Introduction
Oxidative stress is defined as a state in which the
production of reactive oxygen species (ROS) overcomes the
endogenous antioxidant defenses of the host, which leads to lipid,
protein and DNA damage. Lipid peroxidation, which is the main
method by which free radicals induce cellular damage, can cause
decreases in membrane fluidity and permeability, and membrane
protein denaturation. Oxidative stress can also lead to DNA damage,
which is associated with chromosome aberrations and micronucleus
formation (1). Micronuclei (MN)
result from chromosomal fragments or lagging chromosomes during
cell division, which are not included in the main nucleus, existing
independently in the cytoplasm. MN are a main biological marker of
chromosomal instability (2).
An association has been proposed between increased
oxidative stress and poor outcomes in the critically ill,
suggesting a potential role for antioxidant strategies in the
intensive care unit (ICU) (3).
Limiting levels of oxidative stress may prevent cellular death,
decrease inflammation and reduce morbidity and mortality rates
(4); therefore, the antioxidant
properties of sedative drugs should be taken into consideration as
an important part of ICU remedy strategies, particularly when
mechanical ventilation is required. Previously, Kang et al
(5) classified the antioxidant
potential of various drugs used in the perioperative period;
however, to the best of our knowledge, a comparison of the effects
on the antioxidant system of dexmedetomidine, propofol and
midazolam, which are most frequently used in the ICU, has yet to be
documented. The aim of the present study, therefore, was to
investigate the antioxidant properties of the three sedative
drugs.
Numerous clinical studies have revealed the
involvement of ROS in severe invasive surgeries, such as
thoracotomy, open-heart surgery and organ transplantation (6–10). In
the present study, a clinical model was designed in which a single
sedative drug was used for anesthesia induction and maintenance to
achieve a definite depth of anesthesia in esophageal cancer radical
prostatectomy. Venous blood samples obtained prior to surgery (T0)
and at 2 h (T1) and 24 h (T2) after surgery were tested to confirm
the levels of ROS generation (superoxide anion, hydrogen peroxide
and hydroxyl radical), the activity of endogenous antioxidant
enzymes [superoxide dismutase (SOD), glutathione peroxidase
(GSH-Px) and catalase (CAT)] and the levels of lipid peroxidation
product [malondialdehyde (MDA)] (11,12). DNA
damage was detected using the cytokinesis-block micronucleus cytome
assay (CBMN) (2).
Materials and methods
Study subjects
The study was approved by the Ethics Committee of
the Affiliated Yixing Hospital of Jiangsu University (Yixing,
China) and written informed consent was obtained from each of the
participants. Forty-nine patients of Society of Anesthesiologists
physical status I-II, who were undergoing esophageal cancer radical
prostatectomy, were randomly divided into three groups: Midazolam
(M group, n=16), propofol (P group, n=16) and dexmedetomidine (D
group, n=17). Patients with liver or renal dysfunction or
hemostatic disorders were excluded. The administration of
antioxidants, including vitamins C and E, edaravone, ebselen,
resveratrol and other Chinese herbs that have been suggested to
possess antioxidant properties, was not permitted during the
perioperative period.
Anesthesia
All patients received 0.5 mg atropine
intramuscularly as premedication 30 min prior to entering the
operating theatre. In the M group, anesthesia induction was
performed through the intravenous injection of midazolam (0.3
mg/kg), fentanyl (5 µg/kg) and vecuronium bromide (0.15 mg/kg), and
maintained by intravenous infusion of midazolam (0.5–1.5 µg/kg/min)
and fentanyl (0.05 µg/kg/min). In the P group, anesthesia was
induced by intravenous injection of propofol (1 mg/kg), fentanyl (5
µg/kg) and vecuronium bromide (0.15 mg/kg), and maintained by
intravenous infusion of propofol (100–200 µg/kg/min) and fentanyl
(0.05 µg/kg/min). In the D group, anesthesia was induced by
intravenous injection of dexmedetomidine (0.5 µg/kg), fentanyl (5
µg/kg) and vecuronium bromide (0.15 mg/kg), and maintained by
intravenous infusion of dexmedetomidine (0.04–0.08 µg/kg/min) and
fentanyl (0.05 µg/kg/min). All patients received tracheal
intubation and underwent mechanical ventilation with 100% oxygen
(tidal volume, 8–10 ml/kg; respiratory frequency, 10–14/min) with
the aim of achieving an end-tidal carbon dioxide level of 38–40
mmHg during the surgical procedure. An extra fentanyl dose (5
µg/kg) was administered to the patients 3 min before the surgery.
