Introduction
Pneumonia is a lung infection caused by a variety of
germs, including viruses, bacteria, fungi and parasites (1). Symptoms of pneumonia vary depending on
child's age and the cause of the pneumonia. The main symptoms
include sore throat, headache, cough and fever (1,2).
Pneumonia is a major infectious disease responsible for significant
morbidity and mortality worldwide.
Pneumonia caused by mycoplasma bacteria is a less
serious form of infection (3). The
child's secretion sputum is contagious and spreads easily in
children. Mycoplasma pneumonia (MP) is a form of atypical bacterial
pneumonia that damages several organs and systems through local
infection of the respiratory tract. It was extensively spread in
children with an increasing morbidity and is rapidly developing
into a prevalent disease (4–6).
A chest X-ray is the optimal option for diagnosing
pneumonia. However, this test may not be ideal to identify the
cause of pneumonia. Clinical tests are not considered significant,
therefore a lung computed tomography (CT) scan was necessary for
the early diagnosis of the disease (7).
The diagnosis of pediatric pneumonia should be
performed based on the major clinical manifestations and
corresponding CT examination of the children. The present study
prospectively analyzed the clinical data of 1,280 children to
assess the diagnostic value of CT examination in pediatric MP.
Gaining understanding of the children's characteristic imaging data
was beneficial to the clinical diagnosis and treatment of pediatric
MP.
Materials and methods
General information
The current study included 1,280 children (680 males
and 600 females) with pediatric MP in the out- and inpatient
departments from March, 2010 to March, 2014. The age range of the
patients was 3 months to 10 years, with a mean age of 4.3±1.8
years, while the range of disease course was 3–15 days, with a mean
course of 8.9±2.1 days. The clinical manifestations of all the
patients were paroxysmal cough and irritating cough. Most children
were complicated with fever, expectoration, chest stuffiness, and
pharyngolaryngitis to varying degrees. All the children met the
diagnostic criteria of pediatric MP in practical pediatrics
(8). The study was approved by the
Ethics Committee of Xuzhou Children's Hospital (Jiangsu,
China).
Inclusion criteria
Inclusion criteria for the study were: i) Age range
3 months to 12 years (6); ii) major
clinical manifestations meeting the clinical diagnostic criteria,
including cough, fever, loss of appetite, and moist rales in the
lung; iii) disease course of 4–15 days; iv) having signed informed
consent with the agreement of guardians and v) exclusion of
children with bronchitis, asthma, and respiratory infection due to
cold (9).
Examination methods
Whole lung scanning was performed from apex pulmonis
to basis pulmonis with a Philips Brilliance 16-slice spiral CT
(Philips Healthcare, DA Best, The Netherlands). The slice width and
spacing were 5 mm, the pitch was 1.20, and the scanning time was
1.0 sec. The voltage was maintained at 120 kV, the constant at
80–160 mA, the mediastinal window was W450:L45, and the lung window
was W1,000:L2,500. The vertical and coronal planes of the lesion
were reconstructed spontaneously. CT scan with contrast was
performed after the plain scan and the scan parameters were the
same as with those of the plain scan. The contrast agent was
iohexol, which was injected by a high-pressure injector at a rate
of 1.5–3 ml/sec. The mean CT value of the margin and interior of
the lesion was calculated. Children with poor compliance were
orally administered with 3% chloral hydrate (1.5 ml/kg). Children
requiring special care completed the examinations with the
accompaniment of his/her parents'/guardians (10).
CT images
The location, size, shape, density, distribution,
internal structure, margin of the lesion, pleural effusion, hilar
lymph nodes and mediastinal lymph nodes from the lung and
mediastinal window were observed. The imaging data of the lesion,
lesion site, its adjacent tissue and organ lesions obtained from
all the CT examinations were analyzed.
Observational measurements
The lung CT imaging data of all the children were
observed. The number of lobe lesions, including the lesions in the
unilateral and bilateral lobes, the number of lesions in the left
and right lobes and the main imaging features of the lesion lobes
were recorded (11).
