Introduction
Hemorrhagic shock remains a leading cause of
potentially preventable morbidity and mortality in severely injured
civilians and military personnel (1,2).
Although the earlier control of life-threatening hemorrhage can
significantly improve patient outcomes, massive transfusion is
still required and is a critical lifesaving treatment for
hemorrhagic shock (3,4). Massive transfusion is commonly defined
as the administration of ≥10 units of packed red blood cells
(pRBCs) to an individual patient or the transfusion of more than
one blood volume in 24 h (5–9). Alternative definitions that may be more
helpful in the acute situation include a 50% blood volume loss
within 3 h or a rate of loss of 150 ml/min (5).
Severe trauma is the most common reason for massive
transfusion. Massive transfusion is also frequently required as a
treatment for severe hemorrhage in patients undergoing complex
surgery. (3) The rapid
identification of patients who may require massive transfusion is
critically important as it may enable the lives of the most
severely injured patients to be saved. A rational blood transfusion
treatment can improve patient outcomes, but unreasonable
transfusion can increase mortality in patients. Therefore,
determining the optimal ratio of fresh frozen plasma (FFP) to pRBCs
is a major step in delivering optimal care. A number of studies
have reported that a high ratio of FFP to pRBCs at an early phase
may reduce the mortality rate of trauma patients (10–16).
It is noteworthy that the effects of FFP to pRBCs
ratios on patient outcomes in China have not yet been clearly
defined. Therefore, the present retrospective study of 20 centers
in China was performed. The purpose of the study was to determine
the optimal ratio of FFP to pRBCs for severely bleeding patients
who received massive transfusions.
Materials and methods
General information
A multicenter, retrospective analysis was performed
at 20 tertiary hospitals in China. The study protocol was approved
by the institutional review boards at all participating
centers.
Massive transfusion
In this study, massive transfusion was defined as
the receipt of ≥10 U of pRBCs in the first 24 h of admission to the
surgical operation or emergency room or the intensive care unit
(ICU).
Study population
The study population included adults (18 years and
older) who presented to 20 tertiary hospitals between January 2009
and December 2010 and received a massive transfusion due to severe
trauma or surgery. The severely bleeding patients undergoing
surgery consisted of cardiac surgery patients, patients undergoing
general surgery (for example, orthopedic, chest, general, urinary
or hepatobiliary surgery or neurosurgery) and obstetric patients.
Patients were excluded if they had suffered severe hemorrhage due
to blood diseases, liver failure or clotting factor defects. To
eliminate the bias of the delay in availability of plasma, all
trauma patients who succumbed within 30 min of arrival to the
emergency room were excluded.
Groups
The massive transfusion patients were stratified
into three groups according to their receipt of low, middle and
high ratios of FFP:pRBCs in 24 and 72 h, specifically at ratios of
<1:2.3, 1:2.3–0.75, and ≥1:0.75. A FFP:pRBC ratio of 1–1.5:1 is
reported to be required in massive transfusion (17), and a FFP:pRBC ratio of 1:1–2 is
capable of correcting coagulopathy in the massive transfusion
(12,17,18).
Therefore, a FFP:pRBC ratio of 1:1–2 is considered routine, and is
included in the middle ratio group; a FFP:pRBC ratio ≥1:0.75 has a
high proportion of plasma and a FFP:pRBC ratio <1:2.3 has a low
proportion of plasma.
Data collection
The data were collected prior to transfusion. All
measurements of respiration, pulse, systolic blood pressure (SBP),
body temperature, red blood cell (RBC) count, hemoglobin (Hb)
concentration, platelet (PLT) count, prothrombin time (PT),
activated partial thromboplastin time (APTT), thrombin time (TT),
international normalized ratio (INR), and fibrinogen (FIB)
concentration were recorded as often as clinically assessed.
A database was created, and detailed information on
patient demographic characteristics and clinical features were
collected, including age, gender, weight, blood products, the time
and date of injury and admission, mechanism of injury, time of
admission to the ICU, time of surgery, and time from admission to
discharge.
Mortality assessment
Dates of mortality were recorded for those that
occurred between study enrollment and on or before day 30 after
hospital admission. Mortality was defined as death in hospital
within 30 days, prior to discharge.
