Introduction
Treatment of frontal sinus through surgery is
complicated because of narrow frontal drainage channel and complex
anatomical structure adjacent to the anterior skull base and screen
of the artery at orbit board. Furthermore, the postoperative ostium
of the frontal sinus leads to stricture or atresia and results in
unsuccesful surgery (1). Therefore,
the establishment of an optimal frontal sinus drainage channel is
the purpose of frontal sinus endoscopic surgery.
In the present study, 19 cases underwent Draf IIb
endoscopic frontal sinus surgery treatment for frontal sinus
lesions using the agger nasi approach during the period November
2011 to June 2014. The results showed that Draf IIb minimal
invasive treatment for frontal sinus treatment using the agger nasi
approach provides a better result and safe surgical removal of
frontal sinus lesions.
Materials and methods
General information
A total of 19 cases (28 left or and right nasal
cavities) of frontal sinus lesion were diagnosed via endoscopic
sinus surgery at the Henan Provincial People's Hospital during the
period November 2011 to June 2014. Of the 19 cases, 13 male and 6
female cases of frontal sinus lesions were identified. Patients
were aged 20–64 years, with an average age of 42 years, and the
period of frontal sinus lesion was 6 months to 11 years. According
to the criteria of Haikou (2), there
were varying degrees of other sinusitis or nasal polyps associated
with chronic frontal sinusitis in 10 cases. Seven cases with 13
left or and right nasal cavities of type II phase 3 and 3 cases
with 6 left or and right nasal cavities of type III were also
identified. The visual analogue scale (VAS) score was measured
between 7 and 10 points. According to the criteria of Krouse
(3), frontal sinus inverted
papilloma of stage III was identified in 9 cases with 9 left or and
right nasal cavities. The main clinical manifestations were a
frontal headache, stuffy nose, purulent nasal discharge and pus. A
preoperative horizontal position of computed tomography (CT) scan
of nasal sinuses is shown in Fig. 1.
The coronal and sagittal sinus were reconstructed. Antibiotics, and
topical nasal spray hormone with oral steroids were administered to
the patients, 7–10 days prior to surgery of chronic sinusitis. Oral
mucus promoting discharge agent was administered and the nasal
cavity was rinsed with physiological saline prior to surgery.
Surgery
The operation was performed under general
anesthesia. A 0° nasal endoscope (7230AA, Karl Storz, Tuttlingen,
Germany) with conventional surgical resection and uncinate process
between the middle turbinate and lateral nasal wall of the fornix
was performed to remove the nasal dome surface mucosa. An incision
of ~10–12 mm height with 45° of sphenoid sinus rongeur was made to
completely remove the agger nasi posterior wall, a top wall and
frontal surface. A resection of the frontal process of the upper
maxilla to lamina papyracea plane was performed. To reach the
anterior ethmoidal artery a 15-mm incision was made from the front
to the back up to the middle turbinate before the attachment part.
