Introduction
Conjunctivitis is the most common allergic eye
disease and the most frequently observed ocular surface disease in
China (1). According to statistics,
~5% of the global population have sought medical attention due to
an allergic eye disease, 50% of which were cases of conjunctivitis
(1). Recently, in part as a result
of the increased use of eye makeup and the increase of air
pollution in certain regions, the incidence of conjunctivitis has
increased (2).
Conjunctiva is a transparent layer of mucosal
tissue, rich in nerves and blood vessels, that is important for eye
protection and lubrication, serving as the protective film of the
eye (3). Conjunctivitis can be
classified as infectious or non-infectious, with infection taking
precedence as the most common cause (4). Pathogenic microorganisms, including
bacteria (such as chlamydia, rickettsia), viruses, fungi and
parasites (5), are typically
transmitted through air, water, physical contact or via tissue
adjacent to the affected area by inflammation (including the
cornea, eyelid and lacrimal apparatus) (6). Non-infectious conjunctivitis is
typically a result of physical stimuli (namely dust mites, smoke,
dust and ultraviolet light) or chemical stimuli (including
poisonous gas, medical drugs, medical drugs, cosmetics and
shampoos) (7).
Although chronic conjunctivitis displays subjective
symptoms and involves a characteristically slow disease progression
compared with acute conjunctivitis, relapse is common (8). Upon further inspection mild
conjunctival congestion edema, papillary hyperplasia, a small
amount of white mucous or secretions, such as foam samples may be
observed; if not treated promptly, chronic conjunctivitis may
develop into carcinomas able to infiltrate the cornea and affect
vision (9). Therefore, chronic
conjunctivitis requires attention, and further investigation should
be performed to identify its causes, eliminate any responsible
pathogenic factors, and develop the necessary targeted therapies
(10).
Carvedilol is a novel non-selective adrenergic
receptor blocker that displays no inherent sympathetic activity.
Therefore, the drug bypasses the reflexive excitement of the
nervous system often caused by peripheral vascular contraction and
increased peripheral resistance. In addition, carvedilol is an
oxygen free-radical scavenger that regulates cell factors, such as
interleukins and colony stimulating factors, and is involved in a
variety of actions (11,12). However, the effect of carvedilol on
conjunctivitis has rarely been reported. Accordingly, the present
study aimed to evaluate whether the known effects of carvedilol are
able to reduce conjunctivitis clinical scores.
Materials and methods
Animals and modeling
Adult Sprague Dawley (SD) rats (n=24; purchased from
the Animal Experimental Center of Zhejiang University, Zhejiang,
China) weighing 230–300 g were housed in a 12-h light/dark cycle at
a temperature of 22–26°C, and were provided with food and water
ad libitum. The study was approved by the ethics committee
of Zhejiang University School of Medicine (Huangzhou, China). All
SD rats were anesthetized with 75 mg/kg ketamine (injectable
IMALGENE 1000; Merial, Lyon, France) and 10 mg/kg xylazine (Rompun
2%; Beyotime Institute of Biotechnology, Haimen, China) by
intraperitoneal injection (i.p.). Next, each eye of the
anesthetized rats was subconjunctivally injected with 30 µl
lipopolysaccharide (LPS; Sigma-Aldrich Química S.A., Tres Cantos,
Spain). Further treatment of the rats with LPS-induced
conjunctivitis commenced after 24 h.
Study groups
SD rats were randomly divided into three equal
groups: i) Control group, consisting of eight SD rats treated with
1 ml 0.9% NaCl (i.p.) for 4 weeks (i.p.); ii) a model group,
consisting of eight LPS-induced conjunctivitis rats administered
with 1 ml 0.9% NaCl (i.p.) for 4 weeks; and iii) the carvedilol
treatment group, consisting of eight LPS-induced conjunctivitis
rats treated with 50 mg/kg/day carvedilol (i.p.; Sigma-Aldrich, St.
Louis, MO, USA) for 4 weeks.