The Cerebral State Index (CSI) monitor, an
electroencephalogram-based monitor that has a similar performance
to the Bispectral Index in terms of predicting the clinical state
of the patient assessed by the Observer's Assessment of
Alertness/Sedation scale (9), was
used to monitor the depth of anesthesia during the surgery. The CSI
value was maintained at ∼50 by adjusting the dose of the sedative
drugs. Vasopressors were administered to regulate mean arterial
pressure (MAP) at basal level. The vasoactive agents and
corresponding dose ranges were dopamine (6–30 µg/kg/min) and
nitroglycerin (1–5 µg/kg/min).
Post-operative management
Following surgery, the patients were admitted to the
Post-Anesthesia Care Unit (PACU) for monitoring. In addition to
antimicrobial, expectorant, antacid and nutrition therapy,
intravenous morphine infusion (15–25 µg/kg/h) was used for
postoperative analgesia. The patients were extubated when there was
no indication of bleeding and the patient was observed to be alert,
cardiovascularly stable and normothermic, with an arterial oxygen
tension of >74 mmHg, an inspired oxygen concentration of <40%
and a positive end-expiratory pressure of <5 cmH2O.
Prior to the patients being discharged from the ward, three
criteria had to be met: i) Consciousness; ii) spontaneous breathing
without an endotracheal tube; and iii) stable hemodynamics without
vasoactive drug administration.
Study protocol
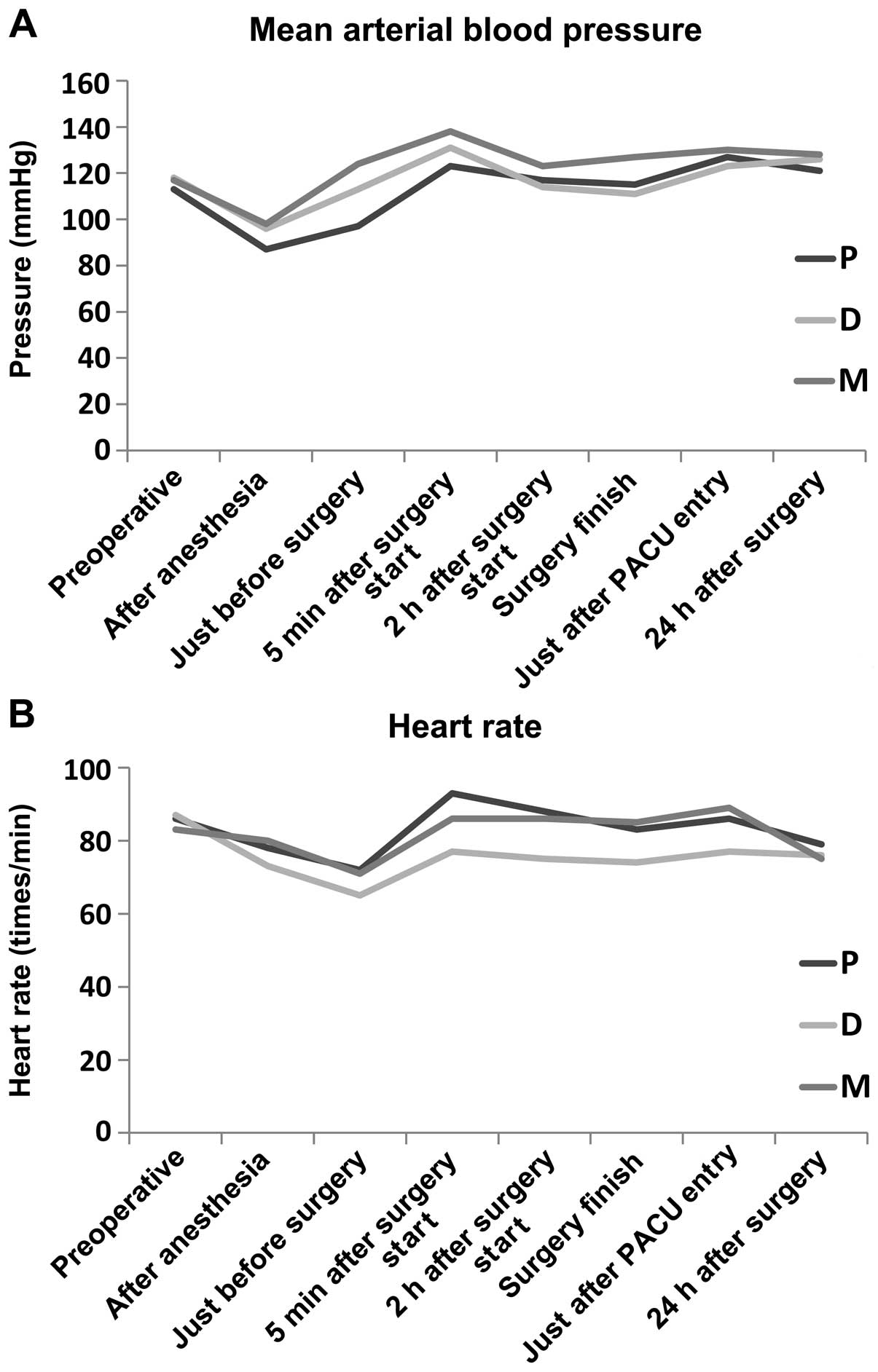
The MAP, heart rate (HR), oxygen saturation and
fluid volume were continuously monitored during the surgical
procedure and in the PACU. The time until recovery of
consciousness, tracheal extubation time and length of PACU stay
were recorded. Venous blood samples were obtained prior to the