Results
Analysis of the lung CT imaging data
of the children
As shown in Table I,
of all the children, there were 688 cases of unilateral lobe
lesions, 592 cases of bilateral lobe lesions, including 338 cases
of left upper lobe lesions, 416 cases of left lower lobe lesions,
370 cases of right upper lobe lesions, 240 cases of left middle
lobe lesions, and 435 cases of right lower lobe lesions. The
lesions were predominantly extensive patchy opacity, mottled
opacity, increased lung marking, streak opacity and ground-glass
opacity. In addition, there were 992 cases of thickened bronchial
wall in the lesions, 128 cases of lymphadenopathy in hilar lymph
nodes and mediastinal lymph nodes, and lung CT showed 32 cases of
pulmonary cavity and 144 cases of pleural effusion.
 | Table I.The analysis of the lung CT imaging
data of the children (no., %) |
Table I.
The analysis of the lung CT imaging
data of the children (no., %)
| Characteristics | No. (%) |
|---|
| Lesion
distribution |
|
| Lesion in
unilateral lobe | 688 (53.8) |
| Right
upper lobe | 370 (28.9) |
| Right
middle lobe | 240 (18.8) |
| Right
lower lobe | 435 (34.0) |
| Left
upper lobe | 338 (26.4) |
| Left
lower lobe | 416 (32.5) |
| Lesions
in bilateral lobes | 592 (46.3) |
| Features of the CT
imaging of the lesions |
|
| Extensive
patchy opacity | 1,101 (86.0) |
| Mottled
opacity | 496 (38.8) |
| Increased
lung marking | 432 (33.8) |
| Streak
opacity | 256 (20.0) |
|
Ground-glass opacity | 192 (15.0) |
| Other lung
manifestations |
|
| Thickened
bronchial wall | 992 (77.5) |
| Hilar and
mediastinal lymphadenopathy | 128 (10.0) |
| Pulmonary
cavity | 32 (2.5) |
| Pleural
effusion | 144 (11.3) |
The analysis of imaging features
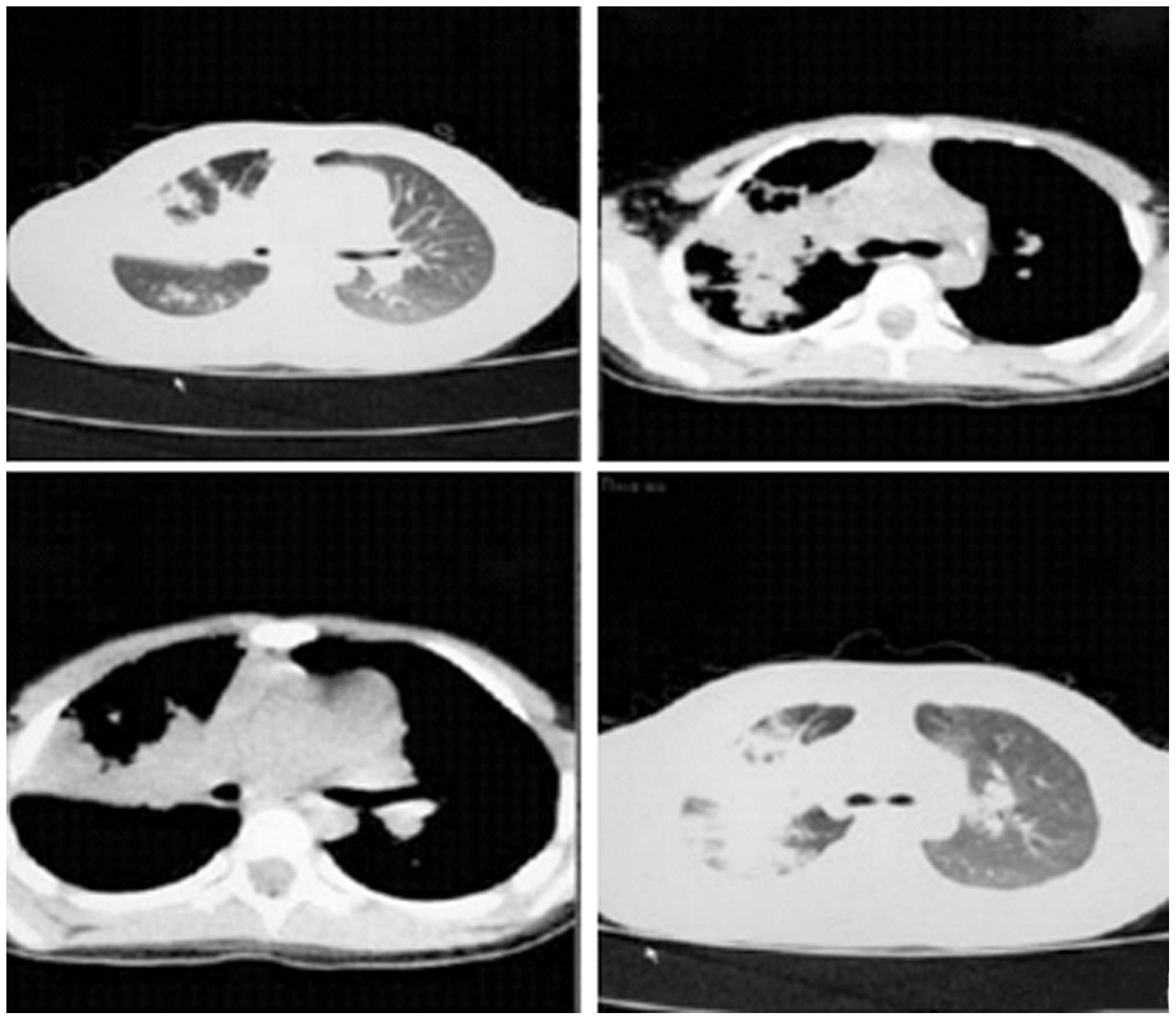
In a case involving a female child ages 5-years and
11 months old, who was hospitalized due to fever and cough for 4
days, the diagnosis was bilateral pneumonia and predominantly
pneumonia in the upper lobe of the right lung. As shown in Fig. 1, the major imaging features included
extensive high-density opacity in the upper lobe of the right lung,
with the sign of bronchial inflation, less uniform lesion density,
blurry boundary and slight thickening of the adjacent pleura,
flocculent opacity and small patchy opacity in the lower lobe of
the right lung. Increased vascular bundles in the bilateral bronchi
were observed albeit they were blurry. Trachea and bilateral
primary bronchi were unobstructed. No obvious density was
