Introduction
The intervertebral disc (IVD) is a complex tissue
located between two bony vertebrae, which is composed of a
centrally located hydrated nucleus pulposus, a peripherally located
elastic and fibrous annulus fibrosus, and cartilaginous endplates
(1). Intervertebral disc
degeneration (IDD) is the leading cause of lower back pain and
certain other disc disorders, and is associated with a reduction in
proteoglycan and type II collagen levels and an increase in type I
collagen levels in the nucleus pulposus (2,3).
Consequently, IDD leads to spinal degenerative diseases, including
lumbar disc herniation (LDH), the most common degenerative spine
disease in elderly people (4,5). The
symptoms of LDH include lower back pain, weakness, numbness, pain
and tingling in the leg or foot, and cauda equina syndrome
(6). The incidence of LDH is higher
in developing countries, particularly in China, and the rate of LDH
remains ~3–13% (7). Similarly to
other complex diseases, the etiology of LDH includes both
hereditary and environmental factors (8,9).
Hereditary factors include family history, and occupational factors
are among the most significant environmental factors, including
lumbar load, heavy physical work, and bending over or twisting
(10,11). Previous studies have demonstrated
that inflammatory cells and inflammatory medium are present in
degenerative lumbar disc tissue, including interleukin (IL)-17 and
tumor necrosis factor (TNF)-α, which are associated with the
degeneration of LDH and hence the pathogenesis of IDD (12–14).
IL-17 is a signature cytokine of T helper 17 cells,
which induces the activation and mobilization of neutrophils, and
triggers the production of chemokines and pro-inflammatory
cytokines through cellular targets (15,16).
IL-17 includes six family members, IL-17A-F, which have roles in
the maturation of hematopoietic progenitor cells (16,17).
Excessive or inappropriate production of IL-17 is associated with
various disorders or diseases, including asthma, rheumatoid
arthritis, ulcerative colitis, IDD, other autoimmune or
inflammatory diseases and cancer (18). Along with TNF-α and interferon-γ,
IL-17 expression has been demonstrated to be elevated in herniated
and IDD tissue samples, which suggested that IL-17 has an important
role in IDD (19).
TNF-α is an inflammatory cytokine is important in
cell growth and death, tumor formation, stress response and immune
response (20,21). The predominant functions of TNF-α
include upregulating the activity of matrix metalloproteinases
(MMPs) and the expression of genes, reducing the synthesis of
collagen and proteoglycans, stimulating the inflammatory response
and the production of other cytokines such as IL-l, IL-6, IL-8 and
prostaglandin E2, promoting cell migration and improving the
permeability of endothelial cells (22–24). One
of the basic pathological changes of IDD is the degradation of the
extracellular matrix (25). MMPs and
tissue inhibitors of metalloproteinases (TIMPs) have an important
role in degradation of the extracellular matrix in IVD (3,10,26).
Previous studies have shown that IL-17 upregulates the expression
of MMP-1/13 in chondrocytes and synovial fibroblasts, enhances the
enzyme activity of aggrecanase and collagenase and the
monocyte-induced damage of the cartilage matrix, promotes the
degradation of cartilage proteoglycan and collagen, and suppresses
the synthesis of cartilage proteoglycan (19,20,27,28).
Recent studies have suggested that TNF-α may stimulate IVD cells to
produce MMP-3, and that MMP-3 can degrade not only the glycoprotein
matrix (including fibronectin, laminin and gelatin) and
proteoglycans, but also type II collagen and elastin, thereby
increasing IDD (29–31). Therefore, IL-17 and TNF-α may both be
involved in the progression of IDD. The aim of the present study
was to examine the expression of IL-17 and TNF-α and their
association with IDD, in order to further understand the
pathogenesis of IDD and provide valuable clinical information for
the treatment of LDH.
Materials and methods
Ethical statement
The present study was approved by the Institutional
Review Board of the Third Affiliated Hospital of Guangzhou Medical
University (Guangzhou, China). Informed written consent was
obtained from each eligible patient and the study was performed in
accordance with the Declaration of Helsinki.
Subjects and study design
A total of 40 patients with LDH (26 male and 14
female; mean age, 35.82±12.45 years; age range, 21–65 years)
admitted to the Department of Orthopedics at the Third Affiliated
Hospital of Guangzhou Medical University between November 2011 and
May 2012 were included in the present study. The diagnosis of LDH
was confirmed by clinical manifestation, medical history, clinical
examinations and imaging examinations, as well as lower nucleus
signal on T2-weighted (TW2) magnetic resonance imaging (MRI). IVD
tissue samples, comprising nucleus pulposus tissue, were surgically
removed from the 40 patients with LDH, and designated as the
experimental group samples. According to the classification of the
North American Spine Society (32)
and clinical experience, the experimental tissue samples were
further divided into an annulus fibrosus disrupted group (18
samples with a ruptured external annulus) and an annulus fibrosus
undisrupted group (22 samples with an intact external annulus).
Five patients had L3-4 intervertebral segment LDH, 24 patients had
L4-5 LDH and 11 patients had L5-S1 LDH.
The present study also included a control group
comprising 10 patients with lumbar vertebra fractures (7 male and 3
female; mean age, 34.55±13.23 years; age range, 21–65 years), who
were examined by MRI and exhibited normal signals from the lumbar
discs. The patients were admitted to the Department of Orthopedics
of the Third Affiliated Hospital of Guangzhou Medical University
between November 2011 and May 2012. Traumatic lumbar disc tissue
(nucleus pulposus) samples were surgically removed from patients
with lumbar vertebra fractures and designated as the control group.
One patient exhibited L3-4 intervertebral segment LDH, 7 patients
had L4-5 LDH, and 2 patients had L5-S1 LDH.
MRI grading
The IDD tissue samples were examined by TW2 MRI and
divided into five grades (Table I)
according to the modified Pearce Standard (33): Grades I and II indicated normal
discs, and grades III–V indicated degenerated discs. The tissue
samples in this experiment were classified as grade I (n=6), grade
II (n=4), grade III (n=14), grade IV (n=13) and grade V (n=13) on
the basis of MRI grading.
 | Table I.Disc degeneration characteristics as
determined by T2-weighted magnetic resonance imaging. |
Table I.
