Introduction
Orthotopic liver transplantation has become the
primary treatment for patients with end-stage liver diseases
(1). It is well known that the high
mortality of end-stage liver disease is a global public health
problem. The clinical manifestation usually involve cirrhosis
caused by different pathological factors, and the prognosis is poor
for those with decompensated cirrhosis, which is defined by the
presence of ascites, variceal bleeding, encephalopathy and/or
jaundice (2). In China, liver
failure of the majority of liver transplant recipients is due to
hepatitis-induced liver cirrhosis, typically combined with portal
hypertension; due to the presence of extensive collateral
circulation, in the anhepatic phase, recirculation of blood is
possible (3). Therefore,
transplantation without veno-venous bypass is the primary type of
surgery (3). Currently, problems
occur in the anhepatic and post-anhepatic phases, such as
hemodynamic instability, metabolic disturbances, and
ischemia-reperfusion injuries, which have attracted great attention
(4,5). Animal models are important tools with
which to investigate these problems, several types of animal models
of portal hypertension are currently available, such as drug
induced models, and common bile duct ligation models, however,
there are a number of major defects in traditional liver
transplantation models, such as the inability to reproduce the
postoperative recovery phase, high levels of complexity and high
mortality rates (6). Therefore,
based on the classical partial portal vein ligation method, the aim
of the present study was to establish a model by which the whole
liver transplantation process, in particular the postoperative
recovery phase, could be reproduced.
Materials and methods
Animals and treatments
8-week old Male Wistar rats (n=135; 250–300 g body
mass) were obtained from the Experimental Animal Center of Hebei
Medical University (Shijiazhuang, China) and were housed under the
same controlled conditions with a temperature of 25±2°C and a
humidity of 50±10%. Rats were fed with standard laboratory chow and
water ad libitum. All the experimental procedures were under the
approval of the Ethical Committee of the Animal Experiment Center
of Hebei Medical University (no. HEBU-2012-02).
Following 1 week of acclimatization, rats were
randomly allocated into three groups (15 in each group). Rats in
the normal control (NC) group underwent a sham surgery; rats in the
portal hypertensive control (PHTC) group underwent partial
portal-vein ligation; and rats in the reperfusion (R) group
underwent partial portal vein ligation as in the PHTC group, then
were subjected to portal vein and inferior vena cava clamping for 1
h, followed by reperfusion for different time periods (0, 6, 12,
24, 48 and 72 h, and 7 days). Free portal pressure (FPP) was
measured and portal venography was performed 3 weeks after portal
vein ligation or the sham surgery. Other parameters measured
included arterial oxygen pressure (PaO2), and
biochemical parameters including alanine aminotransferase (ALT),
aspartate aminotransferase (AST) and total bilirubin (TBil)
expression levels. In addition, pathologic examinations were
performed.
Surgical procedure
All groups received a subcutaneous injection of 2%
atropine (0.05 mg/kg body mass), and low molecular weight heparin
sodium (625 U/kg body mass). After 30 min, rats were anesthetized
with 2% ketamine (200 mg/kg body mass; intraperitoneal injection)
and a 2 cm midline abdominal incision was made. In the PHTC and R
groups, the portal vein was located and surgically isolated from
surrounding tissues. The isolated vessel was stenosed by applying a
3-0 silk thread around the vein, together with an adjacent 20-gauge
blunt-tipped needle and a label ring (made from a 4-F Fogarty
embolectomy catheter, with an external diameter of 1 mm and ~1.5 cm
circumference) lying along the portal vein. After removal of the
needle and adjustment of the location of the label ring (in order
to prevent its potential vein-twisting effect), the efficacy of
partial ligation of the vein was confirmed by observing the
increase in the diameter of the vessel prior to ligation, without
thrombus or tissue necrosis. Then, the abdominal wall was sutured.
Rats in the NC group underwent the same experimental procedure,
minus the stenosing of the isolated portal vein. Following surgery,
rats were housed for 3 weeks to develop portal hypertension in the
corresponding groups.
In the R group, rats received the same treatment as
those in the PHTC group prior to a second surgical procedure
conducted 3 weeks after the first surgery. After anesthesia, rats
received Ringer's lactate (5 ml/h) and heparin sodium (625 U/kg of
body mass) by intubation with a micro-pump in the left external
jugular vein; the left carotid artery was intubated and connected
with an eight-channel physiological recorder (Beijing Electronic
Instrument Factory, Beijing, China) in order to monitor the
arterial blood pressure. A 2 cm incision below the right costal
margin was made, and bleeding due to the abdominal wall vein
varices was stopped by continuous suture of the surgical margin.
The first portal was exposed as indicated by the label ring placed
along the portal vein in the first stage surgery, and then the
label ring was cut down and removed to restore the portal vein.
