Introduction
Viral myocarditis is an inflammatory disease of the
myocardium with heterogeneous clinical manifestations and
progression, which make it challenging to diagnose and treat. It
has been reported that myocarditis occurs in ~12% of young adults,
and may contribute to other myocardial diseases, such as dilated
cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy
(1). The clinical manifestations of
myocarditis vary from mild disease with no symptoms, to heart
failure and mortality. Myocarditis may be associated with heart
tissue necrosis in some cases (2).
There are numerous diagnostic methods for myocarditis, including
cardiac magnetic resonance (CMR) imaging and endo-myocardial
biopsy. CMR imaging is recommended as a credible and useful
approach for monitoring the reversible and irreversible myocardial
tissue injuries, and to distinguish acute myocarditis from healed
myocarditis (3). Myocarditis may be
caused by various viral infections, such as parvovirus B19,
adenovirus and Coxsackie B virus. Therefore, virological detection
of cardiac tissue is important for the diagnosis of myocarditis
(4). Myocarditis may resemble
myocardial infarction (5–7). In this study, a case of viral
myocarditis in a patient with acute retrosternal pain, elevated
cardiac markers and electrocardiographic ST-T changes similar to
the clinical presentation of myocardial infarction is presented.
Informed consent was obtained from the patient.
Case report
Primary diagnosis and treatment in the
Emergency Room (ER)
A 22-year-old male was admitted to the ER with acute
retrosternal pain and tightness that had persisted for >3 h.
Upon presentation, on June 18, 2012, physical examination showed
that his blood pressure was 120/70 mmHg, temperature was 37.2°C and
heart rate was 63 bpm. First and second heart sounds were normal
without any audible murmurs, rubs or gallops. No yellow
discoloration of the skin or mucous membranes, bleeding or rashes
were observed, and the remainder of the examination was normal. No
history of hypertension or diabetes or family history of heart
disease was reported, and the patient never smoked cigarettes or
drank alcohol.
A series of investigations were subsequently
performed in the ER. The results of the cardiac enzyme tests
disclosed that the troponin I (TnI) level was significantly
elevated, up to 7.86 ng/ml (Table
I). The stool studies were negative. Of note were the signs of
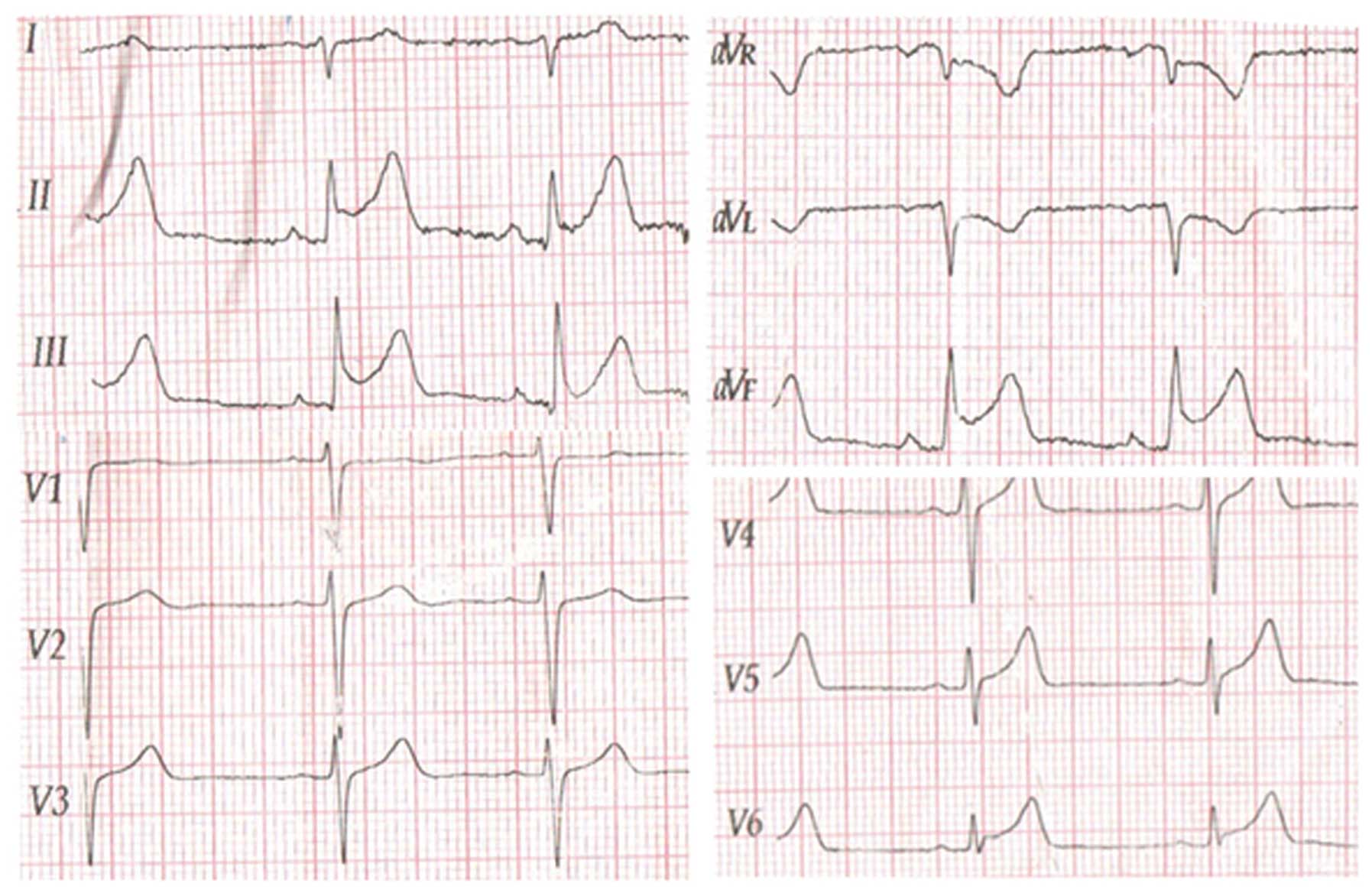
ST-segment elevations in leads II, III and aVF on the
electrocardiogram (ECG), suggestive of myocardial ischemia
(Fig. 1). An echocardiogram showed
that the patient's heart functioned normally with an ejection
fraction of 63%, excluding the possibility of mitral valve prolapse
syndrome.