Disc degeneration characteristics as
determined by T2-weighted magnetic resonance imaging.
| Grade | Structure | Nucleus and annulus
distinction | Signal
intensity | Height of
intervertebral disc |
|---|
| I | Homogeneous, bright
white | Clear | Hyperintense,
isointense to cerebrospinal fluid | Normal |
| II | Inhomogeneous with
or without horizontal bands | Clear | Hyperintense,
isointense to cerebrospinal fluid | Normal |
| III | Inhomogeneous,
gray | Unclear | Intermediate | Normal to slightly
decreased |
| IV | Inhomogeneous, gray
to black | Absent | Intermediate to
hypointense | Normal to
moderately decreased |
| V | Inhomogeneous,
black | Absent | Hypointense | Collapsed disc
space |
Pathological data
The lumbar disc tissue samples were randomly divided
into two groups: One was used for hematoxylin and eosin (H&E)
staining and immunohistochemical staining following fixing with
neutral formaldehyde solution, embedding with paraffin, and
sectioning, and the other was used for semi-quantitative reverse
transcription polymerase chain reaction (RT-PCR) by immersion in
liquid nitrogen.
H&E staining
The LDH tissue sections were fixed in 4%
paraformaldehyde (Linyi Lixing Chemical Co., Ltd., Linyi, China)
for 48 h at room temperature, embedded in paraffin using an
embedding apparatus (SYD-B; Shenyang Tianrong Cable Material Co.,
Ltd., Shenyang, China) and incubated at 60°C for 3 h. Tissues were
then cut (RM2135; Leica Microsystems, Wetzlar, Germany) into 4 µm
sections. The tissue sections were then deparaffinized in twice in
xylene solution (Shanghai Jiuyi Chemical Reagent Co., Ltd.,
Shanghai, China) for 15 min prior to being rehydrated by immersion
in descending grades of ethanol (absolute ethanol twice for 5 min;
100% ethanol for 5 min; 80% ethanol for 5 min; and 70% ethanol for
5 min; Anhui Ante Biological Chemical Co., Ltd., Anhui, China), and
washed three times with distilled water for 2 min. The tissue
sections were stained using H&E (Anhui Ante Biological Chemical
Co., Ltd.), washed with running water for 2 min, dehydrated with
ethanol, vitrified with xylene and sealed on glass coverslips with
gum (Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd.,
Beijing, China). The tissue sections were then observed under a
microscope (BX51; Olympus Corporation, Tokyo, Japan) and the
staining results were recorded.
Immunohistochemical staining
Immunohistochemical staining was performed on the
paraffin-embedded tissue sections. Following incubation at 60°C for
10 min, the tissue sections were deparaffinized twice in xylene for
10 min, hydrated in descending grades of ethanol (100, 90, 75 and
50% ethanol for 5 min each), immersed in distilled water for 5 min
and rinsed three times with phosphate-buffered saline (PBS) for 3
min (pH 7.4; Beijing Dingguo Changsheng Biotechnology Co. Ltd.,
Beijing, China). Subsequently, the tissue sections were incubated
with 3% peroxidase-blocking agent (Guduo Biotechnology Corporation,
Shanghai, China) for 15 min at room temperature to eliminate
endogenous peroxidase activity, and washed again three times with
PBS for 3 min (pH 7.4). Each tissue section was incubated with 50
µl primary rabbit monoclonal antibody against IL-17 (1:50; ab83688,
Abcam, Cambridge, MA, USA) at 37°C for 1 h, and then with 50 µl
biotin-labeled rabbit polyclonal secondary antibody against TNF-α
(1:200; ab6671, Abcam) and 50 µl horseradish peroxidase
streptavidin solution (1:400; Beijing Dingguo Changsheng
Biotechnology Co. Ltd.) at 37°C for 40 min. The tissue sections
were washed three times with PBS for 3 min (pH 7.4) following each
incubation. Subsequently, diaminobenzidine was added and the tissue
sections were observed under a microscope. Finally, the tissue
sections were rinsed with tap water, counterstained using
hematoxylin, dehydrated with an ethanol gradient and sealed with
neutral gum. Staining in the cytoplasm was recorded according to
the following criteria: Brown/yellow, positive; dark brown/yellow,
strongly positive; light brown/yellow, weakly positive; no
staining, negative.
Semi-quantitative RT-PCR
Total RNA (5 µl) of the lumbar IVD tissue samples
was isolated using TRIzol® reagent (Takara Bio, Inc.,
Otsu, Japan) and an ultra-violet spectrophotometer (model Q5000;
Bruker BioSpin, Fällanden, Switzerland) was used to measure the
concentration and purity of the RNA samples with
OD260/OD280. Agarose gel electrophoresis was
then used to examine the integrity of the RNA samples. To avoid
adverse effects of genomic/contaminating DNA on reverse
transcription, a deoxyribonuclease I kit (Sigma-Aldrich, St. Louis,
MO, USA) was used to digest DNA in the total RNA samples according
to the manufacturer's protocol. cDNA was synthesized from total RNA
samples using a ReverTra Ace qPCR RT kit (Toyobo Co., Ltd., Osaka,
Japan) and the product was stored at −20°C until further usage.
RT-PCR was performed using the SYBR Green Real-Time PCR Master Mix
Kit (Toyobo Co. Ltd.) according to the manufacturer's protocol. The
reaction solution (50 µl) consisted of 12 µl DEPC water, 25 µl
THUNGERBIRD SYBR qPCR Mix, 1 µl forward primer, 1 µl reverse
primer, 1 µl 50X ROX reference dye and 10 µl cDNA solution. The
amplification conditions were as follows: 1 Cycle of 50°C for 2 min
and 95°C for 5 min; followed by 40 cycles of 95°C for 15 sec and
60°C for 1 min. Gene amplification was performed on an ABI PRISM
7000 Sequence Detection System (Applied Biosystems; Thermo Fisher
Scientific, Inc., Waltham, MA, USA). After the completion of
amplification, melting curves were obtained by heating to 60°C to
verify the PCR products. The whole sequence of mRNA for each target
gene was obtained from the GenBank sequence database and Primer 5.0
software (Premier Biosoft, Palo Alto, CA, USA) was used to design
the primer sequences. The primers used in the present study are
presented in Table II. All primers
were purchased from Beijing Dingguo Changsheng Biotechnology Co.,
Ltd. Absorbance value (A) was measured using an image analysis
system (JS2012; Beijing Maisiqi High-Tech Co., Ltd., Beijing,
China), and the relative amount of IL-17 or TNF-α mRNA was
expressed as IL-17/β-actin or TNF-α/β-actin.
 | Table II.Primers. |
Table II.
