Introduction
Endometrial polyps (EPs) are common during the
reproductive years, occurring in up to 24% of women, and their
incidence increases with age (1).
EPs are formed due to proliferation and hypertrophy of the basal
layer of the endometrium, and the risk of malignancy is variable
(2). A number of studies have
investigated the association of infertility and EPs (3,4);
however, the interference of EPs in the fertility potential remains
unknown. Certain studies have suggested that women with polyps have
a higher rate of miscarriage, although there is no evidence of
lower pregnancy rates in these women (5). It has been suggested that hysteroscopic
polypectomy should be performed in infertile women (6); however, the importance of routine
hysteroscopic removal of polyps remains unknown.
Techniques for the diagnosis of EP have improved in
recent years; however, the real incidence of EP should be higher
than it is known since numerous polyps are asymptomatic. EPs are
often detected during the investigation of menstrual cycle
disorders, or upon evaluation of an infertility case using
transvaginal sonography (TVS) or hysterosalpingography (HSG)
(7,8). Hysteroscopy is a highly reliable and
sensitive tool for the detection of intrauterine disorders
(9). Upon hysteroscopy examination,
EPs appear soft and smooth, and often present only a small degree
of vascularization. However, due to the invasiveness and cost of
hysteroscopy, it may be the initial technique offered to patients.
While previous ultrasonographic studies have primarily investigated
EPs in patients with abnormal uterine bleeding (10,11), the
association between intrauterine lesions and infertility remains
unclear. The utility of TVS compared with other methods in
diagnosing intrauterine disorders has drawn increased attention of
researchers, however, its usefulness in detecting EPs in infertile
women remains rarely discussed (12). Therefore, the aims of the present
study were to evaluate the significance of TVS in detecting EP and
to assess the pregnancy outcome following hysteroscopic polypectomy
in infertile women.
Materials and methods
Patients
Between March 2011 and December 2011, a total of 145
women diagnosed with primary or secondary infertility and
intrauterine disorders by TVS and HSG at the West China Second
Hospital (Sichuan University, Chengdu, China) were selected and
included for study. All subjects met the following inclusion
criteria: Age of ≤40 years; and at least 12 months of infertility,
without any other complications. All subjects were followed up by
phone or correspondence for their reproductive histories. In total,
120 subjects were followed up by phone or correspondence for their
reproductive histories, while 25 subjects were not able to be
followed up due to incorrect or outdated contact information. The
patients were followed up once a year for three years to
investigate their pregnancy outcome. No significant difference was
detected in the age or type of infertility between patients
followed up and those not. The present study was conducted in
accordance with the Declaration of Helsinki, and with approval from
the Ethics Committee of Sichuan University. Written informed
consent was obtained from all the participants.
Diagnostic technique and surgery
Prior to hysteroscopy, TVS and HSG were performed
for the initial assessment of intrauterine abnormalities.
Irregularities in the size and shape of uterus, the thickness of
the endometrial stripe, endometrial cavity contours and echo
patterns of endometrium in the transverse plane and the long axis
were considered during TVS (13).
Filling defects in the uterine cavity and irregularities in the
uterine wall were considered during HSG (14). Subsequently, all 145 subjects were
examined by laparoscopy (A22001A 4 mm Telescope; Olympus Winter
& IBE GmbH, Hamburg, Germany) in combination with hysteroscopy
as part of their routine infertility evaluation. Depending on their
laparoscopic and hysteroscopic results, patients underwent
procedures to remove possible infertility factors in the first half
of their menstrual cycle. All EPs identified by hysteroscopy were
removed by hysteroscopic polypectomy and sent for independent
histopathological examination for confirmation by the Department of
Pathology. Transvaginal sonography examinations were performed with
Aloka SSD-1000 ultrasound system (Hitachi Aloka Medical, Ltd.,
Tokyo, Japan) and real-time scanners with 5.0 MHz endovaginal
transducers (Hitachi Aloka Medical, Ltd.). For HSG, 5–10 ml
water-soluble contrast medium [Pielograf 70% (amidotrizoato
meglumine); Juste S.A.Q.F., Madrid, Spain] was introduced into the
uterine cavity after placing a balloon catheter set. The soft
rubber Foley catheter was inflated in the cervical canal under
fluoroscopic control using a digital system (MultiDiagnost 3;
Philips Medical Systems Nederland B.V., Best, The Netherlands).
