Introduction
Cancer, also known as malignant neoplasm, comprises
a group of diseases differing widely in their cause and biology.
Cancer is considered to be one of the major global threats to human
health. The occurrence of chest wall cancer in Asian countries is
higher than that in Western European countries (1). Epidemiological data from China shows
that >2.2 million new cancer cases (1.4 million in males, 0.8
million in females) are diagnosed annually, of which ∼1.6 million
cases result in mortality (2).
Furthermore, cancer has become the number one cause of mortality in
China (3).
Neoplasms of the chest wall comprise a heterogeneous
group of lesions that are challenging to both diagnose and treat.
These neoplasms account for <5% of thoracic malignancies and
exhibit a varied pathology, as they can arise from any soft tissue
or bony structure around the thoracic cavity. Chest wall neoplasms
may be either primary or metastatic, with a malignancy rate of ∼50%
(1), and either symptomatic or
asymptomatic, with ∼20% found incidentally on chest radiograph
(4). Malignant tumors typically
involve direct invasion or metastases from adjacent thoracic tumors
(1). Malignant rib tumors include
multiple myeloma, chondrosarcoma, osteosarcoma and Ewing's sarcoma
(4). These tumors characteristically
manifest as painful, rapidly growing, large, palpable masses.
Osteosarcoma with a less favorable prognosis is more malignant than
chondrosarcoma.
The diagnosis of suspected chest wall tumors
includes a careful history, proper physical examination and a plain
chest X-ray, followed by techniques such as chest radiography,
computed tomography (CT), magnetic resonance imaging (MRI) and
positron emission tomography (1).
Although similar imaging features are characteristic of numerous
malignant chest wall tumors, knowledge of the typical radiological
manifestations of the malignant tumors frequently enables their
differentiation from benign chest wall tumors and may allow a
specific diagnosis to be established. The X-ray pattern of specific
tumors such as Ewing's sarcoma and osteosarcoma, for example, aids
in their diagnosis (5). Despite
this, in the majority of cases the radiographic features alone are
inadequate for the provision of a complete diagnosis and a
histological evaluation is therefore required (4). Furthermore, the selection of one method
over the other is usually dependent on the size of the lesion,
extent of resection, requirement for reconstruction and associated
comorbidities. In general, lesions measuring <5 cm undergo
excisional biopsy and lesions >5 cm may either undergo needle
aspiration or incisional biopsy (4).
In cases of osteosarcoma, rhabdomyosarcoma (RMS), Ewing's sarcoma
and other small-cell sarcomas, chemotherapy is normally suggested
as a neoadjuvant therapy, and then continued postoperatively
depending upon the response of tumor (6). The combined use of chemotherapy and
radiotherapy is contentious but has shown efficacy in adjuvant
protocols (2). In earlier studies,
it was found that patients succumbed due to these life-threatening
tumors (7–9); however, recent advances in diagnostic
and treatment techniques have improved survival rates (4,9). The
present study investigated the diagnosis and treatment of various
chest wall neoplasms with various combinations of chemotherapeutic
protocols, surgical resection and radiotherapy. The aim of this
study was to identify the best possible procedure for chest wall
neoplasms with less potential risk and an increased survival
rate.
Materials and methods
Study design and ethical approval
The present study was carried out as a retrospective
analysis of chest wall tumors diagnosed in the Department of
Cardiopulmonary Surgery of Xiangya Hospital (Changsha, China)
between February 1, 2007 and July 31, 2013. This study was approved
by Ethics Committee of Xiangya Hospital and further necessary
permission from the patients for the conduction of the study was
also obtained.
Patients
A total of 50 patients were observed in this study.