 | Table I.Results of the laboratory tests. |
Table I.
Results of the laboratory tests.
| Test | Value | Reference |
|---|
| WBCs
(x109/l) | 5.75 | 4–10 |
| Neutrophils (%) | 55.1 | 50–70 |
| Hemoglobin
(g/l) | 149 | 110–160 |
| Triglyceride
(mmol/l) | 1.06 | 0.30–1.80 |
| Total cholesterol
(mmol/l) | 3.45 | 3.40–6.50 |
| CK-MB (ng/ml) | 31.4 | 0–3.7 |
| MYO1 (ng/ml) | 59.5 | 0–73 |
| Troponin I
(ng/ml) |
| 0.00–0.090 |
| June
18, 2012 | 7.860 |
|
| June
20, 2012 | 8.470 |
|
| June
26, 2012 | 0.295 |
|
| BNP (pg/ml) | 15.2 | 0.0–100.0 |
| ESR (mm/h) | 11 | 2–20 |
| ASO (IU/ml) | 62 | 0–200 |
| U&E/LFT | Normal |
|
| RF | Negative |
|
| PPD | Negative |
|
Based on the findings of retrosternal pain, a
typical ECG pattern of myocardial ischemia and an elevated TnI
level, a tentative diagnosis of acute myocardial infarction was
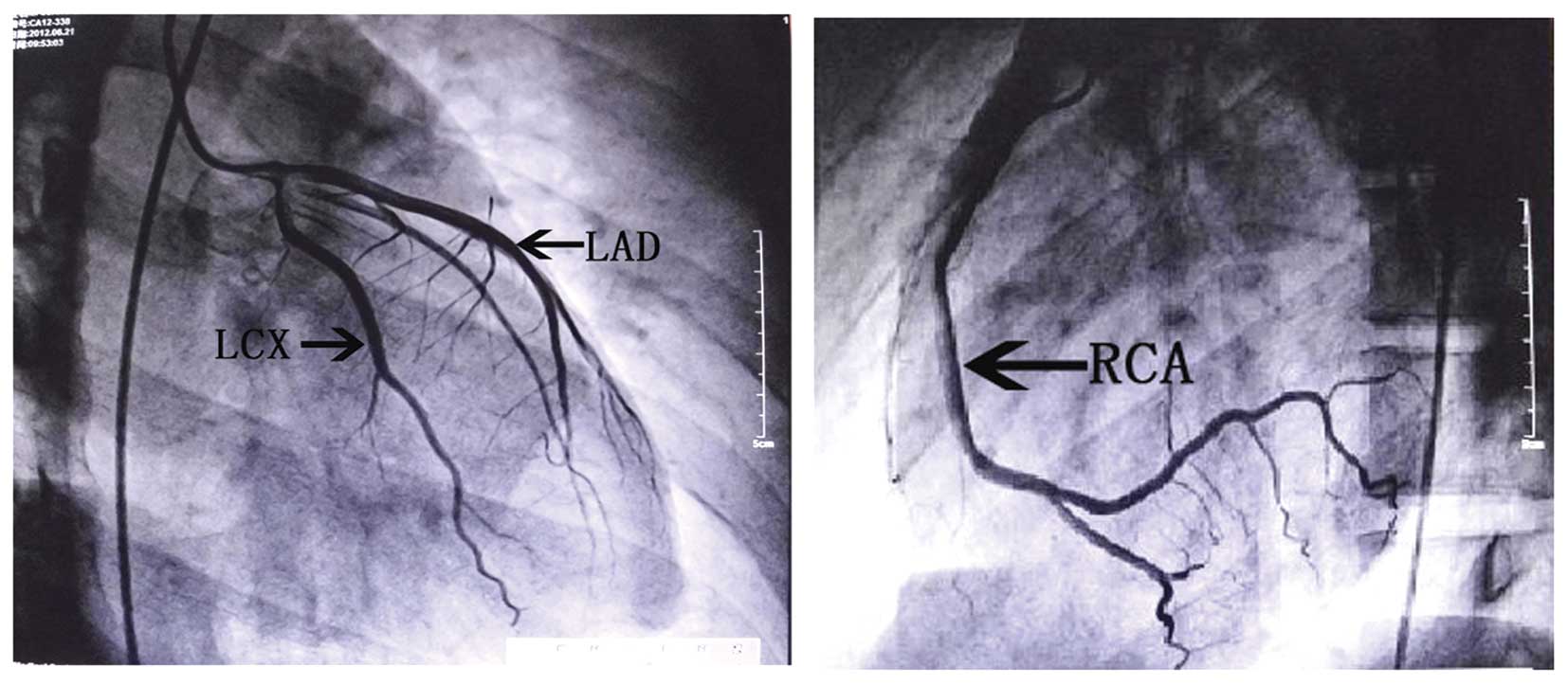
made. The patient immediately underwent coronary angiography, which
showed normal epicardial coronary arteries (Fig. 2), contradictory to the diagnosis of
myocardial infarction. On the second day of admission, June 19,
2012, he was transferred to the cardiology department for further
diagnosis and treatment.