Primers.
| Gene | Sequences
(5′→3′) | Length of products
(bp) |
|---|
| GAPDH |
AGAAGGCTGGGGCTCATTTG | 258 |
|
|
AGGGGCCATCCACAGTCTTC |
|
| IL-17 |
TGCCTTCAAGACTGAACAC | 254 |
|
|
TCTCTGAGGGGCCTTAATC |
|
| TNF-α |
CAATCCCTTTATTACCC | 293 |
|
|
GTCTTCTCAAGTCCTGC |
|
Statistical analysis
All data were expressed as means ± standard
deviation, and all statistical analyses were performed using SPSS
software, version 11.5 (SPSS, Inc., Chicago, IL, USA). Correlation
between two variables was analyzed with Pearson's correlation
analysis. One-way analysis of variance was used for comparison
between multiple groups and least significant difference (LSD)
t-test for comparisons between two groups. P<0.05 was considered
to indicate a statistically significant difference.
Results
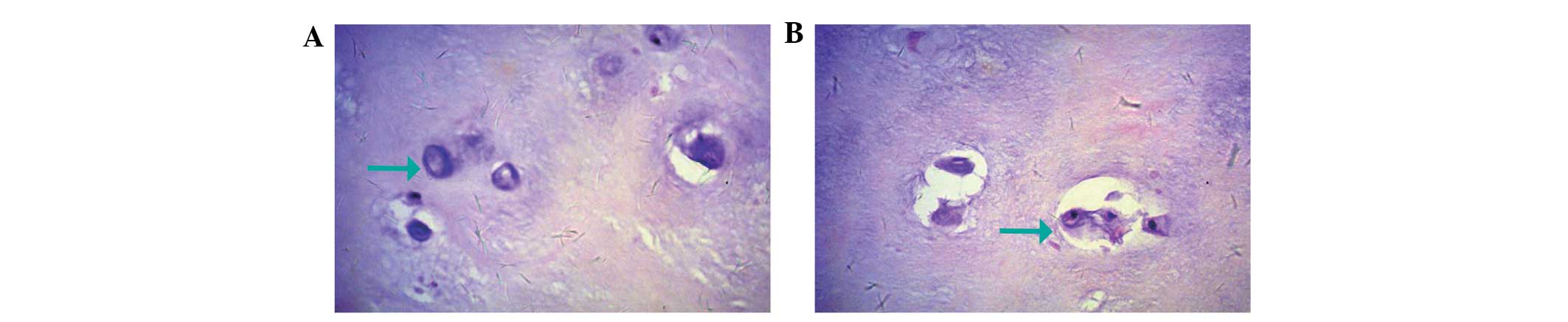
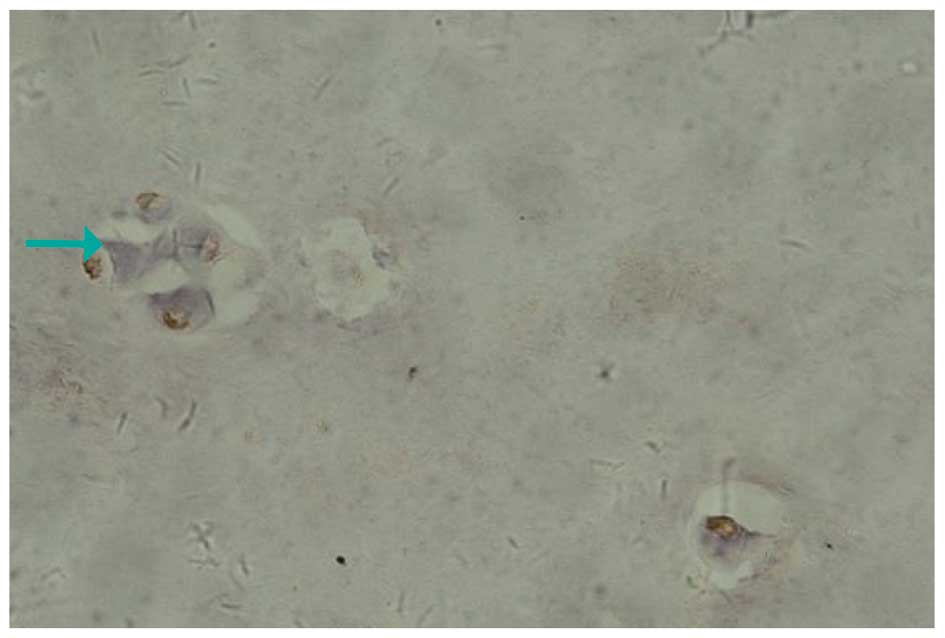
H&E staining
As shown in Fig. 1,
the cell density in the IVD tissue samples was lower and the
distribution of the cell population was markedly inhomogeneous. In
the control group, orbicular-ovate cartilage cells in normal lumbar
IVD presented irregular cartilaginous lacunae. In addition, the
majority of nucleus pulposus cells were isolated in the cellular
lacunae, with a few multinucleated giant cells and cell clusters
occasionally present (Fig. 1A). In
the experimental group, H&E staining revealed that vacuolation
in the cytoplasm of the degenerate nucleus pulposus cells occurred
with large clones of hypertrophic chondrocytes, located in nested
structures. In addition, these large clones of hypertrophic
chondrocytes often appeared surrounding the cracks in the IVD. The
appearance of cracks in the IVDs was an important marker for
degeneration of the IVD (Fig.
1B).
