Introduction
An increasing number of studies have revealed that
the incidence of diabetes is based on the relative or absolute
deficiency of insulin secretion from islet β-cells, which is caused
by high levels of blood glucose (1–3).
Diabetes is characterized by chronic, systemic metabolic disorders,
while diabetic nephropathy (DN) is a systemic complication of
diabetes. DN is a progressive kidney disease caused by angiopathy
of the capillaries in the kidney glomeruli (4) and is characterized by nephrotic
syndrome and diffuse glomerulosclerosis. DN is one of the most
serious, chronic complications of diabetes, seriously affecting the
life of patients, and in certain cases, resulting in mortality
(5).
According to traditional Chinese medicine (TCM)
syndrome differentiation typing, DN is classified as a variety of
types, including ‘Thirsty’, ‘Consumption’ and ‘Edema’ (6). Specifically, DN is associated with
congenital deficiency, diet, emotional disorders, excessive labor
and fever. Currently, TCM considers the pathogenesis of DN to be
involved in spleen and kidney deficiency. Qi is the driving force
of life activities and Yin is the material basis of life activities
(7). Damage of Qi is more common in
early DN (8), and as the disease
progresses, DN gradually causes the damage of Yin (8–10).
Disease of the islet β-cells is closely associated
with the spleen (11). Modern
medicine and TCM considers the kidney to be associated with the
nervous, endocrine, reproductive, exercise, breathing, digestion,
water metabolism, blood and immune systems, as well as other
abnormal physiological functions (12–16). A
previous study indicated that replenishing the kidney to regulate
the peripheral tissue insulin response and glucose tolerance in the
treatment of DN may reduce the blood sugar level caused by
glomerular filtration, and reduce proteinuria (12). A number of studies have found that
the levels of 17-hydroxycorticosteroids are generally lower in
patients with kidney deficiency compared with healthy individuals,
with half of the patients exhibiting a delayed reaction for the
adrenocorticotropic hormone on the second infusion test (ACTH
test), indicating that patients with kidney deficiency have an
altered pituitary-adrenal system (16–19).
Currently, clinical use of TCM in spleen-kidney-care
has achieved a certain therapeutic effect for diabetes (20). Spleen-kidney-care Yiqi Huayu and
Jiangzhuo decoction (SKC-YJ) is a TCM compound that has been
previously applied in DN treatment (21). In the present study, the urinary
albumin excretion rate (UAER), fasting blood glucose (FBG), 2
h-postprandial blood glucose (PBG), glycosylated hemoglobin
(HBAlc), triglyceride (TG), total cholesterol (TC), blood
viscosity, fibrinogen (Fib) and C-reactive protein (CRP) levels
were investigated following treatment with SKC-YJ. The side-effects
of SKC-YJ treatment on the blood, liver, gastrointestinal and renal
functions were also analyzed. Thus, the aim of the present study
was to investigate the effect of SKC-YJ on DN treatment.
Patients and methods
Patients and demographic data
A total of 72 patients with DN were recruited into
the study (22). During the
treatment, four cases withdrew from the treatment group, while two
cases withdrew from the control group. The treatment group included
28 males and 22 females, with an average age of 61±9 years and an
average diabetes duration of 8.4±5.2 years. The control group
included nine males and seven females, with an average age of 60±11
years and an average diabetes duration of 7.9±5.2 years. The study
was approved and registered in the Chongqing Hospital of TCM
(Chongqing, China) in 2011. The Ethics Committee approved the
screening, treatment and data collection of the patients, and all
the subjects provided written informed consent. The study was
conducted in accordance with the Declaration of Helsinki.
Treatment procedure
The two groups of patients were asked to control
their diet by limiting their protein intake (0.8 mg/kg body weight
per meal per day). Patients in the two groups were administered
insulin aspart (dose adjusted according to the patient conditions;
Novo Nordisk, Bagsvaerd, Denmark) or oral hypoglycemic agents to
control their blood glucose levels (FBG, <7.0 mmol/l; PBG,
<10.0 mmol/l). Patients with high blood pressure were
administered losartan potassium tablets to reduce their blood
pressure (≤130/80 mmHg), while those with hyperlipemia were
administered simvastatin to control the level of cholesterol.
Patients in the SKC-YJ treatment group were
administered the SKC-YJ compound containing the following
prescription: Radix Rehmanniae (20 g), Rhizoma Dioscoreae
(20 g), Fructus Corni (15 g), Fructus Psoraleae (20 g), Fructus
Rosae Laevigakea (15 g), Codonopsis pilosula (30 g),
Poria (30 g), Rhizoma Atractylodis Macrocephalae (15 g),
Elecampane (15 g), Astragalus (30 g), Angelica
sinensis (12 g), Salvia miltiorrhiza (30 g), Rhizoma
Curcuma (12 g), leech powder (3 g), coix seed (30 g),
Alisma (15 g) and cooked rhubarb (6 g). SKC-YJ was
administered three times/day for one month. In the control group,
piperazine tablets were administered three times/day for one
month.