Clinical changes following
admission
On the third day of admission, June 20, 2012, the
temperature of the patient was 37.0°C in the morning but rose to
38.4°C at 7:00 p.m. In the following days, his temperature
fluctuated between 35.5 and 38.4°C, and a range of necessary tests
was performed to exclude other diseases that could also lead to
body temperature rises (Table I).
Scattered small red dots appeared on his feet, and the rash further
expanded to his arms and legs 2 days later. A standard 12-lead ECG
on the third day showed that the elevated ST segment in the II, III
and aVF leads began to fall back, coupled with T-wave inversion.
The TnI level increased to 8.470 ng/ml (Table I). Other examinations were performed
during his hospitalization: A chest X-ray showed a normal heart
size and mild markings in the lungs, with no clear indication of
substantive lesion.
Secondary diagnosis, treatment and
prognosis
Evidence of a fluctuating fever and normal coronary
arteries subverted the initial impression of acute myocardial
infarction and aroused the suspicion of viral myocarditis. The
diagnosis of myocarditis was confirmed by the clinical
manifestation of a rash on the arms and legs. The patient was given
an antiviral drug (acyclovir; 0.4 g, 3 times/day) and drugs to
improve cardiac metabolism (trimetazidine; 20 mg, 3 times/day).
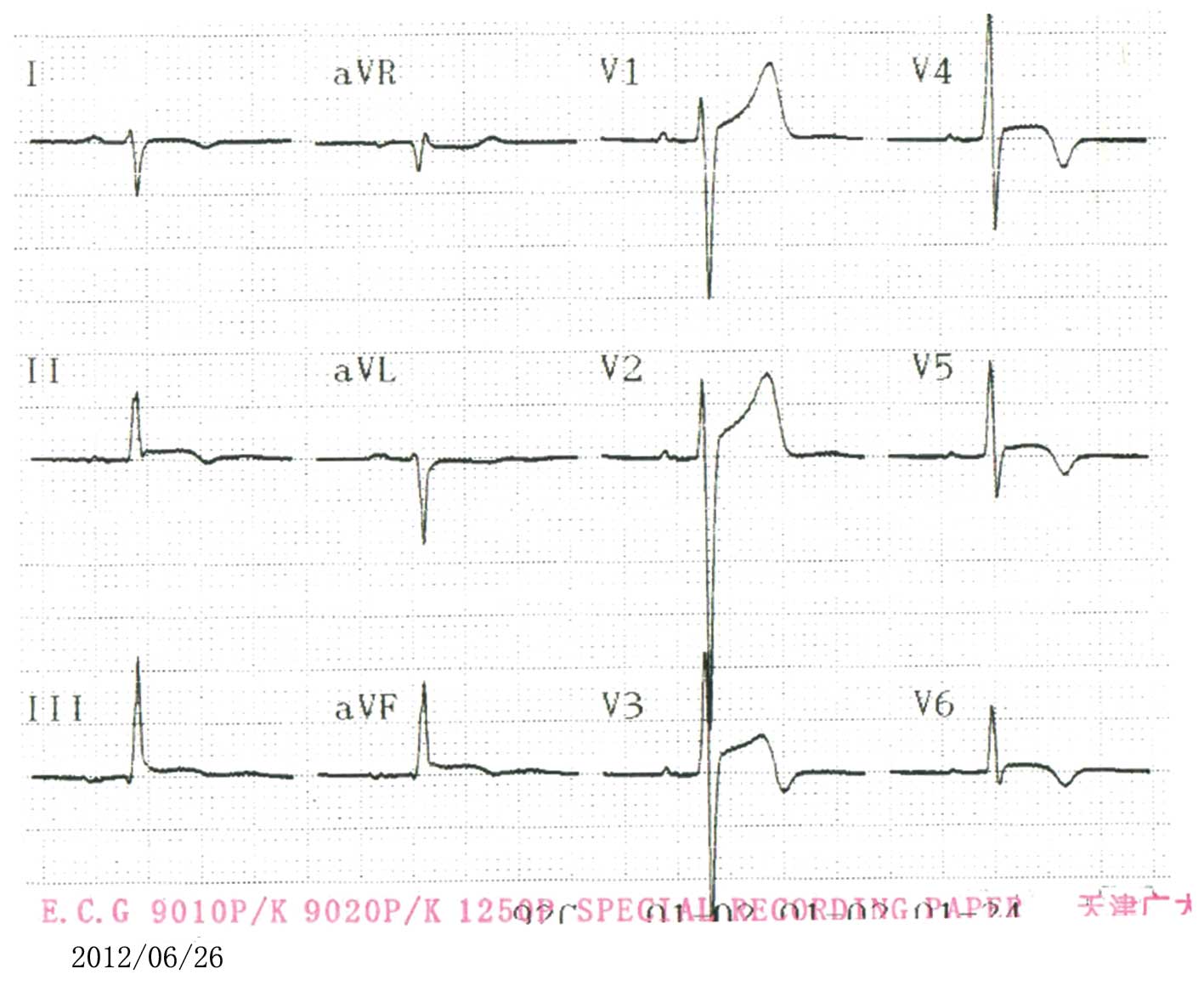
Following 2 days of treatment, on the ninth day of admission (June
26, 2012), an improvement was observed, as indicated by the
elevated ST segment in leads II, III and aVF falling back to
baseline with T-wave inversion (Fig.