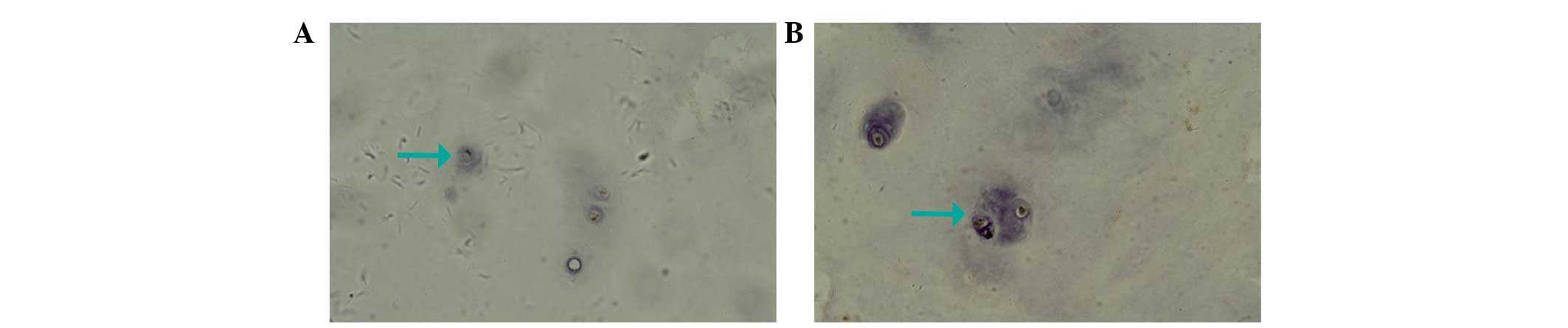
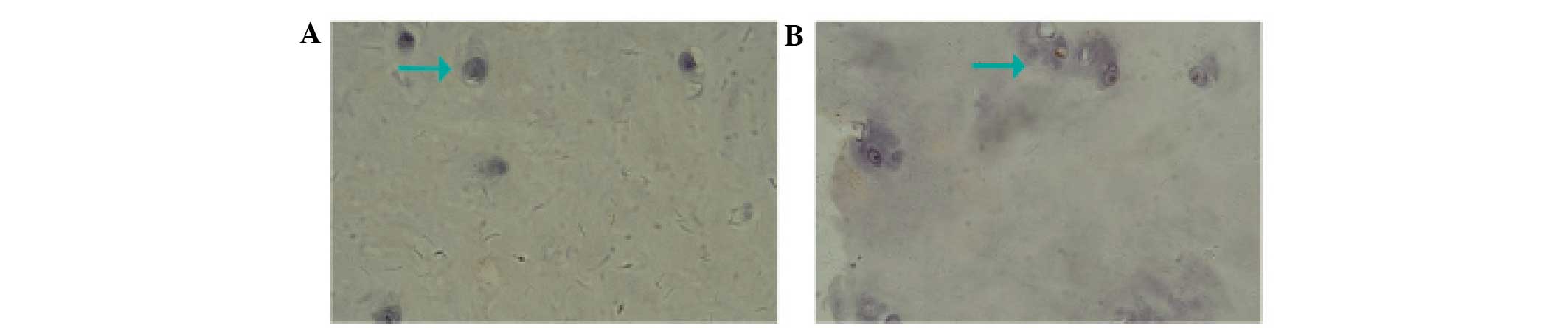
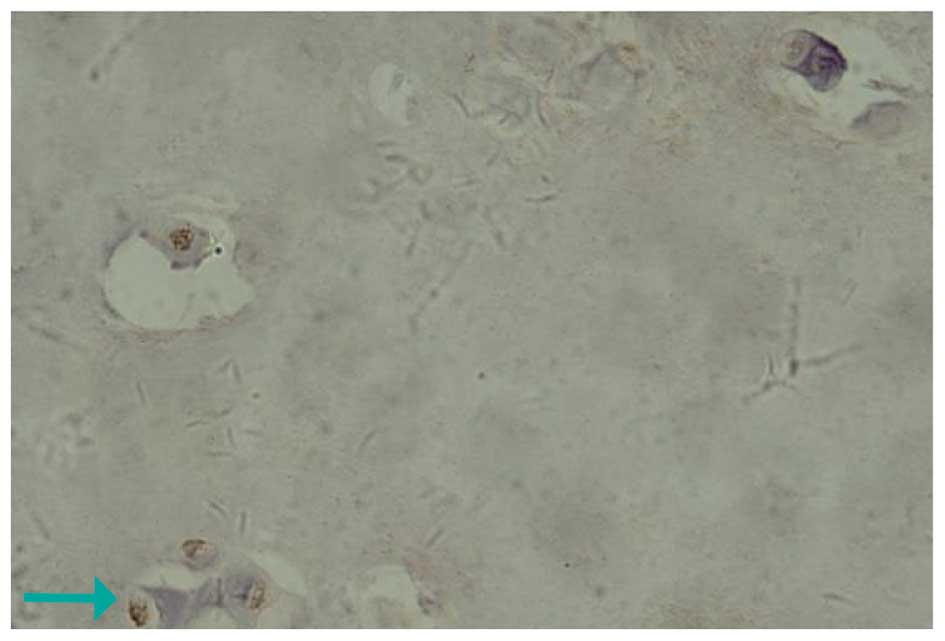
Protein expression of IL-17 and
TNF-α
Fig. 2A and 3A show the expression of IL-17 and TNF-α,
respectively, in the IVD nucleus pulposus tissue samples of the
control group. It was observed that IL-17 and TNF-α in the
cytoplasm presented light yellow/brown staining, suggesting weakly
positive expression. In the experimental group, IL-17 and TNF-α
expression in the cytoplasm of the IVD nucleus pulposus tissue
samples with annulus fibrosus disruption presented dark
yellow/brown staining, which suggested high positive expression
(Figs. 2B and 3B). In addition, IL-17 and TNF-α in the
cytoplasm of IVD nucleus pulposus tissue samples without annulus
fibrosus disruption in the experimental group exhibited positive
expression, presenting yellow/brown or red/brown staining (Figs. 4 and 5).
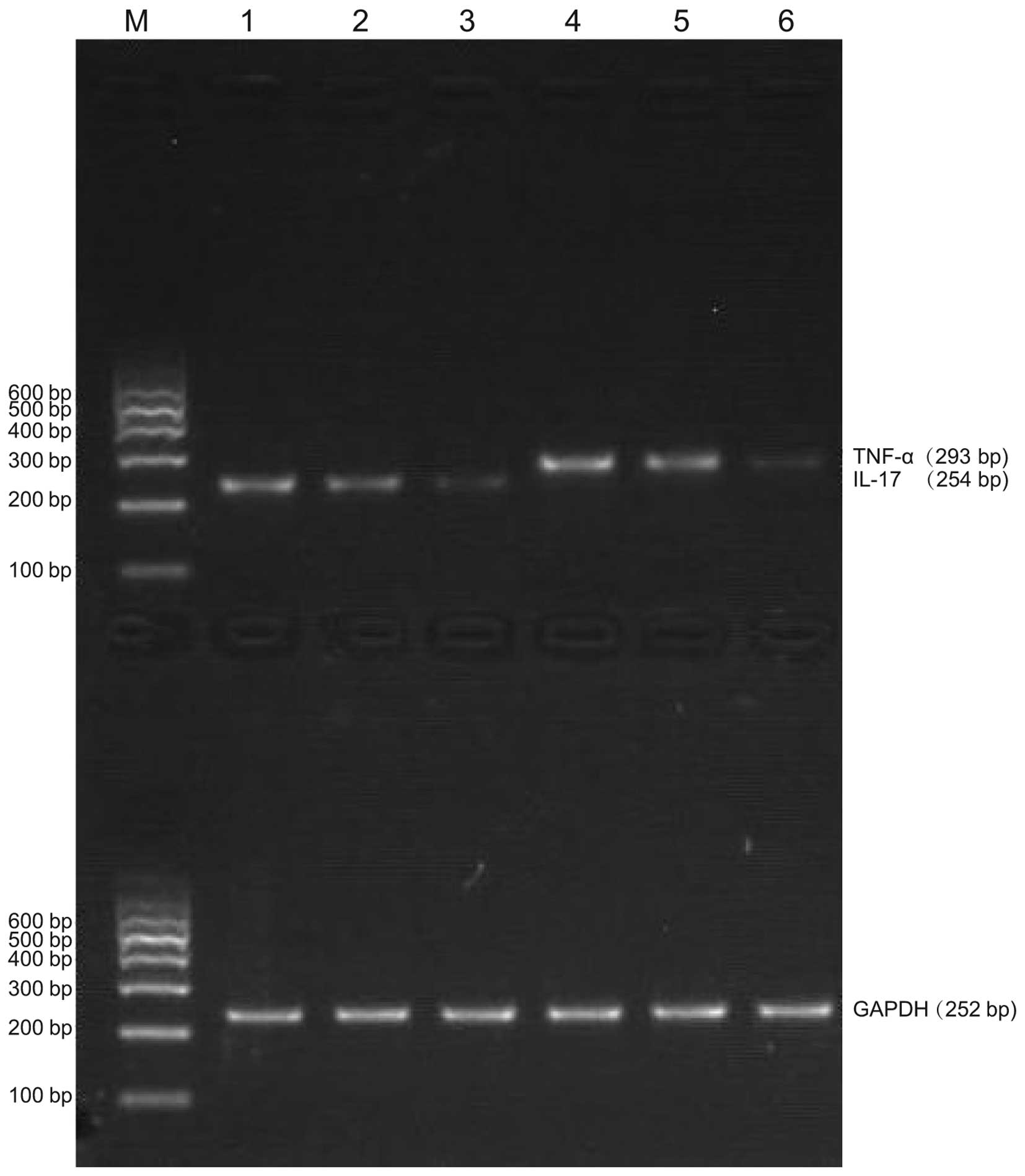
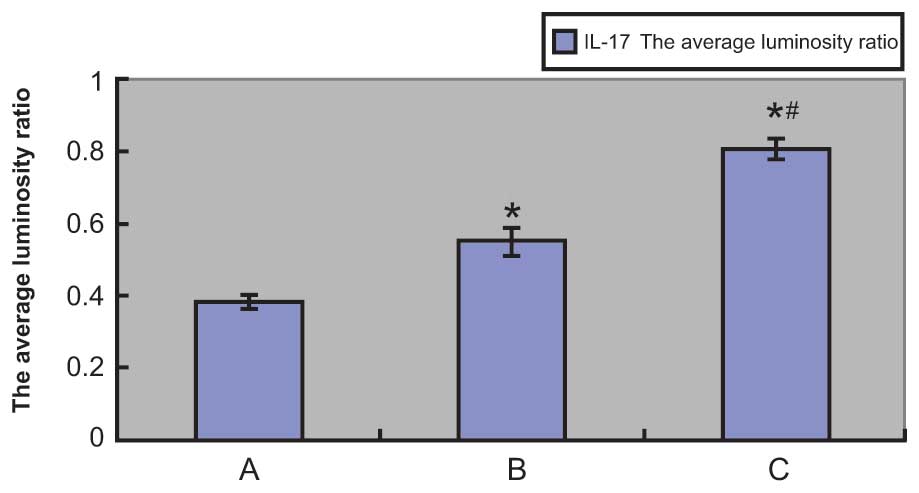
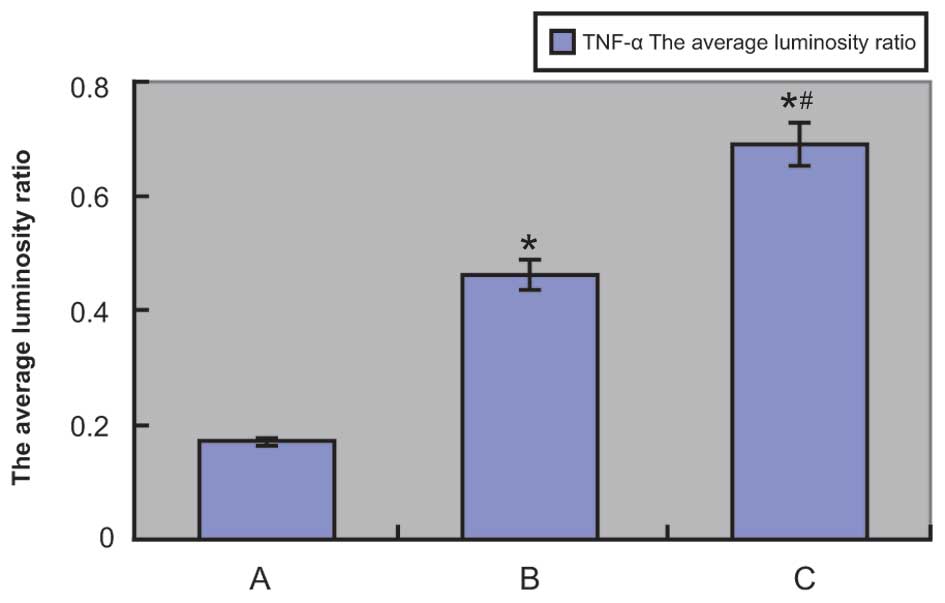
mRNA expression levels of IL-17 and
TNF-α
TNF-α and IL-17 mRNA expression levels were examined
by RT-PCR, which showed TNF-α and IL-17 mRNA expression in both
experimental and control tissue samples. Agarose gel
electrophoresis demonstrated that the sizes of the PCR-amplified