Measurement parameter
Following treatment for one month, the 24 h-urine
protein concentration (g/24 h) and 24 h-urine volume were recorded
(C16200; Abbott Laboratories, North Chicago, IL, USA). Samples of
fasting blood (3 ml) were collected to monitor the levels of FBG,
HBAlc, TC, TG and CRP. HBAlc was tested using an HA-8160 analyzer
(Arkray Factory, Inc., Shiga, Japan), while the levels of FBG, TC,
TG and CRP were detected using a DCA Vantage Analyzer, (Siemens
Healthcare Global, Erlangen, Germany). An automatic blood viscosity
analyzer (LBY-N6Compact; Precil Medical Company, Beijing, China)
was used to measure the whole blood viscosity at high cut (BVH) and
at low cut (BVL), the plasma viscosity (PV), red blood cell
aggregation index (RBCAI), red blood cell electrophoresis time
(RBCET), whole blood reduced viscosity (BRV) and the level of Fib.
Following breakfast, 0.2-ml samples of 2 h-postprandial blood were
collected for a glucose test.
Outcome evaluation
The two groups were compared prior to and following
treatment. The treatment effect was considered to be significant if
the levels of 24 h-urinary protein were <1 g or >50% lower
compared with prior treatment, FBG was <6.1 mmol/l, PBG was
<11.1 mmol/l, HBAlc was <6.0%, TC was <5.2 mmol/l and TG
ester was <1.7 mmol/l. The treatment was considered to be
effective if the level of 24 h-urinary protein was <2 g or
>30% lower compared with prior treatment, FBG was <7.0
mmol/l, PBG was <12.1 mmol/l, HBAlc was <6.5%, TC was <6.0
mmol/l and TG ester was <2.0 mmol/l. The treatment was
considered to be invalid if the level of 24 h-urinary protein was
≥2 g or <30% lower compared with prior treatment, FBG was
>7.0 mmol/l, PBG was >12.1 mmol/l, HBAlc was >6.5%, TC was
>6.0 mmol/l and TG ester was >2.0 mmol/l. Table I lists the standard indices of blood
rheology, including BVH, BVL, PV, RBCAI, RBCET, BRV and Fib, which
were assigned on the basis of a previous study (23).
 | Table I.Standard indices of blood
rheology. |
Table I.
Standard indices of blood
rheology.
| Item | Normal index | One point | Two points | Three points |
|---|
| BVH (µPa ×
sec)a |
|
|
|
|
|
Males | 5.17–6.16 | 6.17–6.50 | 6.51–7.00 | >7.00 |
|
Females | 4.85–5.78 | 5.89–6.30 | 6.31–6.80 | >6.80 |
| BVL (µPa ×
sec)b |
|
|
|
|
|
Males | 9.48–12.23 | 12.24–12.69 | 12.70–13.00 | >13.00 |
|
Females | 9.35–11.98 | 11.98–12.10 | 12.11–12.50 | >12.50 |
| PV (µPa × sec) |
|
|
|
|
|
Males | 1.41–1.63 | 1.64–1.65 | 1.66–1.90 | >1.90 |
|
Females | 1.37–1.58 | 1.59–1.80 | 1.81–2.00 | >2.00 |
| RBCAI |
|
|
|
|
|
Males | 5.81–8.67 | 8.68–8.80 | 8.81–9.00 | >9.00 |
|
Females | 5.92–8.74 | 8.75–8.90 | 8.91–9.00 | >9.00 |
| BRV (µPa × sec) |
|
|
|
|
|
Males | 8.07–13.23 | 13.24–13.30 | 13.31–13.50 | >13.50 |
|
Females | 8.37–14.06 | 14.07–14.30 | 14.31–14.50 | >14.50 |
| RBCET (µPa ×
sec) |
|
|
|
|
|
Males | 17.00–20.00 | 20.01–21.00 | 21.01–22.00 | >22.00 |
|
Females | 17.00–23.00 | 23.01–23.50 | 23.51–24.00 | >24.00 |
| Fibrinogen
(g/l) | 2–4 | 4–5 | 5–6 | >6 |
Statistical analysis
SPSS 13.0 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. All the data are expressed as
the mean ± standard deviation. The χ2 test was used for
count data comparisons, while the Student's t-test was used for
inner group comparisons. In addition, measurement data were
compared between groups using analysis of variance. P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient demographics
Following the voluntary principles, 72 patients with
DN were divided into SKC-YJ treatment (n=54) and control (n=18)
groups, according to the minimum distribution requirements for
allocation. Following treatment, four cases in the experimental
group and two cases in the control group withdrew from the study.
