Introduction
Nail-patella syndrome (NPS), also known as
hereditary onycho-osteodysplasia, Turner-Kieser syndrome, Fong
disease and iliac horn disease, is a rare disorder involving
multiple organs of both ectodermal and mesodermal origin. The
prevalence of NPS is 1/500,000, and there is a high degree of
penetrance with variable expression (1). NPS has autosomal dominant inheritance,
and a loss of function mutation in the LIM homeobox transcription
factor 1-β (LMX1B) gene localized in the long arm of chromosome 9
(9q34), has been identified as a genetic abnormality causing NPS
(2,3).
A variety of symptoms are associated with this
condition, involving, for example, the kidneys, eyes, bone,
tendons, ligaments and muscles. Clinical manifestations are
extremely variable in frequency and severity and there is inter-
and also intra-familial variability (4,5).
NPS primarily affects bones and joints, with
patellar involvement in ~90% of patients; however, complete
patellar aplasia is observed in only 20% of cases, and more
frequently, the patellae are reduced in size and the knee is
unstable because of patellar subluxations or dislocations (6).
Patellar luxation in NPS is often caused by patellar
aplasia or medial patellofemoral ligament (MPFL) attenuation.
Various surgical options, individually and in combination, have
been described for the management of the recurrent patellar
dislocation in such cases (7–10). The
present case report describes a patient with NPS associated with
dislocation of the patella surgically treated by medial
patellofemoral ligament reconstruction using the method previously
described by Christiansen et al (11).
Case report
A 25-year-old man presented in January 2010 at the
First Hospital of Jilin University (Changchun, China) with pain and
an inability to fully flex the knee that had persisted for 1 year.
The history of the patient included a fall, following which the
symptoms started. The patient also reported having a diffuse pain
and swelling around the knee, which was aggravated by going up and
down stairs. The pain was located anteriorly in the knee and was
described as an aching pain with intermittent sharp and severe