products of TNF-α, IL-17 and GAPDH were 293, 254 and 252 bp,
respectively (Fig. 6). The
absorbance values of IL-17 and TNF-α compared with those of the
internal reference (GAPDH) are shown in Figs. 7 and 8, respectively, and also in Tables III and IV, respectively. The IL-17 mRNA expression
levels in the annulus fibrosus disrupted group and annulus fibrosus
undisrupted group were significantly higher compared with that of
the control group (0.7263±0.0396 and 0.4858±0.0292, respectively,
vs. 0.1788±0.0051; P<0.01 for both). As shown in Table IV, the TNF-α mRNA expression levels
in the annulus fibrosus disrupted group and annulus fibrosus
undisrupted group were both significantly higher compared with that
of the control group (0.8061±0.0292 and 0.5488±0.0365,
respectively, vs. 0.3791±0.0181; P<0.01 for both). Furthermore,
IL-17 and TNF-α mRNA expression levels in the annulus fibrosus
disrupted group were both significantly higher compared with that
in the annulus fibrosus undisrupted group (both P<0.01). The LSD
t-test demonstrated a significant difference in TNF-α and IL-17
mRNA expression levels between the experimental and control groups
and between the annulus fibrosus disrupted and annulus fibrosus
undisrupted groups (all P<0.05; Table III and IV).
 | Table III.Interleukin-17 mRNA expression in the
various groups. |
Table III.