The patients were analyzed on the basis of their gender, age
(children, 4–8 years; young adult, 17–29 years; and adult, 41–50
years), disease symptoms, tumor location and histology/type of
tumor. Of all the patients, 37 (74%) were males and 13 (26%) were
females (Table I). Only primary
tumors of the ribs, scapula, clavicle, sternum and their associated
soft tissues were included. All the patients were diagnosed
according to the updated clinical diagnostic criteria (2) and were further followed-up
postoperatively over a period ranging from 14 months to six
years.
 | Table IClinical characteristics of the
patients grouped into five categories on the basis of the tumor
type. |
Table I
Clinical characteristics of the
patients grouped into five categories on the basis of the tumor
type.
| No. of patients | Age (years)/gender
(M:F) | Diagnosis | Primary site | Metastasis | Chemotherapy | Radiotherapy
(cGy) | Outcome | Follow-up interval
(years) |
|---|
| 14 | 4–50/10:4 | MSRCT | Chest wall and
ribs | 8 bones | D-VAC+IE and Cp in
some patients | 1400–4700 except in
three cases | 9 NED | 1.2–6.0 |
|
|
|
|
| 2 pulmonary |
|
| 5 DOD |
|
|
|
|
|
| 4 none |
|
|
|
|
| 9 | 4–46/7:2 | Alveolar RMS | Clavicle and chest
wall | 4 bones | VAC-I+D, E and Cp in
some patients | 1800–3400 except in
two cases | 7 NED | 1.2–6.0 |
|
|
|
|
| 2 pulmonary |
|
| 2 DOD |
|
|
|
|
|
| 3 none |
|
|
|
|
| 6 | 6–50/5:1 | Embryonal RMS | Chest wall and
ribs | 3 bones | VDC-IE+A in some
patients | 1300–2900 except in
one case | 5 NED | 3.9–6.0 |
|
|
|
|
| 2 pulmonary |
|
| 1 DOD |
|
|
|
|
|
| 1 none |
|
|
|
|
| 9 | 6–50/6:3 | Osteosarcoma | Chest wall and
scapula | 3 bones | I-HDM+L in some
patients | 2500–4000 except in
one case | 6 NED | 1.2–6.0 |
|
|
|
|
