Introduction
Although rare, primary synovial sarcoma is one of
the most common variants of pulmonary sarcoma. Primary synovial
sarcoma usually derive from soft tissue, most commonly in young
individuals (1). Diagnosis requires
a tissue sample in the form of a needle or open biopsy. Surgical
resection is the standard primary treatment, and a 5-year distant
metastasis-free survival of >60% may be achievable (2,3).
However, recurrence remains a major problem and is responsible for
treatment failures (4). Clinically,
pulmonary synovial sarcoma may be characterized as an aggressive
tumor; to the best of our knowledge, there has not been a single
report of a long-term follow-up of a patient with pulmonary
synovial sarcoma. The present study describes the case of a patient
with recurrent pulmonary synovial sarcoma, who was effectively
treated with amrubicin (AMR) monotherapy as a third-line
chemotherapy following cisplatin and irinotecan and carboplatin and
etoposide.
Case report
A 68-year-old female was admitted to hospital with a
cough, dyspnea on exertion and a large, right-sided pleural
effusion. The patient was a non-smoking housewife with no history
of asbestos exposure. Thirty-five months prior to this admission,
the patient underwent a left upper lobectomy and mediastinal lymph
node dissection for a mass in the left upper lobe of the lung. The
pathological diagnosis of the resected tumor was small cell lung
cancer (SCLC) due to its weakly positive staining for synaptophysin
and cluster of differentiation (CD) 56. Following the surgery, the
patient received three courses of chemotherapy with cisplatin and
irinotecan; however, local recurrence developed at the left
mediastinum. The patient was therefore referred to the Mito Medical
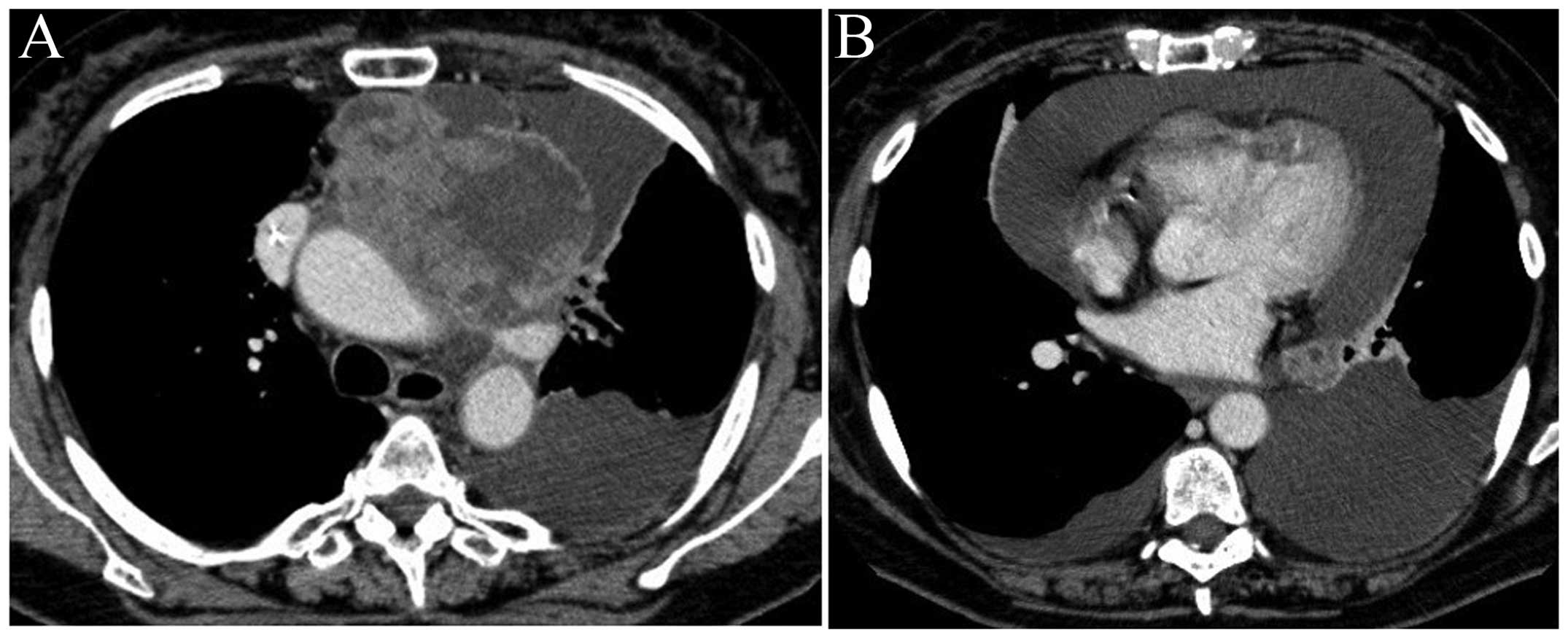
Center (Mito, Japan) to receive further chemotherapy. Chest
computed tomography (CT) revealed a large mass in the left
mediastinum; the mediastinum was shifted to the right and large,
left-sided pericardial and pleural effusions were observed
(Fig. 1). The patient then received
two courses of chemotherapy with carboplatin and etoposide, but the
response was evaluated as a progressive disease, despite severe
myelosuppression (grade 4 thrombocytopenia in the National Cancer
Institute-Common Toxicity Criteria), which required platelet
transfusion. The patient additionally developed cardiac tamponade,
which was successfully treated with tube drainage. Informed consent
was obtained from the patients family.