After exposing the inferior vena cava (above the renal vein, below
the liver), the first portal and the inferior vena cava were
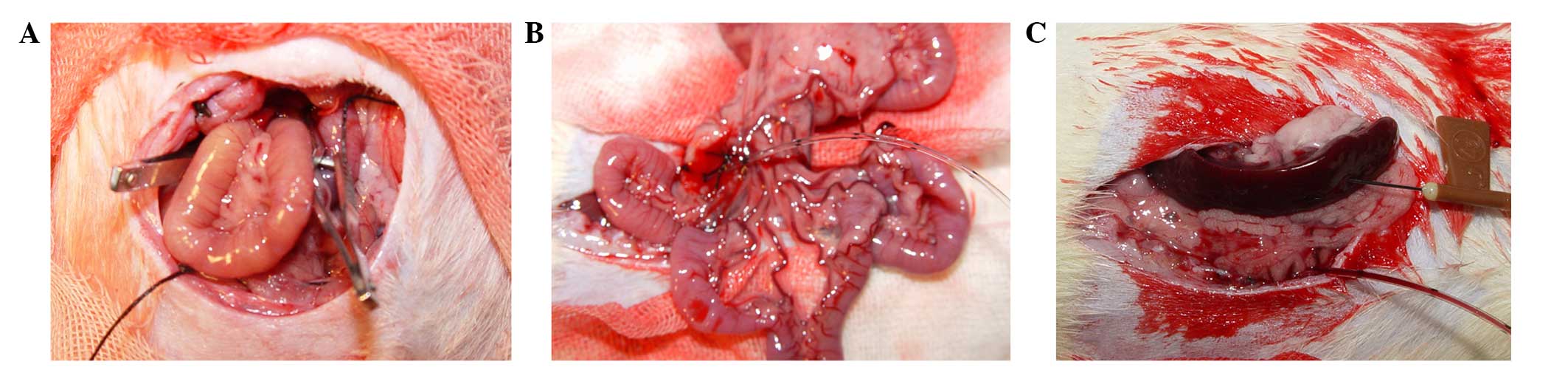
clamped with non-invasive vascular clamps (Fig. 1A). After 60 min, the clamps were
removed and the abdominal wall was sutured.
Portal pressure measurement
Following anesthesia, a 2-cm incision along the
right rectus abdominis was made. A segment of the mesenteric branch
vein was cannulated with a 3-F epidural catheter (Fig. 1B), and the tip of a 25 cm catheter
was advanced into the trunk of portal vein, and the length inserted
was 0.5 cm. The portal pressure was recorded using the pressure
transducer of the eight-channel physiological recorder. The spinal
value was regarded as zero.
Portal venography
Once the portal pressure had been recorded, a
22-gauge needle was introduced into the splenic pulp and 38%
meglumine diatrizoate was injected through the 3-F epidural
catheter using a 22-gauge needle at a rate of 1 ml/3 sec (Fig. 1C). Rats in the R group were injected
with meglumine diatrizoate again at the same administration rate as
before once the label ring had been removed; photographic images
were captured and analyzed using the AX-II 500 mA remote controlled
gastrointestinal X-ray machine (Shimadzu Corporation, Kyoto, Japan)
and IDR-700 digital X-ray diagnosis system (Shimadzu
Corporation).
PaO2 and biochemical
parameter analysis
Blood samples (1 ml) from the abdominal aorta were
obtained for PaO2 measurement using a blood gas analyzer
(Bayer Rapidlab 865; Bayer AG, Fernwald, Germany), and 3-ml blood
samples from the inferior vena cava were centrifuged (1,789xg, 5
min). Levels of ALT, AST and TBil in the serum were analyzed using
an automatic biochemical analyzer (Olympus AU2700; Olympus
Corporation, Tokyo, Japan).
Pathological examination
Anesthesia was performed with 2% ketamine at a dose
of 200 mg/kg. Following anesthesia and sacrifice by cervical
dislocation, 3-mm segments of the lower esophagus were dissected
from rats 3 weeks after ligation. The left lobe of the liver was
dissected from rats 3 weeks after ligation, or at different
reperfusion time points (0, 6, 12, 24, 48 and 72 h, and 7 days).
Then, 3-µm sections of esophagus or liver tissue were fixed in 10%
buffered formalin, embedded in Paraplast and stained using
hematoxylin and eosin (H&E). Pathological examination was
performed using light microscopy (Olympus BX51; Olympus
Corporation), images were recorded, and the vein areas in each
section of the esophageal mucosa were quantified using the
RM6240B/C multichannel bio-signal collection processing system
(Chengdu Implement Co., Chengdu, China).
Statistical analysis
Data are expressed as mean ± standard deviation, and
were compared using one-way analysis of variance followed by
Bonferroni multiple comparison test. P<0.05 was considered to
indicate a statistically significant difference. Statistical
calculations were performed using SPSS version 13.0 software (SPSS,
Inc., Chicago, IL, USA).
