Introduction
Coronary artery disease (CAD) is the single most
frequent cause of death worldwide; nearly 7.4 million individuals
succumb to CAD every year, accounting for 13.1% of all deaths
(1). Furthermore, in patients with
CAD, acute myocardial infarction (AMI) is the twelfth leading cause
of cardiac death (2). Each year,
>3 and 4 million individuals suffer from ST-elevated myocardial
infarction (STEMI) and non-ST-elevated myocardial infarction
(NSTEMI), respectively (3). China is
the largest of the 16 developing countries, with a rapidly
developing economy; in China, ≥500,000 individuals have AMI out of
a total of 2 million cardiovascular disease cases annually
(4). According to research conducted
by Hopkin University, ~45% of the adult population has ≥1 chronic
disease; this proportion increases to 90% in individuals >65
years of age, who represent more than half of patients with
myocardial infarction (5,6). Unfortunately, following AMI,
neurohormonal systems that promote pathological ventricular
remodeling and progressive myocardial damage are activated
(7); patients consequently develop
HF due to an impairment of left ventricular myocardial function
(8), which is associated with high
morbidity and mortality. The appropriate management of AMI,
including pharmacology, thrombolysis and invasive therapy, may
marginally decrease vascular complications, composite bleeding
complications and mortality (9).
However, treatment strategy varies with age, gender, ethnicity,
clinical circumstance and socioeconomic status. In addition, ethnic
differences in etiology, outcome and response to therapy in
patients with HF and discrepancies in clinical practice require
validation (10,11). Numerous studies have been conducted
on HF rates and the beneficial clinical effects of evidence-based
drug therapy have been demonstrated in western countries (12,13).
Chongqing is the biggest industrial and commercial center in
southwest China and is diverse in ethnicity, living standards and
population (14). However, little is
known with regards to the characteristics, prognosis of HF
following AMI and HF medications in patients from China and other
Asian countries in clinical practice. The present study aimed to
compare the baseline clinical profile, clinical treatment in
clinical practice, cardiovascular events and in-hospital mortality
rates of AMI patients with and without HF in southwestern
China.
Materials and methods
Ethics statement
The present investigation was approved by the ethics
committee of the First Affiliated Hospital of Chongqing Medical
University (Chongqing, China). Informed consent was not obtained
since this was a retrospective study and the study protocol
conformed to the ethical guidelines of the Declaration of Helsinki.
The patients' information was anonymized and de-identified when the
data were collected and analyzed.
Study design and population
Patients who were hospitalized in the First
Affiliated Hospital of Chongqing Medical University due to AMI
(including STEMI and NSTEMI) between February 2009 and December
2012 were recruited. Patients <18 years old, those who suffered
from stable or unstable angina instead of myocardial infarction and
those with a history of HF, congenital heart diseases, valvular
heart diseases, cardiomyopathy, viral myocarditis, sarcoidosis, or
severe arrhythmias were excluded from the study. A total of 591
patients were included in the investigation and identified
according to the HF status and the type of AMI.
Data were collected retrospectively from hospital
records, including clinical characteristics, initial evaluations,
therapeutic management, major cardiovascular events (MACEs) and
in-hospital mortality and were compared between the two groups of
AMI patients. The use of the evidence-based drugs, including
angiotensin converting enzyme inhibitors (ACEIs) and β-blockers
(BBs), in AMI patients with HF in clinical practice during
hospitalization was further analyzed. Accordingly, patients were
divided into two groups: Patients receiving co-treatment with BBs
and ACEIs and patients either receiving no treatment or treated
with BBs or ACEIs alone.
Diagnostic criteria
All 591 patients suffered from AMI on at least one
occasion. AMI patients with HF during hospitalization was defined
as: i) Simultaneous presentation of AMI and HF; or ii) development
of HF during hospitalization for AMI in a patient with no previous
history of HF due to other diseases.
According to the European Society of Cardiology, the
American College of Cardiology Foundation, the American Heart
Association and the World Heart Federation universal definition of
AMI (2012) (15) and a previous
study (16), the diagnosis of STEMI
was defined by the following criteria: i) Chest pain lasting for
≥30 min that could not be completely relieved by nitrates; ii) new
ST segment elevation present at the J point in two or more
contiguous leads; iii) increase in serum levels of creatine kinase,
creatine kinase MB (CKMB) fraction, or troponins to more than twice
the upper limit of normal levels; and/or iv) evidence of diseased
vessels as determined by cardiac angiography. A diagnosis of NSTEMI
was accepted in the absence of ST-segment elevation, the presence
of ischemic ST-segment or T-wave changes for ≥24 h with positive
cardiac enzymes and/or a typical clinical presentation. Chronic
obstructive pulmonary disease (COPD) was diagnosed by physicians
according to patient clinical respiratory symptoms (dyspnea, cough
and/or sputum production), laboratory test results (including blood
gas analysis and oxygen saturation) and case histories.
The diagnosis of HF in the present study was based
on the following conditions, which were predominantly established
from the European Society of Cardiology guideline for
AMI-associated HF (17): i) Onset of
cardinal manifestations of HF (such as dyspnea and fatigue); ii)
rales in more than one-third of the lung field (Killip class II or
higher); iii) pulmonary edema or congestion on chest radiography,
with no indication of a non-cardiac cause; and/or iv) varying
degrees of abnormal brain natriuretic peptide or N-terminal pro
β-type natriuretic peptide levels. MACEs included atrial
fibrillation, ventricular arrhythmia, major bleeding, cardiogenic
shock, recurrent ischemia and recurrent myocardial infarction.
Cardiogenic shock was defined as systolic blood
pressure <80 mmHg in the absence of hypovolemia and associated
with cyanosis, cold extremities, changes in mental status and
persistent oliguria (18). Bleeding
complications were assessed by the Thrombolysis In Myocardial
Infarction criteria and were classified as major bleeding
(intracranial, overt bleeding with a >50 g/l reduction in
hemoglobin levels, or hematocrit >15%) or minor bleeding
(spontaneous gross hematuria or hematemesis with a >30 g/l
reduction in hemoglobin levels and a <15% reduction in
hematocrit) (19).
Statistical analyses
Clinical characteristic data were analyzed using
χ2 tests for discrete variables and two-tailed Student's
t-tests for continuous variables and were presented as the number
(frequency) and mean ± standard deviation, respectively. Non-normal
continuous variables were analyzed using a Mann-Whitney U-test and
were presented as the median and range. In addition, logistic
regression analysis was performed using a backward selection model
in the following order: i) Presence of post-AMI HF; ii) risk
factors such as age, gender, heart rate, smoking, drinking,
diabetes, hypertension, COPD, history of angina, prior stroke,
chronic renal failure, hyperlipidemia, family history of coronary
artery disease, history of myocardial infarction, STEMI/NSTEMI
myocardial infarction type at presentation, hospitalization, left
ventricular ejection fraction (LVEF), CKMB and length of hospital
stay; iii) in-hospital events, including atrial fibrillation and
ventricular arrhythmia, re-ischemia, major bleeding, re-infarction
and cardiogenic shock; iv) medications during hospitalization,
including antiarrhythmic, oral BBs, calcium-channel blockers, ACEIs
or angiotensin receptor blockers, aspirin and heparin; and v)
cardiac angiography and primary reperfusion strategies, including
thrombolysis and percutaneous coronary intervention (PCI). As
numerous variables were entered into the logistic regression model,
tests for multicollinearity between variables were performed. A
covariance matrix did not demonstrate significant multicollinearity
and tolerance values of all variables in a linear regression model
were high, indicating low multicollinearity.
