Introduction
Previous decades have heralded the advancement of
cell-based therapy and associated tissue regeneration and wound
repair (1). The use of epithelial
cells in tissue restoration and wound healing has attracted
considerable interest. As such, the number of studies that seek to
employ epithelial cells with high therapeutic potential to create
novel therapies that can target and ultimately restore tissue
integrity has been increasing (2–4). Chronic
cutaneous wounds are one of the most unfavorable pathophysiological
processes in dermatologic surgery; however, they may be treated
using cell-based therapy development (5).
Cutaneous wound healing is a series of processes
involving the epithelial, dermal and mesenchymal tissues, blood
vessels, nerves and immune cells that act within a complex network
of signals (6) to necessitate wound
healing (7,8). Re-establishing epithelial integrity is
essential and the primary step to maintaining a regenerative
response. The scalp has been identified as an excellent donor site
for thin skin grafts (9); however,
the scalp dermal graft presents a limited surface area and is
<3–4% of the total body surface area (10). Clinical and histological evidence has
shown that the rapid healing of the scalp dermal graft is
attributed to the differential potential of the cells in the hair
follicles, and that re-epithelialization can also occur from
grafted hair follicles (11).
Numerous types of cells with multiple differentiation potentials
have been identified in hair follicles, and their relative
contribution to re-epithelialization has been recently determined
(12). Considering the abundance of
evidence suggesting the crucial role of hair follicles as
re-epithelialization promoters, the notion of grafting hair
follicle units harvested from the scalp into chronic cutaneous
wounds was considered in the present study.
The primary aim of the present study was to develop
an effective protocol for the treatment of chronic cutaneous
wounds. The efficacy of the novel therapy that utilized hair
follicle units to promote wound healing was investigated, in
addition to the feasibility and potential healing capabilities of
the hair follicle units that were transplanted into the chronic
cutaneous wound bed. The transplanted hair follicle units were
hypothesized to activate progenitor cells and promote
re-epithelialization in the wound.
Subjects and methods
Patients
In this retrospective case series study, 14 patients
with chronic cutaneous wounds, hospitalized at the Department of
Plastic Surgery of Zhongshan Hospital (Shanghai, China) between
June 2006 and September 2008, were recruited. All patients had
previously received an autologous split-thickness skin graft;
however, partial or completed necrosis had occurred and the graft
was unable to heal independently. Eligible patients had chronic
wounds that had persisted for ≥6 weeks, were non-responsive to
conventional treatment, with signs of delayed healing, and had a
wound area of ≥5 cm2. Patients with alopecia,
coagulopathy and other contraindications of the hair transplant
technique, as well as elderly patients (>80 years), were
excluded from the study. The study was conducted in accordance with
the Declaration of Helsinki and with approval from the Ethics
Committee of the Zhongshan Hospital of Fudan University. Written
informed consent was obtained from all the participants.
Surgical procedures
Debridement of necrotic tissue was preoperatively
performed on all the wounds. In all the patients, the donor area of
the scalp was shaved. Following the application of adrenalized
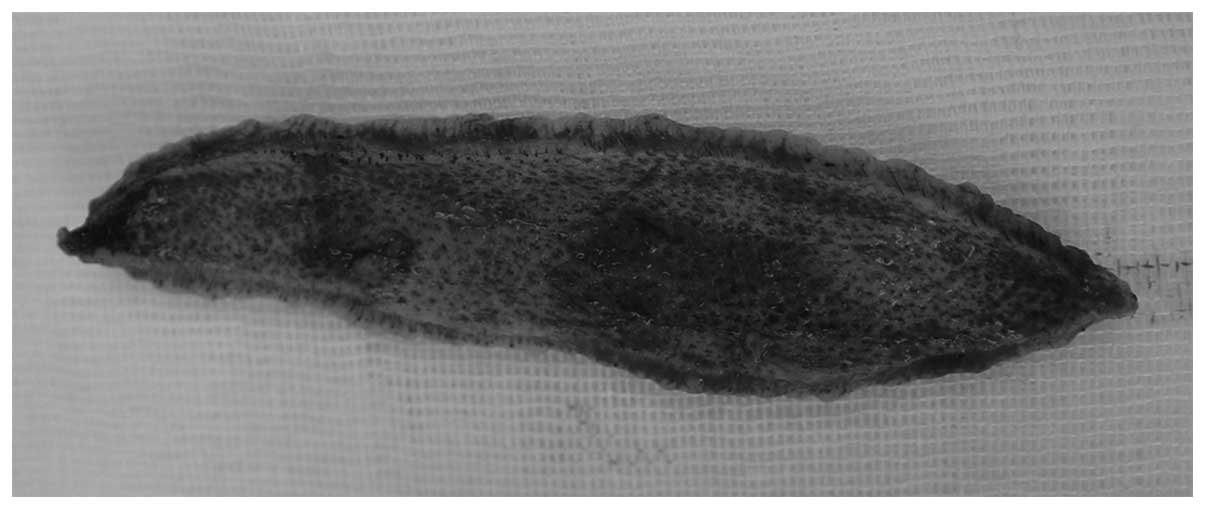
saline into the occipital area of the scalp, a 6.0×1.5 cm scalp
graft was harvested (Fig. 1). The
hair follicle units were dissected from the graft (Fig. 2), and the units were subsequently
transplanted onto the chronic cutaneous wound bed at a density of 4
units/cm2, which was considered the minimum density
required to guarantee tissue regeneration and re-epithelialization
of the treated wound area. Care was taken to avoid hair follicle
unit transection and bleeding was managed with pressure.