| 3 pulmonary |
|
| 3 DOD |
|
|
|
|
|
| 3 none |
|
|
|
|
| 6 | 8–50/4:2 | Synovial
sarcoma | Chest wall | 3 bones | VAC-IE+D in some
patients | 1400–2000 except in
one case | 3 NED | 3–6 |
|
|
|
|
| 1 pulmonary |
|
| 3 DOD |
|
|
|
|
|
| 2 none |
|
|
|
|
| 6 | 17–41/4:2 | Fibrosarcoma | Chest wall | 1 bone | VDC-IE+D and Cp in
some patients | 1400–4800 except in
two cases | 3 NED | 1.2–6.0 |
|
|
|
|
| 3 pulmonary |
|
| 3 DOD |
|
|
|
|
|
| 2 none |
|
|
|
|
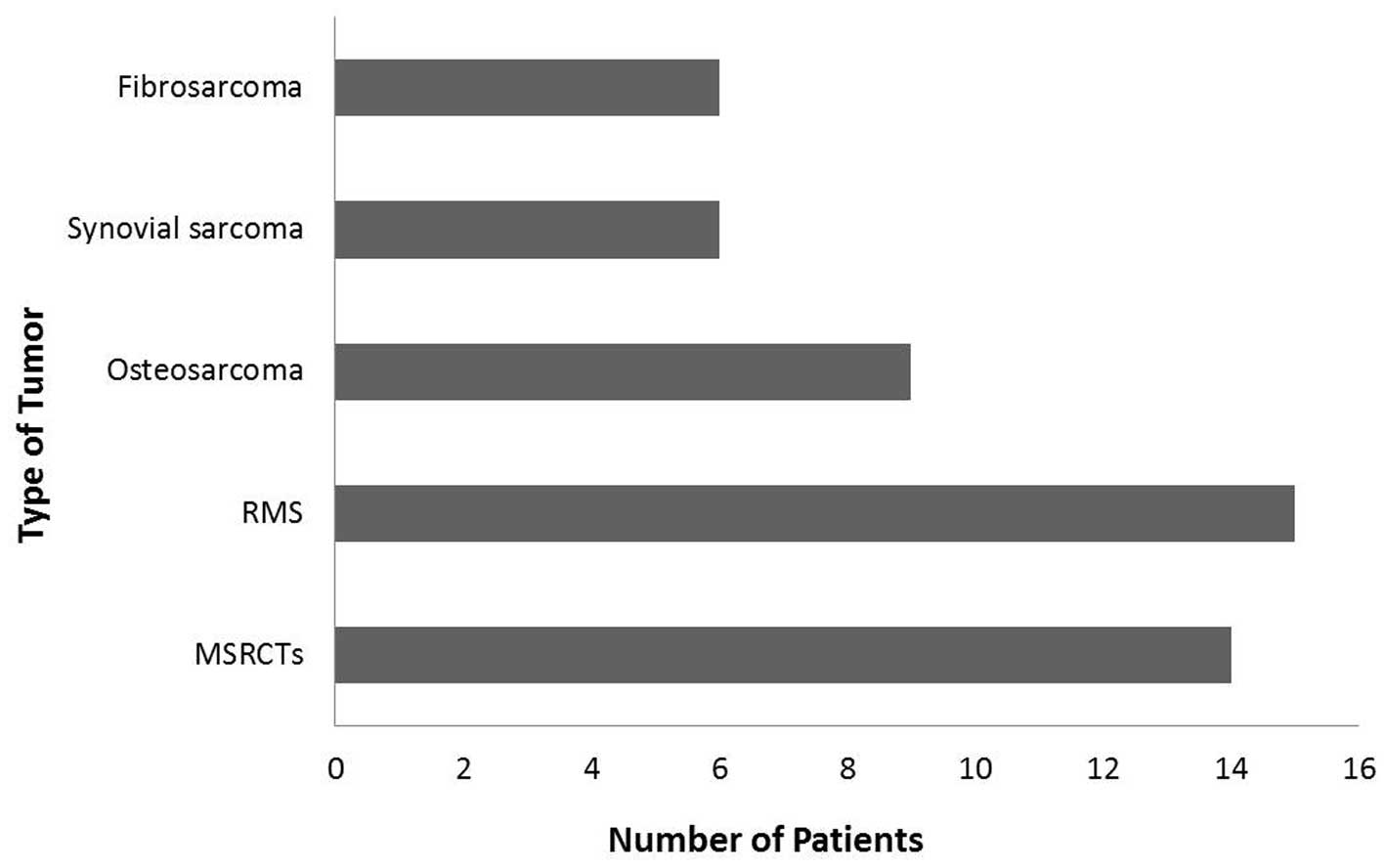
Initial diagnostic techniques, such as CT and MRI,
were carried out on all selected patients. Chest wall CT images
were reviewed by a certified CT radiologist from the Department of
Cardiopulmonary Surgery (Xiangya Hospital). To further extend the
limits of the diagnosis, a four-dimensional scan was carried out to
confirm the different types of chest wall tumors among the
patients. Based on the symptoms and physical observations of the
chest, the patients were grouped into five categories, as shown in
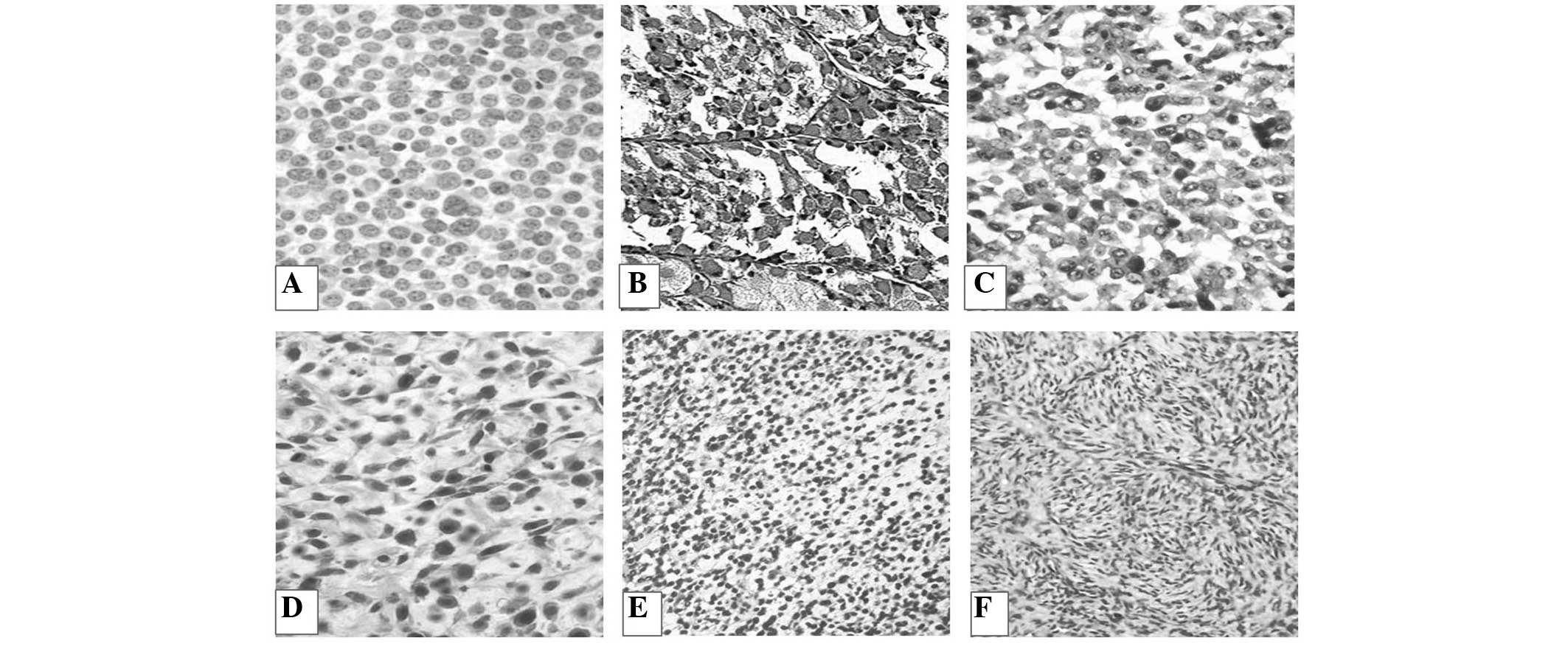
Fig. 1 and Table I. The micrographs of the tumor types
are shown in Fig. 2. The CT/MRI
results revealed that, out of the 50 patients, 14 (28%) showed the
common symptoms of malignant small round cell tumors
(MSRCTs)/Ewing's sarcoma, and these patients were tested with MIC2
marker (10) for confirmation of the
MSRCT diagnosis. Fifteen (30%) patients were diagnosed with RMS,
exhibiting symptoms such as swelling in the body and a persistent
lump in the chest wall, and these diagnoses were further confirmed
by screening tests with myogenin marker (11). Six patients were suffering from
synovial sarcoma, which was confirmed by transduction-like enhancer
gene 1 marker testing (12). Nine