surgery (T0) and at 2 h (T1) and 24 h (T2) after the surgery. The
samples were then centrifuged at 1,000 × g for 15 min at room
temperature and the serum samples were stored at −80°C until
analysis.
Biochemical analysis
In this study, oxidative stress indicators were
divided into three categories: Free radical indicators (superoxide
anion, hydrogen peroxide and hydroxyl radical), free radical damage
indicators (MDA) and endogenous antioxidant indicators (SOD, GSH-Px
and CAT). All procedures were performed according to the
instructions provided with the kits from Jiancheng Bioengineering
Research Institute (Nanjing, China): Superoxide anion, A052;
hydrogen peroxide, A064-1; hydroxyl radical, A018; MDA, A003-1;
SOD, A001-1; GSH-Px, A005; and CAT, A007-2.
CBMN
Blood samples were drawn from the subjects. A sample
of whole blood (0.5 ml) was added to 4.5 ml RPMI-1640 culture
medium and phytohemagglutinin, which was required for lymphocyte
stimulation. Cytochalasin B (6 µg/ml; Sigma-Aldrich, St. Louis, MO,
USA) was added after 44 h of culture to block cytokinesis, which
facilitated the identification of lymphocytes that had divided in
culture. As such, cells that had undergone the first mitotic
division were recognized as binucleated cells and were selectively
screened for the presence of MN, nucleoplasmic bridges (NPBs) and
nuclear buds (NBUDs) (7). Cell
harvesting, hypotonic treatment, fixation and slide preparation
were performed following standard procedures. The presence of MN
was scored blindly in 1,000 binucleated cells, in accordance with
standard criteria, and the frequency was expressed as the number of
binucleated cells containing one or more MN/NPBs/NBUDs per 1,000
cells (2).