Following surgery, a Vaseline® gauze dressing
(Shaoxing ZhengDe Surgical Dressing Co., Ltd., Zhejiang, China) was
applied to the recipient site, which was changed daily until day 5,
and every 3–5 days thereafter. The patients were not administered
any painkillers or anticoagulants.
Assessment of clinical outcomes
Clinical evaluations were performed and digital
images of the recipient sites were captured at weeks 0, 1, 2, 3, 4,
5, 8 and 14 following intervention. An evaluation of the percentage
of viable hair follicle units remaining at the wound site was
conducted at week 2. Clinical evaluation of wound healing was also
performed. Wound healing was measured as the average reduction (%)
in the total area of the wound bed at the intermediate time points,
and was assessed by clinical and anatomopathological signs,
including wound border retraction, the appearance of granulation
tissue and evidence of re-epithelialization. To avoid
misclassification bias, two independent plastic surgeons assessed
the extent of re-epithelialization and measured the wound
areas.
Histology
Histological analysis was performed postoperatively
at week 16, the end point of the study. A 4-mm punch biopsy was
collected from the recipient wound and from the healthy skin around
the wound for each patient using a biopsy trephine (#w100671;
Dongxiyi Technology Co., Ltd., Beijing, China). Samples were fixed
in 10% formaldehyde and embedded in paraffin wax, using standard
histological procedures. The samples were subsequently stained with
hematoxylin and eosin. The samples were analyzed by a pathologist
who was blinded to any clinical data to ensure the unbiased
assessment of the secondary outcomes.
Results
Clinical outcomes
Table I shows the
baseline clinical details of the patients. A total of 14 patients
(male, 9; female, 5; mean age, 60.71±15.20 years; median age, 61
years; age range, 19–76 years) were treated using the novel
protocol. The wound areas were relatively large, ranging between 26
and 220 cm2 (median area, 48 cm2; mean area,
74.14±58.51 cm2). A long wound duration (0.5–13 years)
was also noted for the patients included in the study. Standard
wound care procedures were applied in addition to the hair follicle
unit therapy, and Table II reveals
the details of the therapeutic regimens followed by each
patient.
 | Table I.Sample demographic and clinical
characteristics of the patients (n=14). |
Table I.
Sample demographic and clinical
characteristics of the patients (n=14).
| Characteristic | Result |
|---|
| Age (years) |
|
| Median
(range) | 61 (19–76) |
| Mean
(SD) | 60.71 (15.20) |
| Gender, n (%) |
|
| Male | 9 (64.29) |
|
Female | 5 (35.71) |
| Reference wound area
(cm2) |
|
| Median
(range) | 48 (26–220) |
| Mean
(SD) | 74.14 (58.51) |
| Reference wound
duration (years) |
|
| Median
(range) | 2.5 (0.5–13) |
| Mean
(SD) | 4.18 (3.39) |
 | Table II.Wound care procedures applied to the
wound areas of patients throughout the present study. |
Table II.