Evaluation of clinical sign
scores
Prior to the euthanasia of the SD rats, clinical
sign scores were graded by three blind independent evaluators, as
previously reported (13). The
clinical score signs were recorded prior to induction of
conjunctivitis, and 1, 2, 3 and 4 weeks after carvedilol
administration. Clinical sign scores were obtained by three blind
independent observers according to previously described criteria
(14).
Evaluation of interleukin (IL)-1β,
IL-6, IL-8 and tumor necrosis factor-α (TNF-α) with enzyme-linked
immunosorbent assay (ELISA)
After 4 weeks of treatment with carvedilol, rats
were sacrificed by cervical dislocation. Then, peripheral blood was
collected from the eye sockets of the rats. Blood samples were
centrifuged at 3,000 × g for 20 min, and the supernatant was
collected and stored at −80°C for further assessment. IL-1β
(ml028611), IL-6 (ml002828), IL-8 (ml027376) and TNF-α (ml002859)
expression levels were measured using ELISA, according to the
manufacturer's protocol (Shanghai Boya Biotechnology Co., Ltd.,
Shanghai, China).
Evaluation of nuclear factor-κB
(NF-κB), nerve growth factor (NGF) and vascular endothelial growth
factor (VEGF) expression levels with western blotting. After 4
weeks of treatment with carvedilol, rats were sacrificed by
cervical dislocation
Then, conjunctivitis tissue samples were collected
and homogenized in modified RIPA buffer (pH 7.4; Beyotime Institute
of Biotechnology). Cytosolic protein samples were centrifuged at
12,000 × g for 10 min at 4°C and the supernatant was collected.
Protein concentration was determined using a BCA assay kit
(Shanghai Boya Biotechnology Co., Ltd.) and equal quantities of
protein were separated by 10% sodium dodecyl sulfate-polyacrylamide
gel electrophoresis at room temperature, then transferred by
electroblotting to nitrocellulose membranes (Hybond-C Extra; GE
Healthcare Life Sciences, Pittsburgh, PA, USA). The nitrocellulose
membranes were blocked in blocking buffer (Tris-buffered saline and
0.1% Tween-20; Beijing Biosntech Biotechnology Co., Ltd., Beijing,
China) containing 5% skim milk, incubated with polyclonal rabbit
anti-NF-κB (1:500; sc-7151), polyclonal rabbit anti-NGF (1:2,000;
sc-33602) and polyclonal rabbit anti-VEGF (1:1,000; sc-507) (all
purchased from Santa Cruz Biotechnology Inc., Dallas, TX, USA)
antibodies, washed and then incubated with horseradish
peroxidase-conjugated secondary antibody (1:3,000; sc-45101; Santa
Cruz Biotechnology Inc.). The resultant bands were visualized by
chemiluminescent detection (ECL Western Blotting Detection Reagent;
GE Healthcare, Chalfont, UK) and analyzed using a computer imaging
system (GDS-8000 Image Acquisition and Analysis System; UVP, LLC,
Upland, CA, USA). The reactions were repeated 3 times.
Statistical analysis
All results are expressed as the mean ± standard
deviation, and analysis was performed using two-way analysis of
variance on the computer program SPSS (version 18.0; SPSS, Inc.,
Chicago, IL, USA). A value of P<0.05 was considered to indicate
a statistically significant difference.