out of the 50 patients were sent for physical examination as they
exhibited visible marks of swelling and redness of various body
parts. A diagnosis of osteosarcoma was confirmed by performing
blood tests with C-X-C chemokine receptor type 4 markers (13). The remaining six patients were
reported to be suffering from fibrosarcoma (Fig. 1 and Table
I).
Clinical evaluation and patient
diagnosis
A biopsy was performed for confirmation according to
previous studies (14,15). A total of 10 out of 50 (20%) patients
were referred for biopsy, out of which seven underwent excisional
biopsy and the three underwent incisional/core biopsy. The detailed
treatment of the patients suffering from the reported chest wall
malignancies is summarized in Table
I.
Surgical methods
The surgical approaches were selected based on the
extent of the tumor. Forty patients were exposed to tumor surgical
resection through a posterior approach based on mild metastasis.
Eleven patients with MSRCTs, 12 with rhabdomyosarcoma, eight with
osteosarcoma, five with synovial sarcoma and four patients with
fibrosarcoma were subjected to resection (Table II).
 | Table IIRepresentative number of patients
subjected to various types of surgical procedures. |
Table II
Representative number of patients
subjected to various types of surgical procedures.
| Surgical
procedure | Number of
patients |
|---|
| Chest wall
resection | 24 |
| En bloc
resection | 11 |
| Biopsy | 10 |
| Distal clavicle
resection | 3 |
| Scapular
resection | 2 |
Radiation therapy
Radiotherapy is usually applied to the cancerous
tumor. A total of 15 out of 40 patients were treated with
image-guided radiation therapy (IGRT) and 20 with brachytherapy.
The remaining five patients underwent intensity-modulated radiation
therapy (IMRT).