Due to the limited follow-up period in this study,
the entire length of hospital stay tended to correlate with several
risk factors and in-hospital mortality. The in-hospital survival
curve was calculated using the Kaplan-Meier method and a log-rank
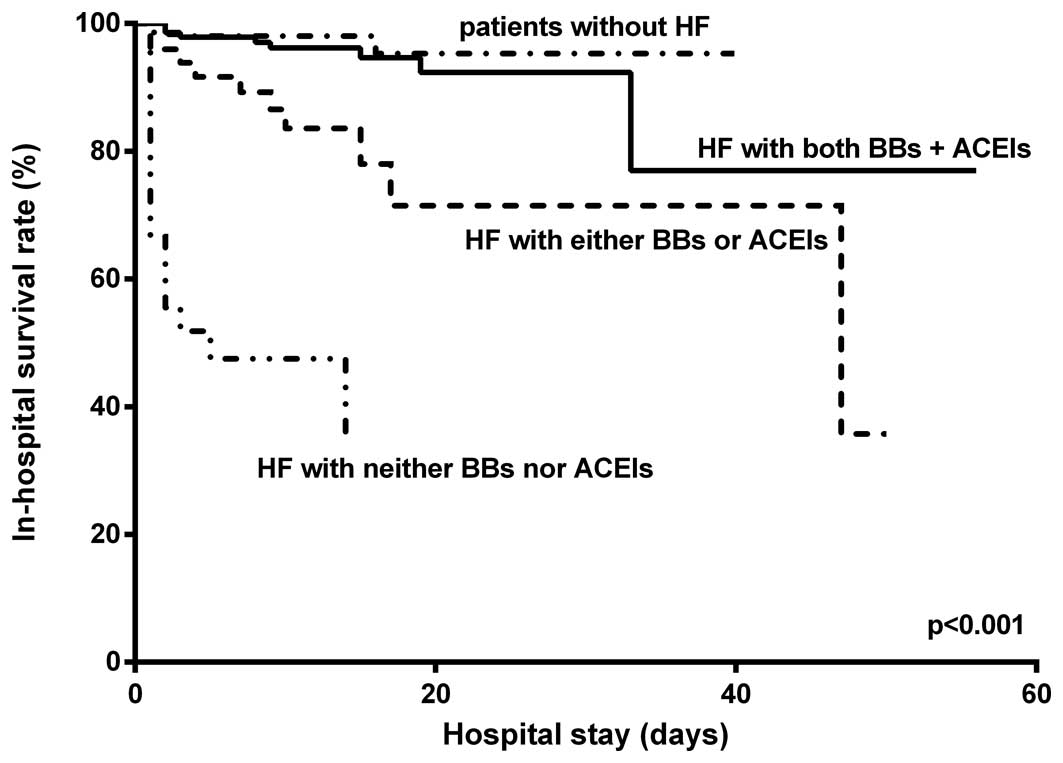
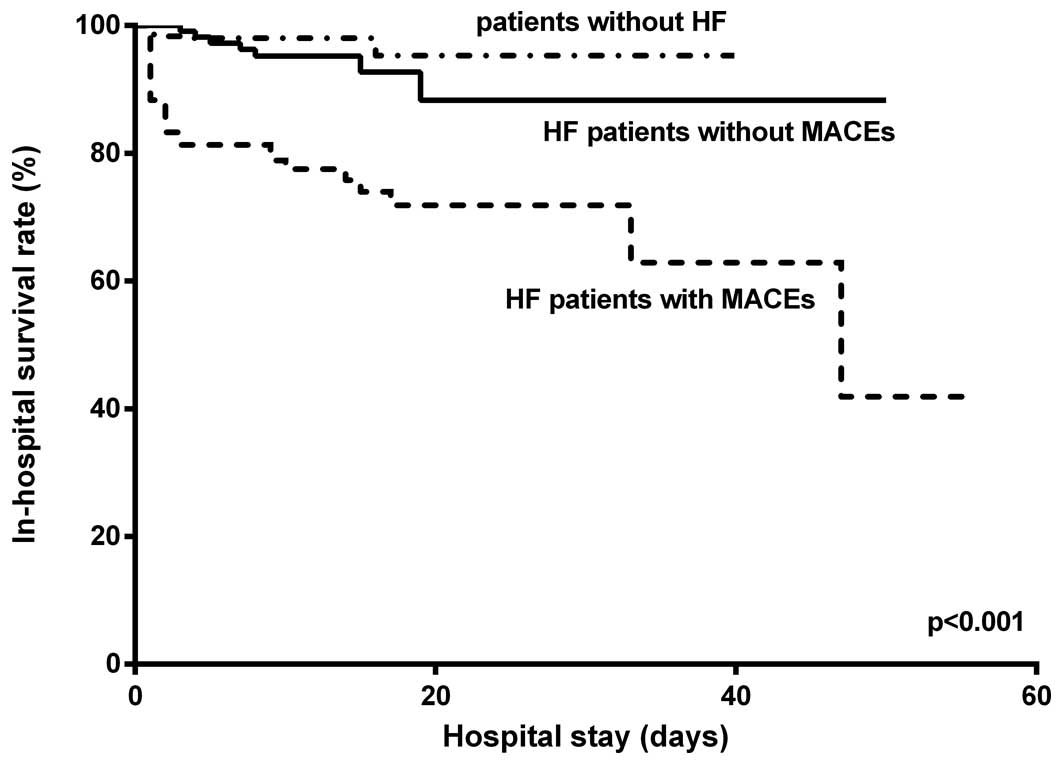
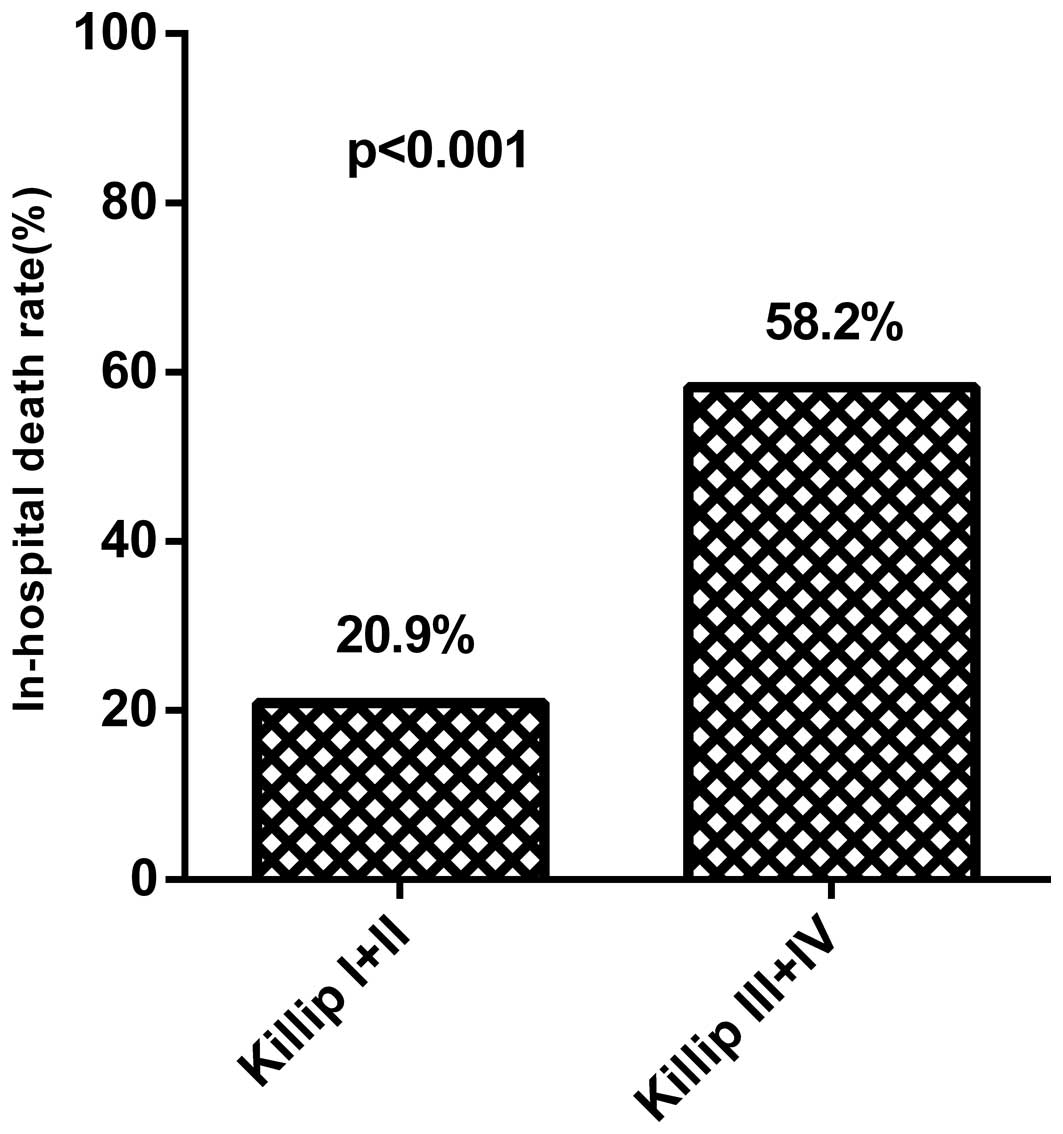
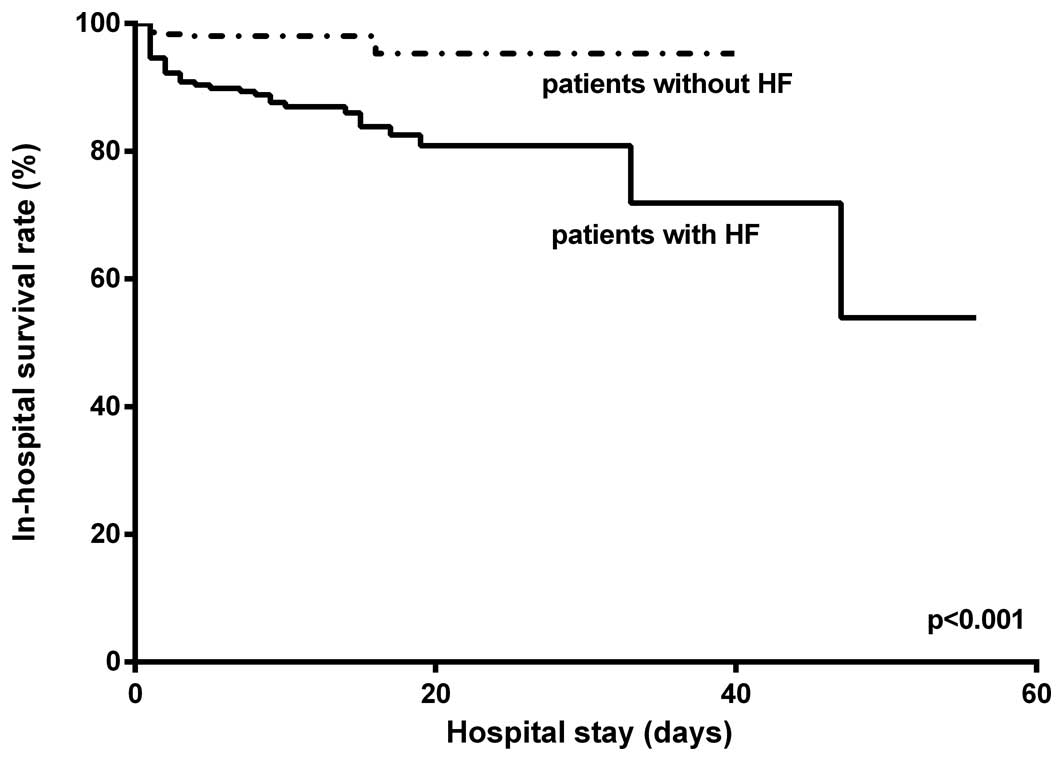
test (Figs. 1–3) and χ2 test (Fig. 4) were used to compare groups.