Results
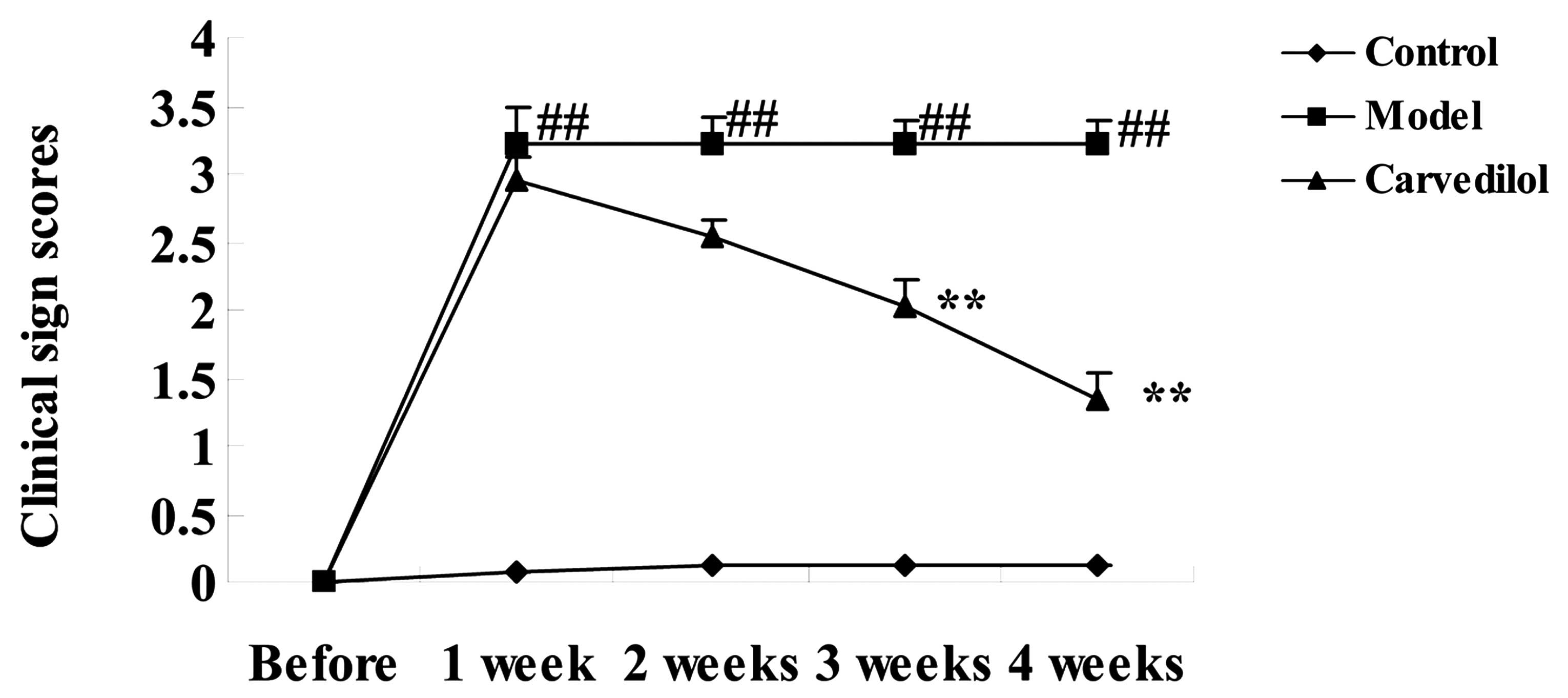
Effects of carvedilol on clinical sign
scores in conjunctivitis rat models
The chemical structure of carvedilol is displayed in
Fig. 1. The effects of carvedilol on
clinical sign scores was examined. LPS significantly increased
clinical sign scores in the conjunctivitis rat model group compared
with the control group (P<0.01). By contrast, carvedilol
significantly blocked the increase of clinical sign scores compared
with the model group in a time-dependent manner (P<0.01;
Fig. 2).
Effects of carvedilol on IL-1β, IL-6,
IL-8 and TNF-α expression levels in conjunctivitis rat models
To evaluate the effects of carvedilol on
inflammation, IL-1β, IL-6, IL-8 and TNF-α expression levels were
analyzed by ELISA. As displayed in Fig.
3, IL-1β (Fig. 3A), IL-6
(Fig. 3B), IL-8 (Fig. 3C) and TNF-α (Fig. 3D) levels were significantly increased
in the conjunctivitis rat model compared with the control group
(P<0.01). Treatment with carvedilol significantly reduced the
augmented expression of all these inflammatory factors compared
with the conjunctivitis model group (P<0.01; Fig. 3).