Results
Gross observations and measurement of
the submucosal vein area in the lower esophagus
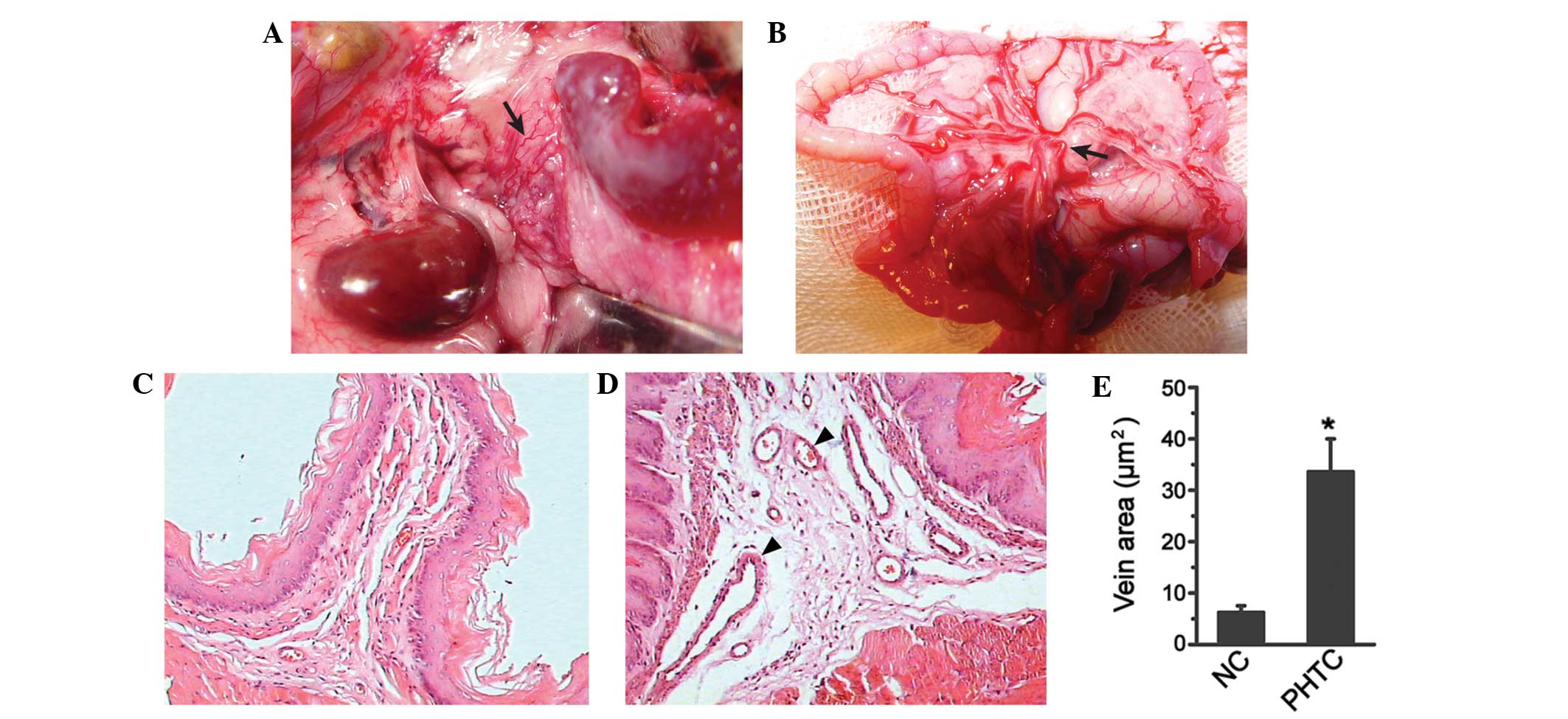
Three weeks following portal vein ligation,
gastric-esophageal vein varices were observed, and the kidneys and
spleen were observed to be enlarged and dark red in color.
Intestinal wall and mesenteric vein varices were also observed,
together with edema of the intestinal wall in the PHTC group
(Fig. 2A and B). Microscopic
examination of the esophagus showed that the submucosal vein in the
lower esophagus was dilated in the PHTC group, and the vein area
(33.58±6.42 µm2) was significantly higher compared with
that of the NC group (5.62±1.30 µm2; P<0.05; Fig. 2C-E).
Portal venography and portal pressure
measurement
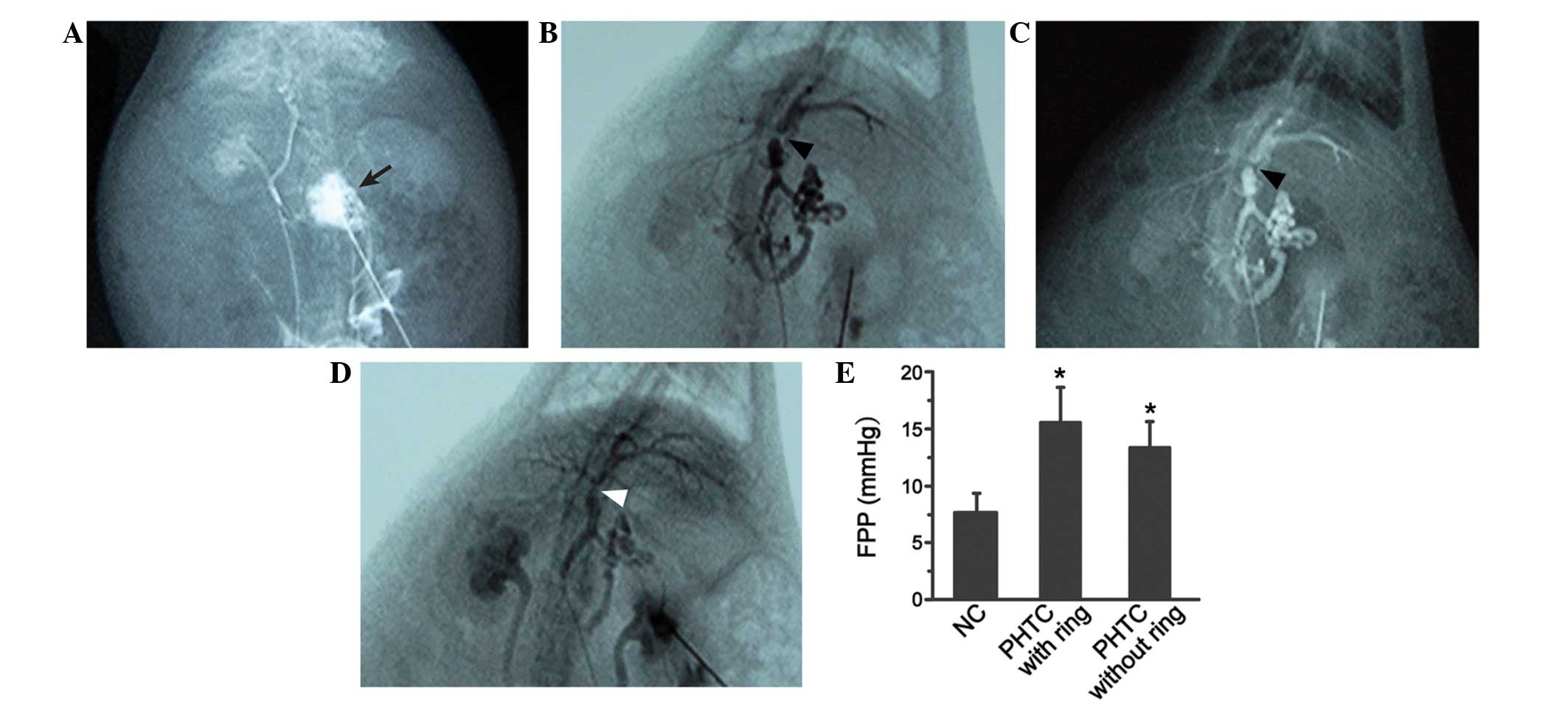
Portal venography results demonstrated that, in the
NC group, the portal vein trunk and its branches were natural in
shape, without the presence of portal-systemic collateral