Interleukin-17 mRNA expression in the
various groups.
| Group | No. | Absorbance (mean ±
SD) | F-value | P-value |
|---|
| Control group | 16 | 0.3981±0.0190 | 889.5 | <0.01 |
| Annulus fibrosus
undisrupted group | 24 |
0.5762±0.0383a,b |
|
| Annulus fibrosus
disrupted group | 19 |
0.8464±0.0307a |
|
 | Table IV.Tumor necrosis factor-α mRNA
expression in the various groups. |
Table IV.
Tumor necrosis factor-α mRNA
expression in the various groups.
| Group | No. | Absorbance (mean ±
SD) | F-value | P-value |
|---|
| Control group | 10 | 0.1788±0.0051 | 1,512.0 | <0.01 |
| Annulus fibrosus
undisrupted group | 22 |
0.4858±0.0292a,b |
|
| Annulus fibrosus
disrupted group | 18 |
0.7263±0.0396a |
|
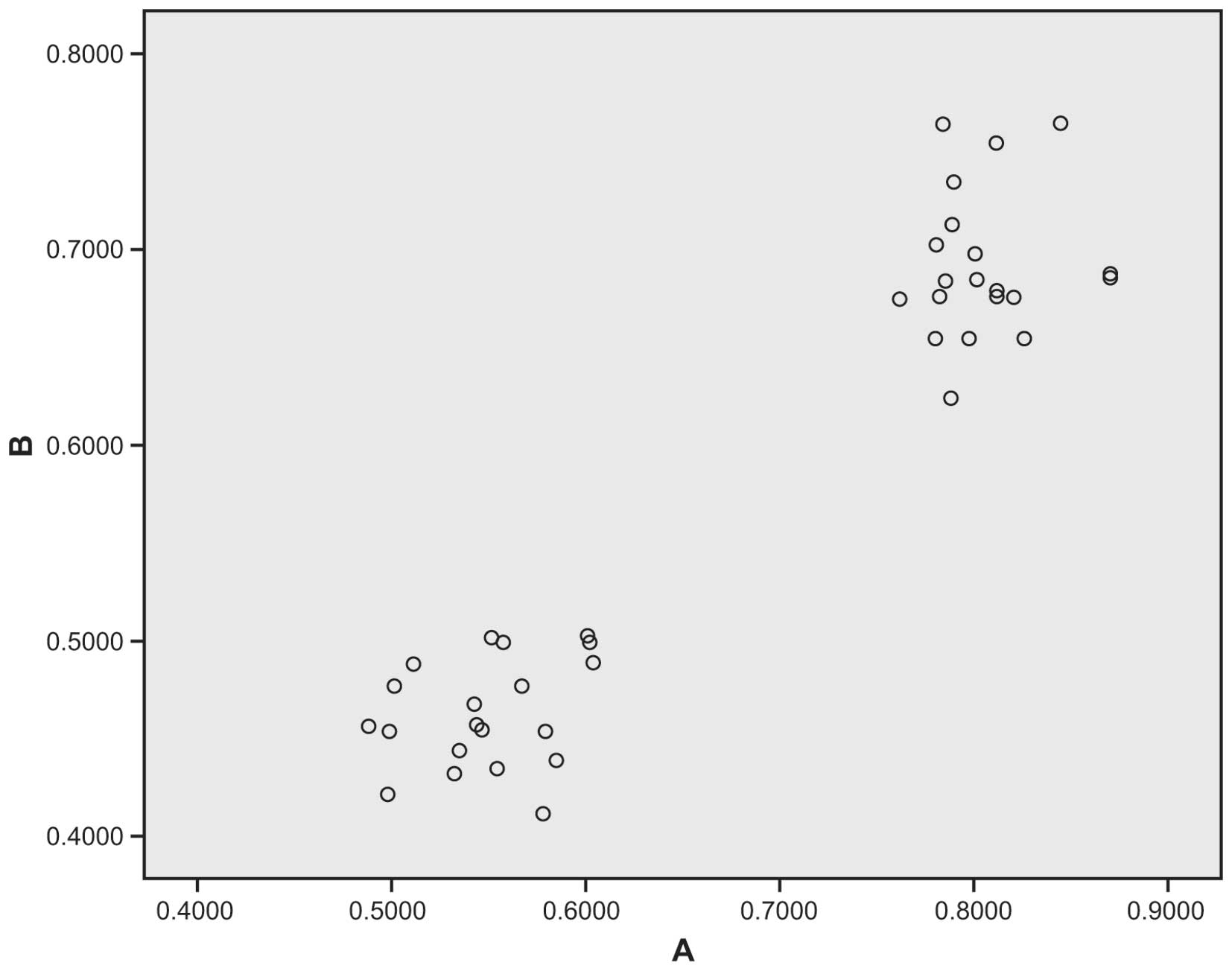
Correlation analysis of IL-17 and
TNF-α mRNA expression
Fig. 9 demonstrates a
correlation between IL-17 and TNF-α mRNA expression in the
experimental group. The average luminosity ratio of IL-17 mRNA
expression to TNF-α mRNA expression suggested a positive
correlation between IL-17 and TNF-α mRNA expression (r=0.957;
P<0.01).
Discussion
The results of present study demonstrate that IL-17
may have an important role during the pathological process of the
degeneration of LDH, and the expression levels of IL-17 may be
associated with the severity of IDD. IL-17 is a known
pro-inflammatory cell factor that regulates and promotes the
secretion of various inflammatory mediators, and underlies the
pathogenesis of various types of inflammatory diseases, including
acute and chronic inflammation (27). Due to its strong pro-inflammatory
properties, IL-17 is the initiation factor for numerous
inflammatory cytokines and is closely associated with inflammatory
diseases, including infection, tumors, allergies, transplantation
and autoimmune diseases, particularly allergic and autoimmune
diseases (34–36). The basic pathology of LDH is thought
to be extracellular matrix degradation, during which MMPs and TIMPs
have an important role in disc extracellular matrix degradation
(37). Furthermore, IL-17
upregulates the expression of MMP-1/3 in chondrocytes and synovial
fibroblasts, and is able to enhance the activity of aggrecanase and
collagen, thereby promoting the degeneration of proteoglycans and
collagen in chondrocytes (38).
Therefore, IL-17 may be involved in the progression of IDD,
although the mechanism underlying this process remains to be
determined, and may contribute to the development of IDD.
