Introduction
Superior mesenteric artery syndrome (SMAS), also
known as Wilkie's syndrome, was first reported by Rokitansky in
1842 (1). It is defined as a
compression of the third part of duodenum by the superior
mesenteric artery (SMA). Numerous risk factors can lead to SMAS,
including weight loss, spasticity, prolonged recumbency and severe
traumatic brain injury (2). Although
SMAS frequently occurs after traumatic brain injury, no cases of
SMAS following brain surgery and cranial radiation have been
reported. To increase awareness of this rare treatable effect of
neurosurgery, the case of a patient who developed SMAS following
cerebellar tumor resection and cranial irradiation is described in
the present study.
Case report
In March 2013, a 21-year-old woman underwent brain
surgery following the diagnosis of neuroglioma at Jiangsu
Provincial People's Hospital (Nanjing, China). The patient was also
received Gamma Knife treatment (local brain radiotherapy)
postoperatively, which stabilized her condition for a while. The
patient, who had an unremarkable medical history, was admitted to a
local hospital in May 2014, with a 3-day history of nausea and
vomiting after eating. Symptom relief was achieved 1 week later
following the treatment of influenza. The patient further developed
chronic intermittent abdominal pain, repeatedly with no known
cause. On initial examination, computed tomography (CT) plain and
enhancement scanning of the abdomen showed duodenal stasis. The
patient was given enteral and parenteral nutritional support
treatment for >10 days. However, the patient exhibited no
improvement and on July 13, 2014 was transferred to Jinling
Hospital (Nanjing, China) for continuing management.
On admission to the hospital, the patient was
generally unwell, exhibiting physical decline and loss of appetite.
Clinical examination was unremarkable. The patient had undergone
significant weight loss since the start of the illness (~10 kg),
with a Patient-Generated Subjective Global Assessment (PG-SGA)
classification of grade C and a Nutritional Risk Screening
(NRS)-2002 score of 6. The patient was 1.63 m in height and weighed
34.5 kg, corresponding to a body mass index of 12.99
kg/m2. Her resting energy expenditure (REE) rate was
measured to be 1,229 kcal/day by indirect calorimetry. Levels of
total protein (57.7 g/l), albumin (37.1 g/l) and prealbumin (154
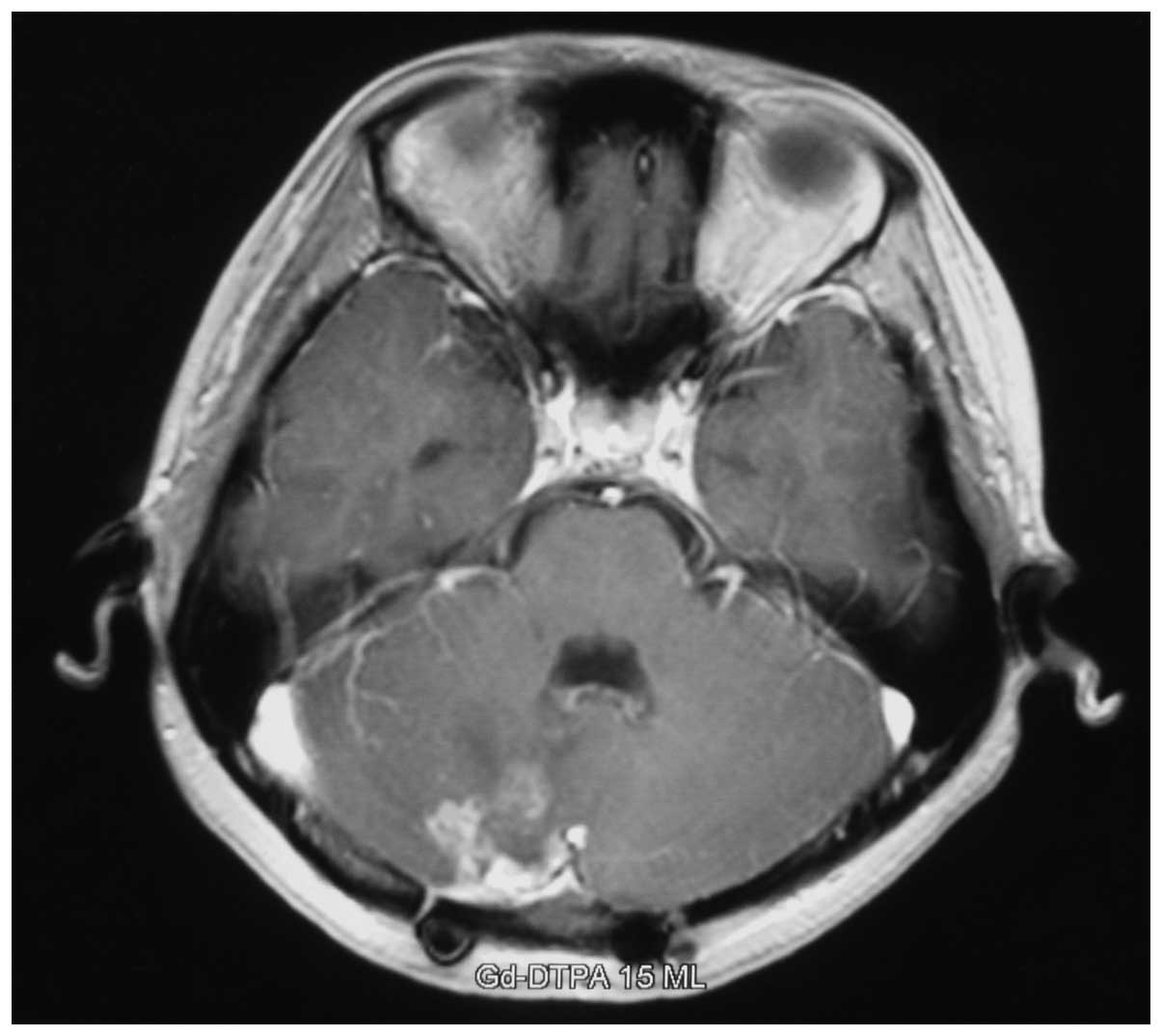
mg/l) were low. The patient underwent magnetic resonance imaging
(MRI) scanning, which revealed an annular focal high-intensity
signal in the region of the right cerebellar hemisphere (Fig. 1). Based on the history of treatment,
tumor recurrence was considered. On July 31, 2014, a CT scan
confirmed compression of the duodenum (Fig. 2), and the diagnosis of SMAS was made
by multidetector computed tomography angiography (CTA; Figs. 3 and 4).