As a third-line chemotherapy, to avoid severe
myelosuppression, weekly AMR monotherapy was selected:
Administration of 35 mg/m2 AMR three times during a
four-week period (5). Myelotoxicity
could then be evaluated prior to the next AMR administration. A
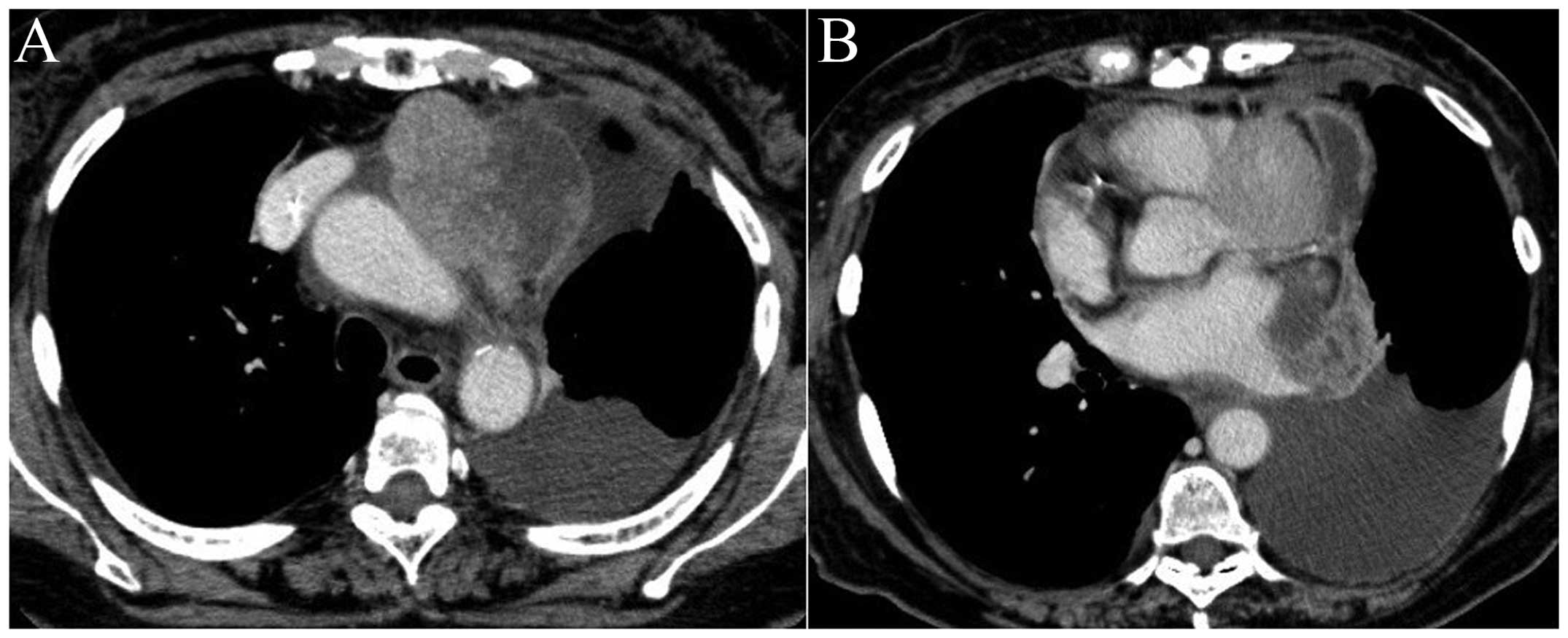
partial response was achieved (Fig.
