Introduction
Multiple myeloma (MM) is a malignancy that is
characterized by the proliferation of clonal plasma cells and the
overproduction of structurally homogeneous immunoglobulins. The
disease comprises ~1% of all malignant diseases and 10% of
hematological malignancies (1). MM
is most commonly observed in elderly individuals, with a median age
at diagnosis of 65 years (2).
Furthermore, the increase in the median age at diagnosis in western
countries has resulted in an increase in the incidence of this
disease. However, the etiology of MM remains unclear (3). MM is most frequently restricted to the
bone marrow; however, there is a subset of patients with
extramedullary disease in whom pathogenic plasma cells are located
at distant anatomical sites, including the liver, kidney, pleura,
breast, testes, skin and meninges. Synthetically, extramedullary
multiple myeloma (EMM) is a type of MM that is defined by the
presence of extraskeletal (soft tissue or visceral) clonal plasma
cell infiltrates (4). EMM may be
present at the point of the initial diagnosis (primary EMM) or at
the time of relapse (secondary EMM) (5), and is typically associated with an
unfavorable prognosis relative to MM with marrow-only disease.
Although plain radiographs of the skeleton, positron emission
tomography (PET), computed tomography (CT) and magnetic resonance
imaging (MRI) are used currently in patients with MM and EMM for
the detection of disease extension, none of the radiological
features of the various imaging techniques are specific for EMM.
Thus, a needle biopsy is mandatory to achieve a confirmed
diagnosis. Although extramedullary lesions may present with other
clinical factors at the time of diagnosis, the onset of a solid
formation as a first clinical feature of MM is unusual.
Case report
A 77-year-old Caucasian male with no history of
trauma was admitted to the Hematology Unit of the National Cancer
Research Center of the Istituto Tumori ‘Giovanni Paolo II’ hospital
(Bari, Italy) in June 2013 with a painful mass protruding from the
right side of his lower back. The patient reported that the mass
had been growing incrementally. Physical examination revealed a
solid, non-tender mass that was localized in the upper region of
the pelvis. The mass was fixed and not reducible with manual