Statistical analysis
Categorical variables are presented as percentages
and continuous variables are expressed as the mean ± standard
deviation. Differences between variables were analyzed using the
Student's t-test (continuous variables) and the χ2 test
(categorical variables). Data analysis was performed using SPSS for
Windows software version 14.0 (SPSS, Inc., Chicago, IL, USA).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Patient characteristics
The clinical characteristics of the patients are
summarized in Table I. The groups
were similar in terms of age, gender, weight, surgery duration,
blood loss, fluid volume, use of vasoactive agents, dose of
intraoperative fentanyl, dose of postoperative morphine and length
of stay in the PACU; however, the time until consciousness was
recovered and tracheal extubation time in the M group were
significantly longer than the results for the other two groups
(P<0.05). All patients in the perioperative period were in
steady state, and no postoperative complications were observed. The
blood pressure, HR and other vital signs of the patients of the
three groups exhibited no significant differences (P>0.05)
(Fig. 1).
 | Table I.Demographics and clinical
characteristics. |
Table I.
Demographics and clinical
characteristics.
| Characteristic | M group | P group | D group |
|---|
| Age (years) | 70.4±4.9 | 72.3±4.6 | 68.7±5.2 |
| Gender
(male/female) | 12/4 | 12/4 | 12/5 |
| Weight (kg) | 61.17±9.52 | 57.43±7.25 | 59.48±8.83 |
| Surgery duration
(h) | 2.4±0.4 | 2.2±0.3 | 2.1±0.3 |
| Blood loss (ml) | 249±45 | 228±36 | 242±34 |
| Fluid balance in
surgery (ml) | 1,356±74 | 1,418±88 | 1,462±93 |
| Use of vasoactive
agents (n) | 6 | 5 | 5 |
| Intraoperative
fentanyl requirement (mg) | 0.68±0.06 | 0.63±0.04 | 0.67±0.05 |
| Postoperative
morphine requirement (mg) | 64.6±4.7 | 62.3±3.6 | 57.8±3.3 |
| Time until recovery
of consciousness (h) | 2.5±0.8 | 1.2±0.4a | 1.6±0.5a |
| Tracheal extubation
time (h) | 4.6±1.3 | 2.8±1.2a | 3.0±0.9a |
| Length of stay in the
PACU (h) | 43.4±4.7 | 41.7±4.2 | 43.1±5.1 |
Levels of free radical, free radical
damage and endogenous antioxidant indicators
To assess the levels of oxidative stress, free
radical indicators (superoxide anion, hydrogen peroxide and
hydroxyl radical) were detected in the plasma at different
time-points. The results showed that the levels of the three
indicators were increased significantly 2 h after surgery, but then
returned to levels approaching those prior to the surgery.
Furthermore, compared with the M group, the levels of the three
indicators were significantly lower in the P and D groups (Table II).
 | Table II.Levels of superoxide anions, hydroxyl
radicals and hydrogen peroxide. |
Table II.
Levels of superoxide anions, hydroxyl
radicals and hydrogen peroxide.
| Indicator | T0 | T1 | T2 |
|---|
| Superoxide anion
(U/l) |
|
|
|
| M
group |
109.0±24.3 |
180.9±45.7a |
126.7±41.9b |
| P
group |
103.7±20.3 |
144.6±34.2a,c |
117.3±32.3b,c |
| D
group |
112.8±31.1 |
160.2±37.7a,c |
113.0±39.0b,c |
| Hydroxyl radical
(U/ml) |
|
| M
group |
336.5±83.8 |
580.3±91.4a |
379.5±78.3b |
| P
group |
339.7±56.6 |
450.7±82.6a,c |
353.4±82.9b,c |
| D
group |
347.3±84.2 |
419.2±77.2a,c |
363.4±79.1b,c |
| Hydrogen peroxide
(mmol/l) |
|
| M
group |
35.4±9.5 |
78.1±12.8a |
38.1±8.3b |
| P
group |
33.6±8.3 |
58.0±16.1a,c |
36.2±7.9b,c |
| D
group |
35.4±8.1 |
55.3±10.8a,c |
35.7±6.4b,c |
The levels of MDA showed similar trends to the free
radical indicators; however, the level of MDA in the D group was
significantly lower than that in the P group at T2, while the
levels in the P and D groups were both lower than that observed in
the M group (Table III).
 | Table III.Levels of malondialdehyde. |
Table III.