The tested or measured data in the two groups are listed in
Table II. Following analysis, the
results revealed that there were no statistically significant
differences (P>0.05) between the two groups prior to treatment
with regard to disease duration, 24 h-urine protein, FBG, PBG,
HBAlc, TC, TG, BVH, BVL, PV, RBCAI, RBCET, BRV, Fib and CRP.
 | Table II.Demographic data of the recruited
patients with diabetic nephropathy in the two groups. |
Table II.
Demographic data of the recruited
patients with diabetic nephropathy in the two groups.
| Variable | Control group | Experimental
group |
|---|
| Age (years) | 60±11 | 61±9 |
| Gender, male/female
(n) | 9/7 | 28/22 |
| Diabetes duration
(years) | 7.9±5.2 | 8.4±5.2 |
| 24 h-urine protein
(g) | 2.6±3.35 | 2.8±2.35 |
| Fasting plasma
glucose (mmol/l) | 8.1±4.52 | 8.3±4.34 |
| Postprandial 2 h
glucose (mmol/l) | 12.9±3.78 | 14.5±4.34 |
| Glycated hemoglobin
(%) | 7.5±1.9 | 7.8±2.5 |
| Cholesterol
(mmol/l) | 6.26±1.35 | 6.8±1.52 |
| Triglycerides
(mmol/l) | 2.58±0.56 | 2.35±0.79 |
| Fibrinogen
(g/l) | 5.27 | 5.62 |
| C-reactive protein
(mg/l) | 19.25±4.35 | 18.76±3.48 |
| Whole blood
viscosity, high cut (µPa × sec) 200/sec |
|
|
|
Males | 6.49±0.68 | 6.53±0.42 |
|
Females | 6.30±0.54 | 6.31±0.39 |
| Whole blood
viscosity, low cut (µPa × sec) 3/sec |
|
|
|
Males | 12.73±0.52 | 12.72±0.62 |
|
Females | 12.08±0.39 | 12.05±0.45 |
| Plasma viscosity
(µPa × sec) |
|
|
|
Males | 1.62±0.73 | 1.65±0.86 |
|
Females | 1.63±0.65 | 1.62±0.67 |
| Red blood cell
aggregation index |
|
|
|
Males | 8.67±0.68 | 8.79±0.49 |
|
Females | 6.75±0.58 | 6.73±0.42 |
| Red blood cell
electrophoresis time (sec) |
|
|
|
Males | 23.19±0.32 | 23.23±0.44 |
|
Females | 22.58±0.54 | 23.01±0.47 |
| Whole blood reduced
