Introduction
Thyroid cancer is the most common malignant tumor of
the endocrine system, accounting for <1% of all carcinomas
(1). Thyroid carcinomas are derived
from two cell types presenting in the thyroid gland. Among them,
papillary and follicular thyroid carcinomas (PTC and FTC), arising
from follicular cells, are also termed as differentiated thyroid
carcinoma (DTC) due to their higher differentiation degree and
iodine-uptake ability. The incidence of thyroid cancer,
particularly PTC, is increasing worldwide (2). PTC is the most common form of thyroid
cancer, accounting for 75–80% of thyroid carcinomas (1) with a 1% mortality rate and almost 5%
recurrence rate (3). PTC has a lower
malignancy rate and better prognosis than other types of thyroid
cancer. It tends to spread through the lymphatic system, and the
percentage of lymph node metastasis to the neck is 50–70% in
patients at the time of diagnosis (3). Distant metastasis, such as in the lung
and bone, is uncommon; however, if it is present, the prognosis is
poor. Iodine-131 (131I) whole-body scanning is very
valuable not only in the diagnosis and positioning of functional
metastatic lesions (4), but also in
the determination of treatment strategies and prognosis assessment
(5).
The present case report describes a patient with PTC
where a benign lesion of the pharynx was misdiagnosed as functional
metastasis. Written informed consent was obtained from the patient
for publication of this case study. The study was approved by the
ethics committee of Tianjin Medical University General Hospital
(Tianjin, China) and adhered to the tenets of the Declaration of
Helsinki.
Case report
A 44-year-old male was admitted to the radionuclide
treatment ward of Tianjin Medical University General Hospital to
accept a third 131I therapy. The patient had suffered
sleep apnea syndrome for >10 years and he had smoked for >20
years, 10 to 20 cigarettes every day. The patient had a remnant