Levels of malondialdehyde.
| Group | T0 | T1 | T2 |
|---|
| M |
5.1±1.0 |
9.5±2.4a |
7.3±1.4b |
| P |
5.2±0.8 |
8.3±0.9a,c |
6.8±1.1b,c |
| D |
5.1±0.9 |
7.9±1.3a,c |
5.3±1.2b,c,d |
With regard to the endogenous antioxidant indicators
(SOD and GSH-Px), the levels at T1 were found to be lower than the
presurgery values in the three groups. Furthermore, the levels of
SOD and GSH-Px were significantly higher in the P and D groups
compared with those in the M group. Notably, the level of CAT did
not exhibit any significant changes among the three groups
(Table IV). In these cases, it was
concluded that more desirable effects were found in the P and D
groups.
 | Table IV.Levels of SOD, GSH-Px and CAT. |
Table IV.
Levels of SOD, GSH-Px and CAT.
| Parameter | T0 | T1 | T2 |
|---|
| SOD (U/ml) |
|
|
|
| M
group |
43.4±7.3 |
31.5±7.3a |
35.3±5.2 |
| P
group |
46.5±7.1 |
39.2±7.5a,c |
45.1±5.7b,c |
| D
group |
47.1±4.7 |
37.9±3.9a,c |
44.4±5.5b,c |
| GSH-Px U |
|
|
|
| M
group |
37.8±8.6 |
19.5±6.0a |
23.5±6.1 |
| P
group |
39.8±9.4 |
27.3±8.9a,c |
33.3±9.6b,c |
| D
group |
38.0±10.5 |
26.1±7.8a,c |
38.1±8.2b,c |
| CAT U/ml |
|
|
|
| M
group |
6.3±1.2 |
5.9±1.1 |
6.3±1.0 |
| P
group |
6.4±1.0 |
6.0±1.3 |
6.2±1.1 |
| D
group |
6.2±0.9 |
6.1±1.2 |
6.2±1.2 |
Chromosomal instability of lymphocytes
in the patients
In order to examine the oxidative damage of the
lymphocytes from the blood samples, the CBMN assay was utilized to
detect the frequencies of MN, NPBs and NBUDs at T0, T1 and T2. It
was found that the micronucleus and NPB frequencies exhibited a
time-dependent effect, with increases at T1 and decreases at T2;
however, no significant differences among the three time-points
were found for the NBUD frequency. It was further noted that the
micronucleus frequency was significantly lower in the P and D
groups than that in the M group at T1 and T2 (Table V). We therefore speculated that
propofol and dexmedetomidine caused less damage than midazolam.
 | Table V.Frequencies of micronuclei,
nucleoplasmic bridges and nuclear buds in 1,000 cells. |
Table V.
Frequencies of micronuclei,
nucleoplasmic bridges and nuclear buds in 1,000 cells.