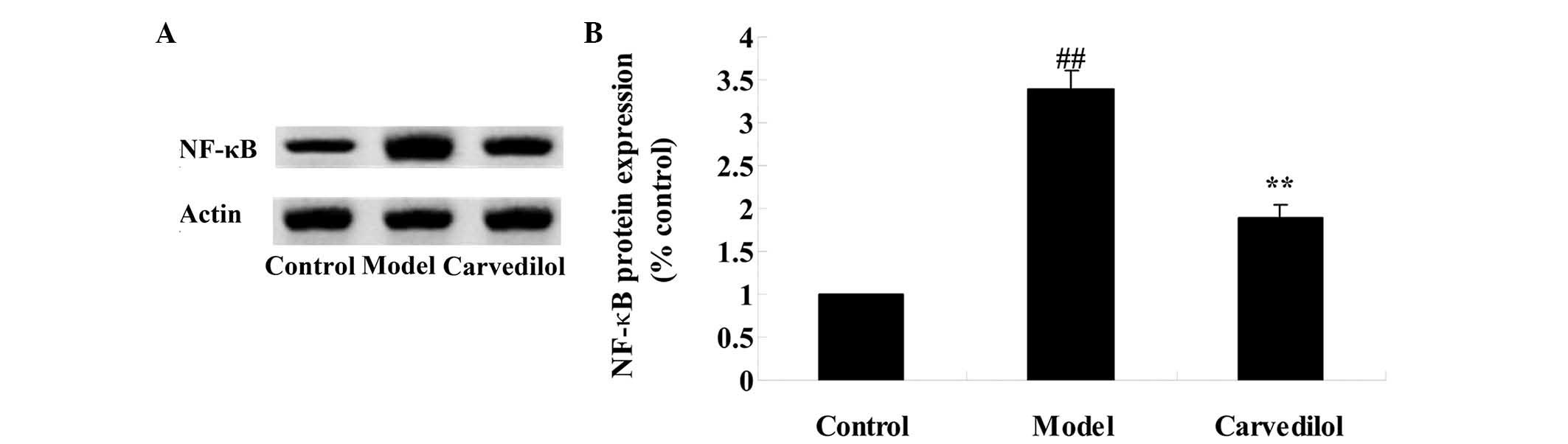
Effects of carvedilol on NF-κB
expression in conjunctivitis rat models
To determine the effects of carvedilol on NF-κB
protein expression levels in conjunctivitis rat models, western
blotting (Fig. 4A) and statistical
analysis of the blots (Fig. 4B) was
performed. The results revealed significantly increased protein
expression levels of NF-κB in the conjunctivitis rat model compared
with the control group (P<0.01). However, treatment with
carvedilol significantly suppressed NF-κB protein expression levels
compared with the model group (P<0.01; Fig. 4).
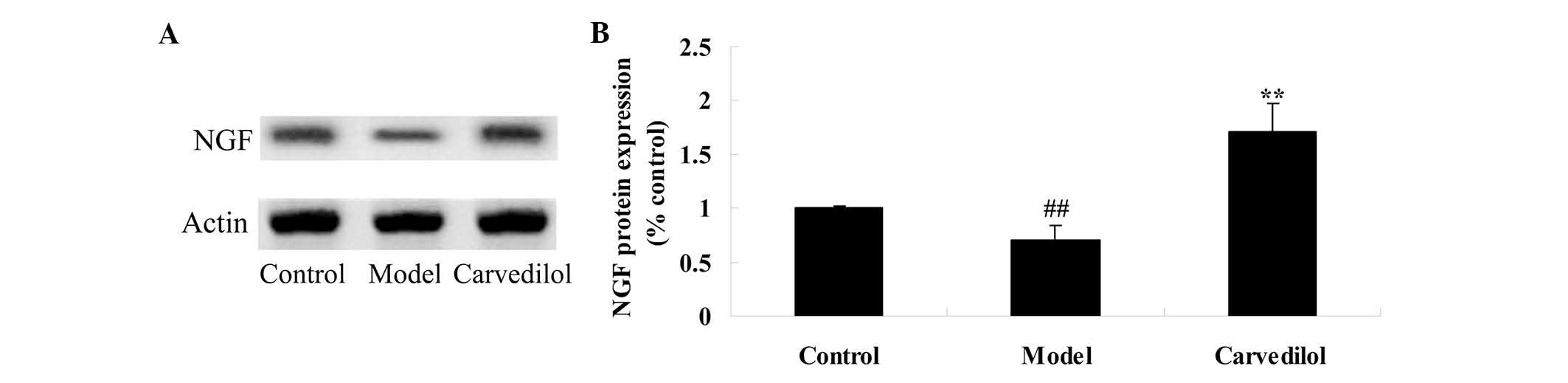
Effects of carvedilol on NGF
expression levels in conjunctivitis rat models
To estimate the effects of carvedilol on NGF protein
expression levels in conjunctivitis rat models, western blotting
(Fig. 5A) and statistical analysis
of the blots (Fig. 5B) was
performed. This revealed that conjunctivitis in rat models resulted
in inhibition of protein expression levels of NGF in the model
group compared with the control group. The administration of
carvedilol significantly increased the protein expression levels of
NGF in the carvedilol-treated group compared with the model group
(Fig. 5).