Wound care procedures applied to the
wound areas of patients throughout the present study.
|
| Week |
|---|
|
|
|
|---|
| Patient number | 1 | 2 | 3 | 4 | 6 | 10 | 14 |
|---|
| 1 | Wound cleaning with
saline + chlorhexidine + vaseline gauze | Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change | Scar removal + wound
cleaning with saline + vaseline gauze | Dressing change | Dressing change |
| 2 |
| Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change | Dressing change | Dressing change | Dressing change |
| 3 |
| Wound cleaning with
chlorhexidine + vaseline gauze | Wound cleaning with
chlorhexidine + vaseline gauze | Dressing change | Dressing change | Wound cleaning with
saline + vaseline gauze | Dressing change |
| 4 |
| Dressing change | Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change | Wound cleaning with
chlorhexidine + vaseline gauze | Dressing change |
| 5 |
| Dressing change | Dressing change | Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change | Dressing change |
| 6 |
| Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change | Dressing change | Dressing change | Dressing change |
| 7 |
| Dressing change | Dressing change | Dressing change | Dressing change | Dressing change | Dressing change |
| 8 |
| Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change | Wound cleaning with
saline + vaseline gauze | Dressing change | Dressing change |
| 9 |
| Dressing change | Wound cleaning with
chlorhexidine + vaseline gauze | Dressing change | Dressing change | Dressing change | Dressing change |
| 10 |
| Fibrin scar cottage +
wound cleaning with saline + vaseline gauze + compression
bandaging | Wound cleaning with
saline + vaseline gauze + compression bandaging | Vaseline gauze +
compression bandaging | Dressing change | Dressing change | Dressing change |
| 11 |
| Dressing change | Scar removal + wound
cleaning with saline + compression bandaging | Wound cleaning with
saline + vaseline gauze + compression bandaging | Dressing change | Wound cleaning with
chlorhexidine + vaseline gauze | Dressing change |
| 12 |
| Wound cleaning with
chlorhexidine + vaseline gauze | Dressing change | Dressing change | Dressing
change | Dressing
change | Dressing
change |
| 13 |
| Dressing
change | Wound cleaning with
chlorhexidine + vaseline gauze | Wound cleaning with
saline + vaseline gauze | Dressing
change | Dressing
change | Dressing
change |
| 14 |
| Dressing
change | Wound cleaning with
chlorhexidine + vaseline gauze | Dressing
change | Dressing
change | Dressing
change | Dressing
change |
The average percentage reduction in the wound area
was measured as the primary outcome. At week 1, the wound bed was
red and unviable hair follicle units were not observed. The
viability evaluation at week 2 revealed the mean percentage of
successful hair follicle units as 71.85±7.75% (Fig. 3). The fabric scarred around the hair
follicle units between weeks 3 and 4. At week 5, clinical
epithelialization was clearly observed and the wound reduction was
significant (Fig. 4). Total healing
was observed in all patients, and a fragile scar of reddish color
was noted after the first 2 months (Fig.
5), which progressively disappeared (Fig. 6). Unlike the scar tissue, the
reception area was elastic, which contributed to improved healing
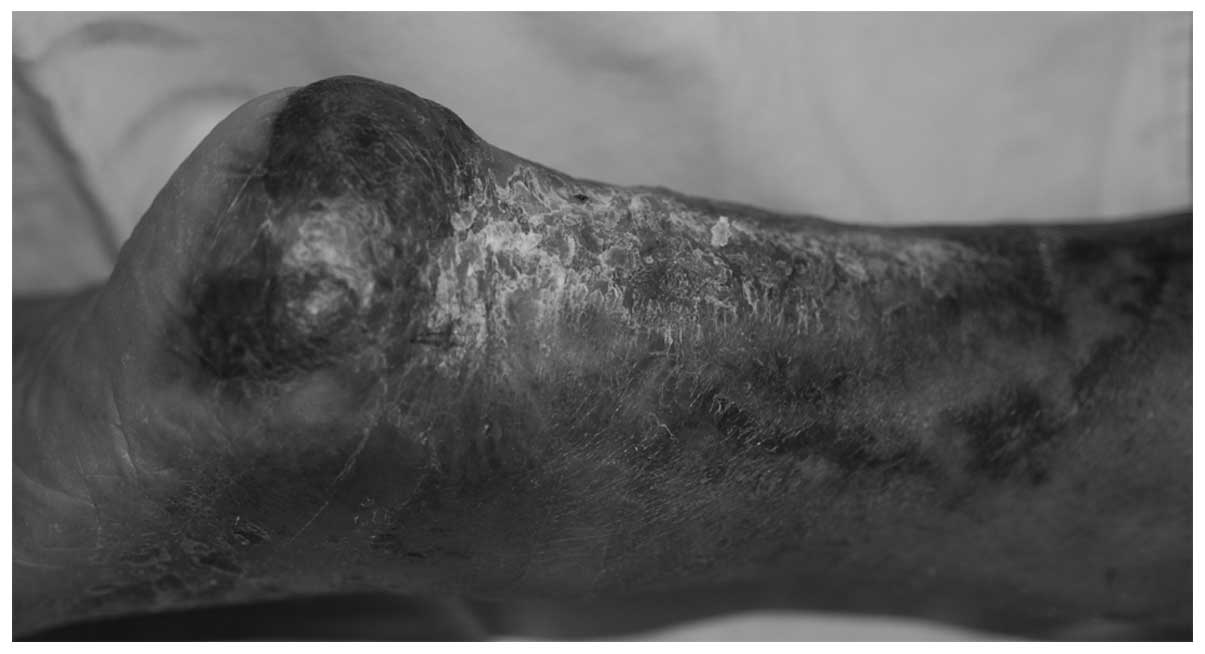
quality. Patient 9, who had a leg wound, developed enhanced
ambulation as a result of the improved treatment method (Fig. 7). The disproportionate rarity of
hair, in contrast to the viability of the hair follicle units, was
also observed. Improvement in clinical symptoms, including wound
border reactivation and a lower amount of exudation, was observed
in 12/14 patients.