viscosity (µPa × sec) |
|
|
|
Males | 13.55±0.76 | 13.52±0.63 |
|
Females | 13.69±0.65 | 14.60±0.45 |
SKC-YJ treatment effectively reduces
the urine protein concentration in DN patients
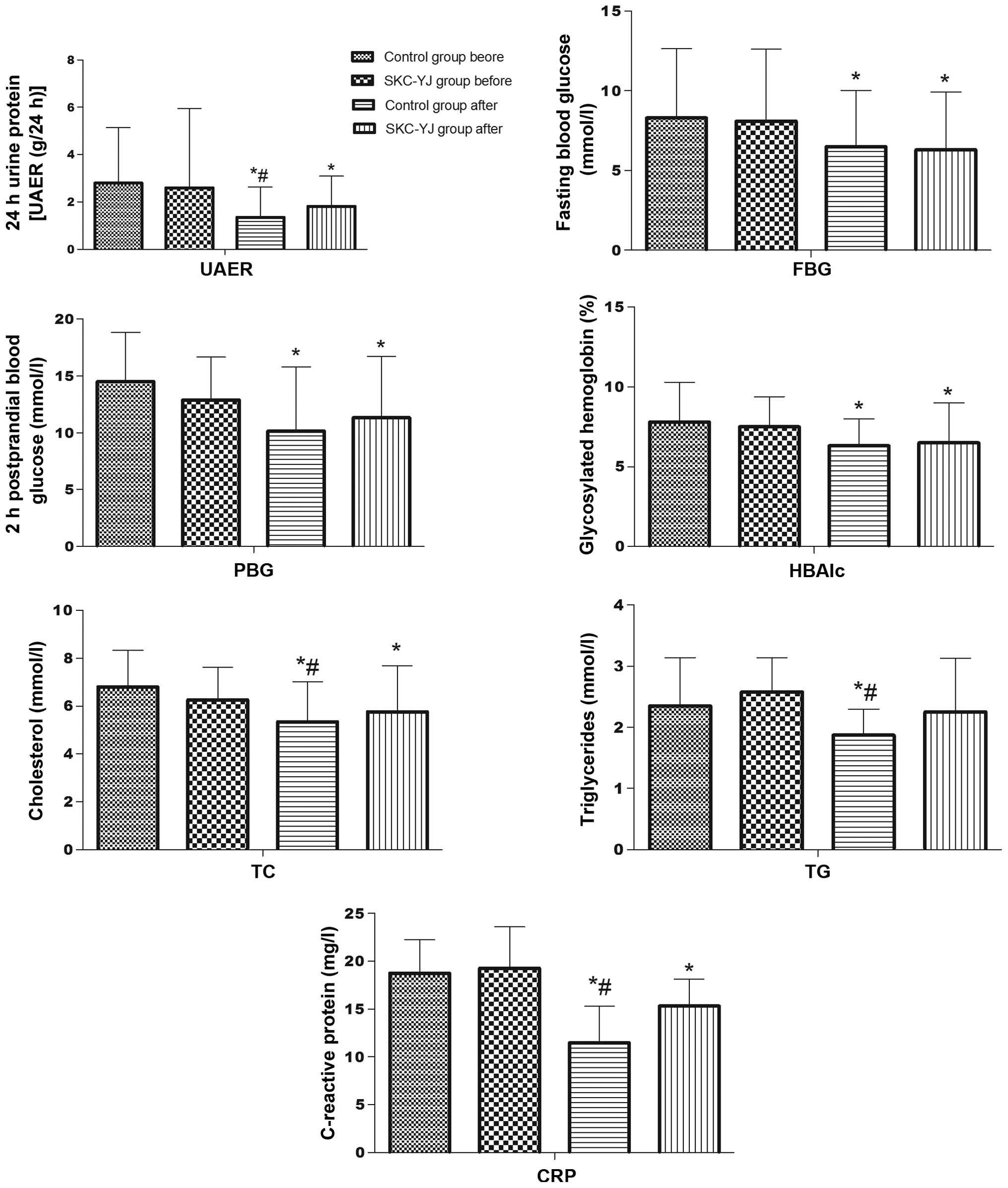
Compared with the levels prior to treatment, the
urine protein concentration after 24 h, FBG, PBG, HBAlc, TC, TG,
BVH, BVL, PV, RBCAI, RBCET, blood viscosity, Fib and CRP were
decreased (P<0.05) following piperazine and SKC-YJ treatment
(Fig. 1). However, piperazine
treatment was shown to decrease the levels of 24 h-urine protein,
TC, TG and CRP significantly more compared with SKC-YJ treatment
(P<0.05).
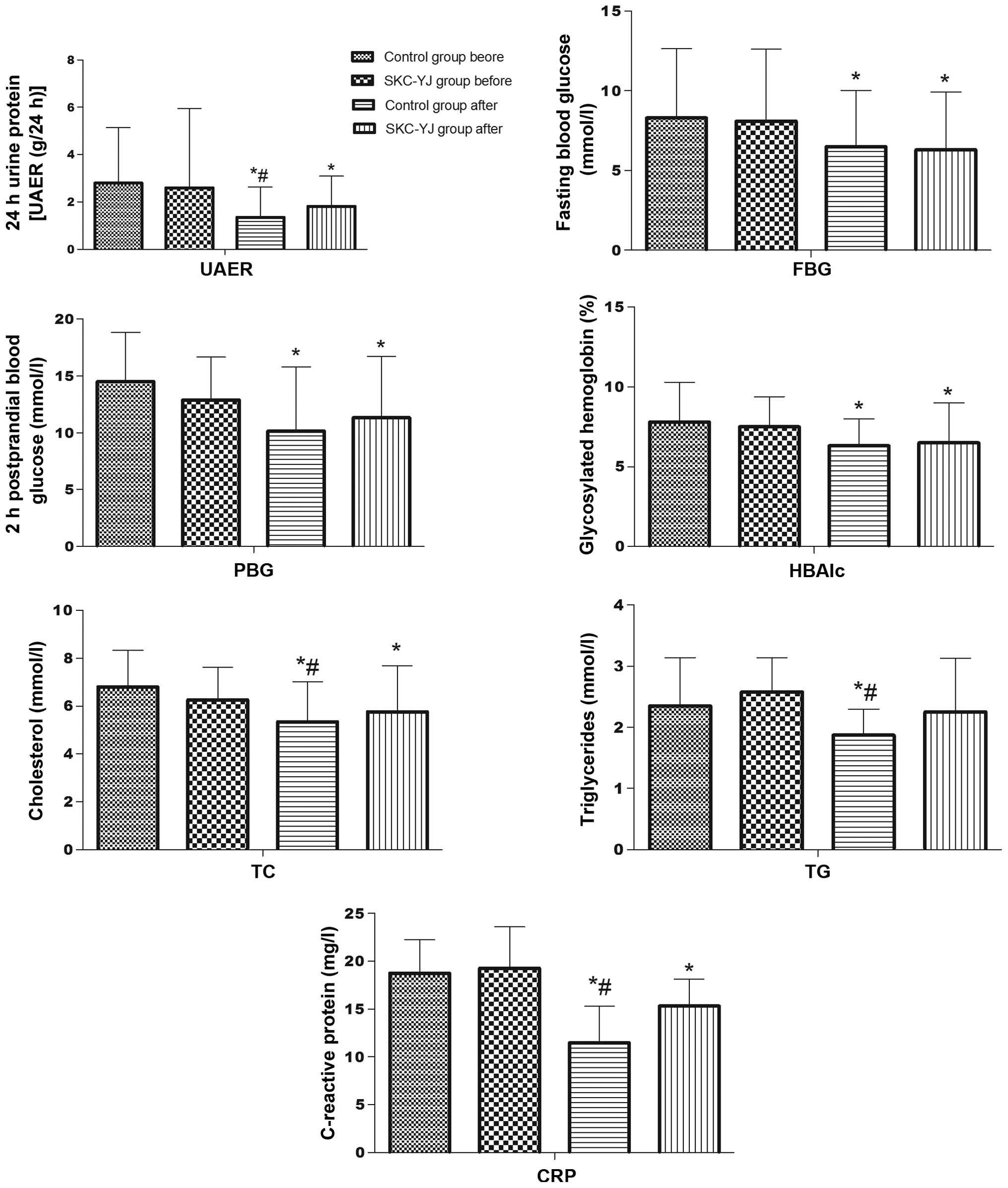 | Figure 1.Comparison of the treatment results
between the two groups with regard to the levels of UAER, FBG, PBG,
HBAlc, TG, TC and CRP. *P<0.05, vs. SKC-YJ group prior to
treatment; and #P<0.05, vs. control group following
treatment. UAER, urinary albumin excretion rate; FBG, fasting blood
glucose; PBG, 2 h-postprandial blood glucose; HBAlc, glycosylated
hemoglobin; TG, triglycerides; TC, total cholesterol; CRP,
C-reactive protein; SKC-YJ, ‘Spleen-kidney-care’ Yiqi Huayu and
Jiangzhuo decoction. |
SKC-YJ reduces the blood glucose level
and improves blood quality
Following treatment, improvements were observed with
regard to BVH, BVL, PV, RBCAI, RBCET, BRV and Fib in the two groups
(Table III). The comparison
results (Fig. 1) indicated that
piperazine was able to reduce the BVH and BVL in males, PV in
females, and RBCAI, RBCET and Fib significantly following treatment
when compared with SKC-YJ treatment.
 | Table III.Comparison of the blood test results
prior to and following treatment in the two groups. |
Table III.
Comparison of the blood test results
prior to and following treatment in the two groups.