Statistical analyses were performed using SPSS software version
18.0 (SPSS, Inc., Chicago, IL, USA). P<0.05 was considered to
indicate a statistically significant result for all tests.
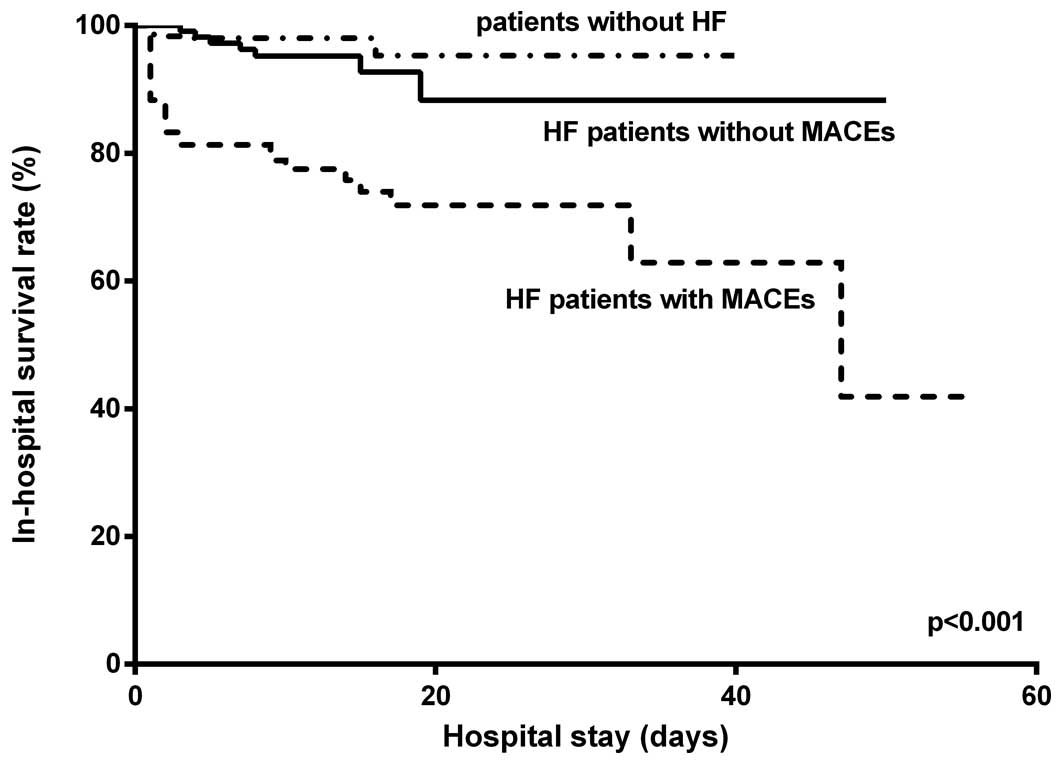 | Figure 3.In-hospital survival rates of non-HF
patients, HF patients with MACEs, and those without MACEs
(P<0.001). Patients without HF, 369 individuals; HF patients
with MACEs, 103 individuals; HF patients without MACEs, 119
individuals. MACEs included atrial fibrillation, ventricular
arrhythmia, major bleeding, cardiogenic shock, recurrent ischemia,
and recurrent myocardial infarction. HF, heart failure; MACEs,
major cardiovascular events. |
Results
Baseline characteristics
The overall demographic and baseline characteristics
of patients with or without first and new-onset HF following STEMI
or NSTEMI are shown in Table I.
Among the 412 STEMI and 179 NSTEMI patients, 162 (38.3%) and 60
(33.5%), respectively, developed first and new-onset HF during
hospitalization. Patients with both STEMI and NSTEMI who developed
in-hospital HF were significantly older and had a higher rate of
renal failure (P<0.05). In addition, these patients had a higher
heart rate, lower LVEF and a higher rate of arrhythmia on admission
(P<0.05), and the rate of atrial fibrillation on admission was
significantly higher in NSTEMI patients with HF (P<0.001). The
rate of ventricular arrhythmia did not differ significantly in
either STEMI and NSTEMI patients according to HF. A preserved LVEF
(≥51%) was noted in 63.6% of STEMI patients and in 63.3% of NSTEMI
patients who developed HF following hospitalization. However, STEMI
patients with HF were more likely to have a history of COPD and a
longer delay prior to hospital presentation (P<0.05).
Accordingly, the peak CKMB value for STEMI patients with
in-hospital HF was significantly higher compared with that for
STEMI patients without HF and the peak serum creatinine and urea
nitrogen values were also higher in HF patients with both AMI
types. A further analysis of post-AMI HF in patients with STEMI
showed that 57.4% of patients had Killip class II AMI, 17.9% had
Killip class III AMI and 21.6% had Killip class IV AMI. Among the
patients with NSTEMI, 70% had Killip class II AMI, 16.7% had Killip
class III AMI and 13.3% had Killip class IV AMI.
 | Table I.Principle characteristics of the
study population evaluated according to HF and AMI status. |
Table I.
Principle characteristics of the
study population evaluated according to HF and AMI status.
|
| STEMI (412
individuals) |
| NSTEMI (179
individuals) |
|
|---|
|
|
|
|
|
|
|---|
| Variable | HF (n=162,
38.3%) | Non-HF (n=250,
60.7%) | P-value | HF (n=60,
33.5%) | Non-HF (n=119,
66.5%) | P-value |
|---|
| Mean age
(years) | 70.7±10.4 | 61.7±11.2 |
<0.001 | 74.0±9.9 | 66.5±11.9 | <0.001 |
| Men | 82
(50.6) | 139 (55.6) | 0.36 | 33 (55.0) | 61 (51.3) |
0.750 |
| Heart
beats/min) | 85.5±24.6 | 76.4±17.0 |
<0.001 | 85.7±21.9 | 75.9±15.9 |
0.001 |
| Diabetes
mellitus | 34
(21.0) | 59
(23.6) |
0.55 | 24 (40.0) | 31 (26.1) |
0.060 |
| Hypertension | 81
(50.0) | 118 (47.2) |
0.61 | 36 (60.0) | 73 (61.3) |
0.870 |
| Smoking | 64
(39.5) | 151 (60.4) |
<0.001 | 20 (33.3) | 49 (41.2) |
0.330 |
| Drinking | 45
(27.8) | 100 (40.0) |
0.01 | 15 (25.0) | 31 (26.1) |
1.000 |
| COPD | 23
(14.2) | 8
(3.2) |
<0.001 | 8
(13.3) | 11 (9.2) |
0.440 |
| Previous
angina | 47
(29.0) | 92
(36.8) |
0.11 | 21 (35.0) | 51 (42.9) |
0.340 |
| Previous MI | 12 (7.4) | 16 (6.4) |
0.69 | 7
(11.7) | 4 (3.4) |
0.050 |
| Stroke | 5
(3.1) | 7
(2.8) |
1.00 | 5 (8.3) | 8 (6.7) |
0.760 |
| Chronic renal
failure | 10 (6.2) | 3
(1.2) |
0.007 | 9
(15.0) | 4 (3.4) |
0.010 |
| Hyperlipidemia | 33 (2.4) | 60
(24.0) |
0.40 | 14 (23.3) | 32 (26.9) |
0.720 |
| Family CAD | 10 (6.2) | 26
(10.4) | 0.16 | 4 (6.7) | 15 (12.6) |
0.310 |
| Killip class |
|
|
|
|
|
|
| II | 93 (57.4) | – | 42 (70.0) | – |
|
III | 29 (17.9) | – | 10 (16.7) | – |
| IV | 35 (21.6) | – | 8 (13.3) | – |
| Arrhythmia | 20
(12.3) | 8
(3.2) | <0.001 | 10 (16.7) | 9 (7.6) |
0.070 |
| AF | 16 (9.9) | 4
(1.6) | 0.11 | 7
(11.7) | 5 (4.2) | <0.001 |
| VA | 4
(2.4) | 4
(1.6) | 0.69 | 3 (5.0) | 4 (3.4) |
0.720 |
| Heart
blockagea | 23
(14.2) | 26
(10.4) | 0.28 | 8
(13.3) | 13 (10.9) |
0.630 |
| Prehospital delay
(h) | 15.1±9.6 | 12.4±9.5 |
0.006 | 18.8±8.1 | 17.0±8.9 |
0.180 |
| LVEF |
|
| <0.001 |
|
| <0.001 |
|
≤40% | 13 (8.0) | 4
(1.6) |
| 6
(10.0) | 4 (3.4) |
|
41~50% | 46
(28.4) | 43
(17.2) |
| 16 (26.7) | 7 (5.9) |
|
≥51 | 103 (63.6) | 203 (81.2) |
| 38 (63.3) | 108 (88.2) |
| Serum creatinine
(µmol/l) | 109.6±86.4 | 80.4±22.2 | <0.001 | 132.4±116.6 | 85.6±36.5 | <0.001 |
| Urea nitrogen
(mmol/l) |
8.0±4.8 | 6.7±6.2 |
0.017 | 9.8±4.9 | 6.7±6.8 |
0.002 |
| CKMBb (ng/ml) and median | 29.45
(0.7–500.0) | 21.00
(0.4–515.0) | 0.04 | 7.7
(0.1–500.0) | 9.3
(0.1–382.8) |
0.850 |
Medical treatment
The medications prescribed to patients with AMI
during hospitalization are listed in Table II. Antiarrhythmic agents and HF
medication (such as diuretics and digitalis) were more often
prescribed to post-AMI (both STEMI and NSTEMI) HF patients. Due to
contraindications (including hemorrhagic disease and stomach
disease) and incomplete original medication administration records
in certain cases, aspirin was prescribed and thus some data bias
may exist. According to standard medical norms, all patients
diagnosed with AMI should receive aspirin treatment except in cases
of severe contraindications. There were no clinically significant
differences in the development of post-AMI HF following the use of
aspirin, BBs and ACEIs, which serve a crucial function in the
prevention of cardiac remodeling and in the treatment of
simultaneous HF and AMI. Therefore, the use of BBs and ACEIs in
patients with or without HF was further analyzed and the results
are shown in Table III. Patients
with HF during hospitalization treated with both classes of
medication (n=142) had a significantly higher survival rate
compared with untreated patients or those treated with either class
of medication alone (n=80; 94.4 vs. 67.5%; P<0.001), although
the two subgroups had similar baseline characteristics. Patients
with HF receiving neither BBs nor ACEIs had the lowest survival
rate (Table III). However, AMI
patients with HF that received both classes of recommended
medication had a significantly lower survival rate compared with
AMI patients without HF (P<0.001; Fig. 1).