identified in the mediastinum, a thymus shadow was observed in the
anterior superior mediastinum, no obvious abnormal shape and size
of the heart shadow was identified and no clear free liquid was
evident in the bilateral thoracic cavities. No obvious abnormality
in the bilateral thoracic spine and ribs was evident, and the
structure of the soft tissue in the chest wall was clear.
Discussion
Pediatric MP is an infective respiratory disease
common in children due to MP (12–14),
accounting for approximately 50% of cases. However, the morbidity
of this disease has been on the increase (15). This disease can damage various organs
and affect the child's normal growth and development. The disease
has a short incubation period with the main symptoms of manifesting
at the early phase of this disease head pain, fever, cough and
pharyngalgia. Pediatric MP is seasonal, occurring primarily in
spring and autumn. The child's secreta such as body fluid and
sputum become contagious. Extensive infection occurs when the
mycoplasma is mutated, and even death may occur when the
disease is severe (16–18).
The X-ray imaging changes were identified as more
significant than those of clinical manifestation (19,20).
X-ray examination showed that at the early phase, the clinical
manifestations of most children were interstitial pneumonia,
increased lung marking, reticular opacity, and uniform blurry
opacity or patchy opacity when the condition was worsened with most
lesions being close to the hilus and predominantly in the lower
lung. Extensive infiltration and solid changes were rare, with some
children having hilar lymphadenopathy, while a few children had
pleural effusion (21). In
comparison with X-ray, CT examination determined bronchitis, mixed
pathological changes, and interstitial pneumonia. Therefore, CT was
usually used for the diagnosis of children. Increasing reports have
focused on the use of CT in the diagnosis of pneumonia. Xinbo
(22) analyzed the CT examinations
of children with pediatric pneumonia and the results indicated that
the lung lesions were predominantly unilateral, the proportion of
solid infiltration lesions was high, and the lung bronchial wall
was thickened while some children had pleural effusion and rare
hilar lymphadenopathy (23,24). In the current study, analysis of the
data indicated that: i) the CT imaging of pediatric MP was a mainly
unilateral lesion (53.8%), and secondly bilateral lesion (46.3%).