Effects of carvedilol on VEGF in
conjunctivitis rat models
To evaluate the effects of carvedilol on VEGF
protein expression levels in rats with LPS-induced conjunctivitis,
western blotting (Fig. 6A) and
statistical analysis of the blots (Fig.
6B) was performed. The model group displayed significantly
reduced expression levels of VEGF compared with the control group
(P<0.01). The VEGF protein expression levels were significantly
reduced in the conjunctivitis model group compared with the
carvedilol group (P<0.01; Fig.
6).
Discussion
Conjunctivitis is a frequently observed allergic eye
disease. In total, ~5% of the population have sought medical advice
as a result of an allergic eye disease, of which >50% were cases
of conjunctivitis (15). In recent
years, due to increases in factors such as air pollution and the
use of contact lenses, the incidence of conjunctivitis has risen
(16). Patients typically present
with itchiness of the eye, photophobia, lacrimation and a foreign
body or burning sensation. Although the majority of conjunctivitis
cases rarely result in severe complications, repeated incidence of
the disease are common, and cause severe eye discomfort and
itching, which may affect the patient's quality of life and work
efficiency by reducing their ability to concentrate (17). To the best of our knowledge, the
present study revealed for the first time that carvedilol
significantly reduces augmented clinical sign scores in a rat model
of conjunctivitis.
A recent study revealed that conjunctival infection
can cause systemic inflammatory responses involving the induction
of inflammatory cytokines, including IL-1β, IL-6, IL-8 and TNF-α
(18). It was previously identified
that IL-1β is an important inflammatory cytokine, and participates
in inflammatory responses to injury and autoimmune diseases. IL-1β,
IL-6, IL-8, TNF-α and neutrophils are also involved in an autocrine
loop of inflammatory mediators (19). Patients commonly develop with acute
conjunctivitis as a result of bacterial or viral infections, which
trigger inflammation, and cause mononuclear cells to produce high
levels of IL-1β, IL-6, IL-8 and TNF-α. This results in elevated
levels of the aforementioned inflammatory cytokines in the blood
plasma. Furthermore, cell response function is reduced in acute
conjunctivitis, resulting in the disruption of the cellular immune
network. In particular, disorders may occur in the percentage of T
and B lymphocytes, resulting in increased plasma expression levels
of inflammatory cytokines (20). In
the present study, elevated IL-1β, IL-6, IL-8, TNF-α and NF-κB
expression levels were revealed to be significantly suppressed
following treatment with carvedilol. Similarly, de Araújo Júnior
et al demonstrated that carvedilol decreased IL-1β and TNF-α
expression levels in a rat model of periodontitis (21). Additionally, Arab and El-Sawalhi
reported that carvedilol alleviated adjuvant-induced arthritis
inflammatory mediators (22). Thus,
the effect of carvedilol on conjunctivitis may involve the
suppression of inflammatory mediators in rats.