pain. The patient also reported instability and apprehension while
performing flexion activities. Upon clinical examination, the two
patella were located at the same height; however, the left patella
was smaller than the right. During range of motion testing, it was
found that the left patella exhibited maltracking and was
dislocated upon flexing the knee beyond 5°. The Q-angle measured at
30° of knee flexion was 5° in the right knee and 0° in the left.
The patella grind test and apprehension test were negative. The
left patella could be manually subluxed to the lateral side without
difficulty but could not be manually subluxed to the medial side,
indicating lateral structure tightness. Thigh circumferences
proximal to the patella were 31.2 mm on the right side and 30.2 mm
on the left, indicating quadriceps atrophy on the left side. The
left patellar tilt test was negative and no palpable tenderness was
identified around either knee. There were no signs of hyperlaxity
in other joints. The fingernails were normal, but the toenails were
relatively poorly developed.
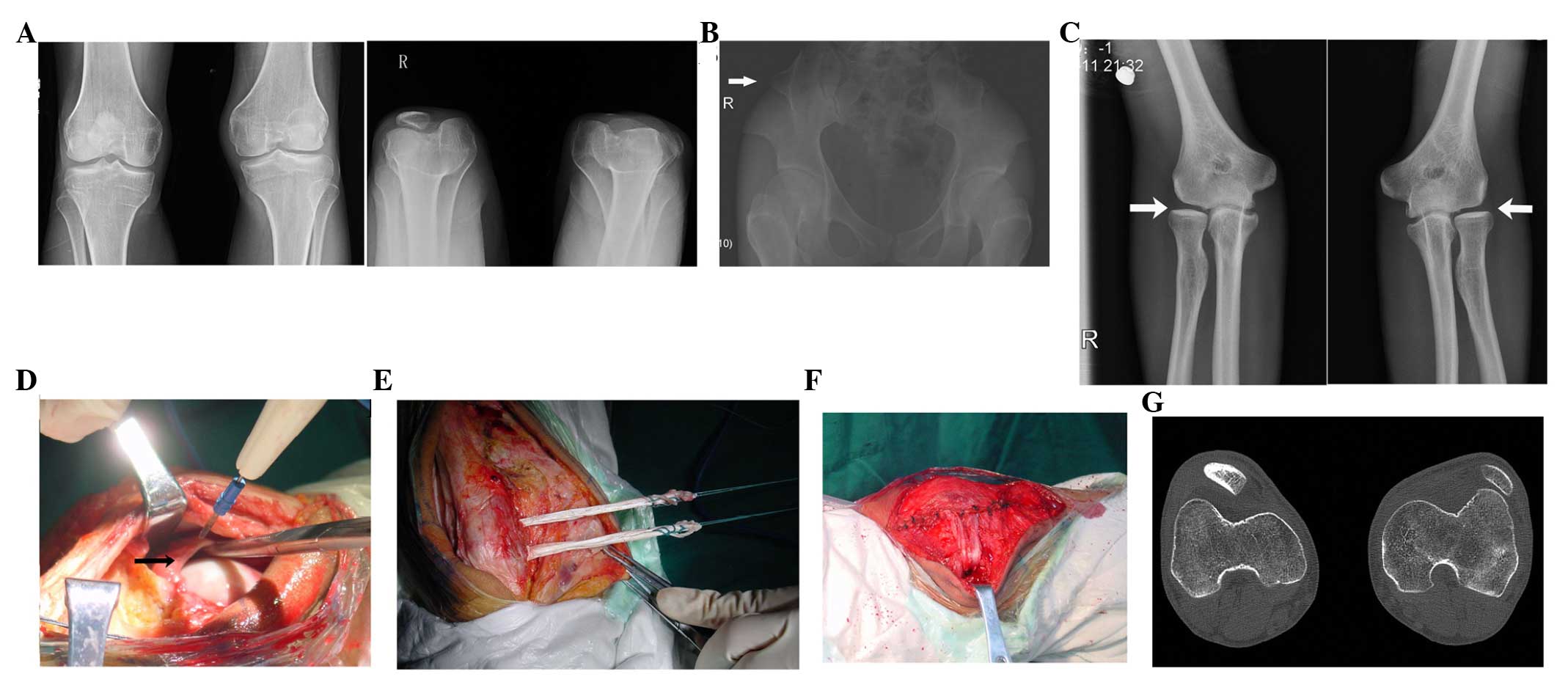
Anteroposterior radiographs (Advantx, GE Healthcare
Life Sciences, Chalfont, UK) revealed a dislocated left patella.
The dimensions of the patellae as measured on the radiographs were
3.33 cm in width and 3.75 cm in height for the right patella and
2.40 cm in width and 2.40 cm in height for the left (Fig. 1A). A right side iliac horn was also
observed (Fig. 1B). Bilateral elbows
showed slight subluxation (Fig.
1C).
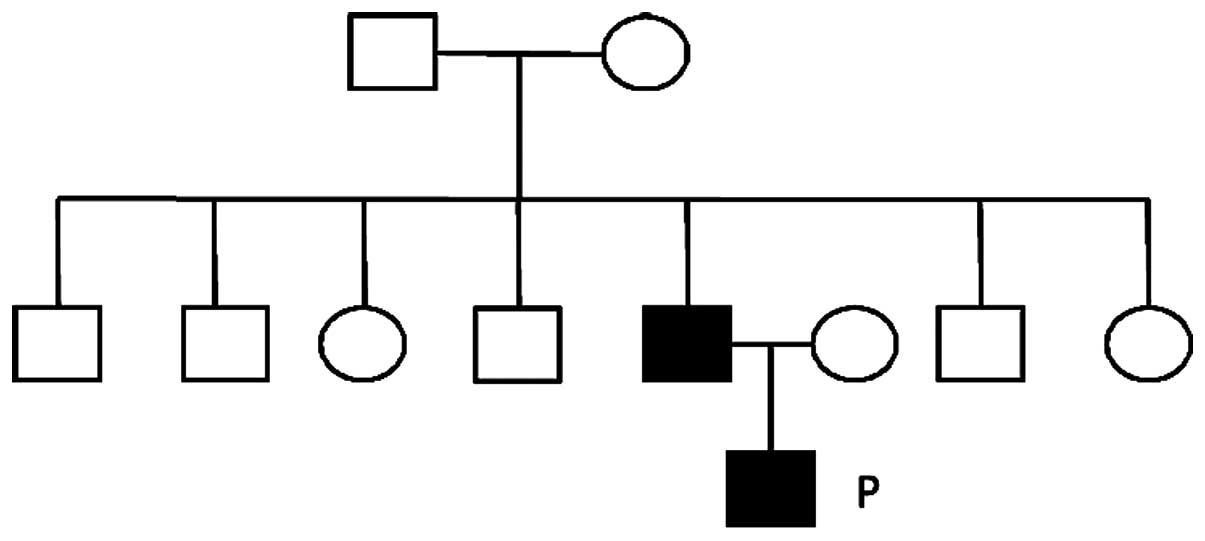
The medical history of the family was traced and it
was found that characteristic symptoms of NPS were exhibited in two
generations of the family (Fig.
2).
A corrective procedure was performed through an
anterior longitudinal incision ~15 cm long. The lateral retinaculum
was tight and so a retinacular release was performed. The medial
plicasynovialis was identified and dissected (Fig. 1D). The medial patellofemoral ligament
structure was not found; therefore, the medial patellofemoral
ligament was reconstructed using the surgical technique described
by Christiansen et al (11).