Results
Patient data
A total of 50 patients varying in age and gender
were selected for this study of the different types of sarcoma of
the chest wall. The majority of the patients showed a positive
response to the various diagnostic techniques used for their
recovery; however, in certain cases the severity of the disease
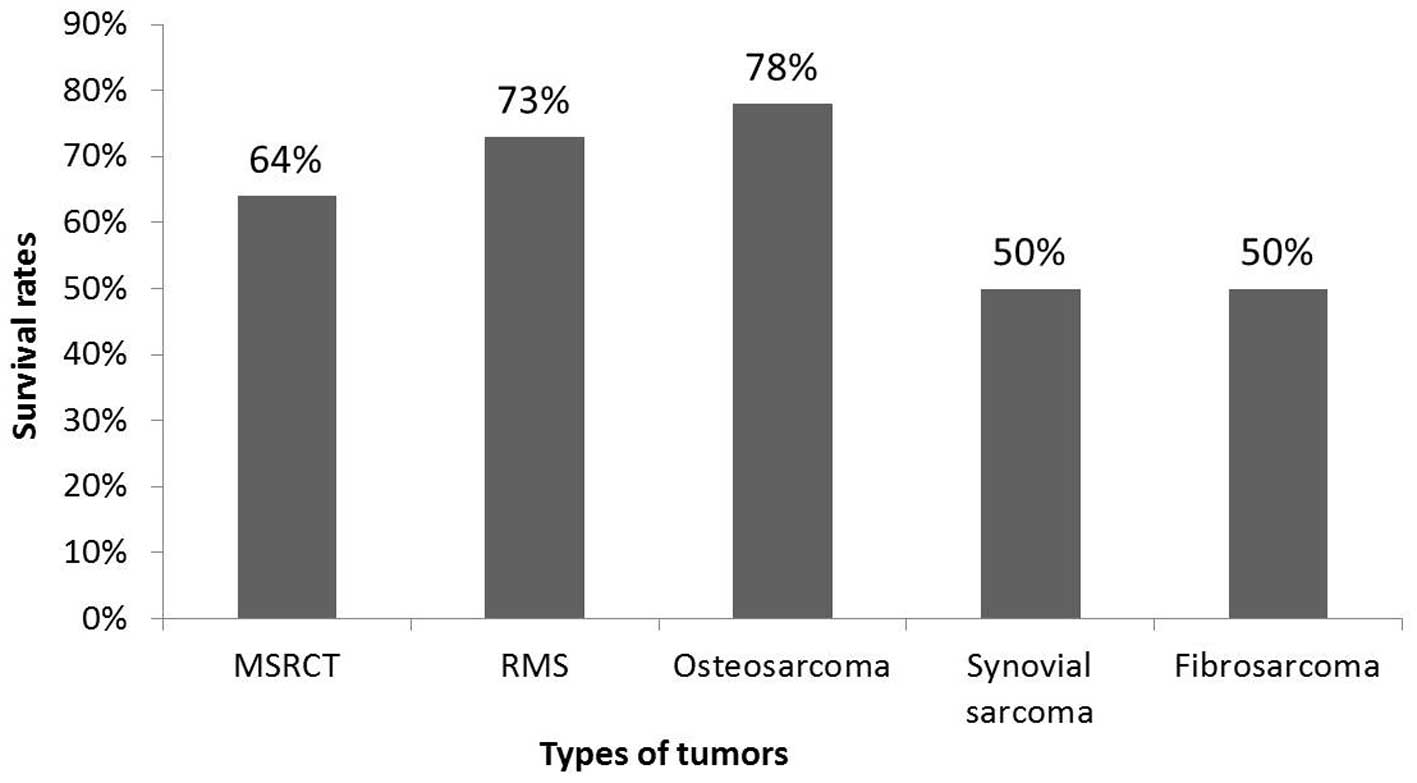
resulted in the mortality of the patient. In general, the survival
rate for each studied chest wall tumor was slightly higher than the
corresponding morbidity rate (Fig.
3). Techniques such as chemotherapy and radiotherapy have been
shown to produce effective results in numerous neoplasms, including
those of the chest wall (6), but in
certain cases in the present study they were unable to increase the
survival rates of the suffering patients to a satisfactory level.