| Parameter | T0 | T1 | T2 |
|---|
| Micronuclei |
|
|
|
| M
group |
19.3±4.8 |
41.5±6.3a |
30.3±4.2b |
| P
group |
17.0±3.0 |
36.2±4.2a,c |
25.1±3.3b,c |
| D
group |
18.4±4.6 |
35.9±3.3a,c |
24.4±3.2b,c |
| Nucleoplasmic
bridges |
|
|
|
| M
group |
7.3±2.3 |
9.8±2.5a |
7.6±4.3b |
| P
group |
6.8±3.1 |
8.8±2.3a |
6.8±4.0b |
| D
group |
7.9±3.2 |
9.3±2.2a |
7.3±4.2b |
| Nuclear buds |
|
|
|
| M
group |
5.6±2.3 |
6.8±2.5 |
6.2±3.3 |
| P
group |
5.3±3.0 |
6.4±2.8 |
5.8±2.1 |
| D
group |
5.9±2.1 |
6.3±2.7 |
5.9±1.2 |
Discussion
Although a previous in vitro study
demonstrated that the majority of sedative drugs exhibit
antioxidant activity (5), the
application of sedative drugs has, for a long time, been mainly
based on the pharmacology and pharmacokinetic properties of the
drugs, without considering their antioxidant activity and effect on
progress and prognosis. Previous studies on the antioxidant
activity of sedatives are predominantly in vitro
investigations (5) that are lacking
clinical data, resulting in conclusion without cogency. In the
present study, a specific major surgery (esophageal cancer radical
prostatectomy) and standardized remedy strategies were selected as
a clinical model of oxidative stress. Various sedative drugs were
then used in general anesthesia; the changes in the levels of
oxidative stress indicators were detected and the antioxidant
activities of the sedatives were evaluated.
A number of different mechanisms can lead to the
increase in free radical levels caused by surgical trauma:
Mitochondrial DNA damage and cytochrome oxidase system dysfunction;
hypoxanthine conversion to xanthine and xanthine conversion to uric
acid catalyzed by xanthine oxidase; increases in the levels of
cytokines, such as tumor necrosis factor and interleukin-1, during
the surgical procedure and following neutrophil and macrophage
stimulation, causing a respiratory burst; and oxygen-derived free
radicals induced by catecholamine release during the perioperative
period. In the present study, it was found that the levels of free
radical indicators (superoxide anion, hydrogen peroxide and
hydroxyl radical) were markedly increased at 2 h after surgery and
decreased at 24 h after surgery, suggesting that surgery induced
oxidative stress and increased the levels of free radicals. We
therefore speculated that the respiratory burst was the main
mechanism of oxidative stress.
Kang et al (5)
found that midazolam exhibited antioxidant properties, but more
recent studies have demonstrated that the clinical concentration of
midazolam does not have a free radical-scavenging capacity
(13). Previous studies
investigating the effects of sedatives on free radicals have shown
that propofol can not only directly react with free radicals
(14), but also enhance heme
oxygenase expression and generate antioxidant activities (15), as its molecular structure is similar
to that of the endogenous antioxidant vitamin E. Nishina et
al (16) found that the clinical
concentration of dexmedetomidine had no effect on the chemotaxis
and phagocytosis of neutrophils and the production of the
superoxide anion; however, Taniguchi et al (17) suggested that dexmedetomidine could
reduce the inflammatory cell response and inhibit the release of
pro-inflammatory cytokines and the generation of oxygen free
radicals. In the present study it was found that the levels of
superoxide anion, hydrogen peroxide and hydroxyl radical in the P
and D groups were lower 2 h after the surgery than those in the M
group, suggesting that propofol and dexmedetomidine are stronger
radical scavengers.
MDA, which is a product of lipid peroxidation, is
the most commonly used indicator of oxidative stress. Lipid
peroxidation, which is the primary mechanism by which free radicals
induce cellular damage, can cause decreases in membrane fluidity
and permeability, and membrane protein denaturation. Hydroxyl
radicals induce the peroxidation of unsaturated fatty acids and
form a lipid peroxidation chain reaction (18); only when two lipid radicals react to
form a non-radical product or when the radicals are quenched by an
antioxidant molecule, such as α-tocopherol (vitamin E), is the
chain reaction terminated (19).
Propofol can reduce lipid peroxidation due to its similar molecular
structure to vitamin E (20). The
present results also showed that the levels of MDA in the P and D
groups at 2 h after surgery were lower than those in the M group,
demonstrating that propofol and dexmedetomidine can significantly
reduce lipid peroxidation during surgery when compared with
midazolam. At 24 h after surgery, the level of MDA in the D group
was the lowest among the three groups, suggesting that
dexmedetomidine exerts the strongest protection against lipid
peroxidation; however, the mechanism has yet to be elucidated.