3) and the TnI level decreasing to 0.295 ng/ml.
The patient was discharged 2 weeks later. A
post-discharge 1-month follow-up visit showed that the patient was
recovering well.
Discussion
Viral myocarditis is a common disease with a
variable natural history. In the present case, the patient had
typical retrosternal pain, elevated cardiac markers and
electrocardiographic ST-T changes on admission, and was initially
diagnosed with acute myocardial infarction; however, emergency
coronary angiography demonstrated normal coronary anatomy. In
addition, in the week following admission the patient presented
with a flu-like illness manifesting as slight chills and fever. His
cardiac enzymes subsequently decreased and the ST-segment elevation
gradually decreased. Other unique characteristics of myocarditis in
this case were the temperature fluctuations and the rash on the
patient's arms and legs, which appeared later during his
hospitalization. Based on these clinical manifestations and
auxiliary examination, the diagnosis of acute myocarditis could be
confirmed.
It is likely that the typical clinical presentations
of myocardial infarction, such as chest pain, ST-segment elevation
and incremental serum markers, appear in patients diagnosed with
myocarditis (8). The diagnosis of
myocarditis is often empirical. Physicians should take into
consideration several lines of evidence, such as clinical
presentation, ECG alterations and cardiac enzyme changes, prior to
making a diagnosis. In addition, epicardial coronary artery disease
should be excluded. The following discussion aims to provide a
comprehensive description of viral myocarditis, including the
pathogenesis, clinical presentation, development of diagnostic
methods and treatment.
With regard to the etiology of the condition, the
advancement of molecular biology has led to the identification of a
number of different viruses and virus subtypes that are causative
factors for myocarditis. The more common viruses are
coxsackievirus, adenovirus, cytomegalovirus and parvovirus B19, as
well as hepatitis C, influenza, herpes simplex and Epstein-Barr
viruses (9,10).
In the first phase of myocarditis, the virus enters
and proliferates in the myocardium, causing direct myocardial
damage, followed by the initiation of the innate immune response.
Both the direct myocardial damage caused by the virus and the
subsequent immune process result in destruction of the
cardiomyocytes and lead to elevations in the serum cardiac Tn and
enzyme levels, mainly to eliminate as many virus-infected cells as
possible to control the infection, which includes the activation of
complement (a process that produces both cell lysis and substances
chemotactic for neutrophils and macrophages), the activation of
various cytokines and the infiltration of T lymphocytes and
macrophages, which can be detected by biopsy (9,11).
Following the first phase, patients will recover or progress into
the second phase in which the adaptive immune response is
activated.
Molecular mimicry accounts for part of the
persisting myocardial damage in the second phase, as the virus
antigens and the myocardial cells share similar epitopes, which
activate the B cells to produce cross-reacting antibodies and thus
activate the effector T cells (12–14).
Lawson et al (14) induced
persisting myocarditis in the susceptible BALB/c strain of mice
with mouse cytomegalovirus, and found that autoantibodies to
cardiac myosin were produced following mouse cytomegalovirus
infection. These affinity-purified anti-cardiac myosin antibodies
cross-reacting with mouse cytomegalovirus proteins suggest that
viral infection may modulate the immune recognition of the common
epitopes shared between the mouse cytomegalovirus proteins and the
heavy chain of myosin (14).
Cross-reacting antibodies with auto-antigens have also been found
in patients with myocarditis (15).
In the third phase, the intensity of the immune response is
downregulated and fibrosis starts (16,17). As
a result, the persistent low-grade immune response leads to
extensive myocardial injury and, eventually, dilated cardiomyopathy
(17,18).
The clinical manifestations of viral myocarditis are
highly variable, ranging from asymptomatic to acute heart failure.