2) with no severe myelotoxicity. The patient received eight
courses of the chemotherapy and was able to undertake ordinary
daily life at home for 13 months from the initiation of the AMR
chemotherapy. Local recurrence at the left mediastinum then
developed and the patient succumbed of the disease, 50 months after
the initial surgical resection of the tumor.
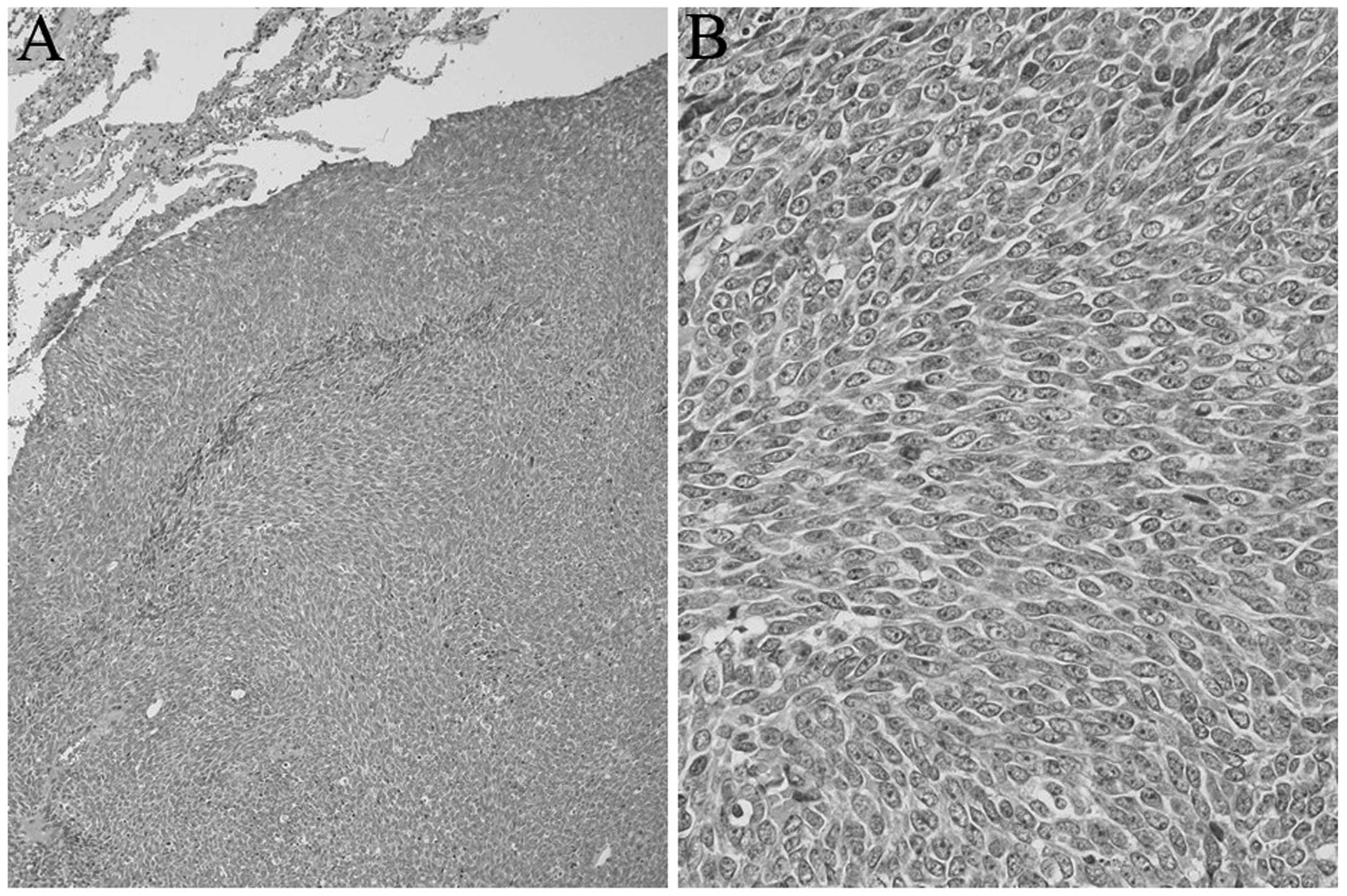
Due to the atypical clinical condition and unusual
response to chemotherapy in this patient, the pathological
examination was repeated. The resected tumor was composed of
spindle cells with increased nuclear chromatin arranged uniformly
(Fig. 3). Immunostaining with
synaptophysin and CD56 revealed negative results. The tumor cells
were positive for vimentin and B-cell lymphoma 2, but negative for
cytokeratin AE1/AE3, α-smooth muscle actin, desmin, S-100, CD34,
chromogranin A and synaptophysin. The SS18 split-signal was
detected in fluorescence in situ hybridization analysis.