compression. The renal function of the patient, in addition to the
levels of electrolytes (sodium, potassium and calcium) and the
hemoglobin level, were all normal. However, serum electrophoresis
revealed an increase in β-globulin, and serum immunofixation
analysis indicated positivity for IgA-κ (1.19 g/dl); Bence Jones
proteinuria was positive for monoclonal light κ chains. M-protein
is known to be present in numerous diseases (hematological or
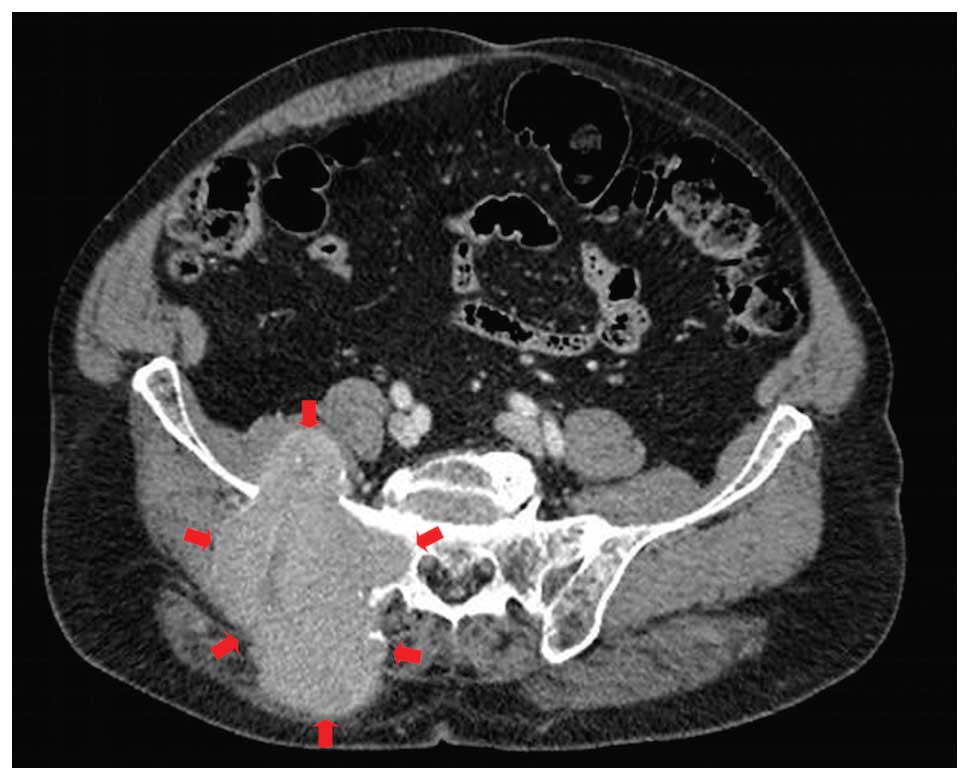
other) encountered in clinical practice. CT examinations of the
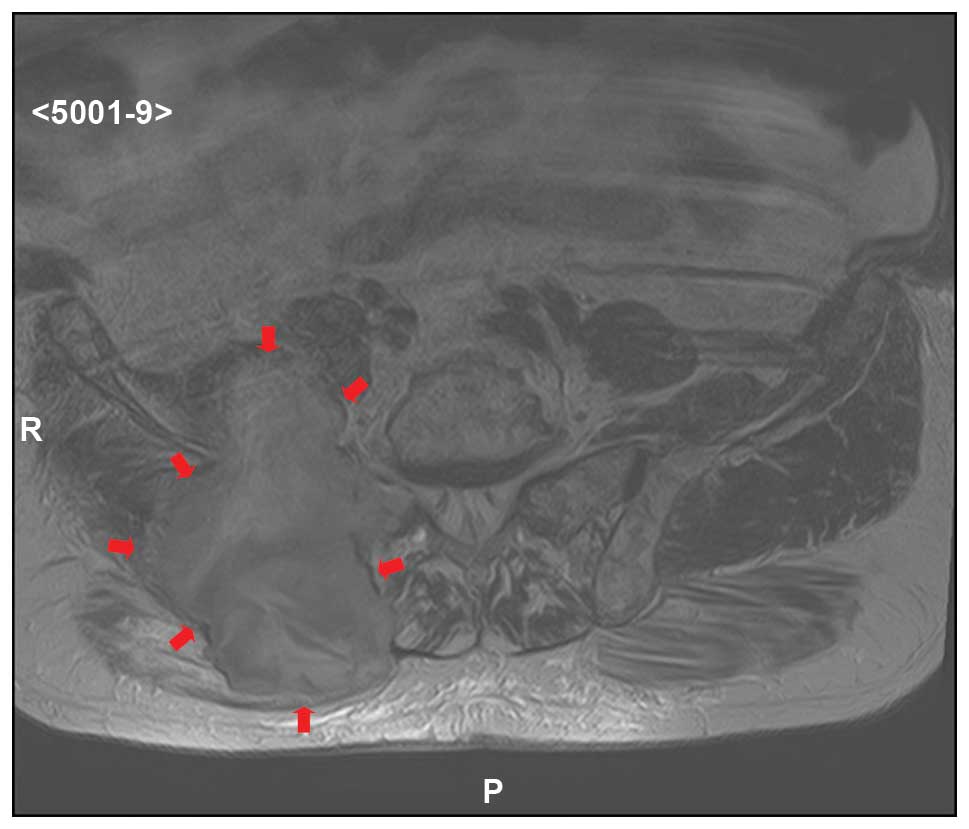
abdomen (Figs. 1 and 2, arrows), which were confirmed by MRI
(Fig. 3, arrows), revealed a
voluminous solid formation with a maximum dimension of 9.3×12 cm in
the area of the right large and medium gluteal muscles, which
extended partially into the small gluteal muscle. Contrast medium
highlighted limited areas of colliquative necrosis. In addition,
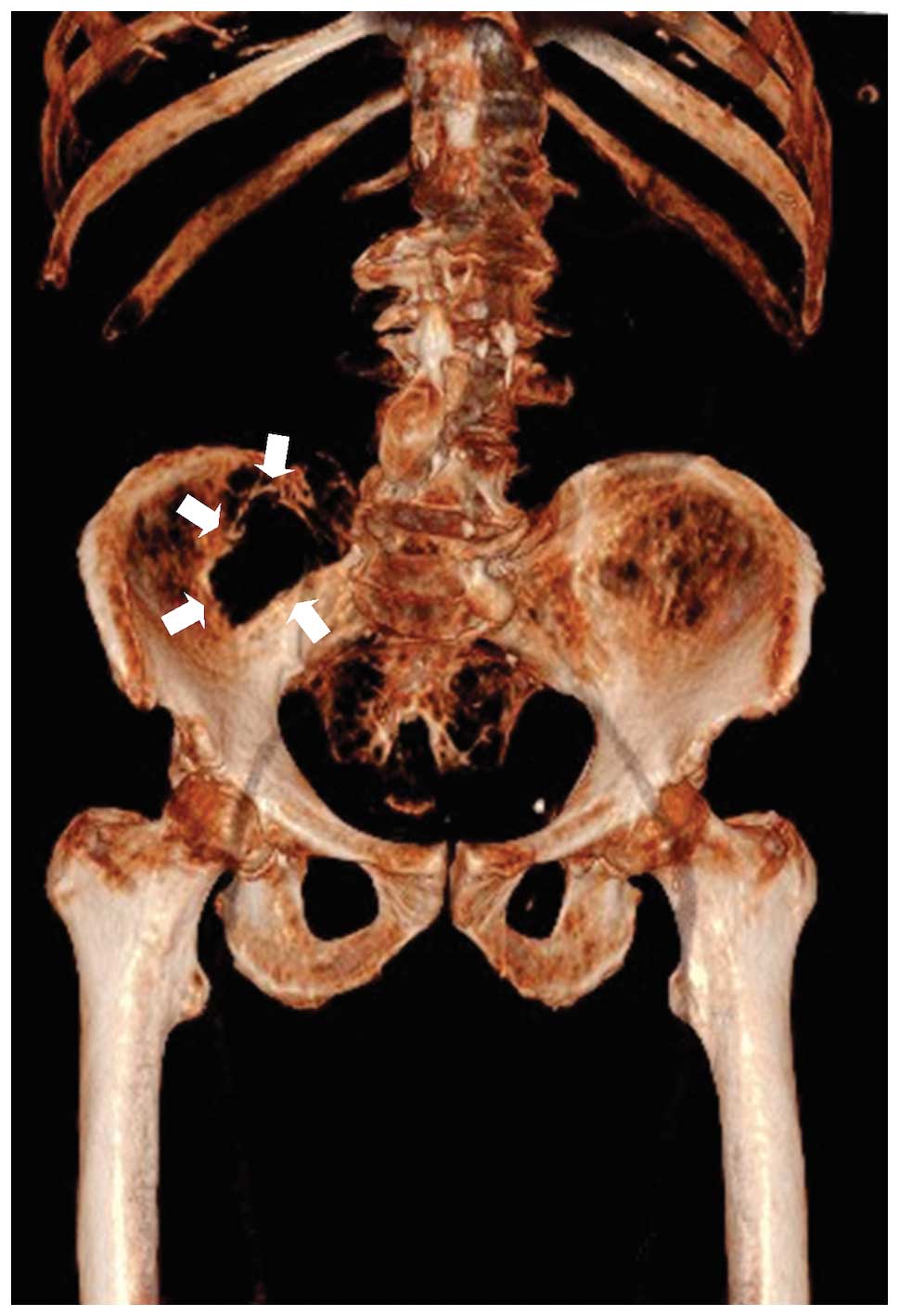
erosion of the right iliac wing, as a result of the solid
formation, was clearly evident in a three-dimensional CT
reconstruction of the bone (Fig. 4,
arrows), and the iliac muscle was also shown to be involved.