The results of the present study also indicated that
TNF-α may take part in the process of IDD, and its expression
levels may be associated with the severity of IDD. Several studies
have demonstrated that TNF-α, a precursor protein synthesized by
catalysis of the TNF-α-converting enzyme and predominantly secreted
by mononuclear cells and macrophages, is a vital cytokine in
immunity, cellular homeostasis, inflammation, and tumor progression
(39,40). TNF-α may stimulate IVD cells to
produce MMP-3, which can degrade the glycoprotein matrix (composed
of laminin, gelatin and fibronectin and elastin), as well as type
II collagen, thereby increasing IDD (29–31). In
the present study, the protein and mRNA expression levels of TNF-α
were higher in the experimental group compared with the control
group, which indicates that TNF-α may be associated with IDD.
The mRNA and protein expression levels of IL-17 and
TNF-α exhibited a positive correlation; previous studies indicate
that this may be due to TNF-α increasing the mRNA stability of
IL-17 and increasing its protein expression levels (19,41,42). The
present study conducted clinical correlation analyses on the
expression levels of IL-17 and TNF-α in degenerative IVD tissue
samples, and determined that the two cytokines were positively
correlated; this is in agreement with previous studies (22,43).
Although the results of the present study identified that IL-17 and
TNF-α were associated, they did not demonstrated that they exhibit
synergistic effects in the pathological processes of IDD; however,
previous studies have demonstrated synergistic effects, therefore
further research to the current study is required (19,27).
These results suggest that IVD cells could produce greater
quantities of inflammatory mediators on the cell surface in
response to the stimulatory effect of the pro-inflammatory
cytokines IL-17 and TNF-α (28,44). In
addition, a possible mechanism underlying the synergistic effects
of IL-17 and TNF-α may be that exposure to TNF-α results in an
increase of IL-17 expression levels, with the upregulated IL-17
expression being indicative of IDD in the tissue samples; in
addition, TNF-α may stabilize mRNA or cellular transcription
processes (41,45).
In conclusion, the results of the present study
demonstrated that IL-17 and TNF-α are potentially involved in the
pathological processes of IDD with positive correlation, and these
cytokines may have synergistic effects. Thus they may act as novel
targets for the prevention and treatment of IDD, and act as
pathological references for future studies. Further clinical and
genetic studies are required in order to elucidate the etiology and
pathogenesis underlying the effects of IL-17 and TNF-α on IDD.
References
|
1
|
Brueck M, Koerholz D, Nuernberger W,
Juergens H, Goebel U and Wahn V: Elimination of l-asparaginase in
children treated for acute lymphoblastic leukemia. Dev Pharmacol
Ther. 12:200–204. 1989.PubMed/NCBI
|
|
2
|
Zou F, Jiang J, Lu F, Ma X, Xia X, Wang L
and Wang H: Efficacy of intradiscal hepatocyte growth factor
injection for the treatment of intervertebral disc degeneration.
Mol Med Rep. 8:118–122. 2013.PubMed/NCBI
|
|
3
|
Siemionow K, An H, Masuda K, Andersson G
and Cs-Szabo G: The effects of age, sex, ethnicity and spinal level
on the rate of intervertebral disc degeneration: A review of 1712
intervertebral discs. Spine (Phila Pa 1976). 36:1333–1339. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xie P, Liu B, Chen R, Yang B, Dong J and
Rong L: Comparative analysis of serum proteomes: Identification of
proteins associated with sciatica due to lumbar intervertebral disc
herniation. Biomed Rep. 2:693–698. 2014.PubMed/NCBI
|
|
5
|
Vural C and Yorukoglu D: Comparison of
patient satisfaction and cost in spinal and general anesthesia for
lumbar disc surgery. Turk Neurosurg. 24:380–384. 2014.PubMed/NCBI
|
|
6
|
Ma D, Liang Y, Wang D, Liu Z, Zhang W, Ma
T, Zhang L, Lu X and Cai Z: Trend of the incidence of lumbar disc
herniation: Decreasing with aging in the elderly. Clin Interv
Aging. 8:1047–1050. 2013.PubMed/NCBI
|
|
7
|
Moliterno JA, Knopman J, Parikh K, Cohan
JN, Huang QD, Aaker GD, Grivoyannis AD, Patel AR, Härtl R and
Boockvar JA: Results and risk factors for recurrence following
single-level tubular lumbar microdiscectomy. J Neurosurg Spine.
12:680–686. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hirose Y, Chiba K, Karasugi T, Nakajima M,
Kawaguchi Y, Mikami Y, Furuichi T, Mio F, Miyake A, Miyamoto T, et
al: A functional polymorphism in THBS2 that affects alternative
splicing and MMP binding is associated with lumbar-disc herniation.
Am J Hum Genet. 82:1122–1129. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim KT, Park SW and Kim YB: Disc height
and segmental motion as risk factors for recurrent lumbar disc
herniation. Spine (Phila Pa 1976). 34:2674–2678. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhao B, Yu Q, Li H, Guo X and He X:
Characterization of microRNA expression profiles in patients with
intervertebral disc degeneration. Int J Mol Med. 33:43–50.
2014.PubMed/NCBI
|
|
11
|
Zhang YG, Zhang F, Sun Z, Guo W, Liu J,
Liu M and Guo X: A controlled case study of the relationship
between environmental risk factors and apoptotic gene polymorphism
and lumbar disc herniation. Am J Pathol. 182:56–63. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Purmessur D, Walter BA, Roughley PJ,
Laudier DM, Hecht AC and Iatridis J: A role for TNFα in
intervertebral disc degeneration: A non-recoverable catabolic
shift. Biochem Biophys Res Commun. 433:151–156. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Andrade P, Hoogland G, Garcia MA,
Steinbusch HW, Daemen MA and Visser-Vandewalle V: Elevated IL-1β
and IL-6 levels in lumbar herniated discs in patients with sciatic
pain. Eur Spine J. 22:714–720. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xu D, Sun Y, Bao G, Liu W, Zhu X, Cui S,
Fan J and Cui Z: MMP-1 overexpression induced by IL-1β: Possible
mechanism for inflammation in degenerative lumbar facet joint. J
Orthop Sci. 18:1012–1019. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Onishi RM and Gaffen SL: Interleukin-17
and its target genes: Mechanisms of interleukin-17 function in
disease. Immunology. 129:311–321. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Iwakura Y, Ishigame H, Saijo S and Nakae
S: Functional specialization of interleukin-17 family members.
Immunity. 34:149–162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kaplan MH, Glosson NL, Stritesky GL, Yeh
N, Kinzfogl J, Rohrabaugh SL, Goswami R, Pham D, Levy DE,
Brutkiewicz RR, et al: STAT3-dependent IL-21 production from T
helper cells regulates hematopoietic progenitor cell homeostasis.