| Index | SKC-YJ group | Control group |
|---|
|
|
|---|
| Before | After | Before | After |
|---|
| BVH (µPa ×
sec)c |
|
|
|
|
|
Males |
6.53±0.42 |
5.35±0.27a,b |
6.49±0.68 |
5.56±0.32a |
|
Females |
6.31±0.39 |
5.05±0.39a,b |
6.30±0.54 |
5.82±0.46a |
| BVL (µPa ×
sec)d |
|
|
|
|
|
Males |
12.72±0.62 |
11.15±0.62a,b |
12.73±0.52 |
11.86±0.36a |
|
Females |
12.05±0.45 |
11.12±0.37 |
12.08±0.39 |
11.79±0.46 |
| PV (µPa × sec) |
|
|
|
|
|
Males |
1.65±0.86 |
1.43±0.78 |
1.62±0.73 |
1.58±0.29 |
|
Females |
1.62±0.65 |
1.12±0.64a,b |
1.63±0.65 |
1.78±0.72a |
| RBCAI |
|
|
|
|
|
Males |
8.79±0.68 |
7.28±0.38a,b |
8.67±0.68 |
8.05±0.33 |
|
Females |
6.73±0.58 |
6.05±0.32a,b |
6.75±0.58 |
6.76±0.66 |
| RBCET (sec) |
|
|
|
|
|
Males |
23.23±0.32 |
21.01±0.27a,b |
23.19±0.32 |
22.89±0.78 |
|
Females |
23.01±0.47 |
21.02±0.53a,b |
22.58±0.54 |
21.89±0.23 |
| BRV (µPa ×
sec) |
|
|
|
|
|
Males |
13.52±0.63 |
13.08±0.71 |
13.55±0.76 |
13.48±0.38 |
|
Females |
14.60±0.45 |
13.78±0.38 |
13.69±0.65 |
13.26±0.45 |
| FIB (g/l) |
5.62±0.45 |
3.68±0.38a,b |
5.27±0.58 |
4.78±0.24 |
SKC-YJ treatment exhibits no toxicity
or side-effects in DN treatment
Side-effects in the liver, kidneys and bone marrow
were observed in the patients with DN. Compared with the levels
prior to treatment, the white blood cell count, neutrophilic
granulocyte ratio, RBC count, platelet count, alanine
aminotransferase, total bilirubin, direct bilirubin, serum
creatinine and blood urea nitrogen parameters were not
significantly different following treatment (P>0.05; Table IV). No significant gastrointestinal
reactions, including nausea, vomiting, abdominal pain and diarrhea,
or allergic reactions, including rash and itching, were observed in
the two groups.