Furthermore, the solid formation was observed to result in the
erosion of the sacrum and spinal muscles on the same side. These
imaging features led to a hypothesis of a sarcoma. With the
exception of the sacrum and right iliac wing, no other bone lesion
was evident during the skeletal survey. A Tru-Cut biopsy of the
lesions was performed, which revealed an infiltration of plasma
cells (CD38+, CD138+ and κ
chains+). In addition, a bone marrow biopsy revealed the
presence of 70% plasma cells (CD38+, CD138+
and κ chains+). Fluorescence in situ
hybridization analysis was performed on the marrow cells, and
revealed monosomy of chromosome 13. Therefore, a diagnosis of
primary EMM was established and the patient underwent nine 6-week
cycles of treatment with melphalan (9 mg per square meter of
body-surface area) and prednisone (60 mg per square meter) on days
1–4. In addition, the patient received bortezomib (1.3 mg per
square meter) on days 1, 8, 22 and 29 during cycles 1–9. After nine
cycles of therapy a reduction of M-protein of 80% and of solid
formation of 40% was observed. Written informed patient consent was
obtained.
Discussion
MM is a plasma cell neoplasm that is associated with
the presence of M-protein in the serum and/or urine, which can be
detected by electrophoresis. The diagnosis of MM requires the
presence of ≥10% bone marrow clonal plasma cells of nucleated cells
in the marrow or the plasmacytoma (6). Distinguishing between asymptomatic
(smoldering) MM and symptomatic MM is possible, since the latter is
defined by the presence of end-organ damage (hypercalcemia, renal
insufficiency, anemia and bone lesions). In order of frequency, the
clinical features of MM are lytic bone lesions (>80%), anemia
(75–80%), bone pain (65–75%), fatigue (35–45%), an increase in the
serum creatinine level (25–30%) and hypercalcemia (15–20%).
Therefore, a conclusive evaluation is based on a combination of
pathological, radiological and clinical features.
Extraskeletal clonal plasma cell infiltrates may be
present at the time of the initial diagnosis (primary EMM);
however, the onset of a solid formation as a first clinical feature
of MM is unusual.
Clinically, three types of EMM can be described: i)
Tumor mass adjacent to the bone and extending into the soft
tissues; ii) soft tissue or visceral tumor that is not connected to
the bone; or iii) diffuse infiltration of organs by plasma cells
without any evident focal lesion (7). However, the majority of studies do not
discriminate among these three types of EMM lesions (7). Primary EMM is identified in 4–16% of MM
patients at the time of diagnosis, while secondary EMM is found in
6–20% of patients during the further disease course of MM (8). However, the precise pathogenic
mechanisms that contribute to the extramedullary spread of clonal
plasma cells remain poorly understood. In addition, the prognosis
of EMM patients is generally poor, and an effective treatment
strategy is yet to be established (9).
Various imaging techniques are used currently in
patients with MM and EMM for the detection of disease extension. A
traditional skeletal survey forms part of the standard of care for
the staging and follow-up of bone lesions in patients with MM
(10), and enables the
identification of osteolytic lesions. In addition, CT examinations
are commonly used to visualize the areas that are unable to be
observed well on conventional radiographs, and may also be used to
characterize soft tissue involvement (11). However, CT observations for MM are
non-specific; thus, CT examinations may be used to guide a needle
biopsy for histological diagnosis.