circulations (Fig. 3A). In the PHTC
group, portal veins were tortuous, and significant narrowing was
observed in the vein trunk near the branches (Fig. 3B and C). In the R group, following
the removing of the label ring, the constricted vein was restored
(Fig. 3D).
The FPP in the NC group was 7.7±1.7 mmHg; while the
FPP in the PHTC group with ring was 15.6±3.1 mmHg, which was
significantly higher compared with that of the NC group
(P<0.05). In addition, the FPP in the PHTC group without the
ring (measured immediately after the ring was removed) was 13.4±2.3
mmHg, which was significantly higher compared with that of the NC
group (P<0.05); however, there was no significant difference
between the PHTC groups with and without the ring (P>0.05;
Fig. 3E).
Serum biochemical parameters and
PaO2
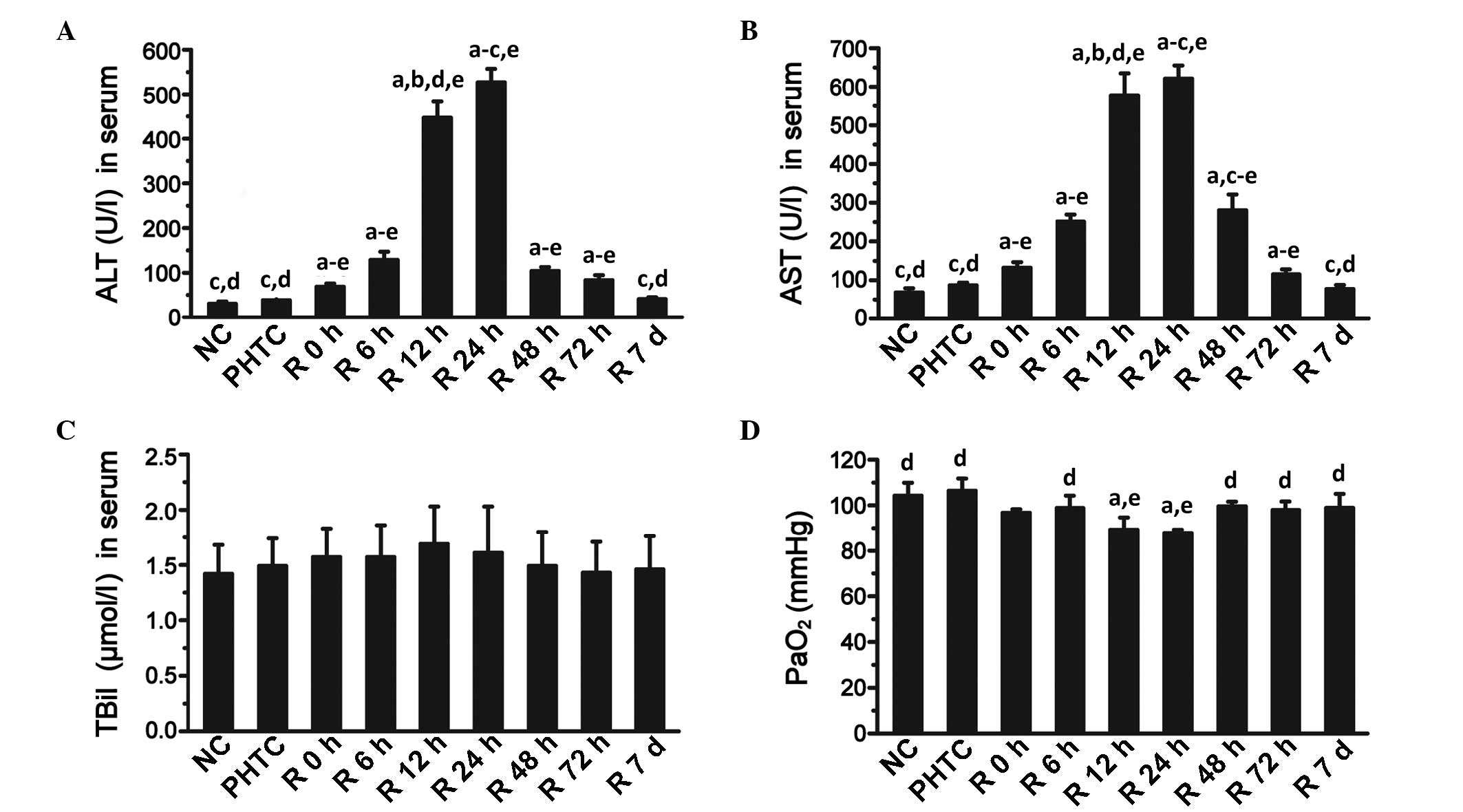
There were no significant differences in the serum
levels of ALT and AST between the NC group and the PHTC group.