 | Table IV.Comparison of side-effects prior and
subsequent to treatment in the two groups. |
Table IV.
Comparison of side-effects prior and
subsequent to treatment in the two groups.
| Group index | SKC-YJ group | Control group |
|---|
|
|
|---|
| Before | After | Before | After |
|---|
| WBC
(x109/l) |
5.36±3.34 |
5.78±7.25a,b |
5.88±3.86 |
6.13±4.38a |
| GR (%) |
70.35±8.42 |
69.52±6.57a,b |
69.87±6.64 |
70.05±4.38a |
| RBC
(x1012/l) |
|
|
|
|
|
Males |
5.87±3.26 |
4.85±4.63a,b |
6.47±5.37 |
6.25±3.86a |
|
Females |
3.75±3.26 |
3.54±3.17a,b |
3.26±5.48 |
4.05±3.44a |
|
PLT(x109/l) |
182±7.55 |
156±6.24a,b |
166±4.53 |
172±3.45a |
| ALT (µ/l) |
25±4.57 |
32±3.32a,b |
32±6.44 |
28±4.82a |
| TBIL (µmol/l) |
7.38±5.63 |
10.28±6.86a,b |
6.24±4.84 |
7.63±2.55a |
| DBIL (µmol/l) |
3.65±3.37 |
5.16±4.18a,b |
3.53±4.58 |
4.62±6.83a |
| Cr (µmol/l) |
|
|
|
|
|
Males |
119.5±7.53 |
110.3±7.86a,b |
109.3±5.46 |
112.6±6.28a |
|
Females |
112.6±4.18 |
109.7±3.98a,b |
108.5±5.25 |
106.8±2.86a |
| BUN (mmol/l) |
6.7±2.75 |
6.9±3.33a,b |
7.1±3.84 |
6.9±2.72a |
Discussion
The major components of SKC-YJ are Codonopsis
pilosula, Poria, Rhizoma Atractylodis
Macrocephalae and Astragalus, which have been shown to
replenish spleen deficiency. In addition, Rehmannia, Rhizoma
Dioscoreae, Fructus Corni, Alisma and Poria are able to
enforce liver and kidney function, while leech, Salvia,
Angelica and Rhizoma Curcuma have been shown to dredge
the main and collateral channels. Furthermore, coix seeds have
been used to stop water swelling, rhubarb has been used
to achieve detoxification and Fructus Rosae Laevigakea has been
used to prevent subtle leakage of the drug effect (6,20).
A previous study demonstrated that major compound
formulas based on Astragalus, Rehmannia, Rhizoma Dioscoreae,
Poria, Alisma, leeches, Angelica and rhubarb can
significantly inhibit early DN advanced glycation end products
(AGEs), with an improved therapeutic effect compared with
benazepril (24). Furthermore, the
protective effects of various doses of rhubarb on C57BL/6J mice
have been observed. The results indicated that rhubarb reduces the
mRNA and protein expression levels of AGEs in the renal
cortex of rats (25); thus, may
exert its effect through inhibiting the expression of renal cortex
AGEs.
An additional important protein in DN, protein
kinase C (PKC), is transported to the cell membrane and activated
due to sustained hyperglycemia. Subsequently, PKC activates
intracellular transcription factors, enhancing associated
transcription factors in the extracellular matrix. In addition, PKC
inhibits nitric oxide (NO) synthase activity, reduces the NO level
and causes vasoconstriction; PKC also promotes blood clotting and
thrombosis. A previous study found that PKC activity in the renal
cortex tissue membrane was increased in diabetic patients (26). Furthermore, Schnackenberg et
al (27) indicated that the
activity levels of antioxidant enzymes (superoxide dismutase and
glutathione peroxidase) in diabetic rat kidneys were significantly
lower than that in normal rat kidneys. Malondialdehyde (MDA), an
oxidative excited-state protein, has been found to be increased
significantly in diabetic rats. Following treatment with a compound
formula of Astragalus, Euonymus and rhubarb, the
expression of MDA reduced significantly compared with the model
group, indicating that this compound exhibits a strong antioxidant
effect and effectively improves the oxidation involved in DN
damage.