Surgical stress can cause a decrease in the
antioxidant enzyme activities of the body (21). A previous study showed that propofol
and dexmedetomidine could enhance the SOD activity of human blood,
with similar effects exhibited by both drugs (22). Another investigation found that
propofol was a more potent enhancer of SOD activity than midazolam
(23). In the present study, the
levels of SOD and GSH-Px in the M group at 2 h after surgery were
markedly lower than those in the P and D groups, suggesting that
surgical trauma would decrease the activities of SOD and GSH-Px and
that propofol and dexmedetomidine could enhance the activities of
the two indicators.
The levels of CAT did not show any differences among
the groups, indicating that surgical trauma and increased free
radical production have few effects on the level of CAT. This may
be a result of GSH-Px replacing the role of CAT in higher
organisms, and particularly in humans (24).
It has previously been shown that the active
metabolites (active oxygen ions, peroxides, free radicals and other
ROS materials) generated by oxidative stress attack the body and
lead to an increase in the micronucleus frequency (25). In the present study, therefore, the
CBMN assay was used to assess the oxidative DNA damage of the
peripheral blood lymphocytes of the patients, and to further to
evaluate the effects of the three sedatives. It was found that the
micronucleus and NPB frequencies were significantly higher at T1
than those at T0, and were lower at T2 than that at T1, showing
that the levels of oxidative DNA damage were higher following
surgery but decreased with time. Furthermore, it was found that the
micronucleus frequencies of the P and D groups at T1 and T2 were
lower than the frequency of the M group, suggesting that propofol
and dexmedetomidine had a superior antioxidant function. Since it
is the NPBs, not the NBUDs, that eventually form MN (25), no significant differences were found
in the frequency of NBUDs.
In conclusion, the administration of propofol or
dexmedetomidine leads to lower levels of oxidative stress and more
desirable effects on the antioxidant system following surgery than
midazolam. Furthermore, dexmedetomidine exerts longer-acting
antioxidant effects than propofol; however, the effects of
sedatives on the antioxidant system, treatment of diseases and
disease outcome require further clinical studies.
Acknowledgements
This study was supported in part by the Medical
Research Project of the Health Department of Jiangsu Province (no.
Z201218) and the Six Talent Peaks Program of Jiangsu Province (no.
WSN-024, 2013).
References
|
1
|
Møller P, Loft S, Lundby C and Olsen NV:
Acute hypoxia and hypoxic exercise induce DNA strand breaks and
oxidative DNA damage in humans. FASEB J. 15:1181–1186. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fenech M: Cytokinesis-block micronucleus
cytome assay. Nat Protoc. 2:1084–1104. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Collier BR, Giladi A, Dossett LA, Dyer L,
Fleming SB and Cotton BA: Impact of high-dose antioxidants on
outcomes in acutely injured patients. JPEN J Parenter Enteral Nutr.
32:384–388. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Christman JW, Blackwell TS and Juurlink
BH: Redox regulation of nuclear factor kappa B: therapeutic
potential for attenuating inflammatory responses. Brain Pathol.
10:153–162. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kang MY, Tsuchiya M, Packer L and Manabe
M: In vitro study on antioxidant potential of various drugs used in
the perioperative period. Acta Anaesthesiol Scand. 42:4–12. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rahman I and MacNee W: Lung glutathione
and oxidative stress: implications in cigarette smoke-induced
airway disease. Am J Physiol. 277:1067–1088. 1999.
|
|
7
|
Rahman I and MacNee W: Role of
transcription factors in inflammatory lung diseases. Thorax.