Conjunctivitis is a complex inflammatory response
involving a variety of factors. Several non-immune factors,
including nerve- and endocrine-related factors, may affect the
pathological changes and clinical manifestations of conjunctivitis
(23). In the serum of patients with
conjunctivitis, NGF expression increases significantly; this
appears to be associated with the infiltration of mast cells in the
palpebral conjunctiva (24).
Patients with conjunctivitis also displayed increased levels of
neuropeptide, which are synthesized and released by various cell
factors involved in NGF regulation and control. Thus, the increased
expression levels of NGF appear to result in increased neuropeptide
expression in patients with conjunctivitis (25). The phenomenon of increased NGF
expression levels is not exclusive to conjunctivitis but also
exists in other systemic allergic diseases (26). In the present study, it was revealed
that carvedilol significantly increases the suppression of NGF
protein expression levels in rat models of conjunctivitis. Shyu
et al revealed that NGF mRNA and protein expression levels
were upregulated by carvedilol in pressure-overloaded rat hearts
(27) and a rat model of
volume-overload heart failure (28).
These results indicate that the effect of carvedilol on
inflammatory mediators may serve to upregulate NGF signaling.
It has been revealed that epithelial cells,
inflammatory cells (eosinophils, monocytes/macrophages) and
conjunctival fibroblasts produce VEGF following stimulation
(29). In angiogenesis, VEGF in
epithelial cells serves a core role in vascular matrix change
(30). Fibroblasts are another
source of the VEGF (31). In the
present study, it was demonstrated that carvedilol significantly
increases VEGF protein expression levels in rat models of
conjunctivitis. Similarly, de Boer et al previously reported
that carvedilol increased VEGF expression levels in patients with
chronic heart failure (32). The
results indicate that the effect of carvedilol on conjunctivitis
may involve the upregulation of VEGF.
In conclusion, carvedilol is able to reduce the
symptoms of conjunctivitis in rat models, and its effect may be
associated with the reversal of the abnormal regulation of
inflammation, as well as increased NGF and VEGF expression levels,
in rats with conjunctivitis. Carvedilol may, therefore, be a
potential novel therapy for conjunctivitis.
Acknowledgements
The present study was supported by the Zhejiang
Provincial Hospital of Traditional Chinese Medicine (Hangzhou,
China; grant no. 2014ZA118).
References
|
1
|
Saha S, Koley M, Ghosh S, Giri M, Das A
and Goenka R: Documentation of prescriptions and clinical outcomes
in a homeopathic hospital setting in West Bengal, India. J Evid
Based Complementary Altern Med. 20:180–185. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schwartz B, Harrison LH, Motter JS, Motter
RN, Hightower AW and Broome CV: Investigation of an outbreak of
Moraxella conjunctivitis at a Navajo boarding school. Am J
Ophthalmol. 107:341–347. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen Y, Zhang X, Yang L, Li M, Li B, Wang
W and Sheng M: Decreased PPAR-γ expression in the conjunctiva and
increased expression of TNF-α and IL-1β in the conjunctiva and tear
fluid of dry eye mice. Mol Med Rep. 9:2015–2023. 2014.PubMed/NCBI
|
|
4
|
Barisani-Asenbauer T, Inic-Kanada A, Belij
S, Marinkovic E, Stojicevic I, Montanaro J, Stein E, Bintner N and
Stojanovic M: The ocular conjunctiva as a mucosal immunization
route: A profile of the immune response to the model antigen
tetanus toxoid. PLoS One. 8:e606822013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Koulikovska M, van der Ploeg I, Herrmann B
and Montan PG: Respiratory syncytial virus and chlamydia are not
detectable by PCR in ongoing vernal keratoconjunctivitis. Ocul
Immunol Inflamm. 9:253–257. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grayston JT, Woolridge RL, Chen CW, Assaad
FA, Maffei S, Yen CH and Yang CY: Bacterial conjunctivitis caused
by a base eye ointment used as a placebo. Rep U S Nav Med Res Lab.