Once the diagnosis of SMAS was established,
treatment with nutrition support was initiated. For this patient,
combined enteral and parenteral nutrition support was the preferred
method. A percutaneous endoscopic gastric jejunum colostomy was
performed for the subsequent management of the patient on August
11, 2014, and a step-by step process was used to enable a gradual
transition to the provision of total enteral nutritional support,
with the aim of inducing the patient to gain weight. The fluid and
electrolyte balance of the patient were also regulated. The patient
was discharged to be cared for by her family on August 18, 2014,
and continued to receive enteral nutritional support. At the last
follow-up 3 months later, the patient's nutritional status had
improved.
Discussion
SMAS is a relatively rare cause of duodenal outlet
obstruction resulting from compression of the third part of the
duodenum between the SMA and the aorta (1,3). In
1982, the prevalence of SMAS in the general population was reported
to be between 0.013 and 0.3% (4). It
has also been reported that SMAS occurs most frequently in older
children and young adults, with a higher incidence in females
(5,6).
There are numerous potential causes of SMAS,
including congenital and acquired factors. Congenital factors are
mainly anatomical anomalies, such as a low take-off position of the
SMA and an abnormally high origin of the ligament of Treitz
(7). Acquired factors include
numerous severe wasting diseases (such as cancer, trauma or burns),
disorders resulting from malnutrition (such as malabsorption or
anorexia nervosa) and prolonged vomiting (2). It is worthy of note that the
postoperative state is also a common cause of SMAS. A study in 2012
reported a case of SMAS resulting from minimally invasive
correction of pectus excavatum (8),
which implies that postoperative malnutrition resulting from
non-abdominal surgery may be a potential cause of SMAS. In
neurosurgery, postoperative malnutrition and vomiting are very
common following brain tumor surgery. In 2008, Bhattacharya et
al described the case of a 3-year-old female child with
pilocytic astrocytoma who had persistent vomiting following
neurosurgical procedures for posterior fossa astrocytoma; during
the recovery period, the patient was diagnosed with SMAS (9). As early as in the 1990s, certain
scholars had observed that severe traumatic brain injury is a cause
of SMAS (2,10). Brain injury and brain surgery
frequently present the same symptoms; managements such as
craniotomy, tumor resection and radiotherapy in patients with brain
tumors are a cause of brain injury. It may be speculated that in
the present patient, a thin younger woman who underwent brain tumor
surgery and radiotherapy, it is likely that prolonged vomiting and
postoperative malnutrition contributed to weight loss, resulting in
the obstruction of the duodenum.