However, ALT and AST serum expression levels were significantly
increased in the R group after 0 h, 6 h, 12 h, 24 h, 48 h and 72 h
of reperfusion, compared with the NC or PHTC groups (all
P<0.05); the levels of these two enzymes reached their maximum
values at 24 h after reperfusion. At 7 days, the ALT and AST serum
levels were decreased and comparable with those of the NC or PHTC
groups (Fig. 4A and B). With regards
to TBil, there were no significant differences in serum expression
levels between all groups (Fig. 4C).
In addition, the PaO2 value was significantly decreased
in the R24 h group compared with the NC or PHTC groups (Fig. 4D) (all P<0.05).
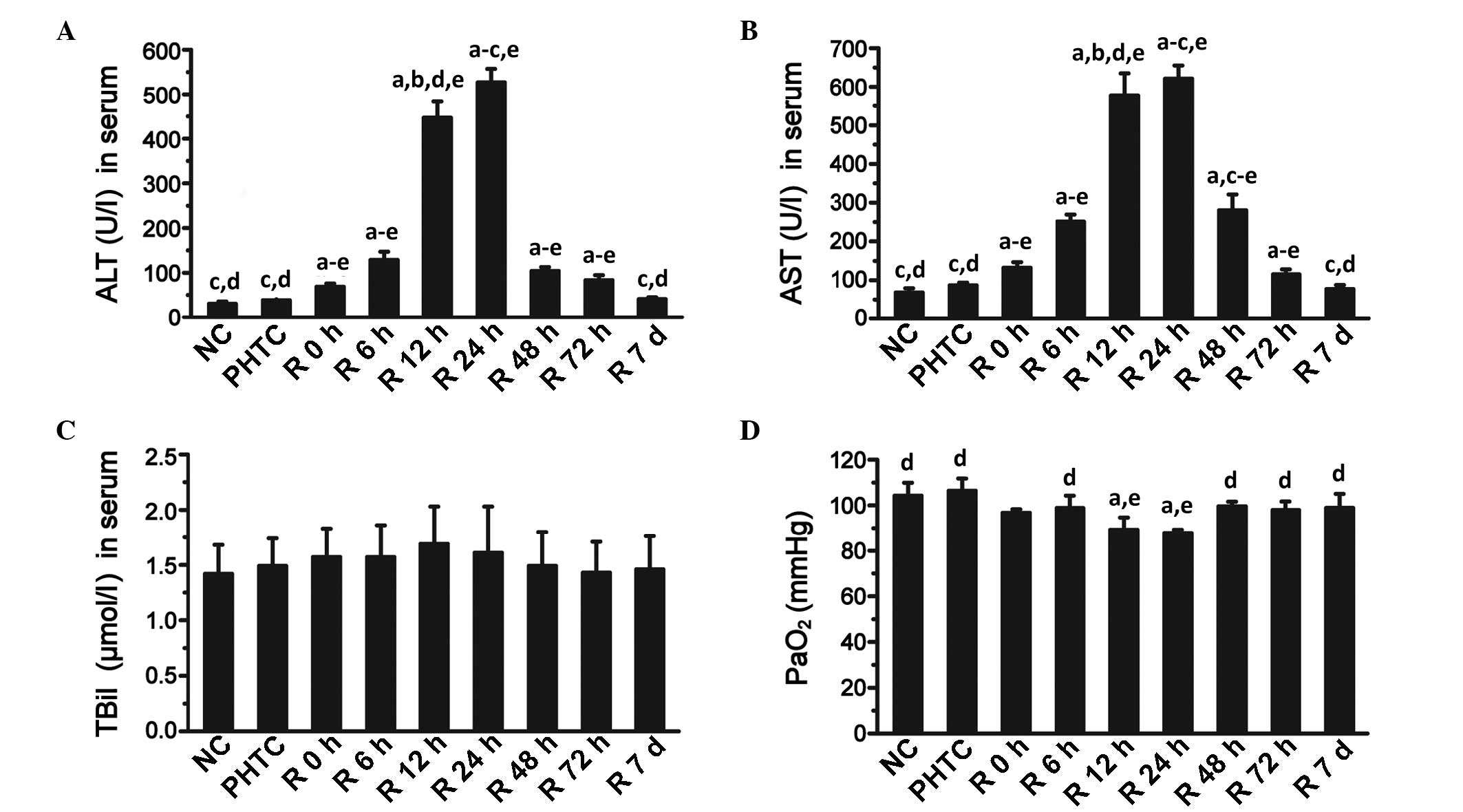 | Figure 4.Serum biochemical parameters and
PaO2. (A) ALT, (B) AST and (C) TBil serum levels, and