Statistical analysis
Statistical analysis was conducted using SPSS
version 18.0 for Windows (SPSS, Inc., Chicago, IL, USA). EpiData
software, version 3.01 (Epidata Association, Odense, Denmark) was
used for double data entry and data construction. Demographic
characteristics and clinical features are expressed as means with
standard deviations or as absolute numbers. Categorical variables
were analyzed by χ2 tests. Continuous variables with
normal distribution were analyzed by the Shapiro-Wilk test,
Student's t-test or Mann-Whitney U test, as appropriate. To adjust
for other risk factors, logistic regression was used. Results from
logistic regression models are reported as odds ratios (OR) with
95% confidence intervals (CI). Survival rates between patients
receiving different ratios of FFP:pRBCs were estimated by the
Kaplan-Meier method and the curves were analyzed using the log-rank
test. A two-sided P-value <0.05 was considered statistically
significant.
Results
Baseline characteristics of study
subjects
Data were obtained from 1,048 patients who received
a massive transfusion. There were no differences among all groups
in gender, age, causes of massive transfusion, and the majority of
the clinical features. The detailed data of baseline
characteristics and clinical features of the patients are listed in
Tables I and II.
 | Table I.Demographic characteristics and
clinical features based on FFP:pRBC ratio in 24 h. |
Table I.
Demographic characteristics and
clinical features based on FFP:pRBC ratio in 24 h.
|
| Ratio |
|
|---|
|
|
|
|
|---|
| Variable | <1:2.3 | 1: 0.75–2.3 | ≥1:0.75 | P-value |
|---|
| Number of
patients | 186 | 591 | 271 |
|
| Demographics |
|
|
|
|
| Age,
years | 45.8±17.2 | 45.4±16.4 | 43.2±17 | 0.160a |
| Male
gender, n (%) | 123 (19.0) | 364 (56.3) | 159 (24.6) | 0.273b |
| Weight,
kg | 59.4±11.5 | 58.6±11.4 | 57.7±11.3 | 0.365a |
| Causes of massive
transfusion |
|
|
|
|
| Trauma,
n | 31 | 111 | 45 | 0.657b |
| Cardiac
surgery, n | 40 | 144 | 83 | 0.056b |
| General
surgery, n | 107 | 304 | 130 | 0.130b |
| Obstetric
delivery, n | 8 | 32 | 13 | 0.798b |
| Investigations before
transfusion |
|
|
|
|
|
Respiration, n/min | 20.4±3.5 | 20.5±3.5 | 20.4±3.9 | 0.898a |
| Pulse,
n/min | 98.7±90 | 91.7±49.5 | 89.9±21.1 | 0.336a |
| SBP,
mmHg | 119.7±31.5 | 111.9±29.1 | 110±31.2 | 0.014a |
|
Temperature, °C | 36.6±0.9 | 36.6±0.5 | 36.4±0.9 | 0.053a |
| RBC,
x1012/l | 3.9±1 | 3.8±1 | 3.9±1.2 | 0.674a |
| Hb,
g/l | 117.8±33.2 | 116.8±43.5 | 115±34 | 0.660a |
| PLT,
x109/l | 175.1±91.5 | 180.3±95.7 | 171.1±99.9 | 0.304a |
| PT,
sec | 13.4±4.2 | 14.1±6.5 | 14.3±6.6 | 0.327a |
| APTT,
sec | 34.2±20.1 | 35.6±21.6 | 35.3±18.7 | 0.793a |
| TT,
sec | 16.4±5.3 | 17.5±11.1 | 17.6±8.1 | 0.463a |
|
INR | 1.2±0.5 | 1.3±1.8 | 1.2±1 | 0.423a |
| FIB
(g/l) | 16.1±65.5 | 9.5±39.6 | 11.7±46.1 | 0.356a |
| Management |
|
|
|
|
| Length
of hospital stay, days | 27.8±19.2 | 31.3±26.3 | 27.7±21.1 | 0.063a |
| Length
of ICU stay, days | 7.8±14 | 7.7±11 | 11.5±42.1 | 0.478a |
| Surgery
time, h | 3.48±3.7 | 3.85±3.05 | 3.45±3.45 | 0.313a |
| pRBC in
24 h, U | 16 | 19 | 20 | 0.107b |
| FFP in
24 h, U | 14 | 12 | 15 | 0.139b |
| PLT in
24 h, U | 7 | 10 | 4 | 0.803b |
| pRBC in
72 h, U | 16 | 18 | 21 | 0.006b |
| FFP in
72 h, U | 14 | 12 | 14 | 0.256b |
| PLT in
72 h, U | 10 | 10 | 3 | 0.734b |
 | Table II.Demographic characteristics and
clinical features based on FFP:pRBC ratio in 72 h. |
Table II.