 | Table II.Medical treatment during
hospitalization (n=591). |
Table II.
Medical treatment during
hospitalization (n=591).
|
| STEMI |
| NSTEMI |
|---|
|
|
|
|
|
|---|
| Variable | HF (n=162) | Non-HF (n=250) | P-value | HF (n=60) | Non-HF (n=119) | P-value |
|---|
| Treatment |
|
|
|
|
|
|
|
Antiarrhythmic agents | 28
(17.3) | 23 (9.2) |
0.020 | 13 (21.7) | 3
(2.5) | <0.001 |
|
β-blockers | 121 (74.7) | 204 (81.6) |
0.110 | 54 (90.0) | 101 (84.9) |
0.490 |
|
CCB | 38
(23.5) | 53
(21.2) |
0.630 | 19 (31.7) | 38
(31.9) |
1.000 |
|
ACEI/ARB | 116 (71.6) | 188 (75.2) |
0.420 | 43 (71.7) | 92
(77.3) |
0.460 |
|
Diuretics | 126 (77.8) |
37(14.8) | <0.001 | 53 (88.3) | 15
(12.6) | <0.001 |
|
Digitalis | 40
(24.7) | 4
(1.6) | <0.001 | 9
(15.0) | 4
(3.4) |
0.010 |
|
Statin | 146 (90.1) | 240 (96.0) |
0.020 | 51 (85.0) | 117 (98.3) |
0.001 |
|
Aspirin | 147 (90.7) | 233 (93.2) |
0.450 | 46 (76.7) | 108 (90.8) |
0.020 |
|
Heparina | 126 (77.8) | 194 (77.6) |
1.000 | 40 (66.7) | 93
(78.2) |
0.110 |
|
Clopidogrel | 156 (96.3) | 246 (98.4) |
0.200 | 57 (95.0) | 115 (96.7) |
0.690 |
|
Thrombolytic therapy | 22
(13.6) | 30
(12.0) |
0.650 | 1 (1.7) | 3
(2.5) |
1.000 |
| Intervention |
|
|
|
|
|
|
| Cardiac
angiography | 99
(61.1) | 188 (75.2) |
0.003 | 26 (43.3) | 83
(69.7) |
0.001 |
|
PCI | 78
(48.1) | 167 (66.8) | <0.001 | 18 (30.0) | 65
(54.6) |
0.002 |
| TIMI flow grade at
PCI 2–3 | 75
(96.2) | 167
(100.0) | – | 18
(100.0) | 65
(100.0) | – |
| Numbers of diseased
vesselsc | 99 | 188 |
0.170 | 26 | 83 |
0.500 |
|
One | 22
(22.2) | 59
(31.4) | – | 4
(15.4) | 29
(34.9) | – |
|
Two | 26
(26.3) | 52
(27.7) | – | 3
(11.5) | 16
(19.3) | – |
|
Three | 51
(51.5) | 77
(40.9) | – | 19 (73.1) | 38
(45.8) | – |
| Culprit
arteryb |
|
|
| 0.23 |
|
0.350 |
| Left anterior
descending | 81
(50.0) | 141 (56.4) | – | 29 (48.3) | 62
(52.1) | – |
| Right
coronary | 63
(38.9) | 87
(34.8) | – | 15 (25.0) | 23
(19.3) | – |
|
Circumflex | 16 (9.9) | 15 (6.0) | – | 0 | 5
(4.2) | – |
| Not
localized | 2 (1.2) | 7
(2.8) | – | 16 (26.7) | 29
(24.4) | – |
 | Table III.Comparison of post-AMI patients with
HF with or without BB and ACEI treatment. |
Table III.
Comparison of post-AMI patients with
HF with or without BB and ACEI treatment.
| Variable | HF patients with
both BB + ACEI (n=142) | Untreated HF
patients or treated with either class of drug (n=80) | P-value |
|---|
| Mean age
(years) | 71.5±10.7 | 71.7±9.8 |
0.940 |
| Men | 74
(52.1) | 41
(51.3) |
1.000 |
| Diabetes
mellitus | 43
(30.3) | 15
(18.8) |
0.080 |
| Hypertension | 74
(52.1) | 42
(52.5) |
1.000 |
| COPD | 16
(11.3) | 15
(18.8) |
0.160 |
| Previous
angina | 48
(33.8) | 20
(25.0) |
0.230 |
| Chronic renal
failure | 11 (7.7) | 8
(10.0) |
0.620 |
| STEMI | 102 (71.8) | 60
(75.0) |
0.640 |
| LVEF (%) | 51.9±9.0 | 51.9±6.7 |
0.950 |
| Killip class |
|
|
0.003 |
| II | 95
(66.9) | 40
(50.0) | – |
|
III | 26
(18.3) | 13
(16.25) | – |
| IV | 17
(11.9) | 26
(32.5) | – |
| Heart beats
(beats/min) | 85.9±22.0 | 84.9±26.9 |
0.750 |
| Arrhythmia | 20
(14.1) | 10 (12.5 |
0.790 |
| AF | 16
(16.3) | 7
(8.75) |
|
| VA | 4
(2.8) | 3
(3.75) |
|
| Serum
creatininea (µmol/l)
median (range) | 88.0 (7.0,
732.0) | 98.0 (39.0,
860.0) |
0.020 |
| Urea nitrogen
(mmol/l) | 8.23±4.94 | 9.02±4.71 |
0.250 |
| CKMBa (ng/ml) median (range) | 19.50 (0.2,
493.1) | 28.90 (0.1,
500.0) |
0.059 |
| PCI | 68
(47.9) | 28
(35.0) |
0.070 |
| In-hospital
cardiogenic shock | 21
(14.8) | 28
(35.0) |
0.001 |
| In-hospital
mortality | 8
(5.6) | 26
(32.5) | <0.001 |
Notably, post-AMI patients with HF were less likely
to undergo cardiac angiography and PCI compared with patients
without HF (P<0.05; Table II).
Although there were no significant differences in culprit vessels
and vessel disease, as in the case of patients with NSTEMI,
patients with STEMI that developed in-hospital HF had severe right
coronary stenosis, left circumflex disease, or three vessel
disease.
Clinical outcomes
As shown in Table IV
and Fig. 2, the in-hospital
mortality rate was significantly higher in STEMI (15.4 vs. 3.3%)
and NSTEMI (15 vs. 0.8%) patients with HF (P<0.001) compared
with those without HF, as was the length of hospital stay.
Non-fatal in-hospital outcomes such as atrial fibrillation and
ventricular arrhythmia were significantly more frequent in post-AMI
patients with HF (P=0.001 and P<0.001, respectively); however,
there were no significant differences in the rates of recurrent
ischemia, major bleeding, re-infarction or high-grade
atrioventricular blockage between HF and non-HF patients. The
prevalence of MACEs was higher in HF patients with either type of
AMI; post-AMI HF patients with MACEs had a higher risk of
in-hospital mortality compared with those without MACEs
(P<0.001; Table IV; Fig. 3).
 | Table IV.Clinical outcomes of the study
population. |
Table IV.