The gracilis tendon was harvested through a 3-cm incision over the
pes anserinus. Two transverse 3.2-mm drill holes were made through
the patella (Fig. 1E). The adductor
tubercle was exposed and identified at the medial femoral condyle.
A 6-mm hole was drilled at the natural MPFL insertion point, just
distal to the tubercle. The tendon passed through the two 3.2-mm
holes in the patella. On the medial side, the free ends of the
tendon were passed under the fascia to the femoral drill hole. The
two tendon ends were tightened into the femoral drill hole using a
Beath pin pullout technique (11).
The tension and isometricity of the reconstruction were tested
through the arc of motion, and once confirmed the tendons were
fixed in the femoral condyle with a bioresorbable interference
screw (Milagro®; DePuy Synthes, Raynham, MA, USA;
Fig. 1F).
The patient began passive knee exercises using a
continuous passive motion machine (HT-B1, Zhejiang Jinhua Huatong
Medical Appliance Co., Ltd., Zhejiang, China) 1 week after the
surgery. Strengthening and conditioning exercises were initiated
simultaneously. Partial weight-bearing exercises on a straight knee
began during week 2 following the surgery and continued until week
6. After 3 months, the patient was permitted to move freely.
Patient informed consent was obtained for this study.
Discussion
NPS is a rare autosomal-dominant pleiotropic genetic
disorder, with a classical clinical tetrad of symptoms,
specifically fingernail dysplasia, hypoplastic or absent patella,
hypoplasia of the radial head and capitellum and iliac horns. Nail
dysplasia and iliac horns cause little or no disability, but
abnormalities affecting the elbows and knees can cause symptoms
requiring treatment. Involvement of the patella is observed in the
majority of cases, which can include patellar absence or hypoplasia
with subluxation (12). The majority
of cases are asymptomatic and surgical intervention is not
necessary. However, congenital permanent dislocation of the patella
(CPDP) requires surgical treatment.
The present case report describes a patient with
atypical manifestation. The patient did not have congenital
patellar subluxation. Instead, the patient reported knee symptoms
following a minor trauma. On the basis of the patient's history and
clinical examination, it was presumed that, subsequent to the minor
trauma, the medial patellofemoral ligament was torn and this
resulted in a chronic subluxed and dislocated state.
Morphologically, the abnormal patella was smaller than the patella
on the unaffected side. This may have contributed to the patellar
instability, and, additionally, it increased the technical
difficulty of performing a MPFL reconstruction.
There are numerous methods for the treatment of
patella subluxation, the selection of which depends on the
underlying cause. A partial list of commonly employed methods
includes double-strand gracilis autograft (13), combined medial patellofemoral
ligament repair and medial patellotibial ligament reconstruction
(14), single-strand middle third
quadriceps tendon autograft (15),
single-strand adductor magnus split tendon transfer (16), and adductor sling (17) and medial collateral ligament sling
techniques (18). The aim of these
surgical methods used in MPFL is to provide an effective
reconstruction without impairment of normal knee function.
Autologous grafts of various types, such as semitendinosus,
gracilis, quadriceps, semimembranosus tendons and the medial
retinacular tissues have been used. Any bone tunnels are required
to be just large enough to enable the graft to pass through. When
two strands of tendon are used, the superomedial corner of the
patella and the junction of the upper and middle thirds of the
medial border of the patella (or just distal to it) are the
recommended fixation sites (11).
The femoral attachment site can be 10 mm proximal and 2 mm
posterior from the medial femoral epicondyle, or 4 mm distal and 2
mm anterior from the adductor tubercle (11). Fluoroscopic imaging of a lateral view
of the knee can be used to identify the femoral insertion point
(19,20).
In the present case, according to the preoperative
computed tomography scan, the trochlea was well developed (Fig. 1G), but the left patella was smaller
than that on the contralateral side. The instability of the patella
was thus secondary to MPL weakness or absence and lateral
retinaculum contracture. Therefore, an anterior longitudinal
incision was chosen to address both of these problems. MPL
reconstruction was performed using the method described by
Christiansen et al (11)
using a free gracilis tendon passed through two transverse tunnels
in the proximal part of the patella. The reason for selecting this
method was the hypothesis that the double band might provide a
stronger grip on the abnormally small patella. An interference
screw was used for femoral fixation at the adductor tubercle. Due
to the small size of the patella, the holes were located far from
the cartilage surface to avoid patellar fracture after surgery. It
has previously been suggested that it is important not to breach
the anterior cortex of the patella, to reduce the risk of fracture
(13). In the present case, care was
taken to ensure that neither cartilage violation nor any anterior
cortical breach occurred.
After the surgery, the patient exhibited a stable
patella with good patellar tracking. The range of motion in the
immediate postoperative period was also an acceptable 80°. Three
months later, the patient could flex the knee to 130° and ambulate
without crutches. No complications such as fracture, wound
infection or re-dislocation occurred.