Demographic characteristics and
clinical features based on FFP:pRBC ratio in 72 h.
|
| Ratio |
|
|---|
|
|
|
|
|---|
| Variable | <1:2.3 | 1:0.75–2.3 | ≥1:0.75 | P-value |
|---|
| Number of
patients | 154 | 469 | 425 |
|
| Demographics |
|
|
|
|
| Age,
years | 46.1±16.4 | 44.4±16.6 | 45±17.0 | 0.576a |
| Male
gender, n (%) | 100 (15.5) | 269 (41.6) | 277 (42.9) | 0.038b |
| Weight,
kg | 60.2±10.9 | 59.1±10.8 | 57.4±12.0 | 0.030a |
| Causes of massive
transfusion |
|
|
|
|
| Trauma,
n | 28 | 89 | 70 | 0.621b |
| Cardiac
surgery, n | 31 | 98 | 138 |
<0.001b |
| General
surgery, n | 89 | 251 | 201 | 0.046b |
|
Obstetric delivery, n | 6 | 31 | 16 | 0.122b |
| Investigations
before transfusion |
|
|
|
|
|
Respiration, n/min | 20.3±2.5 | 20.6±3.9 | 20.4±3.6 | 0.668a |
| Pulse,
n/min | 95.6±67.8 | 90.7±43.6 | 93.4±59.9 | 0.660a |
| SBP,
mmHg | 122.6±32 | 112.5±27 | 108.8±32.3 |
<0.001a |
|
Temperature, °C | 36.6±0.9 | 36.6±0.5 | 36.5±0.8 | 0.210a |
| RBC,
x1012/l | 3.9±1.0 | 3.8±1.0 | 3.9±1.2 | 0.233a |
| Hb,
g/l | 3.8±1.1 | 120.1±34 | 117.4±50.2 | 0.698a |
| PLT,
x109/l | 179.2±96.1 | 180.9±98.7 | 167.1±100.2 | 0.169a |
| PT,
sec | 13.7±5 | 14.3±5.5 | 14.1±6.5 | 0.653a |
| APTT,
sec | 35.6±23.4 | 35.9±15.3 | 37.2±33.1 | 0.801a |
| TT,
sec | 17±5.8 | 17.3±6.0 | 18.1±8.8 | 0.312a |
|
INR | 1.2±0.6 | 1.3±1.4 | 1.2±0.4 | 0.323a |
| FIB
(g/l) | 12.6±27.1 | 7.4±29.9 | 15.3±67.9 | 0.163a |
| Management |
|
|
|
|
| Length
of hospital stay, days | 29.6±25.9 | 31.1±27.2 | 28.3±18.6 | 0.222a |
| Length
of ICU stay, days | 9.2±14.6 | 7.5±11.7 | 10.2±35.7 | 0.649a |
| Surgery
time, h | 3.7±3.9 | 3.8±4.0 | 3.5±4.0 | 0.508a |
| pRBC in
24 h, U | 16 | 19 | 20 | 0.055b |
| FFP in
24 h, U | 14 | 12 | 15 | 0.567b |
| PLT in
24 h, U | 8 | 10 | 4 | 0.737b |
| pRBC in
72 h, U | 16 | 18 | 21 | 0.006b |
| FFP in
72 h, U | 14 | 12 | 14 | 0.256b |
| PLT in
72 h, U | 10 | 10 | 5 | 0.734b |
Outcomes
The overall mortality rate was 10.31% (108 patients
succumbed, 940 patients survived). Although the mortality rate was
the lowest when patients received a 1:2.3–0.75 ratio of FFP:pRBCs
in 24 h, there were no significant differences among the groups
(Table III). In a 72-h treatment
period, a similar trend was observed; however, the mortality rate
was significantly lower than that in the other groups when patients
received a 1:2.3–0.75 ratio of FFP:pRBCs (Table III).
 | Table III.Mortality rates according to the
FFP:pRBC ratio in 24 and 72 h. |
Table III.