Hysteroscopy was performed with an 8-mm hysteroscope (Uteromat
Fluid Control/A4060; Olympus Winter & IBE GmbH) with an 8.5-mm
outer diameter that provides an oblique view of a 12 degree
gradient with the optical axis. Distention of the uterine cavity
during hysteroscopy was accomplished by normal saline insufflation
(13). Classification of the extent
of tubal disease (CETD) and least function (LF) score were employed
during or at conclusion of surgery to assess each patient's tubal
function.
Based on the hysteroscopy findings, the participants
were divided into three groups, including the EP, intrauterine
adhesion and normal groups. The cavity was systematically inspected
for any abnormal findings. EP was localized in relation with the
tubal ostia and the uterine walls or fundus. According to the size
and number of EPs, patients in the EP group were further divided
into two subgroups, including patients with an EP <1 cm, or
patients with an EP ≥1 cm or with multiple EPs. The pregnancy rates
were compared between these two EP subgroups.
Statistical analysis
Analysis of variance was employed to compare the
age, infertility duration, LF score (15) and CETD (16). Survival analysis (Kaplan-Meier) was
performed to ascertain the probability of conceiving in the three
groups. Curves were compared by means of Mantel-Haenszel log-rank
test for categorical variables. The effect of various covariates on
fertility was estimated using Cox's proportional hazards model.
χ2 test was employed to investigate the fertility rates
of the three groups. Analyses were performed using the SPSS version
13.0 statistical package (SPSS, Inc., Chicago, IL, USA), with
statistically significant differences indicated by P<0.05.
Results
Diagnosis and follow-up
The ultrasound scans of EPs were mainly
characterized by strong- or equal-echo mass in the uterine cavity,
interruption in the continuity of the midline echo, or uneven echo
displayed in the endometrium. The present study considered
hysteroscopic results to be the gold standard for the diagnosis of
EPs and intrauterine adhesions. In total, 34 subjects were found to
present EP using TVS. The majority of patients were examined during
the mid- and late follicular phase, and a few during the early
follicular phase. The sensitivity, specificity, positive predictive
value and negative predictive value of TVS in the detection of EPs
were 67, 96, 88.23 and 86.49%, respectively. Compared with
hysteroscopy as the gold standard, the sensitivity of TVS in
detecting EP was relatively low; however, the two methods are
similar in specificity, positive and negative prediction value.
Though TVS may not replace hysteroscopy, it may be helpful to use
TVS for initial screening of EP. When TVS does not indicate
abnormalities, hysteroscopy may not be required.
In total, 120 of the 145 subjects were followed up,
which included 40 patients diagnosed with EPs, 42 with intrauterine
adhesions and 38 with normal cavities. The ages of patients in EP,
normal and adhesions groups were 30±3.5, 30.5±3.9 and 31.3±3.3
years, respectively. The LF scores of the three groups were
5.6±2.4, 4.9±2.7 and 4.9±2.0, respectively. The CETD classes of the
three groups were 1.9±1.4, 2.0±0.9 and 1.9±0.9, respectively. The
infertility duration of the three groups were 4.4±3.5, 4.7±3.1 and
4.4±2.7 years, respectively. No significant differences in age,
type and duration of infertility, LF and CETD were identified
between the three groups, as shown in Table I.
 | Table I.Factors associated with fertility. |
Table I.
Factors associated with fertility.