4:1–11. 1960.
|
|
7
|
Doughty MJ: Sodium cromoglycate ophthalmic
solution as a Pharmacy Medicine for the management of
mild-to-moderate, non-infectious inflammation of the conjunctiva in
adults. Ophthalmic Physiol Opt. 16(Suppl 2): S33–S38. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Buckley P and Lowman DM: Chronic
non-infective conjunctivitis in rabbits. Lab Anim. 13:69–73. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nell B, Walde I, Billich A, Vit P and
Meingassner JG: The effect of topical pimecrolimus on
keratoconjunctivitis sicca and chronic superficial keratitis in
dogs: Results from an exploratory study. Vet Ophthalmol. 8:39–46.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ferreri AJ, Dolcetti R, Du MQ, Doglioni C,
Resti AG, Politi LS, De Conciliis C, Radford J, Bertoni F, Zucca E,
et al: Ocular adnexal MALT lymphoma: An intriguing model for
antigen-driven lymphomagenesis and microbial-targeted therapy. Ann
Oncol. 19:835–846. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen J, Huang C, Zhang B, Huang Q, Chen J
and Xu L: The effects of carvedilol on cardiac structural
remodeling: The role of endogenous nitric oxide in the activity of
carvedilol. Mol Med Rep. 7:1155–1158. 2013.PubMed/NCBI
|
|
12
|
Ronsein GE, Guidi DB, Benassi JC, Filho DW
and Pedrosa RC and Pedrosa RC: Cytoprotective effects of carvedilol
against oxygen free radical generation in rat liver. Redox Rep.
10:131–137. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Merayo-Lloves J, Zhao TZ, Dutt JE and
Foster CS: A new murine model of allergic conjunctivitis and
effectiveness of nedocromil sodium. J Allergy Clin Immunol.
97:1129–1140. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gong L, Sun X, Qu J, Wang L, Zhang M,
Zhang H, Wang L, Gu Y, Elion-Mboussa A, Roy L and Zhu B:
Loteprednol etabonate suspension 0.2% administered QID compared
with olopatadine solution 0.1% administered BID in the treatment of
seasonal allergic conjunctivitis: A multicenter, randomized,
investigator-masked, parallel group study in Chinese patients. Clin
Ther. 34:1259–1272. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chansaenroj J, Vongpunsawad S, Puenpa J,
Theamboonlers A, Vuthitanachot V, Chattakul P, Areechokchai D and
Poovorawan Y: Epidemic outbreak of acute haemorrhagic
conjunctivitis caused by coxsackievirus A24 in Thailand, 2014.
Epidemiol Infect. 143:3087–3093. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chang CJ, Yang HH, Chang CA and Tsai HY:
Relationship between air pollution and outpatient visits for
nonspecific conjunctivitis. Invest Ophthalmol Vis Sci. 53:429–433.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yasin MN, Hussain S, Malik F, Hameed A,
Sultan T, Qureshi F, Riaz H, Perveen G and Wajid A: Preparation and
characterization of chloramphenicol niosomes and comparison with
chloramphenicol eye drops (0.5%w/v) in experimental conjunctivitis
in albino rabbits. Pak J Pharm Sci. 25:117–121. 2012.PubMed/NCBI
|
|
18
|
Tanaka J, Tanaka H, Mizuki N, Nomura E,
Ito N, Nomura N, Yamane M, Hida T, Goshima Y, Hatano H, et al:
Semaphorin 3A controls allergic and inflammatory responses in
experimental allergic conjunctivitis. Int J Ophthalmol. 8:1–10.