Previous studies have demonstrated that during the
process of DN, the number and density of podocytes decreases,
podocyte slit diaphragm key proteins (nepherin and podocin) are
expressed abnormally, and podocyte transmembrane proteins
(podocalyxin) are downregulated (28–31).
These factors result in the loss or fusion of podocytes and
glomerular basement membrane nudity, which leads to damage of the
glomerular filtration barrier. When the glomerular basement
membrane adheres to the package wall, glomerulosclerosis occurs.
Yin et al (32) observed that
a formula consisting of Astragalus, leeches and Fructuo Rosae
Laevigakea was able to promote podocin synthesis, thereby
reducing podocyte injury and maintaining the structure and
functional integrity of the podocytes.
The components of SKC-YJ include rhubarb,
Astragalus, Angelica sinensis and leech powder, among other
ingredients. The therapeutic effect of this TCM on diabetes or DN
has been identified by previous studies (33–35). The
present study demonstrated that SKC-YJ treatment is effective in
improving clinical syndromes, including reducing proteinuria, blood
glucose levels, HBAlc, blood lipids and blood viscosity, as well as
increasing the serum albumin level. Therefore, SKC-YJ may be used
as an effective supplement therapy. Since this study was with a
limited number of cases, more multicenter studies with large
samples should be needed. more systems biology researches will also
be needed to clarify the mechanism of SKC-YJ treatment for DN in
the future.
References
|
1
|
Bernal-Mizrachi E, Fatrai S, Johnson JD,
et al: Defective insulin secretion and increased susceptibility to
experimental diabetes are induced by reduced Akt activity in
pancreatic islet beta cells. J Clin Invest. 114:928–936. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
McKillop AM, Abdel-Wahab YH, Mooney MH,
O'Harte FP and Flatt PR: Secretion of glycated insulin from
pancreatic beta-cells in diabetes represents a novel aspect of
beta-cell dysfunction and glucose toxicity. Diabetes Metab.
28:3S61–3S69. 2002.PubMed/NCBI
|
|
3
|
Sesti G: Apoptosis in the beta cells:
cause or consequence of insulin secretion defect in diabetes? Ann
Med. 34:444–450. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu X, Liu L, Chen P, et al: Clinical
trials of traditional Chinese medicine in the treatment of diabetic
nephropathy - a systematic review based on a subgroup analysis. J
Ethnopharmacol. 151:810–819. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang J and Xiong X: Current situation and
perspectives of clinical study in integrative medicine in China.
Evid Based Complement Alternat Med. 2012:268–542. 2012. View Article : Google Scholar
|
|
6
|
Tong XL, Dong L, Chen L and Zhen Z:
Treatment of diabetes using traditional Chinese medicine: past,
present and future. Am J Chin Med. 40:877–886. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xie W and Du L: Diabetes is an
inflammatory disease: evidence from traditional Chinese medicines.
Diabetes Obes Metab. 13:289–301. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guo DZ, Wang YH, Bian D, Liu XR and Chen
ZQ: Effect of blood-activating and stasis-dissolving herbs on renin
angiotensin system in diabetic nephropathy rats. Zhong Yi Za Zhi.
1:75–78. 2010.(In Chinese).
|
|
9
|
Covington MB: Traditional Chinese medicine
in the treatment of diabetes. Diabetes Spectr. 14:154–159. 2001.
View Article : Google Scholar
|
|
10
|
Wang X, Zhang A and Sun H: Future
perspectives of Chinese medical formulae: chinmedomics as an
effector. OMICS. 16:414–421. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ahmed N: Advanced glycation endproducts -
role in pathology of diabetic complications. Diabetes Res Clin
Pract. 67:3–21. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Song YZ, Song SW, Wu XM, et al: Effect of
therapy of strengthening Qi and nourishing Yin, removing stasis and
dredging collaterals on diabetic nephropathy: An observation of 46
cases. J New Chi Med. 3:232008.
|
|
13
|
Makita Z, Radoff S, Rayfield EJ, et al:
Advanced glycosylation end products in patients with diabetic
nephropathy. N Engl J Med. 325:836–842. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Miura J, Yamagishi Si, Uchigata Y, et al:
Serum levels of non-carboxymethyllysine advanced glycation
endproducts are correlated to severity of microvascular
complications in patients with Type 1 diabetes. J Diabetes
Complications. 17:16–21. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ono Y, Aoki S, Ohnishi K, Yasuda T, Kawano
K and Tsukada Y: Increased serum levels of advanced glycation
end-products and diabetic complications. Diabetes Res Clin Pract.