In conclusion, the occurrence of secondary patella
dislocation is common in NPS. The most likely cause is an MPFL tear
and corrective surgery should be aimed at reconstructing the
ligament. The present case indicates that reconstruction using
gracilis tendon is a safe and effective method and can be used in
NPS cases caused by an MPFL tear.
References
|
1
|
Sweeney E, Fryer A, Mountford R, Green A
and McIntosh I: Nail patella syndrome: A review of the phenotype
aided by developmental biology. J Med Genet. 40:153–162. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Romero P, Sanhueza F, Lopez P, Reyes L and
Herrera L: c.194 A>C (Q65P) mutation in the LMX1B gene in
patients with nail-patella syndrome associated with glaucoma. Mol
Vis. 17:1929–1939. 2011.PubMed/NCBI
|
|
3
|
Witzgall R: How are podocytes affected in
nail-patella syndrome? Pediatr Nephrol. 23:1017–1020. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Granata A, Nori G, Ravazzolo R, Marini M,
Castellino S, Sicurezza E, Fiore CE and Mignani R: Nail-patella
syndrome and renal involvement. Description of three cases and
literature review. Clin Nephrol. 69:377–382. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Turner JW: An hereditary arthrodysplasia
associated with hereditary dystrophy of the nails. JAMA.
100:882–884. 1933. View Article : Google Scholar
|
|
6
|
Choczaj-Kukula, A and Janniger CK:
Nail-patella syndrome. In emedicine: WebMD. http://emedicine.medscape.com/article/1106294-clinical#b4August
22–2014.
|
|
7
|
Scuderi G, Cuomo F and Scott WN: Lateral
release and proximal realignment for patellar subluxation and
dislocation. A long-term follow-up. J Bone Joint Surg Am.
70:856–861. 1988.PubMed/NCBI
|
|
8
|
Brown DE, Alexander AH and Lichtman DM:
The Elmslie-Trillat procedure: Evaluation in patellar dislocation
and subluxation. Am J Sports Med. 12:104–109. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shelbourne KD, Porter DA and Rozzi W: Use
of a modified Elmslie-Trillat procedure to improve abnormal patellar
congruence angle. Am J Sports Med. 22:318–323. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Peterson L, Karlsson J and Brittberg M:
Patellar instability with recurrent dislocation due to
patellofemoral dysplasia. Results after surgical treatment. Bull
Hosp Jt Dis Orthop Inst. 48:130–139. 1988.PubMed/NCBI
|
|
11
|
Christiansen SE, Jacobsen BW, Lund B and
Lind M: Reconstruction of the medial patellofemoral ligament with
gracilis tendon autograft in transverse patellar drill holes.
Arthroscopy. 24:82–87. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brixey AM Jr and Burke RM:
Arthro-onychodysplasia; hereditary syndrome involving deformity of
head of radius, absence of patellas, posterior iliac spurs,
dystrophy of finger nails. Am J Med. 8:738–744. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lind M, Jakobsen BW, Lund B and
Christiansen SE: Reconstruction of the medial patellofemoral
ligament for treatment of patellar instability. Acta Orthop.
79:354–360. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Feller JA, Amis AA, Andrish JT, Arendt EA,
Erasmus PJ and Powers CM: Surgical biomechanics of the
patellofemoral joint. Arthroscopy. 23:542–553. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Steensen RN, Dopirak RM and Maurus PB:
Minimally invasive “crescentic” imbrication of the medial
patellofemoral ligament for chronic patellar subluxation.
Arthroscopy. 21:371–375. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sillanpää PJ, Mäenpää HM, Mattila VM,
Visuri T and Pihlajamäki H: A mini-invasive adductor magnus tendon
transfer technique for medial patellofemoral ligament
reconstruction: a technical note. Knee Surg Sports Traumatol
Arthrosc. 17:508–512. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gomes Ellera JL: Medial patellofemoral
ligament reconstruction for recurrent dislocation of the patella: a
preliminary report. Arthroscopy. 8:335–340. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Deie M, Ochi M, Sumen Y, Yasumoto M,
Kobayashi K and Kimura H: Reconstruction of the medial
patellofemoral ligament for the treatment of habitual or recurrent
dislocation of the patella in children. J Bone Joint Surg Br.
85:887–890. 2003.PubMed/NCBI
|
|
19
|
Sillanpää PJ and Arendt E: Reconstruction
of the medial patellofemoral ligament using the adductor magnus
tendon. Arthroscopy. 28:1749–1750. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Arendt EA: MPFL reconstruction for PF
instability. The soft (tissue) approach. Orthop Traumatol Surg Res.
95(Suppl 1): S97–S100. 2009. View Article : Google Scholar : PubMed/NCBI
|