2015.PubMed/NCBI
|
|
19
|
Enríquez-de-Salamanca A, Calder V, Gao J,
Galatowicz G, García-Vázquez C, Fernández I, Stern ME, Diebold Y
and Calonge M: Cytokine responses by conjunctival epithelial cells:
An in vitro model of ocular inflammation. Cytokine. 44:160–167.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Leonardi A, Curnow SJ, Zhan H and Calder
VL: Multiple cytokines in human tear specimens in seasonal and
chronic allergic eye disease and in conjunctival fibroblast
cultures. Clin Exp Allergy. 36:777–784. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
de Araújo Júnior RF, Souza TO, de Medeiros
CA, de Souza LB, Freitas ML, de Lucena HF, do Socorro Costa Feitosa
Alves M and de Araújo AA: Carvedilol decrease IL-1β and TNF-α,
inhibits MMP-2, MMP-9, COX-2, and RANKL expression, and
up-regulates OPG in a rat model of periodontitis. PLoS One.
8:e663912013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Arab HH and El-Sawalhi MM: Carvedilol
alleviates adjuvant-induced arthritis and subcutaneous air pouch
edema: Modulation of oxidative stress and inflammatory mediators.
Toxicol Appl Pharmacol. 268:241–248. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Levi-Schaffer F, Micera A, Zamir E,
Mechoulam H, Puxeddu I, Piliponsky AM, Aloe L and Pe'er J: Nerve
growth factor and eosinophils in inflamed juvenile conjunctival
nevus. Invest Ophthalmol Vis Sci. 43:1850–1856. 2002.PubMed/NCBI
|
|
24
|
Lambiase A, Bonini S, Micera A, Rama P,
Bonini S and Aloe L: Expression of nerve growth factor receptors on
the ocular surface in healthy subjects and during manifestation of
inflammatory diseases. Invest Ophthalmol Vis Sci. 39:1272–1275.
1998.PubMed/NCBI
|
|
25
|
Kritas SK, Saggini A, Cerulli G, Caraffa
A, Antinolfi P, Pantalone A, Frydas S, Rosati M, Tei M, Speziali A,
et al: Neuropeptide NGF mediates neuro-immune response and
inflammation through mast cell activation. J Biol Regul Homeost
Agents. 28:177–181. 2014.PubMed/NCBI
|
|
26
|
Micera A, Stampachiacchiere B, Normando
EM, Lambiase A and Bonini S and Bonini S: Nerve growth factor
modulates toll-like receptor (TLR) 4 and 9 expression in cultured
primary VKC conjunctival epithelial cells. Mol Vis. 15:2037–2044.
2009.PubMed/NCBI
|
|
27
|
Shyu KG, Liou JY, Wang BW, Fang WJ and
Chang H: Carvedilol prevents cardiac hypertrophy and overexpression
of hypoxia-inducible factor-1alpha and vascular endothelial growth
factor in pressure-overloaded rat heart. J Biomed Sci. 12:409–420.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shyu KG, Lu MJ, Chang H, Sun HY, Wang BW
and Kuan P: Carvedilol modulates the expression of
hypoxia-inducible factor-1alpha and vascular endothelial growth
factor in a rat model of volume-overload heart failure. J Card
Fail. 11:152–159. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang F, Xu P, Xie KC, Chen XF, Li CY and
Huang Q: Effects of tumor microenviromental factors on VEGF
expression. Biomed Rep. 1:539–544. 2013.PubMed/NCBI
|
|
30
|
Taurone S, Ripandelli G, Pacella E,
Bianchi E, Plateroti AM, De Vito S, Plateroti P, Grippaudo FR,
Cavallotti C and Artico M: Potential regulatory molecules in the
human trabecular meshwork of patients with glaucoma:
Immunohistochemical profile of a number of inflammatory cytokines.
Mol Med Rep. 11:1384–1390. 2015.PubMed/NCBI
|
|
31
|
Goi T, Nakazawa T, Hirono Y and Yamaguchi
A: The anti-tumor effect is enhanced by simultaneously targeting
VEGF and PROK1 in colorectal cancer. Oncotarget. 8:6053–6061. 2015.
View Article : Google Scholar
|
|
32
|
de Boer RA, Siebelink HJ, Tio RA, Boomsma
F and van Veldhuisen DJ: Carvedilol increases plasma vascular
endothelial growth factor (VEGF) in patients with chronic heart
failure. Eur J Heart Fail. 3:331–333. 2001. View Article : Google Scholar : PubMed/NCBI
|