Blood. 117:6198–6201. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Neurath MF and Finotto S: IL-6 signaling
in autoimmunity, chronic inflammation and inflammation-associated
cancer. Cytokine Growth Factor Rev. 22:83–89. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gabr MA, Jing L, Helbling AR, Sinclair SM,
Allen KD, Shamji MF, Richardson WJ, Fitch RD, Setton LA and Chen J:
Interleukin-17 synergizes with IFNγ or TNFα to promote inflammatory
mediator release and intercellular adhesion molecule-1 (ICAM-1)
expression in human intervertebral disc cells. J Orthop Res.
29:1–7. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chiricozzi A, Guttman-Yassky E,
Suarez-Fariñas M, Nograles KE, Tian S, Cardinale I, Chimenti S and
Krueger JG: Integrative responses to IL-17 and TNF-α in human
keratinocytes account for key inflammatory pathogenic circuits in
psoriasis. J Invest Dermatol. 131:677–687. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Leppkes M, Roulis M, Neurath MF, Kollias G
and Becker C: Pleiotropic functions of TNF-α in the regulation of
the intestinal epithelial response to inflammation. Int Immunol.
26:509–515. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Risbud MV and Shapiro IM: Role of
cytokines in intervertebral disc degeneration: Pain and disc
content. Nat Rev Rheumatol. 10:44–56. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chu WM: Tumor necrosis factor. Cancer
Lett. 328:222–225. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fallahi-Sichani M, El-Kebir M, Marino S,
Kirschner DE and Linderman JJ: Multiscale computational modeling
reveals a critical role for TNF-α receptor 1 dynamics in
tuberculosis granuloma formation. J Immunol. 186:3472–3483. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Le Maitre CL, Pockert A, Buttle DJ,
Freemont AJ and Hoyland JA: Matrix synthesis and degradation in
human intervertebral disc degeneration. Biochem Soc Trans.
35:652–655. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sun Z, Wang HQ, Liu ZH, Chang L, Chen YF,
Zhang YZ, Zhang WL, Gao Y, Wan ZY, Che L, et al: Down-regulated CK8
expression in human intervertebral disc degeneration. Int J Med
Sci. 10:948–956. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Miossec P and Kolls JK: Targeting IL-17
and TH17 cells in chronic inflammation. Nat Rev Drug Discov.
11:763–776. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shamji MF, Setton LA, Jarvis W, So S, Chen
J, Jing L, Bullock R, Isaacs RE, Brown C and Richardson WJ:
Proinflammatory cytokine expression profile in degenerated and
herniated human intervertebral disc tissues. Arthritis Rheum.
62:1974–1982. 2010.PubMed/NCBI
|
|
29
|
Moe KT, Khairunnisa K, Yin NO,
Chin-Dusting J, Wong P and Wong MC: Tumor necrosis factor-α-induced
nuclear factor-kappaB activation in human cardiomyocytes is
mediated by NADPH oxidase. J Physiol Biochem. 70:769–779. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang YF, Chen PY, Chang W, Zhu FQ, Xu LL,
Wang SL, Chang LY, Luo J and Liu GJ: Clinical significance of tumor
necrosis factor-α inhibitors in the treatment of sciatica: A
systematic review and meta-analysis. PLoS One. 9:e1031472014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ślebioda TJ and Kmieć Z: Tumour necrosis
factor superfamily members in the pathogenesis of inflammatory
bowel disease. Mediators Inflamm. 2014:3251292014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fardon DF and Milette PC: Combined Task
Forces of the North American Spine Society, American Society of
Spine Radiology, and American Society of Neuroradiology:
Nomenclature and classification of lumbar disc pathology. Spine.
26:E93–E113. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Pfirrmann CW, Metzdorf A, Zanetti M,
Hodler J and Boos N: Magnetic resonance classification of lumbar
intervertebral disc degeneration. Spine (Phila Pa 1976).
26:1873–1878. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Miossec P: IL-17 and Th17 cells in human
inflammatory diseases. Microbes Infect. 11:625–630. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xu B, Guenther JF, Pociask DA, Wang Y,
Kolls JK, You Z, Chandrasekar B, Shan B, Sullivan DE and Morris GF:
Promotion of lung tumor growth by interleukin-17. Am J Physiol Lung
Cell Mol Physiol. 307:L497–L508. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Herold R, Rosenbloom J and Granovsky M:
Phylogenetic distribution of enamel proteins: Immunohistochemical
localization with monoclonal antibodies indicates the evolutionary
appearance of enamelins prior to amelogenins. Calcif Tissue Int.
45:88–94. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kozaci LD, Guner A, Oktay G and Guner G:
Alterations in biochemical components of extracellular matrix in
intervertebral disc herniation: Role of MMP-2 and TIMP-2 in type II
collagen loss. Cell Biochem Funct. 24:431–436. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sylvester J, Liacini A, Li WQ and
Zafarullah M: Interleukin-17 signal transduction pathways
implicated in inducing matrix metalloproteinase-3, −13 and
aggrecanase-1 genes in articular chondrocytes. Cell Signal.
16:469–476. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Liu S, Liu S, Wang Y and Liao Z: The
P2/P2′ sites affect the substrate cleavage of TNF-alpha converting
enzyme (TACE). Mol Immunol. 62:122–128. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wu Y and Zhou BP:
TNF-alpha/NF-kappaB/Snail pathway in cancer cell migration and
invasion. Br J Cancer. 102:639–644. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gruber HE, Hoelscher GL, Ingram JA, Norton
HJ and Hanley EN Jr: Increased IL-17 expression in degenerated
human discs and increased production in cultured annulus cells
exposed to IL-1β and TNF-α. Biotech Histochem. 88:302–310. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhu S and Qian Y: IL-17/IL-17 receptor
system in autoimmune disease: Mechanisms and therapeutic potential.
Clin Sci (Lond). 122:487–511. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang XP: Preliminary study on the
relationship between type 2 diabetic patients with atrial
fibrillation. Xin Nao Xue Guan Bing Fang Zhi. 11:201–202. 2011.(In
Chinese).
|
|
44
|
Hot A, Lavocat F, Lenief V and Miossec P:
Simvastatin inhibits the pro-inflammatory and pro-thrombotic
effects of IL-17 and TNF-α on endothelial cells. Ann Rheum Dis.
72:754–760. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Di Martino A, Merlini L and Faldini C:
Autoimmunity in intervertebral disc herniation: From bench to
bedside. Expert Opin Ther Targets. 17:1461–1470. 2013. View Article : Google Scholar : PubMed/NCBI
|