Clinical outcomes of the study
population.
|
| STEMI |
| NSTEMI |
|
|---|
|
|
|
|
|
|
|---|
| Variable | HF (n=162) | Non-HF (n=250) | P-value | HF (n=60) | Non-HF (n=119) | P-value |
|---|
| In-hospital
mortality | 25 (15.4) | 8
(3.2) | <0.001 | 9
(15.0) | 1 (0.8) | <0.001 |
| Atrial
fibrillation | 20 (12.3) | 9
(3.6) |
0.001 | 8
(13.3) | 3 (2.5) |
0.007 |
| Major bleeding | 4 (2.5) | 1
(0.4) |
0.080 | 0 | 0 | – |
| Ventricular
arrhythmia | 28 (17.3) | 14 (5.6) | <0.001 | 7
(11.7) | 9 (7.6) |
0.410 |
| Recurrent
ischemia | 17 (10.5) | 17 (6.8) |
0.200 | 7
(11.7) | 9 (7.6) |
0.410 |
| Re-MI | 2 (1.2) | 4
(1.6) |
1.000 | 2
(3.3) | 2 (1.7) |
1.000 |
| Cardiogenic
shock | 40 (24.7) | 0 | – | 9
(15.0) | 0 | – |
| High-grade AVB | 4 (2.5) | 7
(2.8) |
1.000 | 2
(3.3) | 4 (3.4) |
1.000 |
| MACEs | 82 (50.6) | 41 (16.4) | <0.001 | 21 (35) | 21 (17.6) |
0.015 |
| Hospital stay
(days) | 12.8±9.7 | 9.4±5.3 | <0.001 | 13.9±9.2 | 9.2±4.9 | <0.001 |
Predictors of outcome
The logistic regression analysis performed to assess
the effect of HF while adjusting for potential confounding factors
is shown in Table V. Cardiogenic
shock [odds ratio (OR), 8.21; 95% confidence interval (CI),
2.75–24.48; P<0.001] following AMI was the strongest predictor
of in-hospital mortality, in addition to the onset of HF (OR, 2.88;
95% CI, 1.00–8.28; P=0.049) and age (OR, 1.07; 95% CI, 1.02–1.12;
P=0.006). Similarly, in-hospital mortality rates were over two
times higher in patients with Killip class III and IV AMI compared
with patients with Killip class I and II AMI (Fig. 4), indicating that Killip class was
associated with in-hospital mortality. Conversely, treatment with
oral BBs (OR, 0.43; 95% CI, 0.61–0.92; P=0.045), treatment with
ACEIs (OR, 0.41; 95% CI, 0.49–0.87; P=0.041), the CKMB value (OR,
1.003; 95% CI, 1.00–1.01; P=0.038) and length of hospital stay (OR,
0.93; 95% CI, 0.87–0.99; P=0.034) were inversely correlated with
in-hospital mortality. Co-treatment with BBs and ACEIs was
associated with reduced mortality (OR, 0.24; 95% CI, 0.16–0.37;
P<0.001). Notably, a history of COPD was inversely associated
with in-hospital mortality (OR, 0.05; 95% CI, 0.00–0.67; P=0.023).
The performance of cardiac angiography (OR, 0.12; 95% CI,
0.04–0.35; P<0.001) was associated with decreased in-hospital
mortality. The logistic regression model demonstrated that patients
with COPD in the overall AMI population had a reverse relationship
with in-hospital mortality. Patients with AMI who presented with
COPD were more likely to develop HF and have a higher prescription
rate of diuretics and digitalis (P<0.05), but a reduced use of
BBs (P<0.001; Table VI).
 | Table V.Predictors of in-hospital
mortality. |
Table V.
Predictors of in-hospital
mortality.
| Variable | Adjusted OR | 95% CI | P-value |
|---|
| Post-AMI HF | 2.88 | 1.00, 8.28 | 0.049 |
| Cardiogenic
shock | 8.21 | 2.75,
24.48 | 0.000 |
| Age | 1.07 | 1.02, 1.12 | 0.006 |
| COPD | 0.05 | 0.00, 0.67 | 0.023 |
| Hospitalization
days | 0.93 | 0.87, 0.99 | 0.034 |
| Antiarrhythmic
agents | 4.59 | 1.84,
11.51 | 0.001 |
| β-blockers | 0.43 | 0.61, 0.92 | 0.045 |
| ACEIs | 0.41 | 0.49, 0.87 | 0.041 |
|
Co-prescriptions | 0.24 | 0.16, 0.37 | 0.000 |
| Cardiac
angiography | 0.12 | 0.04, 0.35 | 0.000 |
| CKMB | 1.00 | 1.00, 1.01 | 0.038 |
 | Table VI.Comparison of all AMI patients
stratified according to COPD status. |
Table VI.
Comparison of all AMI patients
stratified according to COPD status.
| Variable | COPD (n=50,
8.5%) | Non-COPD (n=541,
91.5%) | P-value |
|---|
| HF | 31 (62.0) | 191 (35.3) | <0.001 |
| Men | 28 (56.0) | 287 (53.0) | 0.770 |
| Age | 74.2±8.1 |
65.7±11.9 | <0.001 |
| Heart
beats/min |
81.4±23.7 |
79.6±19.8 | 0.540 |
| Serum creatinine
(µmol/l) | 106.4±75.4 |
93.7±63.6 | 0.190 |
| Urea nitrogen
(mmol/l) |
8.7±6.1 |
7.3±5.9 | 0.090 |
| CKMBa | 11.2 (1.5,
489.8) | 18.7 (0.1,
515.0) | 0.260 |
| LVEF | 52.8±9.7 | 54.8±7.5 | 0.080 |
| Hospital stay
(days) | 10.7±6.8 | 10.8±7.4 | 0.890 |
| STEMI | 31 (62.0) | 381 (70.4) | 0.260 |
| ACEI | 36 (72.0) | 403 (74.5) | 0.740 |
| β-blocker | 32 (64.0) | 448 (82.8) | 0.002 |
| CCB | 13 (26.0) | 135 (24.9) | 0.870 |
| Diuretics | 29 (58.0) | 202 (37.3) | 0.006 |
| Digitalis | 10 (20.0) | 48 (8.7) | 0.020 |
| Clopidogrel | 48 (96.0) | 526 (97.2) | 0.650 |
| Aspirin | 45 (90.0) | 489 (90.4) | 0.810 |
| Thrombolytic
therapy | 1 (2) | 55
(10.2) | 0.070 |
| PCI | 19 (38.0) | 309 (57.1) | 0.010 |
| Three-vessel
disease | 9
(18.0) | 176 (32.5) | 0.070 |
| TIMI flow grade at
PCI 2–3 | 18 (36.0) | 307 (56.7) | 0.160 |
| In-hospital
cardiogenic shock | 4 (8.0) | 45 (8.3) | 1.000 |
Discussion
The present study demonstrated that AMI patients
with HF were at a higher risk of adverse in-hospital outcomes and
had a higher incidence of MACEs compared with AMI patients without
HF. In particular, in-hospital mortality was close to five-fold
higher in STEMI patients with HF, as compared with that of patients
without HF and even higher in NSTEMI patients with HF (15.0 vs.
0.8%). Cardiogenic shock and HF during hospitalization were strong
predictors of in-hospital mortality. Medications such as BBs or
ACEIs were insufficiently prescribed, although the prescription
rate was higher compared with that indicated by previous studies
(20,21). AMI patients with HF who received
neither class of recommended medications (BBs or ACEIs) had a
significantly higher risk of in-hospital mortality compared with
those treated with the recommended medications. In addition, they
were less likely to be examined by cardiac angiography and were
treated with reperfusion therapy.
In the present study, HF occurred in 38.3% of
patients with STEMI and in 33.5% of patients with NSTEMI. This
incidence was similar to rates reported in western countries (32.4
and 34%, respectively) (22,23), although the Killip class in the
present study was higher compared with that reported in an earlier
study (24). One possible reason for
the higher Killip class may be a longer pre-hospital delay compared
with studies conducted in western countries (mean time, <6 h)
and a longer delay in revascularization (25). A previous study demonstrated that a
shorter door-to-balloon time was associated with a decline in the
incidence of cardiovascular events and therefore, improved outcome
following AMI (26). Furthermore,
not all patients underwent immediate cardiac angiography or were
taken directly to a PCI-capable center (hospitals with doctors able
and qualified to perform PCI). These results were concordant with
those of a previous study, in which ~50% of the patients with AMI
were transferred to PCI-capable centers from an interim hospital
without PCI capabilities (27).
Pre-hospital system delays vary and are correlated with
geographical and local factors such as urbanization and the
availability of emergency medical services (28). Regardless of location (western
countries or China), the time to reperfusion therapy for patients
with STEMI transferred for primary PCI is often prolonged, with the
guideline-recommended overall time of <90 min being achieved in
only a minority of transferred patients (29). Considering the geography and traffic
situation of southwestern China, the mean pre-hospital delay is
unable to reach the guideline-recommended goals (30). The direct association between total
ischemic time and severity of myocardial injury and mortality has
been well-established for patients with STEMI (31). These results suggest that all efforts
should be aimed at reducing total ischemic time to achieve improved
prognosis and life expectancy.