Mortality rates according to the
FFP:pRBC ratio in 24 and 72 h.
|
| Ratio |
|
|---|
|
|
|
|
|---|
| Patient
outcome | Total | <1:2.3 | 1:0.75–2.3 | ≥1:0.75 |
P-valuea |
|---|
| At 24 h, n (%) |
|
|
|
|
|
|
Mortality | 108 (10.31) | 22 (11.83) | 55 (9.31) | 31 (11.44) | 0.477 |
|
Survival | 940 (89.69) | 164 (88.17) | 536 (90.69) | 240 (88.56) |
|
|
Total | 1,048 (100) | 186 (100) | 591 (100) | 271 (100) |
|
| At 72 h, n (%) |
|
|
|
|
|
|
Mortality | 108 (10.31) | 16 (10.39) | 34 (7.25) | 58 (13.65) | 0.007 |
|
Survival | 940 (89.69) | 138 (89.61) | 435 (92.75) | 367 (86.35) |
|
|
Total | 1,048 (100) | 154 (100) | 469 (100) | 425 (100) |
|
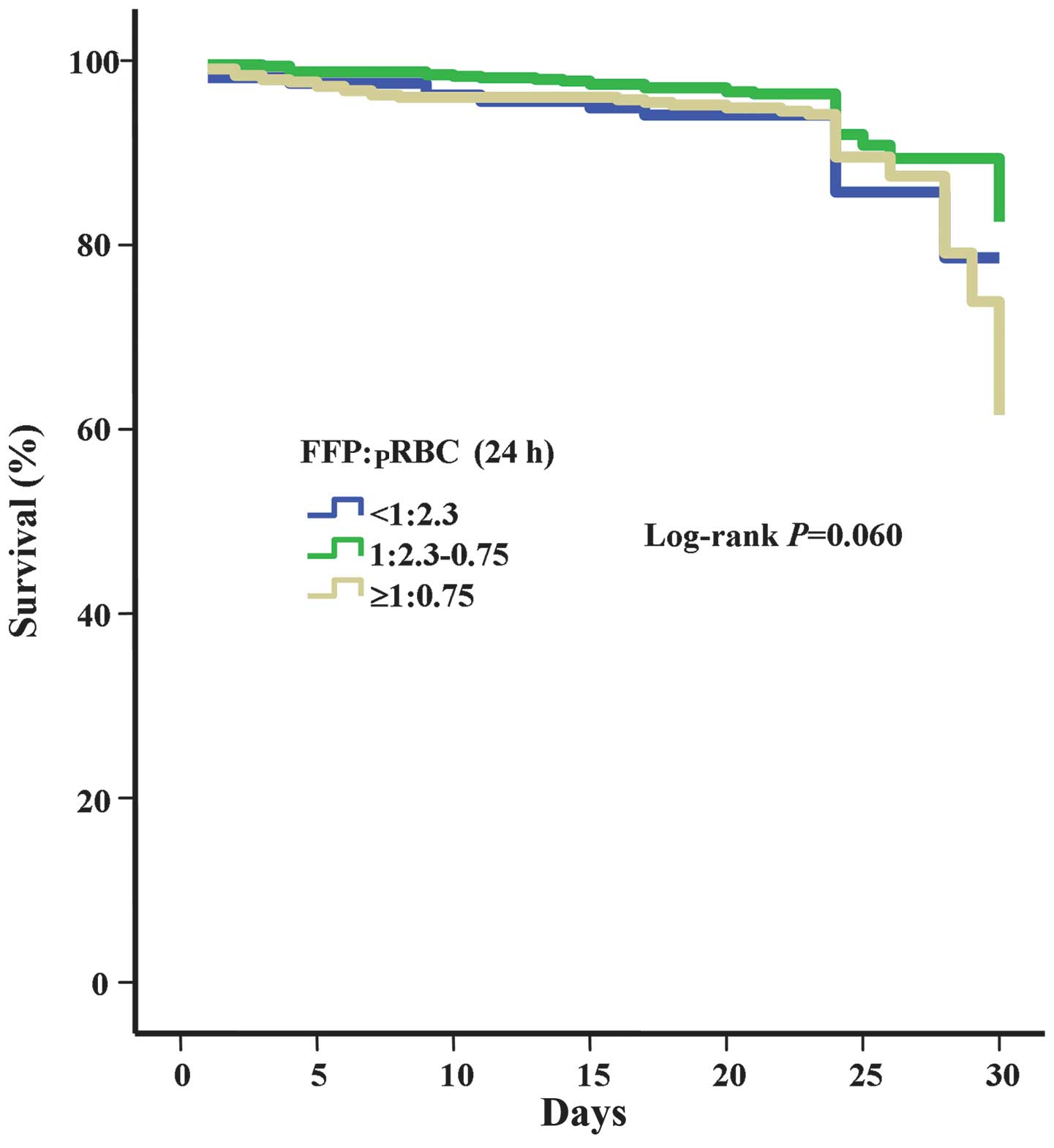
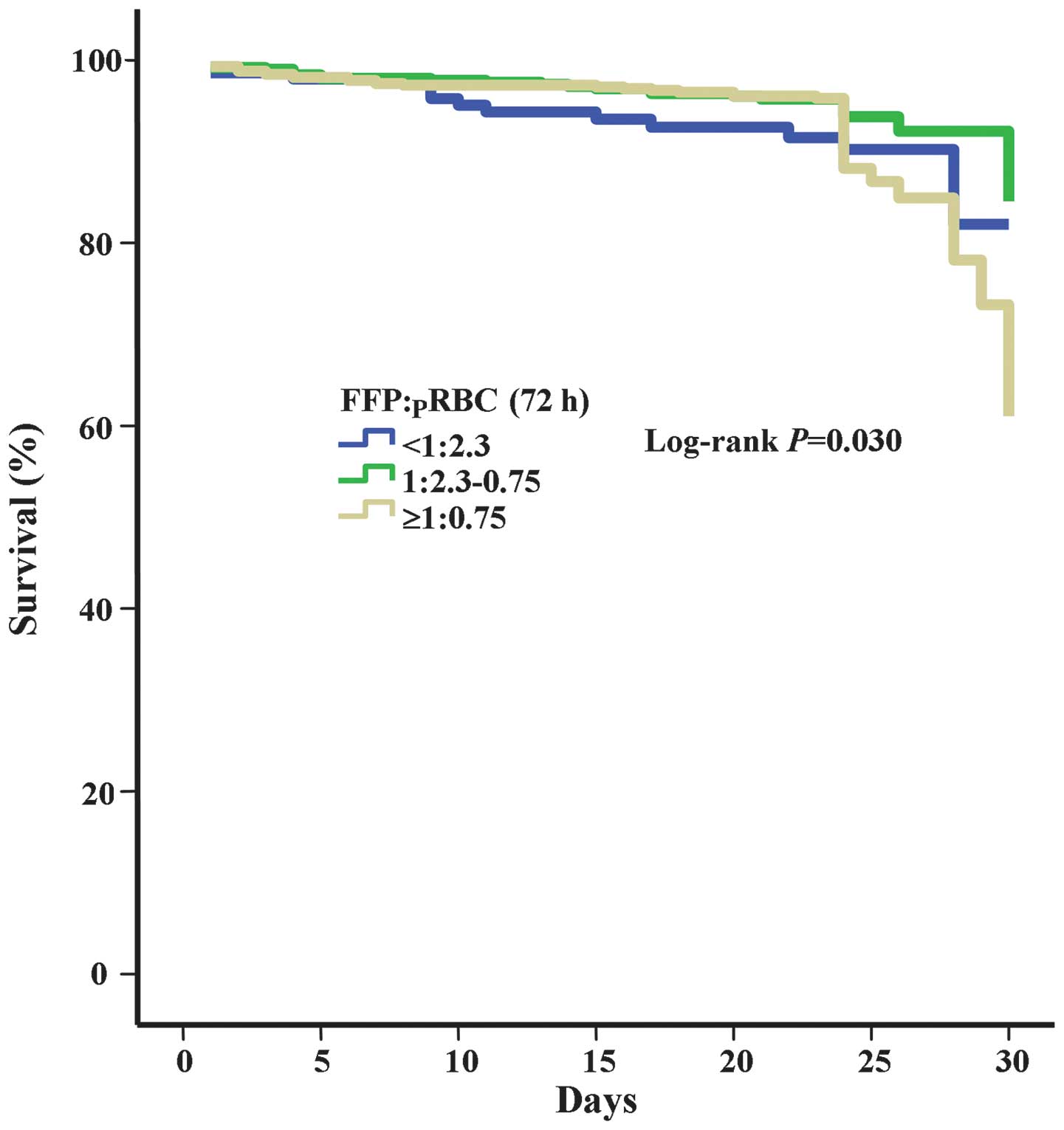
Kaplan-Meier survival analysis with log-rank testing
was performed for calculating the cumulative probability of patient
survival with different ratios of FFP:pRBCs in 24 h and 72 h. The
results revealed no significant differences among the groups with
different ratios of FFP:pRBCs in 24 h (P=0.060; Fig. 1). However, the results highlight the
superiority of a 1:2.3–0.75 ratio of FFP:pRBCs in 72 h with the
highest probability of patient survival (P=0.003; Fig. 2).