MRI has been demonstrated to have a high sensitivity
and specificity for the detection of diffuse and focal forms of MM
in the spine and extra-axial skeleton (12). In T1-weighted imaging, bone myeloma
lesions appear hypointense, while the lesions are visualized as
hyperintense on T2-weighted imaging. Furthermore, bone myeloma
lesions appear hyperintense in short T1 inversion recovery imaging
and enhanced on post-contrast T1 sequences (11). PET is a non-invasive functional
imaging technique that enables whole-body screening in a single
procedure. PET imaging is sensitive for the detection of early bone
marrow involvement, prior to any identifiable bone changes
(13).
In conclusion, all the imaging techniques discussed
are useful for the detection of an extension of MM; however, none
of the radiological features of the various imaging techniques are
specific for EMM. Thus, a needle biopsy is mandatory to achieve a
confirmed diagnosis. The occurrence of a mass as an initial symptom
in MM is uncommon, and may result in a delayed diagnosis. In
addition, considering that M-protein is present in numerous
conditions encountered in clinical practice, there are no specific
radiological features of EMM, and EMM can resemble other neoplasms,
including sarcoma, EMM should be included in the differential
diagnosis of a mass, particularly in patients where M-protein is
detected in the blood and/or urine.
Acknowledgements
The authors thank Ms. Caroline Oakley for revision
of the language in the manuscript and Luca Leone for cooperation in
the selection of the images.
Glossary
Abbreviations
Abbreviations:
|
MM
|
multiple myeloma
|
|
EMM
|
extramedullary multiple myeloma
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
PET
|
positron emission tomography
|
References
|
1
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics. 2010.CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Vincent Rajkumar S: Treatment of multiple
myeloma. Nat Rev Clin Oncol. 8:479–491. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Harousseau JL, Shaughnessy J Jr and
Richardson P: Multiple myeloma. Hematology Am Soc Hematol Educ
Program. 237–256. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Weber DM: Solitary bone and extramedullary
plasmacytoma. Hematology Am Soc Hematol Educ Program. 373–376.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Usmani SZ, Heuck C, Mitchell A, Szymonifka
J, Nair B, Hoering A, Alsayed Y, Waheed S, Haider S, Restrepo A, et
al: Extramedullary disease portends poor prognosis in multiple
myeloma and is over-represented in high-risk disease even in the
era of novel agents. Haematologica. 97:1761–1767. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vincent Rajkumar S: Multiple myeloma: 2014
Update on diagnosis, risk-stratification, and management. Am J
Hematol. 89:999–1009. 2014.PubMed/NCBI
|
|
7
|
Pour L, Sevcikova S, Greslikova H, Kupska
R, Majkova P, Zahradova L, Sandecka V, Adam Z, Krejci M, Kuglik P,
et al: Soft-tissue extramedullary multiple myeloma prognosis is
significantly worse in comparison to bone-related extramedullary
relapse. Haematologica. 99:360–364. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Oriol A: Multiple myeloma with
extramedullary disease. Adv Ther. 28(Suppl 7): 1–6. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Varettoni M, Corso A, Pica G,
Mangiacavalli S, Pascutto C and Lazzarino M: Incidence, presenting
features and outcome of extramedullary disease in multiple myeloma:
A longitudinal study on 1003 consecutive patients. Ann Oncol.
21:325–330. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
International Myeloma Working Group:
Criteria for the classification of monoclonal gammopathies,
multiple myeloma and related disorders: A report of the
International Myeloma Working Group. Br J Haematol. 121:749–757.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mena E, Choyke P, Tan E, Landgren O and
Kurdziel K: Molecular imaging in myeloma precursor disease. Semin
Hematol. 48:22–31. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ghanem N, Lohrmann C, Engelhard M, Pache
G, Uhl M, Saueressig U, Kotter E and Langer M: Whole-body MRI in
the detection of bone marrow infiltration in patients with plasma
cell neoplasms in comparison to the radiological skeletal survey.
Eur Radiol. 16:1005–1014. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Durie BG, Waxman AD, DAgolo A and Williams
CM: Whole-body (18)F-FDG PET identifies high-risk myeloma. J Nucl
Med. 43:1457–1463. 2002.PubMed/NCBI
|