53:601–612. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Biernacki M, Bigda J, Jankowski K, Wozniak
M and Sledziński Z: Increased serum levels of markers of oxidative
stress during kidney transplantation. Transplant Proc. 34:544–555.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Matata BM and Galiñanes M: Cardiopulmonary
bypass exacerbates oxidative stress but does not increase
proinflammatory cytokine release in patients with diabetes compared
with patients without diabetes: Regulatory effects of exogenous
nitric oxide. J Thorac Cardiovasc Surg. 120:1–11. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tsukioka T, Takemura S, Minamiyama Y, et
al: Local and systemic impacts of pleural oxygen exposure in
thoracotomy. Biofactors. 30:117–128. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sun G, Hu W, Zhang J and Lu Y: The nature
of manganese superoxide dismutase expression in esophageal cancer
cell. Int Med J. 20:711–715. 2013.
|
|
12
|
Sun G, Hu W, Wang Y and Li C: The effect
of MnSOD overexpression and BSO on radiosensitivity in esophageal
cancer cells. Int Med J. 20:567–570. 2013.
|
|
13
|
Hata M, Kobayashi K, Yoshino F, et al:
Direct assessment of the antioxidant properties of midazolam by
electron spin resonance spectroscopy. J Anesth. 25:765–769. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Murphy PG, Myers DS, Davies MJ, Webster NR
and Jones JG: The antioxidant potential of propofol
(2,6-diisopropylphenol). Br J Anaesth. 68:613–618. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Liang C, Cang J, Wang H and Xue Z:
Propofol attenuates cerebral ischemia/reperfusion injury partially
using heme oxygenase-1. J Neurosurg Anesthesiol. 25:311–316. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nishina K, Akamatsu H, Mikawa K, Shiga M,
Maekawa N, Obara H and Niwa Y: The effects of clonidine and
dexmedetomidine on human neutrophil functions. Anesth Analg.
88:452–458. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Taniguchi T, Kurita A, Kobayashi K,
Yamamoto K and Inaba H: Dose- and time-related effects of
dexmedetomidine on mortality and inflammatory responses to
endotoxin-induced shock in rats. J Anesth. 22:221–228. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Thorburne SK and Juurlink BH: Low
glutathione and high iron govern the susceptibility of
oligodendroglial precursors to oxidative stress. J Neurochem.
67:1014–1022. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Halliwell B: Oxygen radicals as key
mediators in neurological disease: Fact or fiction? Ann Neurol.
32:Suppl. S10–S15. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Murphy PG, Bennett JR, Myers DS, Davies MJ
and Jones JG: The effect of propofol anaesthesia on free
radical-induced lipid peroxidation in rat liver microsomes. Eur J
Anaesthesiol. 10:261–266. 1993.PubMed/NCBI
|
|
21
|
Keller GA, Barke R, Harty JT, Humphrey E
and Simmons RL: Decreased hepatic glutathione levels in septic
shock. Predisposition of hepatocytes to oxidative stress: An
experimental approach. Arch Surg. 120:941–945. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dülger H, Kelemençe H, Göktaş U, Şekeroğlu
MR, Katı I, Özcan S and Baran FC: The effects of dexmedetomidine
and propofol on the antioxidant system. Eur J Basic Med Sci.
1:21–27. 2011.
|
|
23
|
Xia WF, Liu Y, Zhou QS, Tang QZ and Zou
HD: Comparison of the effects of propofol and midazolam on
inflammation and oxidase stress in children with congenital heart
disease undergoing cardiac surgery. Yonsei Med J. 52:326–332. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Choi KM, Kang CM, Cho ES, Kang SM, Lee SB
and Um HD: Ionizing radiation-induced micronucleus formation is
mediated by reactive oxygen species that are produced in a manner
dependent on mitochondria, Nox1, and JNK. Oncol Rep. 17:1183–1188.
2007.PubMed/NCBI
|
|
25
|
Rao X, Zhang Y, Yi Q, Hou H, Xu B, Chu L,
et al: Multiple origins of spontaneously arising micronuclei in
HeLa cells: Direct evidence from long-term live cell imaging. Mutat
Res. 646:41–49. 2008. View Article : Google Scholar : PubMed/NCBI
|