| Factor | EP (n=40) | Normal (n=38) | Adhesion (n=42) | P-value |
|---|
| Age (years) |
30±3.5 | 30.5±3.9 | 31.3±3.3 | 0.1 |
| LF score | 5.6±2.4 |
4.9±2.7 |
4.9±2.0 | 0.06 |
| CETD | 1.9±1.4 |
2.0±0.9 |
1.9±0.9 | 0.23 |
| ID (years) | 4.4±3.5 |
4.7±3.1 |
4.4±2.7 | 0.14 |
The fertility rates of normal, EP and adhesion
groups were 47.4, 42.5 and 33.3%, respectively. No significant
difference in fertility rate was observed between the three groups,
as shown in Table I
Survival analysis
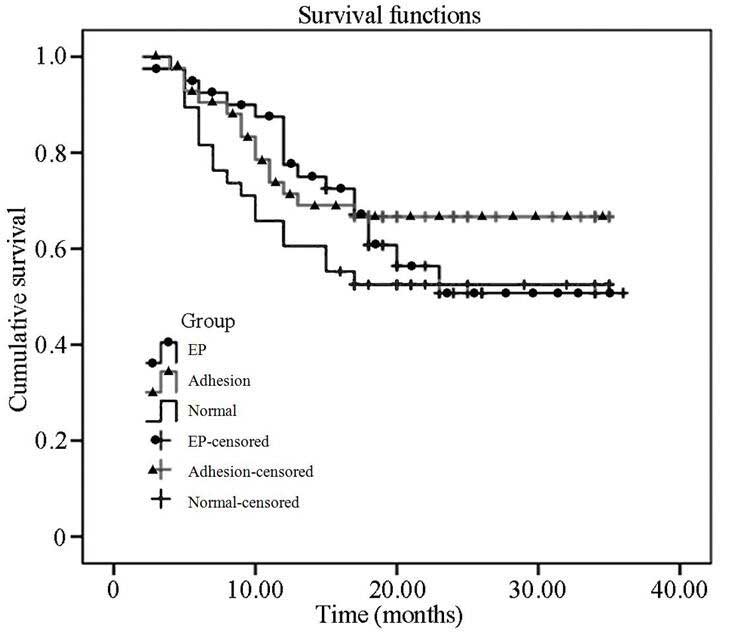
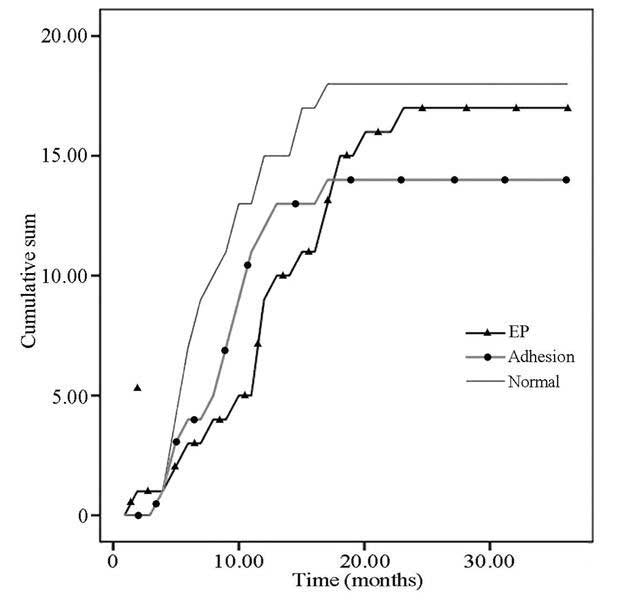
Survival analysis showed that no statistically
significant difference in fertility rate following surgery was
observed between the EP, intrauterine adhesion and normal groups
(P>0.05; Fig. 1) (Table II). Furthermore, no statistically
significant difference was observed in accumulated pregnancy rates
between the three groups (P>0.05; Fig. 2).
 | Table II.Fertility rate in the three
groups. |
Table II.
Fertility rate in the three
groups.
| Group | Fertility rate
(%) |
χ2-test | P-value |
|---|
| Normal (n=38) | 47.4 |
|
|
| EP (n=40) | 42.5 | 0.658a, 0.372b | 0.08a,0.12b |
| Adhesion (n=42) | 33.3 | 1.772a | 0.01a |
Factors affecting fertility
The effects of various covariates on fertility were
estimated using Cox's proportional hazards model analysis. The
results indicated that the age, infertility duration and CETD class
did not appear to have any statistically significant influence on
the pregnancy rate. However, the LF score was found to be
negatively correlated with pregnancy rate (i.e., the higher LF
score, the lower pregnancy rate).
Pregnancy rate and spontaneous abortion rate in the
EP group following hysteroscopic polypectomy were identified to be
45 and 5.6%, respectively. However, there was no statistically
significant difference in the fertility rate between patients with
polyps <1 cm in size and patients with polyps ≥1 cm in or
multiple polyps (χ2=0.02; P=0.96) (Table III).
 | Table III.Fertility rates of patients with
EPs. |
Table III.
Fertility rates of patients with
EPs.
| Group | Fertility rate
(%) |
χ2-test | P-value |
|---|
| <1 cm (n=23) | 46.7 |
|
|
| ≥1 cm (n=17) | 43.5 | 0.02 | 0.96 |
Discussion
EPs are frequently unrecognized, particularly in
cases where they are not sufficiently large or are asymptomatic.
TVS is a non-invasive modality that provides excellent imaging of
the uterus and endometrial abnormalities (17,18).