neck mass that had been present for 2 years following a near-total
thyroidectomy with dissection of lateral lymph node compartments
that yielded a 22 mm diameter, non-encapsulated PTC on the left
lobe. Lymph node metastasis was diagnosed in the left side of the
neck one year ago. A preoperative neck computed tomography (CT)
scan revealed thickening of the oropharyngeal soft tissue.
The first therapeutic dose (3.7 GBq) of
131I was administered 2 months following the surgery.
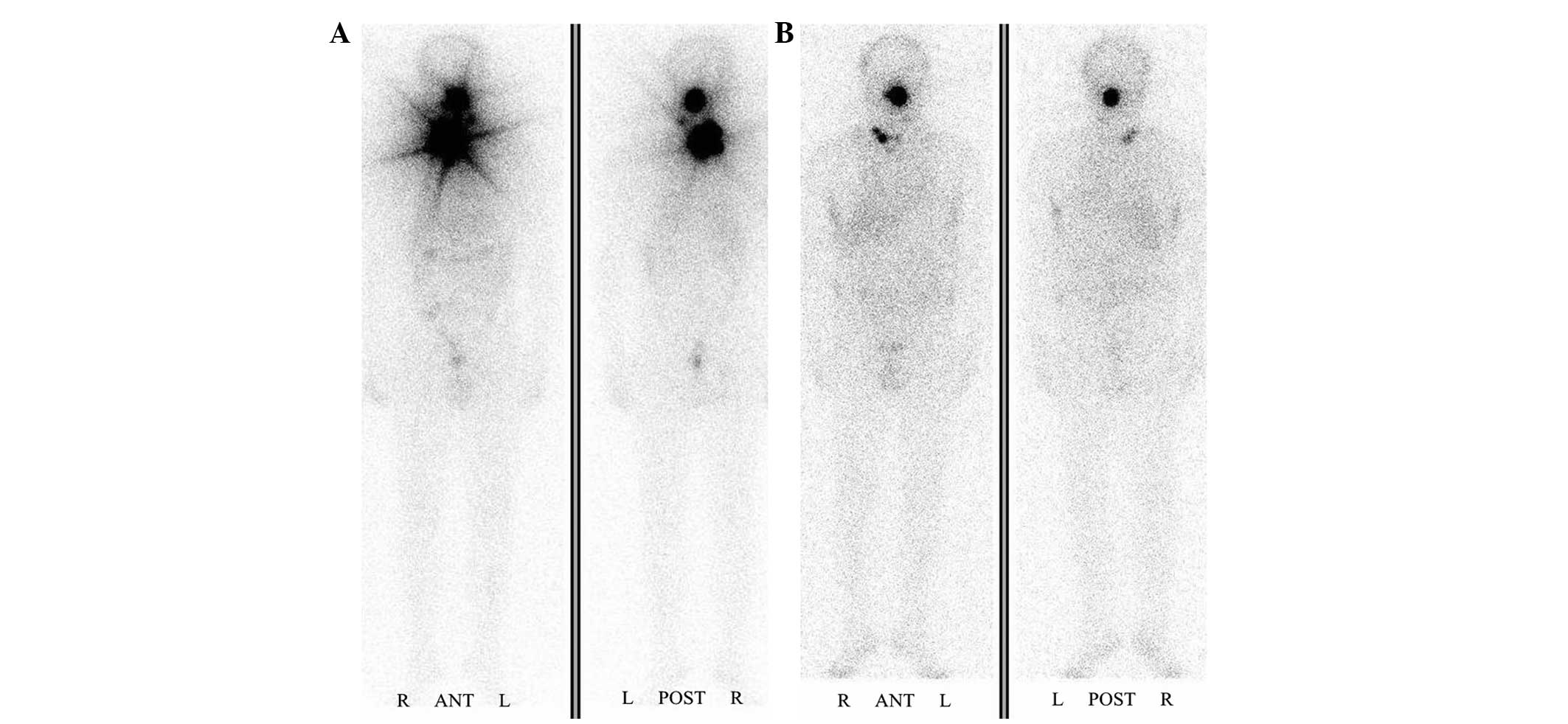
Laboratory findings for the patient are presented in Table I. Whole-body scanning performed with
131I 1 week after administration detected some remnant
thyroid tissue, and an abnormal accumulation of 131I in
the oropharynx and right side of the neck, which could not exclude
the diagnosis of lymph node metastasis (Fig. 1A). Thyroid hormone replacement with
levothyroxine was initiated. The second therapeutic dose (3.7 GBq)
of 131I was administered 4 months later. Scintigraphy
performed 5 days after the second 131I administration
revealed the persistence of 131I accumulation in the
oropharyngeal focus and right lateral neck (Fig. 1B). 131I scanning revealed
that the residual thyroid tissue had almost disappeared, indicating
that the remnant ablation had succeeded; however, quasi-circular
trapping of 131I by the pharynx persisted.
 | Table I.Biological data at each time-point of
therapeutic 131I administration. |
Table I.
Biological data at each time-point of
therapeutic 131I administration.
| Treatment no. | 131I dose
GBq | Free
T3a
(pmol/l) | Free
T4b
(pmol/l) | TSHc (µIU/ml) | Tgd (ng/ml) | TgAbe (IU/ml) |
|---|
| 1 | 3.7 | 3.05 | 7.94 | 45.94 | 6.73 | 23.6 |
| 2 | 3.7 | 2.36 | 6.07 | 50.52 | 6.80 | <20.0 |
| 3 | 3.7 | 2.25 | 6.99 | 56.03 | 4.33 | <20.0 |
The patient stopped using levothyroxine two weeks
prior to admission for the third 131I therapy, and the
blood level of thyroid-stimulating hormone (TSH) was 56.03 µIU/ml.