The clinical symptoms of SMAS are usually
nonspecific, and include epigastric pain, bilious vomiting, nausea,
fullness, postprandial bloating and weight loss (3,11). The
diagnosis is mainly based on the history and clinical features and
can be confirmed by radiological examination of the abdomen, for
example, with CT and a barium meal. The angle between the abdominal
aorta and SMA is usually 38–60°, and the normal distance between
those two blood vessels averages 10–28 mm (12). However, the angle between the
abdominal aorta and SMA in patients with SMAS is usually <22°
and the distance between vessels is <8 mm (13,14). The
angle between the abdominal aorta and SMA observed in the CTA scan
of the present patient was ~10°, which also supports the diagnosis
of SMAS. The choice of treatment is usually dependent upon the
cause of SMAS and degree of obstruction. Conservative therapeutic
approaches include nasogastric decompression, hyperalimentation
(15), maintenance of fluid and
electrolyte balance (3) and
nutritional therapy. Surgical procedures are indicated if there is
no response to conservative treatment.
In conclusion, to the best of our knowledge, the
present patient is the first reported case of SMAS in an adult
following neurosurgical surgery and cranial irradiation. In the
present case, a progressive decline in body weight occurred during
the postoperative period following brain tumor surgery, but in the
absence of effective nutritional therapy, weight loss persisted,
finally resulting in the development of SMAS. When prolonged
vomiting and acute weight loss are observed postoperatively in
patients who have undergone brain surgery or cranial irradiation,
neurosurgeons should consider the possibility of SMAS. A
combination of parenteral and enteral nutritional therapy is
recommended.
Acknowledgements
The authors thank Dr Xie Li and her colleagues from
the Department of Radiology of Jinling Hospital for assistance and
suggestions provided in the diagnosis of the patient.
References
|
1
|
Von Rokitansky C: Lehrbuch der
Pathologischen Anatomie. 3. 3rd. Braumüller; Vienna: pp. 871861,
(In German).
|
|
2
|
Pedoto MJ, O'Dell MW, Thrun M and
Hollifield D: Superior mesenteric artery syndrome in traumatic
brain injury: Two cases. Archives Phys Med Rehabil. 76:871–875.
1995. View Article : Google Scholar
|
|
3
|
Roy A, Gisel JJ, Roy V and Bouras EP:
Superior mesenteric artery (Wilkie's) syndrome as a result of
cardiac cachexia. J Gen Intern Med. 20:C3–C4. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Anderson JR, Earnshaw PM and Fraser GM:
Extrinsic compression of the third part of the duodenum. Clin
Radiol. 33:75–81. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Burkhalter JL and Blumenthal BI:
Radiologic seminar CCVIII: Superior mesenteric artery syndrome: A
case report. J Miss State Med Assoc. 21:240–242. 1980.PubMed/NCBI
|
|
6
|
Walsh TN, McPhillips M and O'Higgins N:
Extrinsic compression of the duodenum - Wilkie's syndrome. Ir J Med
Sci. 152:129–133. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Neri S, Signorelli SS, Mondati E,
Pulvirenti D, Campanile E, Di Pino L, Scuderi M, Giustolisi N, Di
Prima P, Mauceri B, et al: Ultrasound imaging in diagnosis of
superior mesenteric artery syndrome. J Intern Med. 257:346–351.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ricca RL, Kasten J and Javid PJ: Superior
mesenteric artery syndrome after minimally invasive correction of
pectus excavatum: Impact of post-operative weight loss. J Pediatr
Surg. 47:2137–2139. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bhattacharya D, Kamel M and McAuley D:
Superior mesenteric artery syndrome (Wilkie's syndrome)
complicating recovery from posterior fossa surgery in a child - a
rare phenomenon. Childs Nerv Syst. 24:365–367. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Philip PA: Superior mesenteric artery
syndrome: An unusual cause of intestinal obstruction in
brain-injured children. Brain Inj. 6:351–358. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Payawal JH, Cohen AJ and Stamos MJ:
Superior mesenteric artery syndrome involving the duodenum and
jejunum. Emerg Radiol. 10:273–275. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ozkurt H, Cenker MM, Bas N, Erturk SM and
Basak M: Measurement of the distance and angle between the aorta
and superior mesenteric artery: Normal values in different BMI
categories. Surg Radiol Anat. 29:595–599. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Unal B, Aktas A, Kemal G, Bilgili Y,
Güliter S, Daphan C and Aydinuraz K: Superior mesenteric artery
syndrome: CT and ultrasonography findings. Diagn Interv Radiol.
11:90–95. 2005.PubMed/NCBI
|
|
14
|
Sabbagh C, Santin E, Potier A and
Regimbeau JM: The superior mesenteric artery syndrome: A rare
etiology for proximal obstructive syndrome. J Vis Surg.
149:428–429. 2012. View Article : Google Scholar
|
|
15
|
Munns SW, Morrissy RT, Golladay ES and
McKenzie CN: Hyperalimentation for superior mesenteric-artery
(cast) syndrome following correction of spinal deformity. J Bone
Joint Surg Am. 66:1175–1177. 1984.PubMed/NCBI
|