Thus, bilateral lesions were more prevalent with the lesion in the
lower lobe being mostly prevalent in all parts of the lung (the
incidence of bilateral lesions in the lower lobes was >30.0%.)
ii) The CT imaging of pediatric MP indicated various types of
lesions in the lung tissues, including extensive patchy opacity,
mottled opacity, increased lung marking, streak opacity and
ground-glass opacity, with extensive patchy opacity being the main
lesion, accounting for 86.0% of cases. iii) Analysis of the CT
imaging data of 1,280 children with pediatric MP indicated that the
children had simple pathological lobe lesions as well as
complicated lesions in adjacent intrathoracic organs, predominantly
thickened bronchial wall (77.5%). Other signs were not significant
and only identified in some children, including hilar and
mediastinal lymphadenopathy, pulmonary cavity and pleural effusion.
Therefore, a comprehensive diagnosis should be performed based on
the major clinical manifestations and corresponding CT examinations
of the children with pediatric MP. A differential diagnosis should
be performed with other types of pneumonia to determine the
clinical treatment option, achieve early treatment, improve the
diagnostic and cure rates, and promote early recovery (25,26).
In conclusion, the diagnosis of pediatric MP should
be performed based on the major clinical manifestations and CT
imaging data of the children with pediatric MP to accomplish early
diagnosis and treatment. Understanding of the children's
characteristic imaging data was beneficial to clinical diagnosis
and treatment.
References
|
1
|
Rambaud-Althaus C, Althaus F, Genton B and
D'Acremont V: Clinical features for diagnosis of pneumonia in
children younger than 5 years: A systematic review and
meta-analysis. Lancet Infect Dis. 15:439–450. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
José RJ, Periselneris JN and Brown JS:
Community-acquired pneumonia. Curr Opin Pulm Med. 21:212–218. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Edelstein I, Rachina S, Touati A, Kozlov
R, Henin N, Bébéar C and Pereyre S: Mycoplasma pneumoniae
Monoclonal P1 Type 2c Outbreak, Russia, 2013. Emerg Infect Dis.
22:348–350. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Aydogan P, Kahyaoglu S, Saygan S, Kaymak
O, Mollamahmutoglu L and Danisman N: Does cervical
ureaplasma/mycoplasma colonization increase the lower uterine
segment bleeding risk during cesarean section among patients with
placenta previa? A cross-sectional study. Eur Rev Med Pharmacol
Sci. 18:2243–2247. 2014.PubMed/NCBI
|
|
5
|
Zhifeng M: The difference between the
clinical manifestations of X-ray and CT of pediatric mycoplasma
pneumonia. Chin Healthc Nutr. 24:1153–1154. 2014.
|
|
6
|
Wu SH, Chen XQ, Kong X, Yin PL, Dong L,
Liao PY and Wu JM: Characteristics of respiratory syncytial
virus-induced bronchiolitis co-infection with Mycoplasma
pneumoniae and add-on therapy with montelukast. World J
Pediatr. Apr 6–2015.(Epub ahead of print).
|
|
7
|
Kazama I, Tamada T and Nakajima T:
Macroscopic haemoglobinuria associated with Mycoplasma
pneumoniae infection successfully treated by clarithromycin.
Infez Med. 23:74–78. 2015.PubMed/NCBI
|
|
8
|
Fukang Z, Shiting F, Jingdi C, et al: The
represents of pulmonary tuberculoma and inammatory pseudotumor at
helical dynamic enhanced CT. Chinese Journal of CT and MRI.
9:32–34. 2011.
|
|
9
|
Feng S, Huiquan Y, Hong C, et al: The
analysis of the clinical features and extrapulmonary manifestations
of 60 children with pediatric Mycoplasma pneumonia. Chin
Integr Pediatr. 4:261–263. 2012.
|
|
10
|
Xiangying H, Zhaoding H, Kaimei W, et al:
The analysis of the clinical features and imaging features of 260
children with pediatric Mycoplasma pneumonia. Chin J
Misdiag. 11:5929–5930. 2011.
|
|
11
|
Chung HL, Shin JY, Ju M, Kim WT and Kim
SG: Decreased interleukin-18 response in asthmatic children with
severe Mycoplasma pneumoniae pneumonia. Cytokine.
54:218–221. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hanjun D, Ruimeng Y, Yunhai H, et al: The
exploration of 320 cases of first-pass perfusion imaging CT in the
differentiation of benign and malignant tumor. Chin J CT and MRI.