The levels of thyroglobulin (Tg) and Tg antibody (TgAb) were 4.33
ng/ml and <20.0 IU/ml respectively. The Tg level prior to the
first and second treatments was 6.73 and 6.80 ng/ml, respectively
(Table I). Four months following the
second treatement, the patient agreed to accept a third
131I therapy. The patient was admitted to hospital for
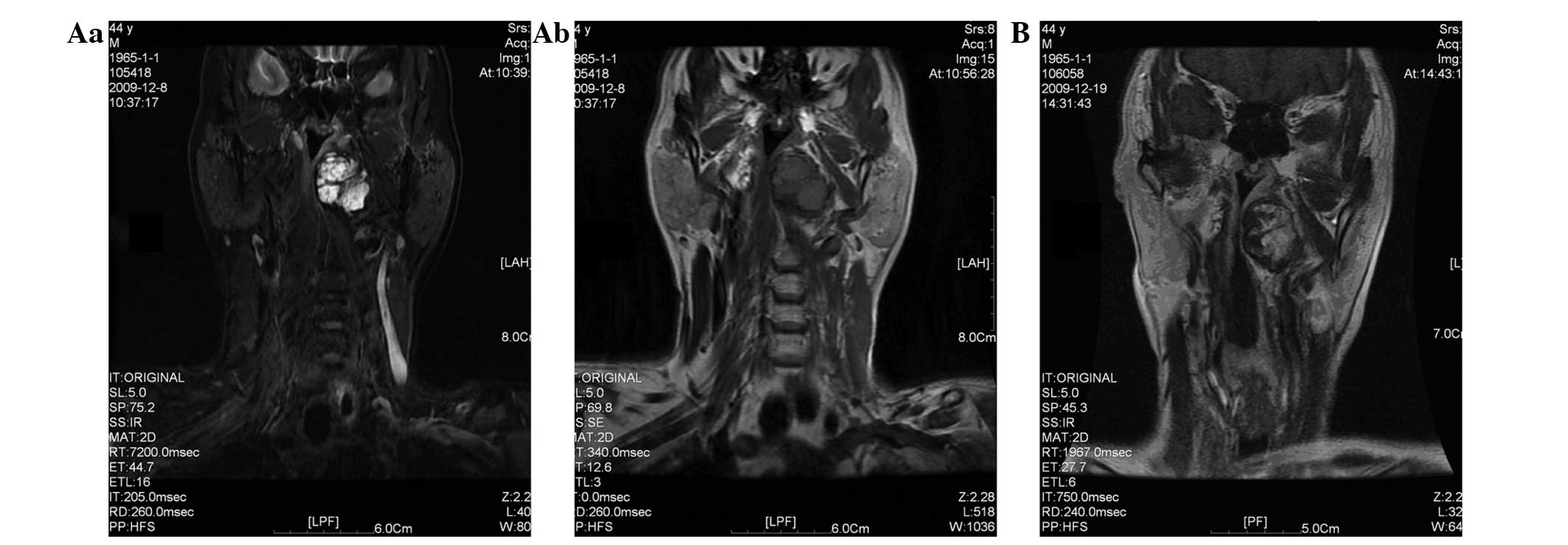
further diagnosis; an examination by magnetic resonance imaging
(MRI) plain and enhanced scanning of the oropharynx was conducted.
The results were as follows: An oval long T1/T2 signal lesion was
observed in the left parapharyngeal space; there were multiple
nodules within the lesion, the size of which was 4.1×3.5×2.2
cm3. The upper border of the lesion was close to the top
of the nasopharynx; the lower boundary was near the bottom of the
oropharyngeal cavity and the outer border was inside the medial
pterygoid. The left sidewall of the nasopharyngeal and
oropharyngeal cavity was compressed and moved to the right. The
nasopharyngeal and oropharyngeal cavity had narrowed. The boundary
between the lesion and the left sidewall of the nasopharyngeal and
oropharyngeal cavity was not clear. MRI enhanced scanning suggested
that the lesion exhibited markedly uneven enhancement on the left
side of the pharynx, and an enhanced nodule and patchy non-enhanced
area were visible inside the lesion (Fig. 2). Following consideration of the
medical history of the patient, the possibility of the lesion being
a metastatic lesion was considered, and indicated that further
examination was necessary. Nasopharyngeal endoscopy revealed that
the nasal septum was deviated, there was a nodular mass at the rear
end of the left septum, the properties of the nasopharyngeal