From these results, the tumor was diagnosed as a monophasic
synovial sarcoma.
Discussion
Pulmonary synovial sarcoma is a rare, aggressive
primary tumor. The neoplasm was first described in 1995 by Zeren
et al (6) as a distinctive
pulmonary tumor of the lung, sharing histological and
immunohistochemical characteristics with the monophasic synovial
sarcoma of the soft tissue. Chest pain, dyspnea, cough and
hemoptysis are the most common symptoms in patients with pulmonary
synovial sarcoma (7); however,
certain patients do not present with any symptoms (8). Radiologically, pulmonary synovial
sarcoma appears mostly as well-circumscribed nodules of
considerable size (9). In order to
diagnose pulmonary synovial sarcoma, it is mandatory to exclude
extrathoracic primary synovial sarcoma by whole-body survey.
Detection of the t(X;18) chromosomal translocation can confirm the
diagnosis (10,11). In the patient in the present case, no
primary site other than the lung was found and positive
split-signals from an SS18 probe were detected; a diagnosis of
synovial sarcoma was thus confirmed. The patient was misdiagnosed
with SCLC due to weakly positive staining for synaptophysin and
CD56. SCLC is a tumor arising in a relatively large bronchus and
predominantly occurs in patients with a smoking habit. In Japan,
the majority of patients with SCLC have been males with a history
of smoking (12). The present case
was a female patient without a smoking habit. In addition, the
patient had no history of exposure to carcinogenic chemicals such
as asbestos. The poor response to platinum-containing chemotherapy
was also unusual. The SCLC in this patient was therefore somewhat
different from that usually observed. The histopathology of the
resected tumor was re-evaluated and a correct diagnosis was
achieved.
Surgical removal of the resectable tumor is the
choice of treatment for pulmonary synovial sarcoma, and the
prognosis of the disease is poor if the complete surgical resection
cannot be performed. Bacha et al (13) reported that successful complete
resection was significantly associated with increased survival, and
that the size and grade of the tumors were not. As there have been
no randomized control trials, the role of chemotherapy for
unresectable and recurrent tumors remains unclear.
AMR is an anthracycline derivative with a structure
similar to that of doxorubicine (14). Anthracyclines are widely used in the
treatment of a variety of sarcomas (15). Although the cumulative dose-limiting
cardiotoxicity is a major obstacle to its use (16), AMR has shown considerably less
cardiotoxicity than doxorubicin in experimental models (17,18) and
clinical trials (19,20). AMR has been demonstrated to be
effective for previously treated SCLC (21,22). In
the clinical course of the present case, the patient developed
myelotoxicity, which required a platelet transfusion subsequent to
the second course of the second-line chemotherapy with carboplatin
and etoposide. AMR was therefore administered weekly (three times
in four weeks at 35 mg/m2), taking the severe
myelotoxicity of the second-line chemotherapy into
consideration.
To the best of our knowledge, this is the first case
of a patient with pulmonary synovial sarcoma to be effectively
treated with AMR. Following AMR administration, the tumor exhibited
a decrease in size on serial chest CT scan, and the survival
benefit was obtained without any severe myelotoxicity and
cardiotoxicity, although the patient had a history of cardiac
tamponade. The present case could demonstrate a specific
chemosensitivity of such a rare tumor.