4:16–17, 44. 2014.
|
|
13
|
Yimenicioğlu S, Yakut A, Ekici A, Carman
Bora K and Cagrı Dinleyici E: Mycoplasma pneumoniae
infection with neurologic complications. Iran J Pediatr.
24:647–651. 2014.PubMed/NCBI
|
|
14
|
Zhuo Z, Li F, Chen X, Jin P, Guo Q and
Wang H: Mycoplasma pneumonia combined with pulmonary
infarction in a child. Int J Clin Exp Med. 8:1482–1486.
2015.PubMed/NCBI
|
|
15
|
Horiba K, Gotoh K, Hattori F, Takeuchi S,
Nishimura N, Ozaki T and Shiraki K: Analysis of 23S rRNA of
Mycoplasma pneumoniae detected from pediatric inpatients
with community-acquired pneumonia in a regional hospital in Japan.
Kansenshogaku Zasshi. 88:715–716. 2014.(In Japanese). PubMed/NCBI
|
|
16
|
Fuchuan W, Peigang N, Tao G, et al: The
multi-slice spiral CT examination of pneumococcal pneumonia. Chin J
CT and MRI. 11:17–19. 2014.
|
|
17
|
Dumke R, Stolz S, Jacobs E and Juretzek T:
Molecular characterization of macrolide resistance of a
Mycoplasma pneumoniae strain that developed during therapy
of a patient with pneumonia. Int J Infect Dis. 29:197–199. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Prindaville B, Newell BD, Nopper AJ and
Horii KA: Mycoplasma pneumonia-associated mucocutaneous
disease in children: dilemmas in classification. Pediatr Dermatol.
31:670–675. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gu L, Chen X, Li H, Qu J, Miao M, Zhou F,
Zhu Y, Wang X, Wang C, Liu Y, et al: A case of lethal hemolytic
anemia associated with severe pneumonia caused by Mycoplasma
pneumoniae. Chin Med J (Engl). 127:38392014.PubMed/NCBI
|
|
20
|
Cheng HH, Tang TT, He Q, Huang LJ, Lin XL,
Chen M, Yang C, Geng DF and Jiang SP: Beneficial effects of statins
on outcomes in pneumonia: a systematic review and meta-analysis.
Eur Rev Med Pharmacol Sci. 18:2294–2305. 2014.PubMed/NCBI
|
|
21
|
Zhou FJ, Zhou CY, Tian YJ, Xiao AJ, Li PL,
Wang YH and Jia JW: Diagnostic value of analysis of H-FABP,
NT-proBNP, and cTnI in heart function in children with congenital
heart disease and pneumonia. Eur Rev Med Pharmacol Sci.
18:1513–1516. 2014.PubMed/NCBI
|
|
22
|
Xinbo Z: The characteristics of the CT
imaging of pediatric mycoplasma pneumonia and the treatments. Chin
Commun Phys Med. 14:233. 2012.
|
|
23
|
Sen V, Kelekci S, Sen Selimoglu H, Yolbas
I, Günes A, Abakay O and Gurkan Fuat M: An evaluation of cases of
pneumonia that occurred secondary to hydrocarbon exposure in
children. Eur Rev Med Pharmacol Sci. 17(Suppl 1): 9–12.
2013.PubMed/NCBI
|
|
24
|
Ucgun I, Dagli CE, Kiremitci A, Yildirim
H, Ak G and Aslan S: Effects of isolation rooms on the prevalence
of hospital acquired pneumonia in a respiratory ICU. Eur Rev Med
Pharmacol Sci. 17(Suppl 1): 2–8. 2013.PubMed/NCBI
|
|
25
|
Kim YH, Kim JE and Hyun MC: Cytokine
response in pediatric patients with pandemic influenza H1N1 2009
virus infection and pneumonia: comparison with pediatric pneumonia
without H1N1 2009 infection. Pediatr Pulmonol. 46:1233–1239. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bruno P, Ricci A, Pezzuto A, Martone L,
Gencarelli G and Mariotta S: Severe pneumonia caused by Nocardia
farcinica and complicated by Staphylococcus haemoliticus
superinfection. Eur Rev Med Pharmacol Sci. 15:401–405.
2011.PubMed/NCBI
|