41:131–137. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shimoike T, Inoguchi T, Umeda F, Nawata H,
Kawano K and Ochi H: The meaning of serum levels of advanced
glycosylation end products in diabetic nephropathy. Metabolism.
49:1030–1035. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rosmond R and Björntorp P: The
hypothalamic-pituitary-adrenal axis activity as a predictor of
cardiovascular disease, type 2 diabetes and stroke. J Intern Med.
247:188–197. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fujisawa I, Nishimura K, Asato R, et al:
Posterior lobe of the pituitary in diabetes insipidus: MR findings.
J Comput Assist Tomogr. 11:221–225. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vuksan V, Whitham D, Sievenpiper JL, et
al: Supplementation of conventional therapy with the novel grain
Salba (Salvia hispanica L.) improves major and emerging
cardiovascular risk factors in type 2 diabetes: results of a
randomized controlled trial. Diabetes Care. 30:2804–2810. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li WL, Zheng HC, Bukuru J and De Kimpe N:
Natural medicines used in the traditional Chinese medical system
for therapy of diabetes mellitus. J Ethnopharmacol. 92:1–21. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu YN, Guo LZ, Wang LH, Zhang LQ and Deng
W: Experimental research on prevention and therapy of diabetic
nephropathy by means of boosting qi nourishing yin transforming
stasis and downgrade turbidity. Zhong Hua Zhong Yi Yao Xue Kan.
26:1711–1713. 2008.(In Chinese).
|
|
22
|
Colman PG, Thomas DW, Zimmet PZ, Welborn
TA, Garcia-Webb P and Moore MP: New classification and criteria for
diagnosis of diabetes mellitus. The Australasian Working Party on
Diagnostic Criteria for Diabetes Mellitus. NZ Med J. 112:139–141.
1999.
|
|
23
|
Weng WL: Clinical significance and
existing problems of hemorrheology. Zhong Guo Wei Xun Huan.
6:52002.(In Chinese).
|
|
24
|
Lv XF, Meng QY and Guo XM: Effect of
Rehmannia glutinosa water extraction on insulin resistance
and gene expression of resistin in type 2 diabetes mellitus rats.
Zhong Guo Zhong Yao Za Zhi. 32:2182–2184. 2007.(In Chinese).
|
|
25
|
Lee MS and Sohn CB: Anti-diabetic
properties of chrysophanol and its glucoside from rhubarb rhizome.
Biol Pharm Bull. 31:2154–2157. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Koya D, Haneda M, Nakagawa H, et al:
Amelioration of accelerated diabetic mesangial expansion by
treatment with a PKC beta inhibitor in diabetic db/db mice, a
rodent model for type 2 diabetes. FASEB J. 14:439–447.
2000.PubMed/NCBI
|
|
27
|
Schnackenberg CG and Wilcox CS: The SOD
mimetic tempol restores vasodilation in afferent arterioles of
experimental diabetes. Kidney Int. 59:1859–1864. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Berg TJ, Bangstad HJ, Torjesen PA, Osterby
R, Bucala R and Hanssen KF: Advanced glycation end products in
serum predict changes in the kidney morphology of patients with
insulin-dependent diabetes mellitus. Metabolism. 46:661–665. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Berg TJ, Snorgaard O, Faber J, et al:
Serum levels of advanced glycation end products are associated with
left ventricular diastolic function in patients with type 1
diabetes. Diabetes Care. 22:1186–1190. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bolton WK, Cattran DC, Williams ME, et al:
Randomized trial of an inhibitor of formation of advanced glycation
end products in diabetic nephropathy. Am J Nephrol. 24:32–40. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Forbes JM, Cooper ME, Thallas V, et al:
Reduction of the accumulation of advanced glycation end products by
ACE inhibition in experimental diabetic nephropathy. Diabetes.
51:3274–3282. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yin X, Zhang Y, Wu H, et al: Protective
effects of Astragalus saponin I on early stage of diabetic
nephropathy in rats. J Pharmacol Sci. 95:256–266. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Gu J, Zhang H, Chen L, Xu S, Yuan G and Xu
X: Drug-target network and polypharmacology studies of a
Traditional Chinese Medicine for type II diabetes mellitus. Comput
Biol Chem. 35:293–297. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ji L, Tong X, Wang H, et al:
Evidence-Based Medical Research of Xiaoke Pill Study Group:
Efficacy and safety of traditional chinese medicine for diabetes: A
double-blind, randomised, controlled trial. PLoS One. 8:e567032013.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tong XL, Dong L, Chen L and Zhen Z:
Treatment of diabetes using traditional Chinese medicine: Past,
present and future. Am J Chin Med. 40:877–886. 2012. View Article : Google Scholar : PubMed/NCBI
|