Multivariate analysis for control of
confounding variables
A multivariate logistic regression analysis was
further performed for control of confounding variables and to
determine which variables are independent predictors of in-hospital
mortality. Adjustment for the confounding effects of age, gender,
surgery time, weight, primary disease, length of stay, ICU stay,
FFP:pRBC ratio in 24 h and FFP:pRBC ratio in 72 h was conducted.
The results revealed that length of hospital stay (OR=1.113; 95%
CI: 1.056–1.172; P<0.001), ICU stay (OR=0.315; 95% CI:
0.137–0.725; P=0.007) and FFP:pRBC ratio in 72 h (OR=0.349, 95% CI:
0.232–0.523; P<0.001) were significantly and independently
associated with in-hospital mortality (Table IV).
 | Table IV.Multivariate analysis for control of
confounding variables. |
Table IV.
Multivariate analysis for control of
confounding variables.
|
Variablea | β | SE | P-value | Odds ratio | 95% CI |
|---|
| Length of hospital
stay | 0.107 | 0.027 | 0.000 | 1.113 | 1.056–1.172 |
| ICU stay | −1.155 | 0.425 | 0.007 | 0.315 | 0.137–0.725 |
| 72-h ratio of
FFP:pRBC | −1.054 | 0.207 | 0.000 | 0.349 | 0.232–0.523 |
| Constant | 3.518 | 0.75 | 0.000 | 33.734 | 1 |
Discussion
This large multicenter study, to the best of our
knowledge, is the first to reveal the associations between the
ratio of FFP to pRBCs and mortality in patients receiving massive
transfusions in China.
The data showed that, in a total of 1,048 massive
transfusion patients, 108 patients succumbed and 940 patients
survived, corresponding to a mortality rate of 10.31%, which is
lower than that reported by other studies 30–70% (19), 19–45% (11) and 39% (20). One reason may be that the subjects of
the present study included a relatively small proportion of trauma
patients.
Numerous studies have demonstrated a potential
survival benefit from higher ratios of FFP to PRBCs in patients
with trauma-induced coagulopathy requiring massive transfusions
(7,21–26).
Borgman et al (13) reported
that the ratio of blood products transfused affects mortality in
patients receiving massive transfusions following a retrospective
chart review of 246 massive transfusion patients. In the review, it
was found that overall mortality rates in the low (1:8), medium
(1:2.5), and high (1:1.4) plasma to RBC ratio groups were 65, 34
and 19%, respectively. Upon logistic regression, a high 1:1.4
plasma to RBC ratio was found to be independently associated with
improved survival. The authors suggested that massive transfusion
protocols should utilize a 1:1 ratio of FFP to pRBCs for all
patients who are hypocoagulable with traumatic injuries. Murad
et al (16) performed a
meta-analysis and confirmed that a ratio of FFP to pRBCs of >1:3
was associated with reduced mortality in massive transfusion
patients.
In the current study, a retrospective analysis was
performed of 1,048 patients who received ≥10 U of pRBCs in the
first 24 h of admission. The patients were divided into three
groups according to their ratio of FFP to pRBCs, namely the low
(<1:2.3), medium (1:2.3–0.75), and high (≥1:0.75) ratio groups.
It was found that the mortality rate when a ratio of 1:2.3–0.75 was
used was the lowest (9.3%). Above and below this ratio, the
mortality rate was higher, but the difference between groups did
not reach statistical significance.