Acute myocarditis often presents with a flu-like illness, including
fever, myalgia, malaise, nausea and vomiting, for a few days to 3
weeks before any cardiac symptoms appear (19). The majority of patients will make a
full recovery; however, a number of patients can rapidly progress
to chest pain, respiratory distress, arrhythmia or even heart
failure, which necessitates hospital admission. Further physical
examination may reveal cardiac pathological signs, such as sinus
tachycardia, low first heart sounds, gallops and murmurs of mitral
or tricuspid insufficiency, which are not specific for myocarditis.
Other unspecific signs, such as the appearance of skin rashes, can
also be found in certain patients (20). In the current case of viral
myocarditis, the patient had fever with temperature fluctuations
between 35.5 and 38.4°C and subsequently showed a rash on the arms
and legs in the week following admission.
Several diagnosis modalities can be helpful in the
diagnosis of myocarditis, including electrocardiography and cardiac
biomarkers. Damage of the myocytes causes abnormal electrical
activity of the heart, which leads to abnormalities in the ECG,
including ST-T wave changes, ST elevation, atrial and ventricular
arrhythmias, atrial-ventricular and intraventricular conduction
defects and variant early repolarization (21); however, these ECG alterations are
non-specific. Myocarditis may share similar ECG changes with
myocardial infarction. TnT, TnI and creatine kinase (CK)-MB are the
most commonly used cardiac biomarkers. Cardiac Tn is mainly
elevated in the acute phase of myocarditis and decreases gradually
as the patient improves (22). The
sensitivity of cardiac biomarkers to myocardial injury varies. As
with electrocardiography, cardiac Tns are non-specific for
myocarditis, although they are more sensitive than CK levels.
Consistently, in this case of viral myocarditis, the TnI level
began rising from the first day of admission, peaked at 8.470 ng/ml
on the third day but then slumped and reached 0.295 ng/ml on the
ninth day. ST-segment elevations in the II, III and aVF leads on
the ECG, accompanied by acute retrosternal pain and elevated
cardiac markers, led to the initial incorrect diagnosis of
myocardial infarction.
Since only certain patients present with elevated
cardiac enzymes, the reliability of cardiac enzymes for diagnosing
myocarditis remains uncertain and should be investigated further.
In addition to cardiac Tns, the level of brain natriuretic peptide
(BNP) measured in the plasma may be a useful biochemical marker for
myocarditis, and high concentrations of BNP may correlate with poor
prognosis in patients with myocarditis (23). Caforio et al (22) suggested that the log-BNP
concentration could be a quantitative biochemical marker of
myocarditis in Kawasaki disease. Viral culture should be considered
to help identify the virus responsible for the disease, although
the virus can only be isolated from the blood in a minority of
cases. Polymerase chain reactions, immunoglobulin antibody assays
and viral titers can help to improve the possibility of detecting
the pathogen.
Echocardiography can also be of use in the diagnosis
of myocarditis. The echocardiographic findings suggestive of
myocarditis are left ventricular dilation, decreased function,
systolic and diastolic dysfunction and regional wall motion
abnormalities. Furthermore, patients may have myocardial
interstitial edema, which can also be detected by echocardiography
through the thickness of the ventricular wall (24). There are additionally non-specific
echocardiographic characteristics associated with acute
myocarditis. In the present study, normal heart function was
suggested by an echocardiogram. Developments in technology have
brought new progress in diagnosis. Notably, recent reports have
recommended that speckle-tracking echocardiography, characterized
by the precise evaluation of regional contractility, should be used
as an adjunctive tool for the diagnosis of acute myocarditis and
inflammatory cardiomyopathy (25,26).
In recent years, cardiac magnetic resonance imaging
(CMRI) has emerged as one of the most useful imaging devices for
detecting and diagnosing myocarditis, as it can provide various
means to visualize and quantify myocardial inflammatory changes
(27,28). CMRI, however, is not accepted by a
proportion of patients with suspected myocarditis due to the
considerable expense. The current patient was one such case.
Finally, the histological and immunological
evaluation of biopsies can be used in the diagnosis of acute
myocarditis. Endomyocardial biopsy (EMB) is not a routine
diagnostic method in the majority of cases of suspected acute
myocarditis, since it is an invasive approach and has a probability
of sampling error due to the characteristic patchy inflammation and
variability in observer interpretation. A 2013 position statement
from the European Society of Cardiology Working Group on Myocardial
and Pericardial Diseases (22)
recommended heart biopsy as a routine test for all cases of
suspected myocarditis. Conversely, the routine application of EMB
was not recommended by the 2013 American College of Cardiology
Foundation/American Heart Association (29); therefore, no consensus has been
reached with regard to the application of EMB in the diagnosis of
myocarditis. EMB was not performed in the present case.
Advances in histological and molecular genetic
technology, such as the polymerase chain reaction and in
situ hybridization, have improved the efficiency of identifying
viral genomes and cardiac inflammation. According to the Canadian
Cardiovascular Society Consensus Conference guidelines on heart
failure (updated 2009), EMB evaluation for myocarditis should
include the use of histopathological markers of inflammation and
necrosis, immunohistochemical markers and the assessment of viral
particles (30); however, it has
been indicated that the histological diagnosis of myocarditis based
on the Dallas criteria lacks sensitivity and specificity (31). Additionally, an absence of sensitive
markers for an active immunological process can limit the use of
histopathological analysis (32).