neoplasm were unclear, and the nasopharyngeal cavity and
nasopharyngeal groove were narrowed, suggesting that a biopsy was
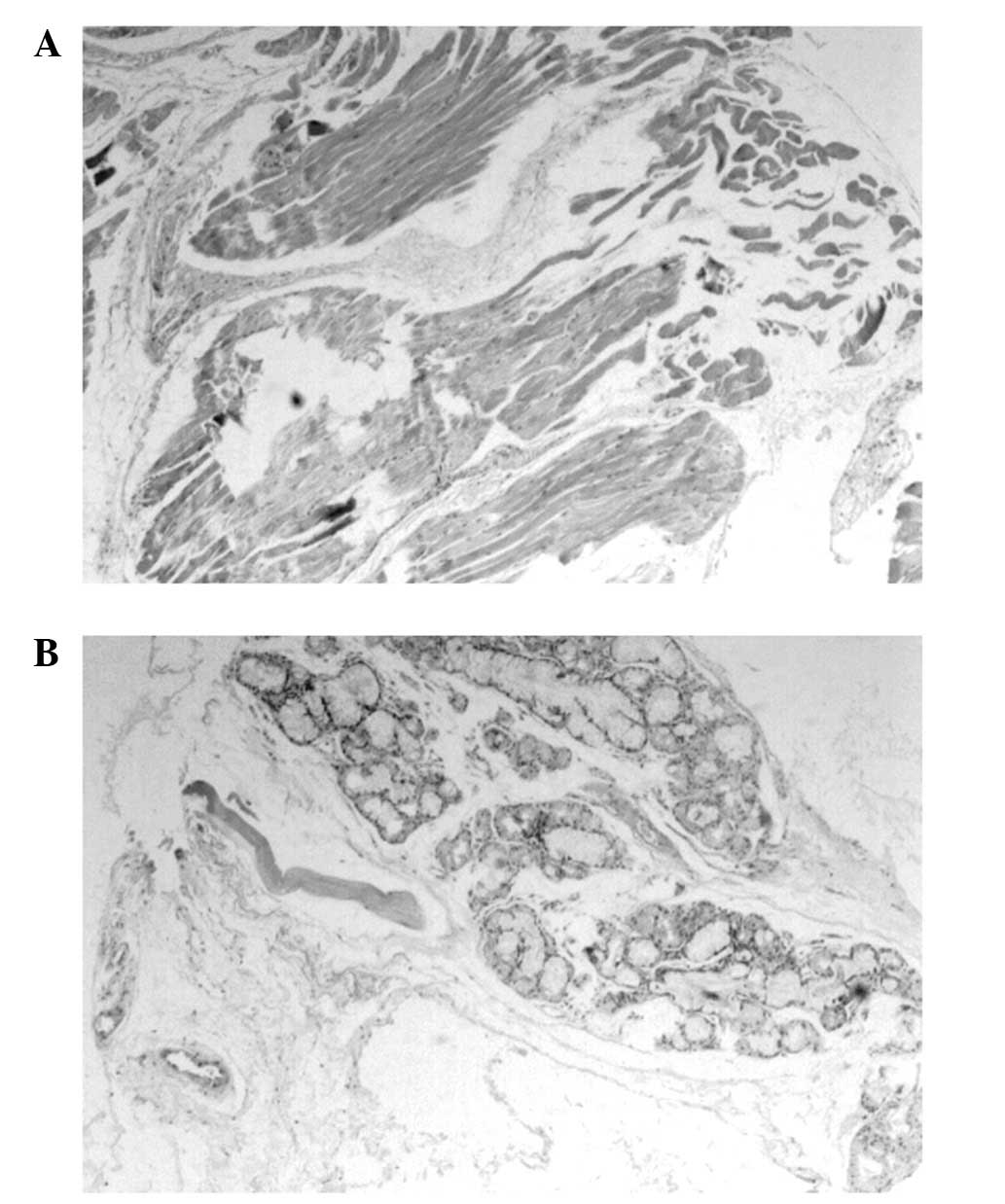
required. A biopsy was then conducted on the left side of the
pharynx under local anesthesia. The pathological examination
revealed that there were a large number of skeletal muscle cells
along with fibrosis in the muscles, salivary gland tissue was found
in the muscle, and the small pieces of mucosal tissue present in
the covering epithelium exhibited chronic inflammation (Fig. 3). When the wound was healed, the
patient was given the third therapeutic dose (3.7 GBq) of
131I. Whole-body scanning with a therapeutic dose of
131I demonstrated that the abnormal accumulation of
131I in the right side of the neck had faded, the
abnormal accumulation in the oropharyngeal cavity had reduced in
size, and the degree of accumulation was unchanged.
Discussion
Total or near-total thyroidectomy, adjuvant
radioactive iodine therapy and TSH suppression therapy with
levothyroxine are recognized as the best comprehensive treatment
protocols for patients with DTC (6).
The treatment of DTC and the diagnosis of its metastases are based
on the capacity of thyroid cells to actively trap radioactive
131I (7). 131I
whole-body scanning is very valuable, not only in the selection of
the treatment strategy and appropriate therapeutic dosage but also
in follow-up visits and for determining recurrence and metastasis
risks effectively (8,9). However, 131I whole-body
scanning may present some false positive results, the reasons being
physiological uptake, pathological accumulation and the retention
of secretions (10).
Two therapeutic doses of 131I were given
to the patient on the second and sixth months after surgery.