References
|
1
|
Siegel HJ, Sessions W, Casillas MA Jr, et
al: Synovial sarcoma: clinicopathologic features, treatment, and
prognosis. Orthopedics. 30:1020–1025. 2007.PubMed/NCBI
|
|
2
|
Liu CY, Yen CC, Chen WM, et al: Soft
tissue sarcoma of extremities: the prognostic significance of
adequate surgical margins in primary operation and reoperation
after recurrence. Ann Surg Oncol. 17:2102–2111. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stojadinovic A, Leung DH, Hoos A, Jaques
DP, Lewis JJ and Brennan MF: Analysis of the prognostic
significance of microscopic margins in 2,084 localized primary
adult soft tissue sarcomas. Ann Surg. 235:424–434. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Morrison BA: Soft tissue sarcomas of the
extremities. Proc (Bayl Univ Med Cent). 16:285–290. 2003.PubMed/NCBI
|
|
5
|
Kitagawa C, Saka H, Kajikawa S, Mori K,
Oki M and Suzuki R: Phase I and pharmacologic study of weekly
amrubicin in patients with refractory or relapsed lung cancer:
Central Japan Lung Study Group (CJLSG) 0601 trial. Cancer Chemother
Pharmacol. 69:1379–1385. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zeren H, Moran CA, Suster S, Fishback NF
and Koss MN: Primary pulmonary sarcomas with features of monophasic
synovial sarcoma: A clinicopathological, immunohistochemical and
ultrastructural study of 25 cases. Hum Pathol. 26:474–480. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hartel PH, Fanburg-Smith JC, Frazier AA,
et al: Primary pulmonary and mediastinal synovial sarcoma: A
clinicopathologic study of 60 cases and comparison with five prior
series. Mod Pathol. 20:760–769. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Watzka SB, Setinek U, Prosch H and Müller
MR: Primary synovial sarcoma of the lung as an incidental finding.
Interact Cardiovasc Thorac Surg. 9:1026–1028. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Frazier AA, Franks TJ, Pugatch RD and
Galvin JR: From the archives of the AFIP: Pleuropulmonary synovial
sarcoma. Radiographics. 26:923–940. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
dos Santos NR, de Bruijn DR and van Kessel
AG: Molecular mechanisms underlying human synovial sarcoma
development. Genes Chromosomes Cancer. 30:1–14. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miura Y, Keira Y, Ogino J, et al:
Detection of specific genetic abnormalities by fluorescence in situ
hybridization in soft tissue tumors. Pathol Int. 62:16–27. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cuffe S, Moua T, Summerfield R, Roberts H,
Jett J and Shepherd FA: Characteristics and outcomes of small cell
lung cancer patients diagnosed during two lung cancer computed
tomographic screening programs in heavy smokers. J Thorac Oncol.
6:818–822. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bacha EA, Wright CD, Grillo HC, et al:
Surgical treatment of primary pulmonary sarcomas. Eur J
Cardiothorac Surg. 15:456–460. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shah CM: Amrubicin: A synthetic
anthracyclin analogue in the treatment of extensive stage small
cell lung cancer. Recent Pat Anticancer Drug Discov. 4:241–245.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Walczak BE and Irwin RB: Sarcoma
chemotherapy. J Am Acad Orthop Surg. 21:480–491. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Weiss RB: The anthracyclines: Will we ever
find a better doxorubicin? Semin Oncol. 19:670–686. 1992.PubMed/NCBI
|
|
17
|
Suzuki T, Minamide S, Iwasaki T, Yamamoto
H and Kanda H: Cardiotoxicity of a new anthracycline derivative
(SM-5887) following intravenous administration to rabbits:
Comparative study with doxorubicin. Invest New Drugs. 15:219–225.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Noda T, Watanabe T, Kohda A, Hosokawa S
and Suzuki T: Chronic effects of a novel synthetic anthracycline
derivative (SM-5887) on normal heart and doxorubicin-induced
cardiomyopathy in beagle dogs. Invest New Drugs. 16:121–128. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fulbright JM, Huh W, Anderson P and
Chandra J: Can anthracycline therapy for pediatric malignancies be
less cardiotoxic? Curr Oncol Rep. 12:411–419. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ogawara D, Fukuda M, Nakamura Y and Kohno
S: Efficacy and safety of amrubicin hydrochloride for treatment of
relapsed small cell lung cancer. Cancer Manag Res. 2:191–195.
2010.PubMed/NCBI
|
|
21
|
Onoda S, Masuda N, Seto T, et al: Thoracic
Oncology Research Group Study 0301: Phase II trial of amrubicin for
treatment of refractory or relapsed small-cell lung cancer:
Thoracic Oncology Research Group Study 0301. J Clin Oncol.
24:5448–5453. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Harada T, Oizumi S, Ito K, et al: Hokkaido
Lung Cancer Clinical Study Group: A phase II study of amrubicin as
a third-line or fourth-line chemotherapy for patients with
non-small cell lung cancer: Hokkaido Lung Cancer Clinical Study
Group Trial (HOT) 0901. Oncologist. 18:439–445. 2013. View Article : Google Scholar : PubMed/NCBI
|