Immunohistochemical techniques can enable the quantification and
identification of activated inflammatory cells, including T
lymphocytes, B cells, macrophages and natural killer cells. Among
those cells, T lymphocytes are essential for diagnosing active
myocarditis. Immunostains for cell-specific markers may also help
confirm the presence of myocardial inflammation. The analysis of
viral replication in the myocardium through the use of the
polymerase chain reaction and in situ hybridization can help
quantify the specific viral variants accounting for myocardial
damage. Previous findings using these novel diagnostic tests point
toward a broader spectrum of viral genomes responsible for acute
myocarditis, indicating a shift from enterovirus and adenovirus to
parvovirus B19 and human herpes-virus 6 as the viruses most
frequently causing acute myocarditis (33–35).
With regard to the treatment of the condition, ~50%
of the patients with acute myocarditis are likely to spontaneously
recover within a month, ~25% will develop persistent impaired
cardiac function and up to 25–30% may either progress to dilated
cardiomyopathy, making heart transplantation a necessity, or
succumb to the condition (35,36).
For symptomatic treatment of acute myocarditis,
physical activity should be avoided, as sports may promote viral
replication and increase the burden on the heart. As long as the
patient has symptoms such as chest pain, respiratory distress, ECG
abnormalities, increased levels of TnI/T or CK-MB, symptomatic
treatment should be undertaken, including diuretics, β-blockers,
angiotensin-converting enzyme-inhibitors or angiotensin II receptor
blockers. Patients presenting with heart failure should be
administered suitable drugs, including positive inotropic agents,
vasodilators and diuretics. In the case of severe heart failure,
mechanical circulatory support should be introduced, such as an
intra-aortic balloon pump or a left ventricular assist device
(33,37). Heart transplantation should be
considered if the aforementioned measures fail. Arrhythmia is
common, particularly ventricular arrhythmia. If patients present
with severe refractory ventricular arrhythmias or atrioventricular
blocks, they may require antiarrhythmic medication or the insertion
of implantable cardioverter defibrillators or temporary pacemakers,
respectively (32).
Since patients are generally diagnosed with
myocarditis within days or weeks after the initial viral infection,
antiviral therapy is seldom used in clinical practice in the early
phase of myocarditis, although antiviral therapy has been reported
to have a positive effect in the acute viremic stage (38). A patient with
parvovirus-B19-associated fulminant myocarditis was reported to
show a complete recovery with immunosuppressive and antiviral
therapy (intravenous immunoglobulin and acyclovir) within 2 weeks
(39). Furthermore, the antiviral
effect of interferon-β therapy, enhanced by the transcription
suppressor 4E-BP1, has been reported in myocarditis induced by
coxsackievirus B3 (40).
Consistently, in the present study, the patient was administered
the antiviral drug acyclovir and cardiac metabolism-promoting drugs
and recovered within 2 weeks.
Immune suppression may be beneficial in patients
with systemic disease-related or autoimmune myocarditis but may
increase virus replication and worsen myocardial injury in viral
myocarditis. A recent study showed that immunosuppressive treatment
taken immediately on detection of sclerotic heart disease proved
effective in preventing cardiac damage progression (41). Similarly, an improved performance of
immunosuppressive therapy (azathioprine and prednisone) was
reported for children with chronic myocarditis, regardless of the
presence of viral infection, compared with conventional therapy
(42). By contrast, Hia et al
(43) reviewed the impact of
immunosuppressive therapy on the outcome of acute myocarditis in
children, and the 18 years of data suggested that immunosuppressive
therapy does not significantly improve outcomes in children with
acute myocarditis, providing negative evidence for its routine use
(43). It is therefore necessary to
evaluate the type of myocarditis carefully prior to starting the
immunosuppressive therapy in order to avoid its ill effects.
Despite considerable progress, it remains a daunting
challenge for physicians to discriminate between acute myocarditis
and myocardial infarction, particularly in the early phase. An
integrated assessment and evaluation of evidence, including medical
histories, clinical presentation and results of other auxiliary
tests, are necessary for the accurate diagnosis of myocarditis and
can guide treatment accordingly. In the current case, a patient
with viral myocarditis presented with retrosternal pain, elevated
cardiac marker levels and ST-T changes on the ECG, similar to the
clinical manifestations of acute myocardial infarction. Clinical
manifestations, including a fever with temperature fluctuations and
the appearance of a rash on the arms and legs, coronary angiography
and the results of auxiliary examinations, could aid in the
differential diagnosis between acute myocarditis and myocardial
infarction. The etiology, pathology, diagnostics and therapy of
myocarditis remain controversial. Future investigations are
required to further unravel these questions.
References
|
1
|
Friedrich MG, Sechtum U, Schulz-Menger J,
Holmvang G, Alakija P, Cooper LT, White JA, Adel-Aty H, Gutberlet
M, Prasad S, et al: International Consensus Group on Cardiovascular
Magnetic Resonance in Myocarditis: Cardiovascular magnetic
resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol.