This method is relatively painless and cheap, and is well accepted
by patients. The appropriate time to perform a TVS examination of
the endometrium is during the follicular phase. As the normal
endometrium is thin, EP can be certainly recognized. In the present
study, the sensitivity, specificity, positive predictive value and
negative predictive value of TVS in the detection of EPs were 67,
96, 88.23 and 86.49%, respectively. This result is similar to the
findings of another study, in which the results of these parameters
were 71.4, 100, 100 and 97.1%, respectively (19). A study by Yantapant (20) examined 60 EP patients with a mean age
of 31–40 years. In that study, sensitivity, specificity and
accuracy of the diagnosis of EPs by TVS were 60, 33.3 and 57.6%,
respectively (20). Vitner et
al (21) identified that,
although hysteroscopy presented improved predictive values for
diagnosing uterine polyps when compared with TVS, the difference
was not statistically significant, and TVS had a significantly
higher sensitivity in diagnosing retained products of conception.
Though all these studies pointed to similar advantages of TVS, it
should be noted that TVS may provide insufficient information in
certain cases. For instance, small endometrial structures
protruding into the cavity may be missed (22). The results also seem to be associated
with the experience and skill of the physicians. Nevertheless,
patients with normal findings on TVS do not require further
examination by hysteroscopy, which will help reduce the high cost
of hysteroscopy and morbidity. The morbidity rate of EP in
infertile women is associated with the examination method employed
and the cases studied. Ahmadi et al (23) previously reported a sensitivity of
91.4% and a specificity of 80.2% for three-dimensional
hysterosonography in diagnosing polyps, respectively.
The high morbidity rate of EP in infertile women
indicates that EP may interfere in the gestation. De Placido et
al (24) considered 950 female
candidates for an in vitro fertilization (IVF) program. Of
these females, 602 cases were examined with a mini-hysteroscope and
348 women with a 5 mm hysteroscope, and EP was detected in 146
(24.2%) and 82 cases (23.6%), respectively (20). Similarly, a study by Silló-Seidl
(25) reported the presence of
polyps in 10.8% of patients in a series of 1,000 sterile patients,
and pregnancy was achieved in 8 of these patients following
polypectomy. By contrast, Hereter et al (26) investigated 33 patients with EP and
280 patients without EP, and identified no significant differences
between the two groups with respect to implantation and abortion in
IVF cycles. In addition, a study by Varasteh et al (27) in 23 sterile women reported a
correlation between the polypectomy and the accumulated pregnancy
rate of 65.2%, while polypectomy in infertile women was likely to
increase the pregnancy rate by a factor of 3–4 times. However,
polyps and myomas were mixed in the study, and thus the conclusions
drawn by the authors were questionable (27). In another series, 19 out of 25
infertile patients (76%) undergoing polypectomy were able to
conceive within a 12-month period (28). Furthermore, Stamatellos et al
(29) reported that the total
pregnancy rate subsequent to hysteroscopic polypectomy was 61.4%, a
percentage that is comparable with the aforementioned studies.
Another study investigated intrauterine insemination (IUI) in
infertile women whose only known problem was EP, and the proportion
of patients achieving pregnancy in the EP group was 64%, which was
nearly twice that of the control group (30). In addition, the authors reported that
pregnancies following polypectomy were frequently obtained
spontaneously, while waiting for IUI. In the present study, the
total pregnancy rate was 42.5%, and the risk of spontaneous
abortion was 5.6%, which is less than the values previously
reported (31), but is similar the
value reported for the normal group. All the studies suggest that
hysteroscopic polypectomy is an effective measure.
Certain studies identified a significant association
of pregnancy rate with the size of myomas, as the probability of
pregnancy increased proportionally with the size of the resected
myoma (27,31). However, it has been suggested that
asymptomatic polyps (<2 cm in diameter) do not appear to
interfere with IVF and embryo transfer conception rates, but may
increase the risk of spontaneous abortion (5). Persistent functional EPs are likely to
impair fertility, even when these are small. Therefore, removal of
such lesions may improve subsequent reproductive performance
(32). Another study suggested that
the hysteroscopic removal of small polyps improved the reproductive
outcome, and it is recommended for infertile women to undergo
assisted reproductive technology procedures (30,33).
These findings are similar with the results of the current study,
since no association was observed between the polyp size and the
chance of pregnancy. In addition, it is suggested that EPs
contribute to infertility and therefore should be removed
irrespective of their size or number. EP's interference with
fertility does not appear to be associated with a space-occupying
lesion mechanism. However, further studies are required to address
this question.