The survival rate of patients suffering from osteosarcoma (78%) was
higher than that of patients with RMS (73%), followed by that of
patients with MSRCT (64%). In the cases of synovial sarcoma and
fibrosarcoma, the survival and mortality rates of the suffering
patients were equal, as shown in Fig.
3. Certain patients from each of the five groups succumbed due
to disease progression, despite being subjected to intensive
regimes of chemotherapy and/or radiotherapy over a period of one to
six years. These patients included five suffering from MSRCT, four
from RMS, two from osteosarcoma and three each from synovial
sarcoma and fibrosarcoma (Table
I).
Complications
Several patients experienced complications following
chemotherapy (30%). Furthermore, infections occurred in eight out
of 14 patients with MSRCT. Additional surgery was therefore
performed for these eight patients. Nine out of the 15 (60%)
patients with RMS experienced side effects, which included nausea,
hair loss and the development of low blood cell counts. The
survival rates with IGRT, IMRT and brachytherapy were found to be
∼5% with a follow-up of six years.
Discussion
Chest wall tumors have long represented a clinical
challenge for surgeons. Incorrect diagnosis, incomplete resection
and unsuccessful reconstruction of large thoracic wall defects have
resulted in high rates of perioperative morbidity and mortality.
The analysis of the prognosis of a large series of patients
following resection has indicated that surgical treatment may be
the best option for primary tumors and for selected secondary
tumors of the chest wall (7).
Furthermore, surgery has been demonstrated to be the most
efficacious curative option for patients with chest wall tumors
(16). Unlike metastatic cases, the
overall five-year survival rates of patients with localized disease
have been enhanced to ∼80% with the combined use of surgery,
radiation therapy and chemotherapy (17).
The blue cell tumor Ewing's sarcoma, one of a group
of cancers collectively known as the Ewing's sarcoma family of
tumors (ESFT), is the third most common malignant chest wall tumor
overall and is not uncommon in the pediatric and young adult
populations. The ESFT constitutes an aggressive tumor family with
high recurrence rates and a high likelihood of metastases (18,19).
RMS, on the other hand, is a relatively rare form of cancer but is
the most common soft tissue sarcoma in children. The tumor usually
manifests as an expanding mass and the treatment constitutes wide
resection followed by radiotherapy and chemotherapy, resulting in a
five-year survival rate of ∼70%. Ewing's sarcoma and RMS arise and
can extend into soft tissue in up to 6.5% (20) and 5% of pediatric patients (21). In the present study, the most
frequent tumor sites were found to be a single rib (48%), followed
by the chest wall (34%), clavicle (12%) and scapula (6%). These
findings were in contrast to previous studies, in which the most
common site of primary tumor occurrence was reported to be the rib
(22,23). Treatment regimens for MSRCTs and RMS
act to control the local disease and distant spread. Shimotake
et al (24) reported that the
local control of MSRCTs could be achieved with radiotherapy,
depending on the location, size and volume of the primary tumor,
whereas Paulino et al (18)
demonstrated that doses of 5,000–6,000 cGy exhibited 80–85%
effectiveness in patients. The majority of the selected patients in
the present study were administered different doses of
radiotherapy, ranging from 1,300 to 4,800 cGy, and the overall
survival rates were ∼65% (Fig. 3 and
Table I).
A previous study on treatment with vincristine,
doxorubicin and cyclophosphamide, along with etoposide and
ifosfamide, showed increased survival rates (14). In the present study, such drugs were
administered to the selected patients in varying concentrations as
per the chemotherapeutic requirement (Table I). The majority of the patients
showed a positive response to the chemotherapeutic doses, with the
exception of a few severe cases, which were later referred for
alternative treatments. The current results were consistent with
those published by Casey et al (25), which concluded that a course regimen
consisting of the short-term, high-dose administration of multiple
selective drugs was optimal for primitive neuroectodermal tumors
and Ewing's sarcoma in children and young adults.