An analysis of the effect on survival of the ratio
of FFP to pRBCs in massive transfusion patients in the first 72 h
of admission was also performed. The results indicated that the
mortality rate with a 1:2.3–0.75 FFP:pRBC ratio was the lowest
(7.25%); above and below this ratio, the mortality rates were
higher (13.65 and 10.39%, respectively). The mortality rate with a
high FFP level was particularly high. Therefore, a suitable ratio
of FFP to pRBCs (1:2.3–0.75) can improve the survival rate of
patients with massive transfusion in the first 72 h; however,
transfusion with a high FFP content increased mortality. The
findings of the present study were in contrast to those of previous
studies (13,16,27),
which suggested that transfusion with a high FFP transfusion can
improve survival. The factors leading to the divergence require
further study.
Whether the results were influenced by confounding
factors was also investigated. The results of multivariate analysis
demonstrated that length of stay, ICU stay and FFP:pRBC ratio in 72
h were significantly and independently associated with in-hospital
mortality. By contrast, Scalea et al (28) found that the ratio of FFP to pRBCs
was not an independent risk factors for in-hospital mortality.
In conclusion, to the best of our knowledge, this
study is the first retrospective analysis of the effect of the
ratio of FFP to pRBCs on survival in a large multicenter
population. The data demonstrated that the optimal ratio of FFP to
pRBCs was 1:2.3–0.75 in massive transfusion patients in the first
72 h of admission. The optimal ratio of FFP to pRBCs was also found
to be 1:2.3–0.75 in massive transfusion patients in the first 24 h
of admission, but this was not statistically significant.
Transfusion with a high ratio of FFP to pRBCs in 72 h is an
independent risk factor for in-hospital mortality.
Acknowledgements
The authors thank collaborators from the other 19
centers participating in this study: Shi-Jie Mu, Ai-Jun Xia and
Xian-Qin Zhang from Xijing Hospital, the Fourth Military Medical
University (Xi'an, China); Dai-Yu Li from Affiliated Hospital of
Luzhou Medical College (Luzhou, China); Shu-Min Zhao from Xinang
Southwest Hospital, the Third Military Medical University
(Chongqing, China); Wei Jiao from the People's Hospital of Zhuang
Autonomous Region (Nanning, China); Li Tong from First Affiliated
Hospital of Kunming Medical University (Kunming, China); Qing-Bao
Meng from Shenzhen People's Hospital (Shenzhen, China); Jie Li from
the Fourth Clinical Medical College of Hebei Medical University
(Shijiazhuang, China); Shi-Ming Yang from Tangdu Hospital, the
Fourth Military Medical University (Xi'an, China); Suo-Liang Yao
from Xi'an Hong Hui Hospital (Xi'an, China); Bi-Juan Li from
Xiangya Hospital Center of South University (Changsha, China);
Qiu-Shi Wang from Shengjing Hospital of China Medical University
(Chenyang, China); Cui-Ying Li from General Hospital of Chengdu
Military Region (Chengdu, China); Mei-Ning Han from the Second
Affiliated Hospital of Medical College of Xi'an Jiaotong University
(Xi'an, China); Zhi-Xi Hu from Yan'an University Affiliated
Hospital (Yan'an, China); Jin-Shan Jiao from the First Affiliated
Hospital of Shanxi Medical University (Taiyuan, China); Xian-Ping
Lv from the First Affiliated Hospital of Zhengzhou University
(Zhengzhou, China); Yan-Li Bai from Xi'an Central Hospital (Xi'an,
China); Xiao-Xia Shi from Xianyang 215 Hospital (Xianyang, China);
and Fang-Xiang Chen from Daping Hospital, the Third Military
Medical University (Chongqing, China).
References
|
1
|
MacLeod J, Lynn M, McKenney MG, Cohn SM
and Murtha M: Early coagulopathy predicts mortality in trauma. J
Trauma. 55:39–44. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Teixeira PG, Inaba K, Hadjizacharia P, et
al: Preventable or potentially preventable mortality at a mature
trauma center. J Trauma. 63:1338–1346. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sihler KC and Napolitano LM: Massive
transfusion new insights. Chest. 136:1654–1667. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sihler KC and Napolitano LM: Complications
of massive transfusion. Chest. 137:209–220. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Stainsby D, MacLennan S, Thomas D, Isaac J
and Hamilton PJ: Guidelines on the management of massive blood
loss. Br J Haematol. 135:634–641. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hewitt PE and Machin SJ: ABC of
transfusion. Massive blood transfusion. BMJ. 300:107–109. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Malone DL, Hess JR and Fingerhut A:
Massive transfusion practices around the globe and a suggestion for
a common massive transfusion protocol. J Trauma. 60:(6 Suppl).