Complications
Overall, the procedure appeared to be safe. However,
three patients presented with minor unrelated complications during
the study period (patients 2 and 6 had atrial fibrillation, and
patient 12 had a recurrent edema in the lower right extremity).
Evaluation of the scalp-donor sites during the
follow-up revealed no evidence of hair thinning, hair loss or
alopecia. All donor sites were healed by day 7 following
surgery.
Histological analysis
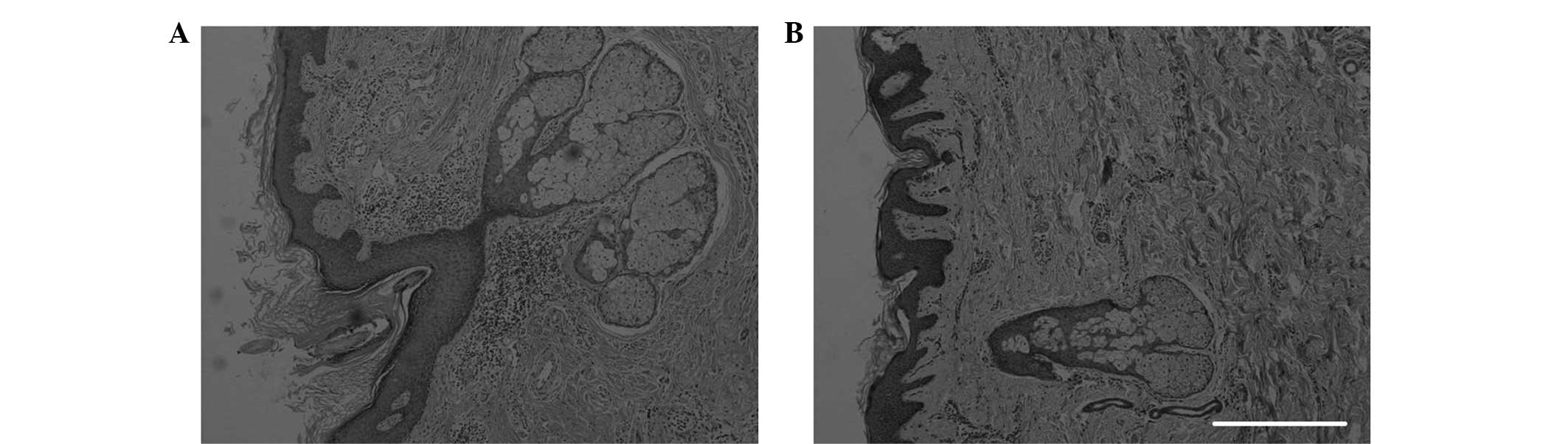
Punch biopsies were performed on the recipient
square at week 16 following surgery. Histological analysis revealed
that the epidermis and papillary dermis were contained within the
recipient square. Adnexal structures and the reticular dermis were
also observed. The outer hair shafts were macroscopically visible
within the recipient wound area in the majority of patients
(Fig. 8).
Discussion
Chronic cutaneous wounds, regardless of
pathogenesis, can be devastating to patients, even when treated,
and can result in a huge financial burden on medical
establishments. Complete closure and protection of the wound is
important for patients. Despite numerous therapeutic advances, the
gold-standard protocol used in routine practice is an autologous
split-thickness skin graft. This procedure involves removing a
piece of skin from a secondary surgical site and reapplying the
graft onto the wound bed. Although the clinical outcome of the skin
graft treatment is reasonable, donor sites are limited and
secondary injury is inevitable. Technological developments,
including suspending cells in fibrin-collagen gel (13), have been investigated in an attempt
to obtain an improved treatment for wound healing. However, these
are costly to produce and are not covered by Chinese health
insurance companies.