As patients with HF are generally older and have
co-morbidities, physicians may hesitate to recommend cardiac
medications or procedures despite an advantageous risk-to-benefit
ratio due to concerns regarding adverse effects (32). Cardiovascular drugs frequently
prescribed to patients with HF were more frequently administered,
except for BBs, ACEIs and aspirin. Although the utilization rate of
BBs and ACEIs remained lower in patients with HF compared with AMI
patients without HF during each period under study, the use of
these two medications increased progressively for HF through the
early 1990s (33,34). However, the issue of a persistent gap
between ideal practice and the actual use of ACEIs for HF cannot be
ignored. It is difficult to close this gap in the adequate use of
evidence-based medications due to numerous clinical conditions or
complex natural and human factors (including co-morbid illnesses,
economics, geography, ethnic or racial differences and genetic
factors) (10,11). Notably, the present analysis
demonstrated that patients with the poorest cardiac function
benefited as much as patients with better function. Data from the
United States indicates that the percentage of patients receiving
ACEIs or angiotensin-receptor blockers is <80% (35), whereas in western Australia, the
prescription rate is 71% (36).
Differences in ethnicity have been reported among these patients
with HF with preserved systolic function (the BB prescription rate
is 80% in Caucasians, 13.4% in African Americans, 1.0% in Asians
and 0.4% in Native Americans). Another study demonstrated that
African Americans with hypertension do not respond as well as
Caucasians to treatment with BB, which may be due to differences in
the sympathetic nervous system or in the use of drugs (37,38).
According to East Asian studies, patients with HF had a better
utilization rate of ACEIs (70–90%) and BBs (60–70%) (12,39),
which may partly explain the lower mortality rate (2.3%, 6.6%).
Patients treated with ACEIs and BBs had a lower all-cause mortality
rate, lower cardiovascular mortality rate and higher long-term
survival rate (33,36,40). In
certain metropolitan regions of China, the utilization rates of
ACEIs and BBs were ~70 and 50% among patients with HF, respectively
(41,42), whereas the utilization rate of BBs
was <40% in general hospitals (43) and lower in rural areas. The
prescription rates of ACEIs (42.8–68.4%) (22,44) and
BBs (37.7–77%) (36,45) in previous studies in other countries
were lower compared with those reported in the present study
(ACEIs, 71.6% and BBs, 74.7–90%), which may partly explain the
higher short-term mortality rates in the previous studies
(15.9–17.7%) compared with those of the present study (15–15.4%).
Furthermore, the MONICA plan (Sino-MONICA project) reported that
the annual morbidity and mortality of Chinese patients with
cardiovascular disease are below worldwide rates and similar rates
were observed in Japan, Korea and other Asian countries (46). As the first-line therapy for AMI with
HF according to the European Society of Cardiology guidelines for
the diagnosis and treatment of HF (47), treatment with ACEIs should be
administered in all patients with preserved ejection fraction as
rapidly as possible following HF diagnosis and maintained during
the various stages, unless there is a contraindication. Oral BBs
should be initiated in the first 24 h in patients with STEMI
without severe contraindications. Following logistic regression,
treatment with BBs or ACEIs had a beneficial effect against
in-hospital mortality, whereas calcium-channel blockers did not
affect in-hospital mortality (48,49).
Meta-analyses of the use of ACEIs in patients with AMI and left
ventricular systolic dysfunction showed a significant reduction in
cardiovascular events and mortality with ACEI use. International
recommendations emphasize the protective role of BBs in patients
with both AMI and HF (50,51). However, further efforts are required
to reduce the gap between ideal practice and the actual use of
recommended medications in China due to a deficient medical system
and an underdeveloped medical information system, in a country with
cultural and demographic similarities and geographical and social
and physical environmental differences (52). China is currently undergoing rapid
socioeconomic changes further to economic reforms, particularly,
increases in the gross national product, average income and
personal expenditure have been reported (46). Further studies are required in order
to investigate the differences between Asia and the rest of the
world and to identify the most effective ways to improve the
utilization rate of recommended medications that have recently
become more available.
In line with the results of previous studies, the
present study demonstrated that AMI patients with HF were less
likely to undergo primary PCI than non-HF patients (22,23).
Early revascularization has been shown to decrease infarct size,
improve cardiac function and decrease the rate of cardiogenic
shock. Although studies have reported the survival benefit of
thrombolysis and PCI in patients with HF (53), other studies including the present
one have not (54). Thrombolysis and
PCI are negatively associated with in-hospital mortality in
patients with HF, which may be explained by prolonged pre-hospital
delay, lower reperfusion rates, associated mechanical complications
(such as mitral regurgitation) or complete infarction. The limited
sample size, short-term follow-up and unavoidable sample bias in
the present study may have masked the positive effects of the
revascularization strategy. According to the 2013 American College
of Cardiology Foundation/American Heart Association guidelines for
MI, primary PCI is the recommended method of reperfusion when it
can be performed in a timely manner (≤90 min) by experienced
operators. However, if thrombolysis therapy is indicated or
selected as the primary reperfusion strategy, it should be
administered within 30 min of hospital arrival (30). Similar to the results of previous
studies (54,55), cardiac angiography had a positive
effect on in-hospital mortality, likely due to the fact that
cardiac angiography can be used to grade the complexity and extent
of AMI and patients can receive relevant therapy accordingly in a
timely and appropriate manner. In addition, cardiac angiography can
be used to assess the requirement for revascularization therapy for
lesions, the number of diseased coronary arteries and the location
and calcification of the vessels that determine AMI complexity
(54). However, further
investigation is required to clarify whether primary PCI is
superior to thrombolysis therapy for AMI patients with HF.
In the present study, the in-hospital mortality rate
was 15–15.4% in the HF group, in the mid-range of previously
reported in-hospital mortality rates in western countries (21.6%)
(22) and China (12.3%) (56). Certain hospital-based studies in
China have reported short-term mortality rates following AMI
ranging from 8.1–13.1% (41,57), which was higher compared with that in
South Asian and Caucasian patients. This may be partly explained by
a delayed presentation to emergency departments from the onset of
AMI symptoms (58). Considering the
large and complex population in China, health education in
cardiovascular patients as well as in healthy individuals is
lacking, resulting in lack of attention in acute severe cases. In
contrast to numerous studies (59,60), the
logistic regression model of the present study for the overall AMI
population demonstrated that COPD was inversely correlated with
in-hospital mortality. AMI patients with COPD were more likely to
develop HF and had higher prescription rates of diuretics and
digitalis (P<0.05), but a lower BB prescription rate (P=0.002).
It is plausible that in these patients with COPD, the alterations
in inflammation, endothelial function and associated platelet
reactivity may have destabilized the underlying coronary disease.
As a result of inflammation, patients with COPD had a decreased
platelet volume and an increased platelet count (61). Marked platelet inhibition may reduce
cardiac adverse events in patients with COPD; however, this
hypothesis requires validation (62). Another explanation may be that COPD
patients suffered from chronic hypoxia, which is responsible for
hemodynamic changes and the activation of the rennin-angiotensin
system. Therefore, these patients with COPD may have a strong
tolerance against the pathological changes of MI or HF; further
studies are required to clarify the underlying mechanisms. The
present cross-sectional study only assessed prognosis in terms of
length of hospital stay (in-hospital mortality), which limited a
long-term follow-up to determine whether the short-term and
long-term prognoses of AMI patients with COPD differ. The
Sino-MONICA project demonstrated that in China, cardiovascular
disease mortality and risk factor levels were higher in the north
and lower in the south (63).
Similar to previous findings, a higher Killip class was associated
with increased hospital mortality, and therefore the Killip
classification serves as an accurate tool for early risk assessment
of in-hospital mortality in patients with AMI (64). Although the incidence and survival
rates of patients with HF have improved in the last decade
(13), the association between a
higher Killip class and worse prognosis has not changed.
Several limitations and strengths are noteworthy in
the present study. Firstly, in an HF setting with a short hospital
stay, medications could not reach the recommended level of
titration. Secondly, patients with HF could not undergo cardiac
angiography and rapidly receive sufficient therapy due to their
poor condition. However, this study has notable strengths as well.
Data from the hospital are real-case observations and were
collected consecutively. With these representative data, the
present investigation demonstrated how AMI was managed in daily
clinical practice in southwestern China and thus demonstrate how it
may be improved.
The present results demonstrated that AMI patients
with HF have a higher mortality rate and are at greater risk of
hospital-associated adverse outcomes compared with AMI patients
without HF in Southwestern China. Guideline-recommended medications
and invasive testing are used less frequently in these patients. In
China, the persistent gap between ideal practice and actual use of
ACEIs and BBs for HF cannot be ignored. The performance of precise
diagnostic methods such as cardiac angiography and timely
administration of standard recommended medications were associated
with improved in-hospital mortality.
Acknowledgements
The authors of the present study are grateful to all
the participating professors and students, specifically Dr Michael
Fu of the Sahlgrenska University Hospital/Östra Hospital and the
staff at the The First Affiliated Hospital of Chongqing Medical
University for their helpful cooperation. The study was supported
by the National Key Clinical Specialties Construction Program of
China (grant no. 170).
References
|
1
|
World Health Organization: Cardiovascular
diseases: Fact sheet 317. http://www.who.int/mediacentre/factsheets/fs317/en/index.htmlAccessed.
March 19–2016
|
|
2
|
Zhao S, Zhang Z, Long Q, Ma Y, Lian X,
Yang Y, Gao W, Chen X and Wang L: Association between time of day
of sports-related physical activity and the onset of acute
myocardial infarction in a Chinese population. PLoS One.