(D) PaO2 were measured in the NC, PHTC and R groups. In
the R group, measurements were made at 0, 6, 12, 24, 48 and 72 h,
and 7 days (d). aP<0.05 vs. NC; bP<0.05
vs. PHTC; cP<0.05 vs. R 12 h; dP<0.05
vs. R 24 h; eP<0.05 vs. R 7 d. Values are presented
as mean ± standard deviation (n=15). ALT, alanine aminotransferase;
AST, aspartate aminotransferase; TBil, total bilirubin;
PaO2, arterial oxygen pressure; NC, normal control;
PHTC, portal hypertensive control; R, reperfusion. |
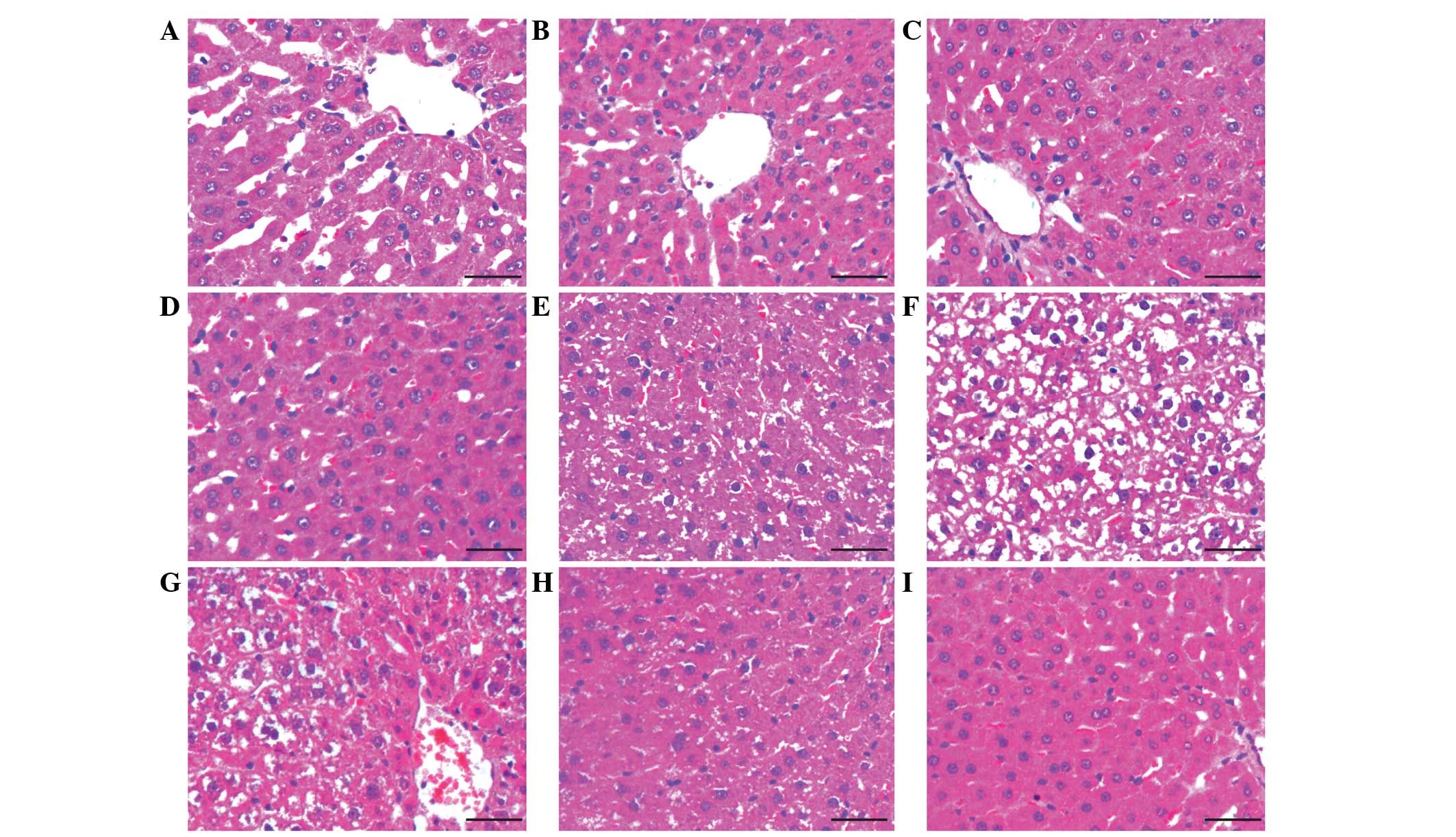
Liver pathology examination
H&E-stained slides were investigated using light
microscopy. Results demonstrated that in the NC and PHTC groups,
liver cells were well organized, and the hepatic lobules were
well-arranged without liver cell edema or neutrophil infiltration.