The epithelium can be restored by the migration of
epithelial cells from the old epithelium adjoining a wound or by
centrifugal migration from any hair follicle that remains within
the wound (14). Several studies
have unambiguously identified the hair follicle as a major reserve
of adult stem cells (15,16). Dermal grafts from the scalp (10), early implantation of microdissected
hair follicles through a silicone epidermis (11) and hair grafting (17) are used for cutaneous wound repair;
however, the procedures are complicated. In the present study, hair
follicles without epidermal or interfollicular tissue were
transplanted. The hair follicles were microdissected as individual
units and transplanted into the wound bed. The function of the hair
follicles as promoters of re-epithelialization was observed in the
current study.
The present study was originally conceived as
research into the feasibility of a novel therapy. Questions
relating to the surgical technique were not specifically assessed;
however, placing the hair follicles onto the wound (partially
trialled on patients 1 and 2) resulted in a lower degree of
viability compared with other patients in the present study (data
not shown). Patient 1 displayed a relatively large wound area (186
cm2) and patient 2 had a long wound duration (13 years,
including primary and repeating recurrent).
The clinical results indicate that the method of
transplanting hair follicle units into the cutaneous wound is not
only feasible in practice, but is also successful in improving the
long-term clinical healing of wounds. In all the cases, the hair
follicles augmented epithelialization and the formation of
granulation tissue at the wound site. At the study endpoint, the
hair follicle-treated wound area appeared to be elastic, unlike
scar tissue, which contributed to the improved healing quality and
allowed enhanced ambulation for one patient with a wounded leg.
Although complete healing was observed in all the patients, an
objective healing rate should be based on more substantial data and
stronger evidence. A larger sample size is required in future
studies.
Histological analysis provided evidence of
re-epithelialization and the existence of outer hair shafts. The
recovered area was likely to have contained a number of adnexa of
the skin. However, when analyzing the histological results, the
exact position of the biopsies may differ due to the varying
overall aspect of the entire wound.
Recent advances in epithelial stem cell biology have
improved the understanding of the role of hair follicles in wound
healing mechanisms, and have provided a basis for the development
of novel therapies (18). Various
follicular cells contribute to wound healing through different
methods. Bulge stem cells produce transiently amplifying epidermal
progeny, while non-hair follicle-fated isthmus stem cells generate
long-lasting populations in the wound epidermis (19,20).
Clinical and experimental data indicate that the involvement of
follicle-derived dermal cells results in qualitatively improved
dermal repair (18,21). Consistent with previous studies, the
observations of the present study support the hypothesis that hair
follicles perform an important function in the repair of cutaneous
wounds (22,23). Prior to the dissection of hair
follicle units, the epithelium was intentionally removed from the
graft. This step allowed for the formal exclusion of the
possibility that the healing effect was due to non-follicular
tissue. However, in the current study, the limited sample size
(which was small since the study was the first to be conducted in
clinical practice) and experimental methods may have affected the
quality of the results; the data are unable to confirm that
re-epithelialization occurred from the stem cells specifically.
Nevertheless, wound healing initiated by the follicles applied to
the chronic wound bed was observed and may have indirectly
supported the hypothesis that hair follicles perform an important
function in the repair of cutaneous wounds. Although there have
been numerous advances in stem cell therapy, further studies are
essential.
In conclusion, the present study demonstrated the
capacity of hair follicle units to repair chronic cutaneous wound
sites. Complete healing was observed and the procedure appeared to
be safe. With the exclusion of alopecic, insufficiently hairy and
elderly patients, the present method may be used when donor sites
are rare, due to the reduced donor-site morbidity, and may be a
novel surgical method to avoid more complicated, costly and
time-consuming procedures. By combining the hair transplantation
and plastic reconstruction techniques, a novel surgical protocol
may be developed, which may provide an additional option for
secondary surgery on chronic wounds. However, this method requires
a surgeon with advanced training in hair follicle unit
harvesting.
Acknowledgements
The authors thank the patients who participated in
the study. The study was supported by a grant provided by the
Shanghai Municipal Science and Technology Commission (#07JC14013;
2007).