11:e01464722016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Baron T, Hambraeus K, Sundström J, Erlinge
D, Jernberg T and Lindahl B: TOTAL-AMI study group: Type 2
myocardial infarction in clinical practice. Heart. 101:101–106.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xu T, Li W, Teo K, Wang XY, Liu LS and
Yusuf S: INTER-HEART China Investigators: Association of
psychological risk factors and acute myocardial infarction in
China: The INTER-HEART China study. Chin Med J (Engl).
124:2083–2088. 2011.PubMed/NCBI
|
|
5
|
Wolff JL, Starfield B and Anderson G:
Prevalence, expenditures, and complications of multiple chronic
conditions in the elderly. Arch Intern Med. 162:2269–2276. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schmidt M, Jacobsen JB, Lash TL, BØtker HE
and SØrensen HT: 25 year trends in first time hospitalization for
acute myocardial infarction, subsequent short and long term
mortality, and the prognostic impact of sex and comorbidity: A
Danish nationwide cohort study. BMJ. 344:e3562012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cabiddu R, Trimer R, Monteiro CI,
Borghi-Silva A, Trimer V, Carvalho P, Rocha T, Paredes S, Bianchi
AM and Henriques J: Correlation between autonomous function and
left ventricular performance after acute myocardial infarction.
Conf Proc IEEE Eng Med Biol Soc. 2015:3343–3346. 2015.PubMed/NCBI
|
|
8
|
Hunt SA, Abraham WT, Chin MH, Feldman AM,
Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K,
et al: ACC/AHA 2005 guideline update for the diagnosis and
management of chronic heart failure in the adult: a report of the
American College of Cardiology/American Heart Association Task
Force on Practice Guidelines (Writing Committee to Update the 2001
Guidelines for the Evaluation and Management of Heart Failure).
American College of Cardiology. http://www.acc.org/clinical/guidelines/failure//index.pdfAccessed.
December 17–2015
|
|
9
|
Greco C, Rosato S, D'Errigo P, Mureddu GF,
Lacorte E and Seccareccia F: Trends in mortality and heart failure
after acute myocardial infarction in Italy from 2001 to 2011. Int J
Cardiol. 184:115–121. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kramer JM, Newby LK, Chang WC, Simes RJ,
Van de Werf F, Granger CB, Lee KL, White HD, Piegas LS, Topol EJ,
et al: SYMPHONY and 2nd SYMPHONY Investigators: International
variation in the use of evidence-based medicines for acute coronary
syndromes. Eur Heart J. 24:2133–2241. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fischbacher CM, Bhopal R, Povey C, Steiner
M, Chalmers J, Mueller G, Jamieson J and Knowles D: Record linked
retrospective cohort study of 4.6 million people exploring ethnic
variations in disease: Myocardial infarction in South Asians. BMC
Public Health. 7:1422007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yoo BS, Oh J, Hong BK, Shin DH, Bae JH,
Yang DH, Shim WJ, Kim HS, Kim SH, Choi JO, et al: Survey of
guideline adherence for treatment of systolic heart failure in real
world (SUGAR): A multi-center, retrospective observational study.
PLoS One. 9:e865962014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gjesing A, Schou M, Torp-Pedersen C, Køber
L, Gustafsson F, Hildebrandt P, Videbæk L, Wiggers H, Demant M,
Charlot M and Gislason GH: Patient adherence to evidence-based
pharmacotherapy in systolic heart failure and the transition of
follow-up from specialized heart failure outpatient clinics to
primary care. Eur J Heart Fail. 15:671–678. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chongqing Municipality Bureau of
Statistics. Chongqing Statistical Yearbook 2015 (Beijing). Chines
Statistics Press. 2015.
|
|
15
|
Thygesen K, Alpert JS, Jaffe AS, Simoons
ML, Chaitman BR and White HD: Writing Group on behalf of the Joint
ESC/ACCF/AHA/WHF Task Force for the Universal Definition of
Myocardial Infarction: Third universal definition of myocardial
infarction. Glob Heart. 7:275–295. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Juillière Y, Cambou JP, Bataille V, Mulak
G, Galinier M, Gibelin P, Benamer H, Bouvaist H, Méneveau N, Tabone
X, et al: Heart failure in acute myocardial infarction: A
comparison between patients with or without heart failure criteria
from the FAST-MI registry. Rev Esp Cardiol (Engl Ed). 65:326–333.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yancy CW, Jessup M, Bozkurt B, Butler J,
Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi
JL, et al: 2013 ACCF/AHA guidelines for the management of heart
failure: A report of the American college of cardiology
foundation/American heart association task force on practice
guideline. J Am Coll Cardilo. 62:e147–e239. 2013. View Article : Google Scholar
|
|
18
|
Goldberg RJ, Spencer FA, Gore JM, Lessard
D and Yarzebski J: Thirty-year trends (1975 to 2005) in the
magnitude of, management of and hospital death rates associated
with cardiogenic shock in patients with acute myocardial
infarction: A population-based persective. Circulation.
119:1211–1219. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pham PA, Pham PT, Pham PC, Miller JM, Pham
PM and Pham SV: Implications of bleeding in acute coronary syndrome
and percutaneous coronary intervention. Vasc Health Risk Manag.
7:551–567. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Andersson C, Mérie C, Jørgensen M,
Gislason GH, Torp-Pedersen C, Overgaard C, Køber L, Jensen PF and
Hlatky MA: Association of β-blocker therapy with risks of adverse
cardiovascular events and deaths in patients with ischemic heart
disease undergoing noncardiac surgery: A Danish nationwide cohort
study. JAMA Intern Med. 174:336–344. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hersi A, Alhabib KF, Alsheikh-Ali AA,
Sulaiman K, Alfaleh HF, Alsaif S, Al-Mahmeed W, Asaad N, Amin H,
Al-Motarreb A and Al Suwaidi J: Short-term and long-term mortality
associated with ventricular arrhythmia in patients hospitalized
with acute coronary syndrome: Findings from the Gulf RACE
registry-2. Coron Artery Dis. 24:160–164. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
McManus DD, Chinali M, Saczynski JS, Gore
JM, Yarzebski J, Spencer FA, Lessard D and Goldberg RJ: 30-year
trends in heart failure in patients hospitalization with acute
myocardial infarction. Am J Cardiol. 107:353–359. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kaul P, Ezekowitz JA, Armstrong PW, Leung
BK, Savu A, Welsh RC, Quan H, Knudtson ML and McAlister FA:
Incidence of heart failure and mortality after acute coronary
syndromes. Am Heart J. 165:379–385.e2. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gupta T, Harikrishnan P, Kolte D, Khera S,
Subramanian KS, Mujib M, Masud A, Palaniswamy C, Sule S, Jain D, et
al: Trends in management and outcomes of ST-elevation myocardial
infarction in patients with end-stage renal disease in the United
States. Am J Cariol. 115:1033–1041. 2015. View Article : Google Scholar
|
|
25
|
Geng W, Tian X, Fu X, Wang P, Wang Y, Wang
X, Li W and Liu X: Early routine angioplasty versus selective
angioplasty after successful thrombolysis in acute ST-segment
elevation myocardial infarction. Coron Artery Dis. 24:238–243.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Poulin MF, Appis A, Purim-Shem-Tov Y,
Schaer GL and Snell J: Impact of a Novel international platform and
hospital design on the door-to-balloon time in patients presenting
with ST-segment elevation myocardial infarction. Crit Pathw
Cardiol. 14:39–43. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Concannon TW, Nelson J, Goetz J and
Griffith JL: A percutaneous coronary intervention lab in every
hospital? Circ Cardiovasc Qual Outcomes. 5:14–20. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fosbøl EL, Granger CB, Peterson ED, Lin L,
Lytle BL, Shofer FS, Lohmeier C, Mears GD, Garvey JL, Corbett CC,
et al: Prehospital system delay in ST-segment elevation myocardial
infarction care: A novel linkage of emergency medicine services and
inhospital registry data. Am Heart J. 165:363–370. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Koul S, Andell P, Martinsson A, Gustav
Smith J, van der Pals J, Scherstén F, Jernberg T, Lagerqvist B and
Erlinge D: Delay from first medical contact to primary PCI and
all-cause mortality: A nationwide study of patients with
ST-elevation myocardial infarction. J Am Heart Assoc.
3:e0004862014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
O'Gara PT, Kushner FG, Ascheim DD, Casey
DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM,
Franklin BA, et al: CF/AHA Task Force: 2013 ACCF/AHA guideline for
the management of ST-elevation myocardial infarction: executive
summary: A report of the American College of Cardiology
Foundation/American Heart Association Task Force on Practice
Guidelines. Circulation. 127:529–555. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Minha S, Loh JP, Satler LF, Pendyala LK,
Barbash IM, Magalhaes MA, Suddath WO, Pichard AD, Torguson R and
Waksman R: Transfer distance effect on reperfusion: Timeline of
ST-elevation patients transferred for primary percutanenous
coronary intervention. Cardiovasc Revasc Med. 15:369–374. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lazzarini V, Mentz RJ, Fiuzat M, Metra M
and O'Connor CM: Heart failure in elderly patients: Distinctive
features and unresolved issue. Eur J Heart Fail. 15:717–723. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ong HT, Ong LM and Ho JJ:
Angiotensin-converting enzyme inhibitors (ACEIs) and
angiotensin-receptor blockers (ARBs) in patients at high risk of
cardiovascular events: A meta-analysis of 10 randomized
placebo-controlled trials. ISRN Cardiol. 2013:4785972013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hernandez AF, Hammill BG, O'Connor CM,
Schulman KA, Curtis LH and Fonarow GC: Clinical effectiveness of
beta-blockers in heart failure: Findings from the OPTIMIZE-HF
(organized program to initiate lifesaving treatment in hospitalized
patients with heart failure) registry. J Am Coll Cardiol.
