin: a 2-year study. Int J Clin
Pract. 64:562–576. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Srivastava S, Saxena GN, Keshwani P and
Gupta R: Comparing the efficacy and safety profile of sitagliptin
versus glimepiride in patients of type 2 diabetes mellitus
inadequately controlled with metformin alone. J Assoc Physicians
India. 60:27–30. 2012.PubMed/NCBI
|
|
19
|
Li WH, Lin M and Zhang XJ: Comparison on
adding sitagliptin or glimepiride in poorly controlled overweight
type 2 diabetes with oral metformin. Zhongguo Yi Yuan Yao Xue Za
Zhi. 32:792–794. 2012.(In Chinese).
|
|
20
|
Higgins JPT and Altman DG: Assessing risk
of bias in included studies. Cochrane Handbook for Systematic
Reviews of Interventions. Higgins JPT and Green S: John Wilry &
Sons; Chichester: pp. 187–241. 2008, View Article : Google Scholar
|
|
21
|
DeFronzo RA: Pharmacologic therapy for
type 2 diabetes mellitus. Ann Intern Med. 131:281–303. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Inzucchi SE: Oral antihyperglycemic
therapy for type 2 diabetes: scientific review. JAMA. 287:360–372.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bergman AJ, Stevens C, Zhou Y, et al:
Pharmacokinetic and pharmacodynamic properties of multiple oral
doses of sitagliptin, a dipeptidyl peptidase-IV inhibitor: a
double-blind, randomized, placebo-controlled study in healthy male
volunteers. Clin Ther. 28:55–72. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Herman GA, Stevens C, Van Dyck K, et al:
Pharmacokinetics and pharmacodynamics of sitagliptin, an inhibitor
of dipeptidyl peptidase IV, in healthy subjects: results from two
randomized, double-blind, placebo-controlled studies with single
oral doses. Clin Pharmacol Ther. 78:675–688. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Maedler K, Carr RD, Bosco D, et al:
Sulfonylurea induced beta-cell apoptosis in cultured human islets.
J Clin Endocrinol Metab. 90:501–506. 2005. View Article : Google Scholar
|
|
26
|
Drucker DJ: Enhancing incretin action for
the treatment of type 2 diabetes. Diabetes Care. 26:2929–2940.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Krentz AJ and Bailey CJ: Oral antidiabetic
agents: current role in type 2 diabetes mellitus. Drugs.
65:385–411. 2005. View Article : Google Scholar : PubMed/NCBI
|