53:1475–1487. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cooper LT Jr.: Myocarditis. N Engl J Med.
360:1526–1538. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zagrosek A, Abdel-Aty H, Boyé P, Wassmuth
R, Messroghli D, Utz W, Rudolph A, Bohl S, Dietz R and
Schulz-Menger J: Cardiac magnetic resonance monitors reversible and
irreversible myocardial injury in myocarditis. JACC Cardiovas
Imaging. 2:131–138. 2009. View Article : Google Scholar
|
|
4
|
Schultz JC, Hilliard AA, Cooper LT
Jr..Rihal CS: Diagnosis and treatment of viral myocarditis. Mayo
Clin Proc. 84:1001–1009. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Xu B, Michael Jelinek V, Hare JL, Russell
PA and Prior DL: Recurrent myocarditis - an important mimic of
ischaemic myocardial infarction. Heart Lung Circ. 22:517–522. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Costantini M, Tritto C, Licci E, Sticchi
G, Capone S, Montinaro A, Bruno A, Nuzzaci G and Picano E:
Myocarditis with ST-elevation myocardial infarction presentation in
young man. A case series of 11 patients. Int J Cardiol.
101:157–158. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Walenta K, Kindermann I, Gärtner B,
Kandolph R, Link A and Böhm M: Dangerous kisses: Epstein-barr virus
myocarditis mimicking myocardial infarction. Am J Med. 119:e3–e6.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Costantini M, Oreto G, Albanese A, Ranieri
A, De Fabrizio G, Sticchi I, Lauretti A, Capone S, Tritto C,
Fachechi C, et al: Presumptive myocarditis with ST-Elevation
myocardial infarction presentation in young males as a new
syndrome. Clinical significance and long term follow up. Cardiovasc
Ultrasound. 9:2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ikeda T, Saito T, Takagi G, Sato S, Takano
H, Hosokawa Y, Hayashi M, Asai K, Yasutake M and Mizuno K: Acute
myocarditis associated with coxsackievirus B4 mimicking influenza
myocarditis electron microscopy detection of causal virus of
myocarditis. Circulation. 128:2811–2812. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nielsen TS, Hansen J, Nielsen LP, Baandrup
UT and Banner J: The presence of enterovirus, adenovirus and
parvovirus B19 in myocardial tissue samples from autopsies: An
evaluation of their frequencies in deceased individuals with
myocarditis and in non-inflamed control hearts. Forensic Sci Med
Pathol. 10:344–350. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kühl U, Pauschinger M, Bock T, Klingel K,
Schwimmbeck CP, Seeberg B, Krautwurm L, Poller W, Schultheiss HP
and Kandolf R: Parvovirus B19 infection mimicking acute myocardial
infarction. Circulation. 108:945–950. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lawson CM: Evidence for mimicry by viral
antigens in animal models of autoimmune disease including
myocarditis. Cell Mol Life Sci. 57:552–560. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Angelini A, Calzolari V, Calabrese F,
Boffa GM, Maddalena F, Chioin R and Thiene G: Myocarditis mimicking
acute myocardial infarction: Role of endomyocardial biopsy in the
differential diagnosis. Heart. 84:245–250. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lawson CM, O'Donoghue HL and Reed WD:
Mouse cytomegalovirus infection induces antibodies which
cross-react with virus and cardiac myosin: A model for the study of
molecular mimicry in the pathogenesis of viral myocarditis.
Immunology. 75:513–519. 1992.PubMed/NCBI
|
|
15
|
Caforio AL, Mahon NJ, Tona F and McKenna
WJ: Circulating cardiac autoantibodies in dilated cardiomyopathy
and myocarditis: Pathogenetic and clinical significance. Eur J
Heart Fail. 4:411–417. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Radziwolek L, Radunski UK, Koopmann K,
Bohnen S, Zeller T, Lund G, Krull AD, Hauschild N, Stehning C, et
al: Myocardial injury and fibrogenesis: Extracellular volume
expansion is associated with elevated Galectin-3 levels in patients
with myocarditis. J Cardiovasc Magn Reson. 16:(Suppl 1). 2902014.
View Article : Google Scholar
|
|
17
|
Camporeale A, Marino F, Papageorgiou A,
Carai P, Fornero S, Fletcher S, Page BD, Gunning P, Forni M,
Chiarle R, et al: STAT3 activity is necessary and sufficient for
the development of immune-mediated myocarditis in mice and promotes
progression to dilated cardiomyopathy. EMBO Mol Med. 5:572–590.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Maekawa Y, Ouzounian M, Opavsky MA and Liu
PP: Connecting the missing link between dilated cardiomyopathy and
viral myocarditis virus, cytoskeleton and innate immunity.