53:184–192. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Eschalier R, Chenaf C, Mulliez A, Yalioua
A, Clerfond G, Authier N, Vorilhon C, Citron B, Pereira B, Jean F,
et al: Impact of clinical characteristics and management on the
prognosis of unselected heart failure patients. Cardiovasc Drugs
Ther. 29:89–98. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Hung J, Teng TH, Finn J, Knuiman M, Briffa
T, Stewart S, Sanfilippo FM, Ridout S and Hobbs M: Trends from 1996
to 2007 in incidence and mortality outcomes of heart failure after
acute myocardial infarction: A population-based study of 20, 812
patients with first acute myocardial infarction in Western
Australia. J Am Heart Assoc. 2:e0001722013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Materson BJ, Reda DJ, Cushman WC, Massie
BM, Freis ED, Kochar MS, Hamburger RJ, Fye C, Lakshman R,
Gottdiener J, et al: The Department of Veterans Affairs Cooperative
Study Group on Antihypertensive Agents: Single-drug therapy for
hypertension in men: A comparison of six antihypertensive agents
with placebo. N Engl J Med. 328:914–921. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Prisant LM and Mensah GA: Use of
beta-adrenergic receptor blockers in blacks. J Clin Pharmacol.
36:867–873. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Youn YJ, Yoo BS, Lee JW, Kim JY, Han SW,
Jeon ES, Cho MC, Kim JJ, Kang SM, Chae SC, et al: KorHF Registry:
Treatment performance measures affect clinical outcomes in patients
with acute systolic heart failure. Circ J. 76:1151–1158. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Gomez-Soto FM, Romero SP, Bernal JA,
Escobar MA, Puerto JL, Andrey JL, Almenara J and Gomez F: Mortality
and morbidity of non-systolic heart failure treated with
angiotensin-converting enzyme inhibitors: A propensity-adjusted
case-control study. Int J Cardiol. 139:276–282. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Guo S, Yang Z, Wu D, Yang C, Tao Y, Chen
F, Su W, Zheng R, Yang S, Li X and Chen J: A multi-centre survey on
the therapeutic status of patients with acute myocardial infarction
in Wuxi city of China. Zhonghua Xin Xue Guan Bing Za Zhi.
42:309–313. 2014.PubMed/NCBI
|
|
42
|
Lai EJ, Grubisic M, Palepu A, Quan H, King
KM and Khan NA: Cardiac medication prescribing and adherence after
acute myocardial infarction in Chinese and South Asian Canadian
patients. BMC Cardiovasc Disord. 11:562011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Jiang H and Ge J: Epidemiology and
clinical management of cardiomyopathies and heart failure in China.
Heart. 95:1727–1731. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Teo KK, Liu L, Chow CK, Wang X, Islam S,
Jiang L, Sanderson JE, Rangarajan S and Yusuf S: INTERHEART
Investigators in China: Potential modifiable risk factors
associated with myocardial infarction in China: The INTERHEART
China study. Heart. 95:1857–1864. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Doughty RN, Rodgers A, Sharpe N and
MacMahon S: Effects of beta-blocker therapy on mortality in
patients with heart failure: A systematic overview of randomized
controlled trails. Eur Heart J. 18:560–565. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yang ZJ, Liu J, Ge JP, Chen L, Zhao ZG and
Yang WY: China National Diabetes and Metabolic Disorders Study
Group: Prevalence of cardiovascular disease risk factor in the
Chinese population: The 2007–2008 China National Diabetes and
Metabolic Disorders Study. Eur Heart J. 33:213–220. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
McMurray JJ, Adamopoulos S, Anker SD,
Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C,
Gomez-Sanchez MA, et al: ESC Committee for Practice Guidelines: ESC
Guidelines for the diagnosis and treatment of acute and chronic
heart failure 2012: The Task Force for the Diagnosis and Treatment
of Acute and Chronic Heart Failure 2012 of the European Society of
Cardiology. Developed in collaboration with the Heart Failure
Association (HFA) of the ESC. Eur Heart J. 33:1787–1847. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Strauss MH and Hall AS: The divergent
cardiaovascular effects of angiotensin converting enzyme inhibitors
and angiotensin receptor blockers on myocardial infarction and
death. Prog Cardiovasc Dis. Nov 14–2015.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Xie W, Zheng F, Song X, Zhong B and Yan L:
Renni-angiotensin-aldosterone system blockers for heart failure
with reduced ejection fraction or left ventricular dysfunction:
Network meta-analysis. Int J Cardiol. 205:65–71. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Swedberg K, Cleland J, Dargie H, Drexler
H, Follath F, Komajda M, Tavazzi L, Smiseth OA, Gavazzi A, Haverich
A, et al: Task Force for the Diagnosis and Treatment of Chronic
Heart Failure of the European Society of Cardiology: Guidelines for
the diagnosis and treatment of chronic heart failure: Executive
summary (update 2005): The Task Force for the Diagnosis and
Treatment of Chronic Heart Failure of the European Society of
Cardiology. Eur Heart J. 26:1115–1140. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Van de Werf F, Ardissino D, Betriu A,
Cokkinos DV, Falk E, Fox KA, Julian D, Lengyel M, Neumann FJ,
Ruzyllo W, et al: Task Force on the Management of Acute Myocardial
Infarction of the European Society of Cardiology: Management of
acute myocardial infarction in patients presenting with ST-segment
elevation. Eur Heart J. 24:28–66. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Dang H, Wang Q, Wang H, Yan M and Liu X:
The integration of Chinese material medica into the Chinese Health
Care Delivery System, an update. Phytother Res. 30:292–297. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Huynh T, Perron S, O'Loughlin J, Joseph L,
Labrecque M, Tu JV and Théroux P: Comparison of primary
percutaneous coronary intervention and fibrinolytic therapy in
ST-segment-elevation myocardial infarction: Bayesian hierarchical
meta-analyses of randomized controlled trials and observational
studies. Circulation. 119:3101–3109. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Harjola VP, Follath F, Nieminen MS,
Brutsaert D, Dickstein K, Drexler H, Hochadel M, Komajda M,
Lopez-Sendon JL, Ponikowski P and Tavazzi L: Characteristics,
outcomes and predictors of mortality at 3 months and 1 year in
patients hospitalized for acute heart failure. Eur J Heart Fail.
12:239–248. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Goldberg RJ, Samad NA, Yarzebski J,
Gurwitz J, Bigelow C and Gore JM: Temporal trends in cardiogenic
shock complicating acute myocardial infarction. N Engl J Med.
340:1162–1168. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Khan NA, Grubisic M, Hemmelgarn B,
Humphries K, King KM and Quan H: Outcomes after acute myocardial
infarction in South Asia, Chinese, and white patients. Circulation.
122:1570–1577. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zhou L, Honma T and Kaku N: Comparison of
incidence, mortality and treatment of acute myocardial infarction
in hospitals in Japan and China. Kurume Med J. 39:279–284. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Jones DA, Gallagher S, Rathod KS, Redwood
S, de Belder MA, Mathur A, Timmis AD, Ludman PF, Townend JN and
Wragg A: NICOR (National Institute for Cardiovascular Outcomes
Research): Mortality in South Asians and Caucasians after
percutaneous coronary intervention in the United Kingdom: An
observational cohort study of 279, 256 patients from the BCIS
(British cardiovascular intervention society) national database.
JACC Cardiovasc Interv. 7:362–371. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Campo G, Guastaroba P, Marzocchi A,
Santarelli A, Varani E, Vignali L, Sangiorgio P, Tondi S, Serenelli
C, De Palma R and Saia F: Impact of COPD on long-term outcome after
ST-segment elevation myocardial infarction receiving primary
percutaneous coronary intervention. Chest. 144:750–757. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Vestbo J, Hurd SS, Agustí AG, Jones PW,
Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ,
Nishimura M, et al: Global stragegy for the diagnosis, management
and prevention of chronic obstructive pulmonary disease: GOLD
executive summary. Am J Respir Cirt Care Med. 187:347–365. 2013.
View Article : Google Scholar
|
|
61
|
Wang RT, Li JY, Cao ZG and Li Y: Mean
platelet volume is decreased during an acute exacerbation of
chronic obstructive pulmonary disease. Respirology. 18:1244–1248.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Campo G, Pavasini R, Malagù M, Punzetti S,
Napoli N, Guerzoni F, Papi A, Ceconi C and Contoli M: Relationship
between troponin elevation, cardiovascular history and adverse
events in patients with acute exacerbation of COPD. COPD.
12:560–567. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Wu Z, Yao C, Zhao D, Wu G, Wang W, Liu J,
Zheng Z and Wu Y: Sino-MONICA project: A collaborative study on
trends and determinants in cardiovascular diseases in China, Part
i: Morbidity and mortality monitoring. Circulation. 103:462–468.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Mello BH, Oliveira GB, Ramos RF, Lopes BB,
Barros CB, Carvalho Ede O, Teixeira FB, Arruda GD, Revelo MS and
Piegas LS: Validation of the Killip-Kimball classification and late
mortality after acute myocardial infarction. Arq Bras Cardiol.
103:107–117. 2014.(In English and Portuguese). PubMed/NCBI
|