In the R group at 6 h, the liver cell morphology and structure
appeared normal; mild liver cell edema was observed while the
hepatic lobule structure was maintained; in the R group at 12 h,
prominent liver cell edema and a small number of infiltrating
granulocytes were observed. In the R group at 24 h, a number of
liver cells had become necrotic, and a large quantity of
infiltrating granulocytes were observed. These pathological
appearances were alleviated in the R group at 48 h and 72 h, and
the cells were almost restored to normal in the R group after 7
days (Fig. 5).
Discussion
Orthotopic liver transplantation without veno-venous
bypass, in which the first portal vein and inferior vena cava are
clamped simultaneously, has become a mainstream method of surgery
in China (3,5). It is advantageous as there is no need
to dissect the second portal vein, the liver can be rapidly
removed, and complications caused by veno-venous bypass or outflow
tract obstruction are avoided. However, the incidence of
perioperative complications remains high due to the occurrence of
ischemia-reperfusion injury during the process (7). Therefore, it is imperative to establish
a model of reversible pre-hepatic portal hypertension and thus to
simulate the anhepatic phase of orthotopic liver transplantation
without veno-venous bypass, for the purpose of studying different
aspects of this process.
Numerous types of animal models of portal
hypertension are currently available, including the following: i)
Drug induced models, in which carbon tetrachloride (8), thioacetamide (9) or dimethylnitrosamine (10) is used to induce liver injury.
Although prominent cirrhosis and portal hypertension are present in
these models, portal-systemic collateral circulation is not
evident, and longer time periods of induction may be required
(11–15 weeks). In addition, portal hypertension is irreversible in
these models and thus cannot be used to simulate the liver
transplantation process (11,12). ii)
Common bile duct ligation models, in which bile duct ligation or
dissection, cirrhosis, portal hypertension and portal-systemic
collateral circulation can be established in 25–28 days. However,
in these models, increases in portal pressure are not evident
(13) and no typical pseudolobules
are formed in the liver (14). iii)
Partial portal vein ligation models, which are easy to reproduce
and inexpensive. Presinusoidal portal hypertension develops quickly
in these models, and 1 week after portal vein ligation, portal
hypertension and portal-systemic collateral circulation can be
observed (15). In preliminary
experiments for the present study, the use this model was
attempted; however, a number of shortcomings were found when this
model was used for the purpose of simulating the liver
transplantation process. Firstly, heavy adhesion was observed near
the first portal vein, which was difficult to dissect, thus the
bleeding increased. Secondly, changes to the portal vein were
irreversible, despite the ligation being opened. iv) Other models,
such as portal hypertension models without liver fibrosis induced
by feeding rats with methionine and choline deficient feed
(16), and injecting rats with 80-µm
micro-balls through the portal vein (17). In summary, all of the aforementioned
models are not suitable for accurately simulating the process of
liver transplantation, including the pre-operative cirrhosis
combined with portal hypertension, the intraoperative anhepatic
phase and the postoperative portal pressure recovery phase.
Based on the portal vein ligation model, the present
study established a reversible model of pre-hepatic portal
hypertension in rats. In the first stage of surgery, the trunk of
the portal vein was stenosed with an adjacent 20-gauge blunt-tipped
needle and a label ring; then, the needle was removed to partially
constrict the portal vein [the diameter of the needle and label
ring together was 1.9 mm, which is longer than that of the portal
vein (1.5 mm-1.8 mm)]. In addition to making the portal vein
recoverable, the application of a label ring may also be used as a
marker, following which the first portal vein can be easily
exposed, thus reducing the difficulty of the surgery and reducing
the level of bleeding.
The results in the present study demonstrate that,
in accordance with classical partial portal vein ligation models,
during the first surgical period, the FPP in the PHTC group was
significantly elevated compared with that in the NC group, and
ascites, varicose epigastric and visceral veins were observed. In
addition, the submucosal vein area in the lower esophagus was
significantly increased in the PHTC group compared with the NC
group. Portal venography results demonstrated that typical
portal-systemic collateral circulation had been developed. During
the second surgical period, significant ischemia-reperfusion injury
in the liver was observed in the histological examination, serum
biochemical parameters (ALT, AST and TBil) and arterial
PaO2 measurements. In addition, due to the recovery of
the constricted portal vein in the R group, the portal pressure and
vein varices were attenuated gradually, and the portal-systemic
collateral circulation gradually disappeared. These changes share
great similarities with the clinical post-operative state of liver
transplantation (18).
There are a number of shortcomings in the present
model. Firstly, a certain level of surgical skill is required to
perform the number of steps involved in the surgery. Secondly, the
introduction of the label ring may increase the incidence of
postoperative infection. Finally, typical pseudolobules in the
liver may not develop in the model, which limits its application.
This is due to the fact that the portal hypertension induced in the
model is more evident than drug-induced models or common bile duct
ligation models. However, there are still differences between the
liver tissues of the portal hypertension model and the realistic
portal hypertension, as the latter are usually induced by a chronic
pathological stimulus and with typical pseudolobules, whereas, the
former is not as usually in an acute condition.