S91–S96. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kozek-Langenecker S: Management of massive
operative blood loss. Minerva Anestesiol. 73:401–415.
2007.PubMed/NCBI
|
|
9
|
Schuster KM, Davis KA, Lui FY, Maerz LL
and Kaplan LJ: The status of massive transfusion protocols in
United States trauma centers: massive transfusion or massive
confusion? Transfusion. 50:1545–1551. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zink KA, Sambasivan CN, Holcomb JB,
Chisholm G and Schreiber MA: A high ratio of plasma and platelets
to packed red blood cells in the first 6 h of massive transfusion
improves outcomes in a large multicenter study. Am J Surg.
197:565–570. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Riskin DJ, Tsai TC, Riskin L, et al:
Massive transfusion protocols: the role of aggressive resuscitation
versus product ratio in mortality reduction. J Am Coll Surg.
209:198–205. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ho AM, Dion PW, Yeung JH, et al:
Fresh-frozen plasma transfusion strategy in trauma with massive and
ongoing bleeding. Common (sense) and sensibility. Resuscitation.
81:1079–1081. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Borgman MA, Spinella PC, Perkins JG, et
al: The ratio of blood products transfused affects mortality in
patients receiving massive transfusions at a combat support
hospital. J Trauma. 63:805–813. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Stansbury LG, Dutton RP, Stein DM, et al:
Controversy in trauma resuscitation: do ratios of plasma to red
blood cells matter? Transfus Med Rev. 23:255–265. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Peiniger S, Nienaber U, Lefering R, et al:
Balanced massive transfusion ratios in multiple injury patients
with traumatic brain injury. Crit Care. 15:R682011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Murad MH, Stubbs JR, Gandhi MJ, et al: The
effect of plasma transfusion on morbidity and mortality: a
systematic review and meta-analysis. Transfusion. 50:1370–1383.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ho AM, Dion PW, Cheng CA, et al: A
mathematical model for fresh frozen plasma transfusion strategies
during major trauma resuscitation with ongoing hemorrhage. Can J
Surg. 48:470–478. 2005.PubMed/NCBI
|
|
18
|
Yoon S, Park AJ and Kim HO: Clinical
observation study of massive blood transfusion in a tertiary care
hospital in Korea. Yonsei Med J. 52:469–475. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cinat ME, Wallace WC, Nastanski F, et al:
Improved survival following massive transfusion in patients who
have undergone trauma. Arch Surg. 134:964–968. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Como JJ, Dutton RP, Scalea TM, Edelman BB
and Hess JR: Blood transfusion rates in the care of acute trauma.
Transfusion. 44:809–813. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hirshberg A, Dugas M, Banez EI, et al:
Minimizing dilutional coagulopathy in exsanguinating hemorrhage: a
computer simulation. J Trauma. 54:454–463. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Johansson PI and Stensballe J: Effect of
haemostatic control resuscitation on mortality in massively
bleeding patients: a before and after study. Vox Sang. 96:111–118.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duchesne JC, Hunt JP, Wahl G, et al:
Review of current blood transfusions strategies in a mature level I
trauma center: were we wrong for the last 60 years? J Trauma.
65:272–276. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jansen JO, Thomas R, Loudon MA and Brooks
A: Damage control resuscitation for patients with major trauma.
BMJ. 338:b17782009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Holcomb JB, Wade CE, Michalek JE, et al:
Increased plasma and platelet to red blood cell ratios improves
outcome in 466 massively transfused civilian trauma patients. Ann
Surg. 248:447–458. 2008.PubMed/NCBI
|
|
26
|
Kor DJ, Stubbs JR and Gajic O:
Perioperative coagulation management-fresh frozen plasma. Best
Pract Res Clin Anaesthesiol. 24:51–64. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Spinella PC, Perkins JG, Grathwohl KW, et
al: Effect of plasma and red blood cell transfusions on survival in
patients with combat related traumatic injuries. J Trauma. 64:(2
Suppl). S69–S78. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Scalea TM, Bochicchio KM, Lumpkins K, et
al: Early aggressive use of fresh frozen plasma not improve outcome
in critically injured trauma patients. Ann Surg. 248:578–584.
2008.PubMed/NCBI
|