Circulation. 115:5–8. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mamas MA, Fraser D and Neyses L:
Cardiovascular manifestations associated with influenza virus
infection. Int J Cardiol. 130:304–309. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bigalke B, Klingel K, May AE, Kandolf R
and Gawaz M: Human herpes virsus 6 subtype A-associated myocarditis
with ‘apical ballooning’. Can J Cardiol. 23:393–395. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Morgera T, Di Lenarda A, Dreas L,
Pinamonti B, Humar F, Bussani R, Silvestri F, Chersevani D and
Camerini F: Electrocardiography of myocarditis revisited: Clinical
and prognostic significance of electrocardiographic changes. Am
Heart J. 124:455–467. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Caforio AL, Pankuweit S, Arbustini E, et
al: Current state of knowledge on aetiology, diagnosis, management
and therapy of myocarditis: A position statement of the European
Society of Cardiology Working Group on Myocardial and Pericardial
Diseases. Eur Heart J. 34:2636–2648. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang C, Shen D, Sun H, Zhang L, Ma Y and
Huang D: Prognostic value of brain natriuretic peptide in people
with viral myocarditis. Zhonghua Shi Yan He Lin Chuang Bing Du Xue
Za Zhi. 26:125–126. 2012.(In Chinese). PubMed/NCBI
|
|
24
|
Felker GM, Boehmer JP, Hruban RH, et al:
Echocardiographic findings in fulminant and acute myocarditis. J Am
Coll Cardiol. 36:227–232. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Escher F, Kasner M, Kühl U, et al: New
echocardiographic findings correlate with intramyocardial
inflammation in endomyocardial biopsies of patients with acute
myocarditis and inflammatory cardiomyopathy. Mediators Inflamm.
2013:8754202013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hsiao JF, Koshino Y, Bonnichsen CR, et al:
Speckle tracking echocardiography in acute myocarditis. Int J
Cardiovasc Imaging. 29:275–284. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Olimulder M, Van Es J and Galjee MA: The
importance of cardiac MRI as a diagnostic tool in viral
myocarditis-induced cardiomyopathy. Neth Heart J. 17:481–486. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chan A, Tan T, Sosnovik D, Francis S and
Ghoshhajra B: Acute viral myocarditis diagnosis by cardiac magnetic
resonance imaging. Cardiovascular Images. 582014.
|
|
29
|
Yancy CW, Jessup M, Bozkurt B, et al: 2013
ACCF/AHA guideline for the management of heart failure: a report of
the American College of Cardiology Foundation/American Heart
Association Task Force on Practice Guidelines. J Am Coll Cardiol.
62:e147–e239. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Howlett JG, McKelvie RS, Arnold JM, et al:
Canadian Cardiovascular Society Consensus Conference guidelines on
heart failure, update 2009: Diagnosis and management of right-sided
heart failure, myocarditis, device therapy and recent important
clinical trials. Can J Cardiol. 25:85–105. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Baughman KL: Diagnosis of myocarditis:
Death of Dallas criteria. Circulation. 113:593–595. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kuhl U and Schultheiss HP: Viral
myocarditis: Diagnosis, aetiology and management. Drugs.
69:1287–1302. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Dennert R, Crijns HJ and Heymans S: Acute
viral myocarditis. Eur Heart J. 29:2073–2082. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Basso C, Calabrese F, Angelini A, Carturan
E and Thiene G: Classification and histological,
immunohistochemical and molecular diagnosis of inflammatory
myocardial disease. Heart Fail Rev. 18:673–681. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bock CT, Düchting A, Utta F, et al:
Molecular phenotypes of human parvovirus B19 in patients with
myocarditis. World J Cardiol. 6:1832014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kindermann I, Barth C, Mahfoud F, et al:
Update on myocarditis. J Am Coll Cardiol. 59:779–792. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Grinda JM, Chevalier P, D'Attellis N, et
al: Fulminant myocarditis in adults and children: Bi-ventricular
assist device for recovery. Eur J Cardiothorac Surg. 26:1169–1173.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gupalo E, Mironova N, Stukalova O, Zykov
K, Buryachkovskaya L and Golitsyn S: A case of arrhythmia due to
myocarditis treated by antiviral therapy: New diagnostic approaches
using peripheral biomarkers. Eur Heart J. 34:172013. View Article : Google Scholar
|
|
39
|
Dennert R, Velthuis S, Westermann D, et
al: Case report Parvovirus-B19-associated fulminant myocarditis
successfully treated with immunosuppressive and antiviral therapy.
Antivir Ther. 15:681–685. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
40
|
Burke JD, Sonenberg N, Platanias LC and
Fish EN: Antiviral effects of interferon-β are enhanced in the
absence of the translational suppressor 4E-BP1 in myocarditis
induced by Coxsackievirus B3. Antivir Ther. 16:5772011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Pieroni M, De Santis M, Zizzo G, et al:
Recognizing and treating myocarditis in recent-onset systemic
sclerosis heart disease: Potential utility of immunosuppressive
therapy in cardiac damage progression. Semin Arthritis Rheum.
43:526–535. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Camargo PR, Okay TS, Yamamoto L, Del Negro
GM and Lopes AA: Myocarditis in children and detection of viruses
in myocardial tissue: Implications for immunosuppressive therapy.
Int J Cardiol. 148:204–208. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hia CP, Yip WC, Tai BC and Quek SC:
Immunosuppressive therapy in acute myocarditis: An 18 year
systematic review. Arch Dis Child. 89:580–584. 2004. View Article : Google Scholar : PubMed/NCBI
|