In conclusion, TVS features high sensitivity,
specificity and certain unique sonographic characteristics in
diagnosing EPs. Due to the invasiveness and cost of hysteroscopy,
TVS may be of interest for use as a preliminary diagnostic
procedure to screen patients for hysteroscopy. Hysteroscopic
polypectomy is an effective procedure for removing EPs. The
mechanism by which EPs interfere with fertility potential remains
unclear, hysteroscopic removal of EPs of any size appears to help
improve the pregnancy outcome of infertile women
Acknowledgements
The authors would like to thank all the women who
participated in the present study, as well as all the staff
involved at the West China Second University Hospital.
References
|
1
|
Valle RF: Therapeutic hysteroscopy in
infertility. Int J Fertil. 29:143–148. 1984.PubMed/NCBI
|
|
2
|
Bakour SH, Khan KS and Gupta JK: The risk
of premalignant and malignant pathology in endometrial polyps. Acta
Obstet Gynecol Scand. 81:182–183. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tanos V: Endometrial polyps and
infertility. Reproductive Surgery in Assisted Conception. Metwally
M and Li TC: Springer London. (London). 219–221. 2015.
|
|
4
|
Bocca SM: Endometrial polyps. Ultrasound
Imaging in Reproductive Medicine. Stadmauer LA and Tur-Kaspa I:
Springer London. (London). 133–149. 2014. View Article : Google Scholar
|
|
5
|
Lass A, Williams G, Abusheikha N and
Brinsden P: The effect of endometrial polyps on outcomes of in
vitro fertilization (IVF) cycles. J Assist Reprod Genet.
16:410–415. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shen L, Wang Q, Huang W, Wang Q, Yuan Q,
Huang Y and Lei H: High prevalence of endometrial polyps in
endometriosis-associated infertility. Fertil Steril. 95:2722–2724.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Haider Z, Alkatib M, Syed A and Bourne T:
Transvaginal scan (TVS) versus TVS and saline infusion
hydrosonography for the diagnosis of endometrial polyps and
submucous fibroids. BJOG. 113:868. 2006.
|
|
8
|
Gao YY, Xin YL, Wei XQ, Hou QN and Zhang
CL: A study on the diagnostic value of three examination methods
for endometrial polyps in patients with infertility. Xian Dai Sheng
Wu Yi Xue Jin Zhan. 15:3053–3057. 2015.(In Chinese).
|
|
9
|
Farquhar C, Ekeroma A, Furness S and Arrol
B: A systematic review of transvaginal ultrasonography,
sonohysterography and hysteroscopy for the investigation of
abnormal uterine bleeding in premnopausal women. Acta Obstet
Gynecol Scand. 82:493–504. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Timmermans A, Gerritse MB, Opmeer BC,
Jansen FW, Mol BW and Veersema S: Diagnostic accuracy of
endometrial thickness to exclude polyps in women with
postmenopausal bleeding. J Clin Ultrasound. 36:286–290. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dueholm M, Jensen ML, Laursen H and Kracht
P: Can the endometrial thickness as measured by trans-vaginal
sonography be used to exclude polyps or hyperplasia in
pre-menopausal patients with abnormal uterine bleeding? Acta Obstet
Gynecol Scand. 80:645–651. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Song Y, Shen LC, Huang W, Lei HK, Wang QS
and Zhu HL: Diagnostic value of endometrial thickness determined by
transvaginal sonography in infertile women with endometrial polyps.
Chin Med J (Engl). 125:2279–2283. 2012.PubMed/NCBI
|
|
13
|
Balić D: Balić: Office hysteroscopy,
transvaginal ultrasound and endometrial histology: A comparison in
infertile patients. Acta Medica Academica. 40:34–38. 2011.
View Article : Google Scholar
|
|
14
|
Roma Dalfó A, Ubeda B, Ubeda A, Monzón M,
Rotger R, Ramos R and Placio A: Diagnostic value of
hysterosalpingography in the detection of intrauterine
abnormalities: A comparison with hysteroscopy. American Journal of
Roentgenology. 183:1405–1409. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Adamson GD and Pasta DJ: Pregnancy rates
can be predicted by validated endometriosis fertility index (EFI).