References
|
1
|
Castilla DM, Liu ZJ, Tian R, Li Y,
Livingstone AS and Velazquez OC: A novel autologous cell-based
therapy to promote diabetic wound healing. Ann Surg. 256:560–572.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lau K, Paus R, Tiede S, Day P and Bayat A:
Exploring the role of stem cells in cutaneous wound healing. Exp
Dermatol. 18:921–933. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hu L, Zhao J, Liu J, Gong N and Chen L:
Effects of adipose stem cell-conditioned medium on the migration of
vascular endothelial cells, fibroblasts and keratinocytes. Exp Ther
Med. 5:701–706. 2013.PubMed/NCBI
|
|
4
|
Dittmer J and Leyh B: Paracrine effects of
stem cells in wound healing and cancer progression (Review). Int J
Oncol. 44:1789–1798. 2014.PubMed/NCBI
|
|
5
|
Brower J, Blumberg S, Carroll E, Pastar I,
Brem H and Chen W: Mesenchymal stem cell therapy and delivery
systems in nonhealing wounds. Adv Skin Wound Care. 24:524–534.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jahoda CA and Christiano AM: Niche
crosstalk: Intercellular signals at the hair follicle. Cell.
146:678–681. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Murawala P, Tanaka EM and Currie JD:
Regeneration: The ultimate example of wound healing. Semin Cell Dev
Biol. 23:954–962. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Waters JM, Richardson GD and Jahoda CA:
Hair follicle stem cells. Semin Cell Dev Biol. 18:245–254. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mimoun M, Chaouat M, Picovski D, Serroussi
D and Smarrito S: The scalp is an advantageous donor site for
thin-skin grafts: A report on 945 harvested samples. Plast Reconstr
Surg. 118:369–373. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zakine G, Mimoun M, Pham J and Chaouat M:
Reepithelialization from stem cells of hair follicles of dermal
graft of the scalp in acute treatment of third-degree burns: first
clinical and histologic study. Plast Reconstr Surg. 130:42e–50e.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Navsaria HA, Ojeh NO, Moiemen N, Griffiths
MA and Frame JD: Reepithelialization of a full-thickness burn from
stem cells of hair follicles micrografted into a tissue-engineered
dermal template (Integra). Plast Reconstr Surg. 113:978–981. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Plikus MV, Gay DL, Treffeisen E, Wang A,
Supapannachart RJ and Cotsarelis G: Epithelial stem cells and
implications for wound repair. Semin Cell Dev Biol. 23:946–953.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Skardal A, Mack D, Kapetanovic E, Atala A,
Jackson JD, Yoo J and Soker S: Bioprinted amniotic fluid-derived
stem cells accelerate healing of large skin wounds. Stem Cells
Transl Med. 1:792–802. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brown JB and McDowell F: Epithelial
healing and the transplantation of skin. Ann Surg. 115:1166–1181.
1942. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jaks V, Kasper M and Toftgård R: The hair
follicle - a stem cell zoo. Exp Cell Res. 316:1422–1428. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jiménez F, Garde C, Poblet E, et al: A
pilot clinical study of hair grafting in chronic leg ulcers. Wound
Repair Regen. 20:806–814. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jahoda CA, Horne KA and Oliver RF:
Induction of hair growth by implantation of cultured dermal papilla
cells. Nature. 311:560–562. 1984. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hill RP, Gardner A, Crawford HC, et al:
Human hair follicle dermal sheath and papilla cells support
keratinocyte growth in monolayer coculture. Exp Dermatol.
22:236–238. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jensen KB, Collins CA, Nascimento E, Tan
DW, Frye M, Itami S and Watt FM: Lrig1 expression defines a
distinct multipotent stem cell population in mammalian epidermis.
Cell Stem Cell. 4:427–439. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Snippert HJ, Haegebarth A, Kasper M, et
al: Lgr6 marks stem cells in the hair follicle that generate all
cell lineages of the skin. Science. 327:1385–1389. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jahoda CA and Reynolds AJ: Hair follicle
dermal sheath cells: unsung participants in wound healing. Lancet.
358:1445–1448. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Leirós GJ, Kusinsky AG, Drago H, et al:
Dermal papilla cells improve the wound healing process and generate
hair bud-like structures in grafted skin substitutes using hair
follicle stem cells. Stem Cells Transl Med. 3:1209–1219. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Baquerizo Nole KL and Kirsner RS: Hair
follicles and their potential in wound healing. Exp Dermatol.
24:95–96. 2015. View Article : Google Scholar : PubMed/NCBI
|