Levothyroxine was administered to the patient to suppress the TSH
level regularly between doses. The first of these two whole-body
scans with a therapeutic dose of 131I demonstrated an
abnormal accumulation in the oropharynx, which was considered as a
metastatic lesion. However, the serological test results of the
patient, which showed that the Tg level did not rise, did not
support the diagnosis of progressive disease. Therefore, an MRI
scan of the oropharynx was arranged for this patient in order to
make a definitive diagnosis. The scan revealed a space-occupying
lesion in the left parapharyngeal space, which was unevenly
enhanced in the enhanced MRI scan, and the possibility that the
lesion was a metastatic lesion was considered when the medical
history of the patient with regard to the tumor was considered. The
histopathological examination of the biopsy tissue confirmed that
the abnormal 131I-accumulating mass was benign. The main
reason of this false positive result may be physiological uptake by
the salivary gland tissue present in the lesion. Furthermore, the
pathological accumulation of 131I in the lesion may be
connected with chronic inflammation (11). In addition, a certain degree of
radiation injury took place in the benign mass, with pathological
changes including fibrous connective tissue hyperplasia in skeletal
muscle cells (12), showing that the
lesion presented a certain degree of degeneration.
At present, there is no examination considered as
the gold standard for the diagnosis of the recurrence and
metastasis of DTC. The authors of the present study believe that a
combination of 131I whole-body scanning,
18F-fluorodeoxyglucose positron emission tomography, CT
and MRI is the optimal method for the detection of recurrent and
metastatic disease. It is necessary to analyze the imaging results,
as well as serologic testing outcomes and pathological findings
comprehensively, in order to make the correct diagnosis as early as
possible and to enable patients to be treated properly with
individualized strategies.
References
|
1
|
Cobin RH, Gharib H, Bergman DA, et al:
Thyroid Carcinoma Task Force: AACE/AAES medical/surgical guidelines
for clinical practice: management of thyroid carcinoma. American
Association of Clinical Endocrinologists. American College of
Endocrinology. Endocr Prac. 7:202–220. 2001.
|
|
2
|
Al-Humadi H, Zarrros A, Al-Saigh R and
Liapi C: Genetic basis and gene therapy trials for thyroid cancer.
Cancer Genomics Proteomics. 7:31–49. 2010.PubMed/NCBI
|
|
3
|
Hay ID: Papillary thyroid carcinoma.
Endocrinol Metab Clin North Am. 19:545–576. 1990.PubMed/NCBI
|
|
4
|
Sarkar SD, Kalapparambath TP and Palestro
CJ: Comparison of 123I and 131I for whole-body imaging in thyroid
cancer. J Nucl Med. 5:632–634. 2002.
|
|
5
|
Grewal RK, Tuttle RM, Fox J, et al: The
effect of posttherapy 131I SPECT/CT on risk classification and
management of patients with differentiated thyroid cancer. J Nucl
Med. 9:1361–1367. 2010. View Article : Google Scholar
|
|
6
|
Chinese Society of Endocrinology,
Endocrine Group of Surgery Branch of Chinese Medical Association,
Committee for Head and Neck Oncology of Chinese Anti-cancer
Association, Society of Nuclear Medicine of Chinese Medical
Association, . Clinical guidelines for the diagnosis and management
of thyroid nodules and differentiated thyroid cancer. Zhonghua He
Yi Xue Yu Fen Zi Ying Xiang Za Zhi. 33:96–115. 2013.[In
Chinese].
|
|
7
|
Leger AF, Pellan M, Dagousset F, et al: A
case of stunning of lung and bone metastases of papillary thyroid
cancer after a therapeutic dose (3.7 GBq) of 131I and review of the
literature: implications for sequential treatments. Br J Radiol.
78:428–432. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lind P and Kohlfürst S: Respective roles
of thyroglobulin, radioiodine imaging and positron emission
tomography in the assessment of thyroid cancer. Semin Nucl Med.
36:194–205. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Spanu A, Solinas ME, Chessa F, et al: 131I
SPECT/CT in the follow-up of differentiated thyroid carcinoma:
incremental value versus planar imaging. J Nucl Med. 50:184–190.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mitchell G, Pratt BE, Vini L, et al: False
positive 131I whole body scans in thyroid cancer. Br J Radiol.
73:627–635. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ma C, Kuang A, Xie JW and Ma TK: Possible
explanations for patients with discordant findings of serum
thyroglobulin and 131I whole-body scanning. J Nucl Med.
46:1473–1480. 2005.PubMed/NCBI
|
|
12
|
Mandel L and Liu F: Salivary gland injury
resulting from exposure to radioactive iodine: case reports. J Am
Dent Assoc. 138:1582–1587. 2007. View Article : Google Scholar : PubMed/NCBI
|