Fertil Steril. 77(Suppl 1): S482002. View Article : Google Scholar
|
|
16
|
Rock JA, Katayama KP, Martin EJ, Woodruff
JD and Jones HW Jr: Factors influencing the success of
salpingostomy techniques for distal fimbrial obstruction. Obstet
Gynecol. 52:591–596. 1978.PubMed/NCBI
|
|
17
|
de Jong P, Doel F and Falconer A:
Outpatient diagnostic hysteroscopy. Br J Obstet Gynaecol.
97:299–303. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Granberg S, Wickland M, Karlsson B,
Norström A and Friberg LG: Endometrial thickness as measured by
endovaginal ultrasonography for indetifying endometrial
abnormality. Am J Obstet Gynecol. 164:47–52. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shalev J, Meizner I, Bar-Hava I, Dicker D,
Mashiach R and Ben-Rafael Z: Predictive value of transvaginal value
of transvaginal sonography performed before routing diagnostic
hyseroscopy for evaluation of infertility. Fertil Steril.
73:412–417. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yantapant A: Comparison of the accuracy of
transvaginal sonography and hysteroscopy for the diagnosis of
endometrial polyps at Rajavithi Hospital. J Med Assoc Thai.
95(Suppl 3): S92–S97. 2012.PubMed/NCBI
|
|
21
|
Vitner D, Filmer S, Goldstein I, Khatib N
and Weiner Z: A comparison between ultrasonography and hysteroscopy
in the diagnosis of uterine pathology. Eur J Obstet Gynecol Reprod
Biol. 171:143–145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mendelson EB, Bohm-Velez M, Josef N and
Neiman HL: Endometrial abnormalities: Evaluation with transvaginal
sonography. AJR Am J Roentgenol. 150:139–142. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ahmadi F, Rashidy Z, Haghighi H, Akhoond
M, Niknejadi M, Hemat M and Shamsipour M: Uterine cavity assessment
in infertile women: Sensitivity and specificity of
three-dimensional hysterosonography versus hysteroscopy. Iran J
Reprod Med. 11:977–982. 2013.PubMed/NCBI
|
|
24
|
De Placido G, Clarizia R, Cadente C,
Castaldo G, Romano C, Mollo A, Alviggi C and Conforti S: Compliance
and diagnostic efficacy of mini-hysteroscopy versus traditional
hysteroscopy in infertility investigation. Eu J Obstet Gynecol
Reprod Biol. 135:83–87. 2007. View Article : Google Scholar
|
|
25
|
Silló-Seidl G: The analysis of the
endometrium of 1,000 sterile women. Hormones. 2:70–75.
1971.PubMed/NCBI
|
|
26
|
Hereter L, Carreras O, Pascual MA,
Martinez F and Barri PN: Repercussion of the presence of
endometrial polyps in an I.V.F. cycle. Minerva Medica.
29:1071–1074. 1998.
|
|
27
|
Varasteh NN, Neuwirth RS, Levin B and
Keltz MD: Pregnancy rates after hysteroscopic polypectomy and
myomectomy in infertile women. Obstet Gynecol. 94:168–171. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Spiewankiewicz B, Stelmachów J, Sawicki W,
Cendrowski K, Wypych P and Swiderska K: The effectiveness of
hysteroscopic polypectomy in cases of female infertility. Clin Exp
Obstet Gynecol. 30:23–25. 2003.PubMed/NCBI
|
|
29
|
Stamatellos I, Apostolides A,
Stamatopoulos P and Bontis J: Pregnancy rates after hysteroscopic
polypectomy depending on the size or number of the polyps. Arch
Gynecol Obstet. 277:395–399. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Pérez-Medina T, Bajo-Arenas J, Salazar F,
Redondo T, Sanfrutos L, Alvarez P and Engels V: Endometrial polyps
and their implication in the pregnancy rates of patients undergoing
intrauterine insemination: A prospective, randomized study. Hum
Reprod. 20:1632–1635. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fernandez H, Sefrioui O, Virelizier C,
Gervaise A, Gomel V and Frydman R: Hysteroscopic resection of
submucosal myomas in patients with infertility. Hum Reprod.
16:1489–1492. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shoekir TA, Shalan HM and El Shafei MM:
Significance of endometrial polyps detected hysteroscopically in
eumenorrhoeic infertile women. J Obstet Gynaecol Res. 30:84–89.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Preutthipan S and Herabutya Y:
Hysteroscopic polypectomy in 240 premenopausal and postmenopausal
women. Fertil Steril. 83:705–709. 2005. View Article : Google Scholar : PubMed/NCBI
|