In conclusion, the authors of the current study
successfully established a reversible model of pre-hepatic portal
hypertension in rats. Thus, the clinical context of orthotopic
liver transplantation without veno-venous bypass could be
reproduced (as shown in the R group). This model may be helpful in
investigating important mechanisms involved in the process of
orthotopic liver transplantation without veno-venous bypass, such
as the hemodynamic changes, biochemical parameter alterations, and
the non-liver organism injuries involved in the anhepatic and
post-anhepatic phases.
Acknowledgements
This study was supported by a grant from the Key
Project of the Health Department of Hebei Province (grant no.
20150286).
Glossary
Abbreviations
Abbreviations:
|
PaO2
|
arterial oxygen pressure
|
|
ALT
|
alanine aminotransferase
|
|
AST
|
aspartate aminotransferase
|
|
TBil
|
total bilirubin
|
References
|
1
|
Kim DY, Huh IY, Cho YW, Park ES, Park SE,
Nah YW and Park CR: Experience without using venoveno bypass in
adult orthotopic liver transplantation. Korean J Anesthesiol.
60:19–24. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim HJ and Lee HW: Important predictor of
mortality in patients with end-stage liver disease. Clin Mol
Hepatol. 19:105–115. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen ZS, Zeng FJ, Ming CS, Lin ZB, Zhang
WJ, Wei L, Jiang JP, Zhu XH, Gong NQ, Liu B, et al: Classic
orthotopic liver transplantation without venovenous bypass: A
report of 45 cases. Transplant Proc. 35:364–365. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wall WJ, Grant DR, Duff JH, Kutt JL, Ghent
CN and Bloch MS: Liver transplantation without venous bypass.
Transplantation. 43:56–61. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang Y, Liu Y, Han R, Zhu Z, Zhang Y, Wang
X, Wang L and Shen Z: Hemostatic variation during perioperative
period of orthotopic liver transplantation without venovenous
bypass. Thromb Res. 122:161–166. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Abraldes JG, Pasarín M and García-Pagán
JC: Animal models of portal hypertension. World J Gastroenterol.
12:6577–6584. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhai Y, Petrowsky H, Hong JC, Busuttil RW
and Kupiec-Weglinski JW: Ischaemia-reperfusion injury in liver
transplantation - from bench to bedside. Nat Rev Gastroenterol
Hepatol. 10:79–89. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Deng G, Huang XJ, Luo HW, Huang FZ, Liu XY
and Wang YH: Amelioration of carbon tetrachloride-induced cirrhosis
and portal hypertension in rat using adenoviral gene transfer of
Akt. World J Gastroenterol. 19:7778–7787. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao W, Li HY, Wang LX, Hao LJ, Gao JL,
Zheng RJ, Cai CJ and Si YL: Protective effect of omeprazole on
gastric mucosal of cirrhotic portal hypertension rats. Asian Pac J
Trop Med. 7:402–406. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang XB, Liu P, Tang ZP, Li FH, Liu CH, Hu
YY and Xu LM: Cordyceps mycelia extract decreases portal
hypertension in rats with dimethylnitrosamine-induced liver
cirrhosis: A study on its histological basis. Zhong Xi Yi Jie He
Xue Bao. 6:1136–1144. 2008.(In Chinese). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Domenicali M, Caraceni P, Giannone F,
Baldassarre M, Lucchetti G, Quarta C, Patti C, Catani L, Nanni C,
Lemoli RM and Bernardi M: A novel model of CCl4-induced
cirrhosis with ascites in the mouse. J Hepatol. 51:991–999. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Méndez M, Méndez-López M, López L, Aller
MA, Arias J and Arias JL: Working memory impairment and reduced
hippocampal and prefrontal cortex c-Fos expression in a rat model
of cirrhosis. Physiol Behav. 95:302–307. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Van de Casteele M, Sägesser H, Zimmermann
H and Reichen J: Characterisation of portal hypertension models by
microspheres in anaesthetised rats: A comparison of liver flow.
Pharmacol Ther. 90:35–43. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Davies NA, Hodges SJ, Pitsillides AA,
Mookerjee RP, Jalan R and Mehdizadeh S: Hepatic guanylate cyclase
activity is decreased in a model of cirrhosis: A quantitative
cytochemistry study. FEBS Lett. 580:2123–2128. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wen Z, Zhang JZ, Xia HM, Yang CX and Chen
YJ: Stability of a rat model of prehepatic portal hypertension
caused by partial ligation of the portal vein. World J
Gastroenterol. 15:4049–4054. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Francque S, Wamutu S, Chatterjee S, Van
Marck E, Herman A, Ramon A, Jung A, Vermeulen W, De Winter B,
Pelckmans P and Michielsen P: Non-alcoholic steatohepatitis induces
non-fibrosis-related portal hypertension associated with splanchnic
vasodilation and signs of a hyperdynamic circulation in vitro and
in vivo in a rat model. Liver Int. 30:365–375. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li XN, Benjamin I and Alexander B: A new
rat model of portal hypertension induced by intraportal injection
of microspheres. World J Gastroenterol. 4:66–69. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ito T, Kiuchi T, Yamamoto H, Oike F, Ogura
Y, Fujimoto Y, Hirohashi K and Tanaka AK: Changes in portal venous
pressure in the early phase after living donor liver
transplantation: pathogenesis and clinical implications.
Transplantation. 75:1313–1317. 2003. View Article : Google Scholar : PubMed/NCBI
|