Fibrosarcoma is a tumor of mesenchymal cell origin
that accounts for <10% of soft tissue tumors (26). It occurs more frequently in males,
typically in the lower extremities. The treatment for fibrosarcoma
involves excision, usually combined with radiation therapy
(27). The synovial sarcoma
constitutes ∼10% of soft tissue sarcomas. Treatment for this type
of sarcoma consists of radical or wide excision of the tumor with
adjuvant therapy (chemotherapy and/or radiation therapy) (28). A previous report on fibrosarcoma
revealed unsatisfactory results with chemotherapy, while the
complete removal of the tumor resulted in survival without local
reoccurrence (29). Unni et
al (30) studied the
significance of fibrosarcoma with a low survival rate of 30%. In
the present study, the patients with fibrosarcoma from the selected
population of 50 diseased individuals were subjected to a
combination of chemotherapy and radiotherapy, and exhibited a 50%
survival rate with a follow-up of approximately six years. The same
results were obtained for patients with synovial sarcoma, where the
survival rate was 50% with a follow-up period of three to six years
(Table I). By contrast,
osteosarcoma, a malignant mesenchymal neoplasm that rarely occurs
in the thorax, was treated by a wide resection of the tumor,
including the entire bone, rib, sternum and adjacent soft
tissue.
The present study has shown a favorable survival
rate in patients with chest wall tumors. Regarding radiotherapy, it
is difficult to make any definite recommendations based on the
present data due to the small number of patients; however, the
local control of the disease is fundamental in the treatment
process, as failure to achieve this control can result in the
reappearance of the disease and the possible development of distant
metastases. In the present study, the tumors and all involved
structures were surgically removed through a wide excision, and
chemotherapy was subsequently administered in a regimen similar to
that used prior to surgery. Following chemotherapy, adjuvant
radiotherapy was performed to remove the remaining tumor and
destroy microscopic lymphatic and hematogenous deposits of cancer
spread. In pre-operative planning, the most successful method of
characterizing the type and extent of the tumor is through CT or
MRI techniques. On the basis of our experience, it can be concluded
that planning the most appropriate surgical procedure and
determining pre-operative staging using CT is useful technique and
can facilitate the detection of abnormalities. Chest wall tumors
are a motivating analytic and therapeutic challenge for
reconstructive surgeons, and histopathology reports and
radiographic images should be evaluated prior to surgery. For
numerous patients, a multidisciplinary approach may be most
effective with regard to survival and long-term function. For
patients with malignant and metastatic tumors of the chest wall,
optimal outcomes can be achieved with complete surgical resection
and appropriate reconstruction. Achieving local control of the
disease can be challenging. The present study on a small group of
patients provides a foundation for further studies on tumors of
chest wall, which may, in turn, decrease cancer-based mortality
rates.
Acknowledgements
The authors would like to thank the General Hospital
of Chengdu Military Region of PLA (Chengdu, China) for providing
assistance with the histomorphological studies.
References
|
1
|
D'ddario G, Früh M, Reck M, Baumann P,
Klepetko W and Felip E: Metastatic non-small-cell lung cancer: ESMO
Clinical Practice Guidelines for diagnosis, treatment and
follow-up. Ann Oncol. 21:v116–v119. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ma X, Lin C and Zhen W: Cancer care in
China: A general review. Biomed Imaging Interv J. 4:e392008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
He J, Gu D, Wu X, et al: Major causes of
death among men and women in China. N Engl J Med. 353:1124–1134.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
David EA and Marshall MB: Review of chest
wall tumors: a diagnostic, therapeutic, and reconstructive
challenge. Semin Plast Surg. 25:16–24. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tateishi U, Gladish GW, Kusumoto M, et al:
Chest wall tumors: radiologic findings and pathologic correlation:
part 2. Malignant tumors. Radiographics. 23:1491–1508. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Smith SE and Keshavjee S: Primary chest
wall tumors. Thorac Surg Clin. 20:495–507. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
La Quaglia MP: Chest wall tumors in
childhood and adolescence. Semin Pediatr Surg. 17:173–180. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shah AA and D'Amico TA: Primary chest wall
tumors. J Am Coll Surg. 210:360–366. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim JY and Hofstetter WL: Tumors of the
mediastinum and chest wall. Surg Clin North Am. 90:1019–1040. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ambros IM, Ambros PF, Strehl S, Kovar H,
Gadner H and Salzer-Kuntschik M: MIC2 is a specific marker for
Ewing's sarcoma and peripheral primitive neuroectodermal tumors.
Evidence for a common histogenesis of Ewing's sarcoma and
peripheral primitive neuroectodermal tumors from MIC2 expression
and specific chromosome aberration. Cancer. 67:1886–1893. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kumar S, Perlman E, Harris CA, Raffeld M
and Tsokos M: Myogenin is a specific marker for rhabdomyosarcoma:
an immunohistochemical study in paraffin-embedded tissues. Mod
Pathol. 13:988–993. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Terry J, Saito T, Subramanian S, et al:
TLE1 as a diagnostic immunohistochemical marker for synovial
sarcoma emerging from gene expression profiling studies. Am J Surg
Pathol. 31:240–246. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huang CY, Lee CY, Chen MY, et al: Stromal
cell-derived factor-1/CXCR4 enhanced motility of human osteosarcoma
cells involves MEK1/2, ERK and NF-kappaB-dependent pathways. J Cell
Physiol. 221:204–212. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hsu PK, Lee HC, Hsieh CC, et al:
Management of primary chest wall tumors: 14 years' clinical
experience. J Chin Med Assoc. 69:377–382. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Soyer T, Karnak I, Ciftci AO, Senocak ME,
Tanyel FC and Büyükpamukçu N: The results of surgical treatment of
chest wall tumors in childhood. Pediatr Surg Int. 22:135–139. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tukiainen E: Chest wall reconstruction
after oncological resections. Scand J Surg. 102:9–13. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Punyko JA, Mertens AC, Baker KS, Ness KK,
Robison LL and Gurney JG: Long-term survival probabilities for
childhood rhabdomyosarcoma. Cancer. 103:1475–1483. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Paulino AC, Nguyen TX and Mai WY: An
analysis of primary site control and late effects according to
local control modality in non-metastatic Ewing sarcoma. Pediatr
Blood Cancer. 48:423–429. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van Rossen ME, Verduijn P and Mureau M:
Survival of pedicled pectoralis major flap after secondary myectomy
of muscle pedicle including transection of thoracoacromial vessels:
does the flap remain dependent on its dominant pedicle? J Plast
Reconstr Aesthet Surg. 64:323–328. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chattopadhyay A, Nagendhar Y and Kumar V:
Osteosarcoma of the rib. Indian J Pediatr. 71:543–544. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dang NC, Siegel SE and Phillips JD:
Malignant chest wall tumors in children and young adults. J Pediatr
Surg. 34:1773–1778. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Burt M, Karpeh M, Ukoha O, et al: Medical
tumors of the chest wall. Solitary plasmacytoma and Ewing's
sarcoma. J Thorac Cardiovasc Surg. 105:89–96. 1993.PubMed/NCBI
|
|
23
|
Sabanathan S, Salama FD, Morgan WE and
Harvey JA: Primary chest wall tumors. Ann Thorac Surg. 39:4–15.
1985. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shimotake T, Fumino S, Aoi S, Tsuda T and
Iwai N: Respiratory insufficiency in a newborn with mesenchymal
hamartoma of the chest wall occupying the thoracic cavity. J
Pediatr Surg. 40:E13–E16. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Casey DA, Wexler LH, Merchant MS, et al:
Irinotecan and temozolomide for Ewing sarcoma: The Memorial
Sloan-Kettering experience. Pediatr Blood Cancer. 53:1029–1034.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Radaelli S, Stacchiotti S, Casali PG and
Gronchi A: Emerging therapies for adult soft tissue sarcoma. Expert
Rev Anticancer Ther. 14:689–704. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Folpe AL: Fibrosarcoma: a review and
update. Histopathology. 64:12–25. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Thway K and Fisher C: Synovial sarcoma:
defining features and diagnostic evolution. Ann Diagn Pathol.
18:369–380. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Papagelopoulos PJ, Galanis EC,
Trantafyllidis P, Boscainos PJ, Sim FH and Unni KK:
Clinicopathologic features, diagnosis, and treatment of
fibrosarcoma of bone. Am J Orthop (Belle Mead NJ). 31:253–257.
2002.PubMed/NCBI
|
|
30
|
Unni KK and Inwards CY: Dahlin's Bone
Tumors: General Aspects and Data on 10,165 Cases. Lippincott
Williams & Wilkins; Philadelphia, PA: 2010
|