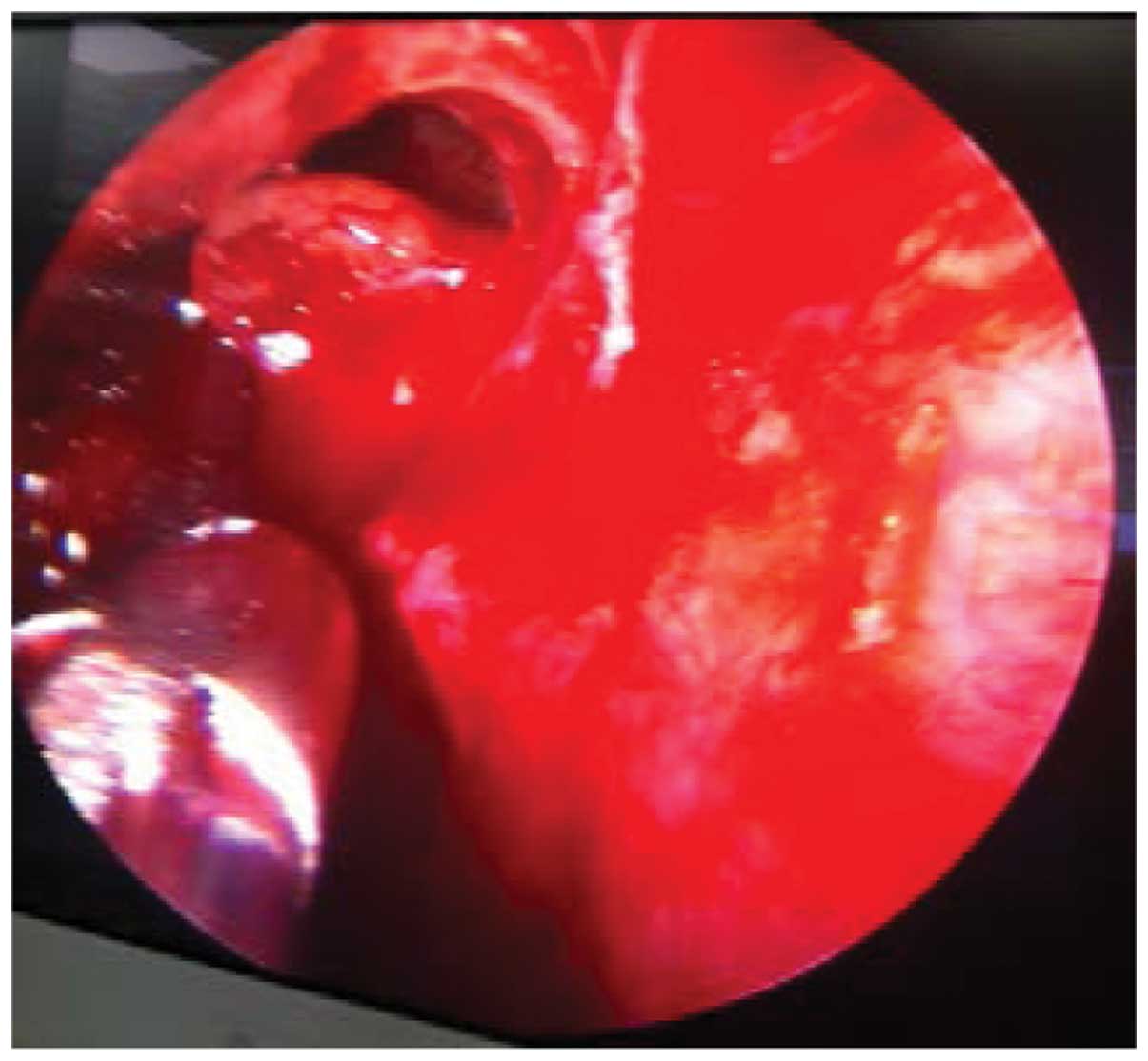
Subsequently, resection of the bottom wall of a frontal sinus of
the middle turbinate and medial attachment up to the ostium of the
frontal sinus medial to the nasal septum was performed. To expose
the top and anterior walls of the frontal sinus, a section of the
frontal ridges was ground using a frontal drill (1883672HS,
Medtronic, Minneapolis, MN, USA). Frontal sinus lesions are shown
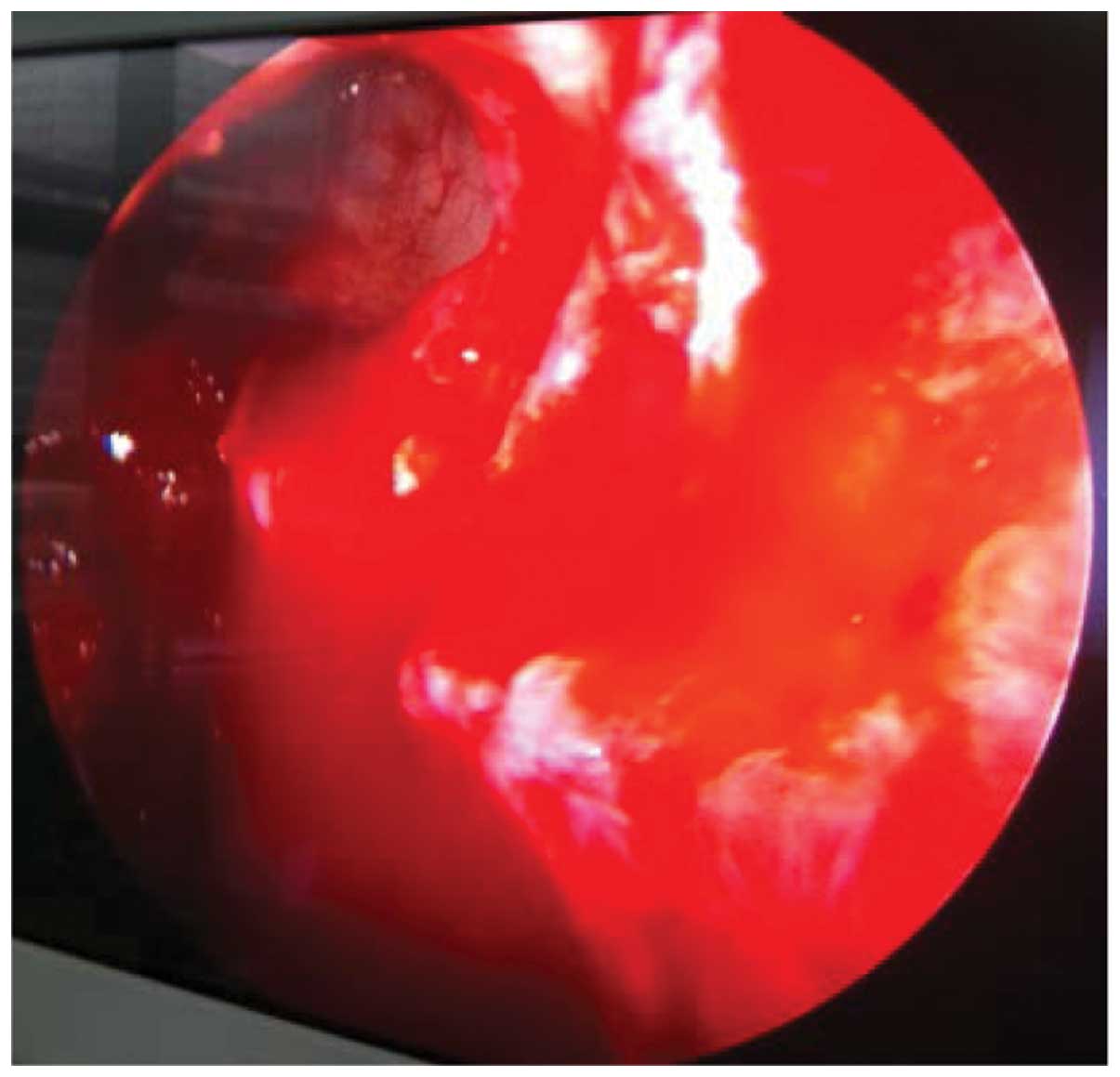
clearly in Fig. 2. Fully open ostium
of the frontal sinus is shown in Fig.
3. For the intraoperative treatment of frontal sinus inverted
papilloma, drill grinding was employed with the exception of basal
tumor bone and electric coagulation of the root. Hemostatic and
anti-adhesive material were utilized as a rapid link.
Post-processing
After the chronic sinusitis operation, tropical
nasal spray hormone and physiological saline were used to rinse the
nasal cavity. Oral mucus promoting discharge agent, antibiotics,
and oral steroid were also administered. First cleaning treatment
was performed after 1–2 weeks of operating on the cavity. Suction
was utilized to remove crusted debris and pseudomembrane. The
subsequent operation cavity processing was conducted as per the
recovery of operation cavity. Therefore, if an increased number of
more vesicles, and granulation were identified the nasal cavity,
review was conducted 2 weeks after the operation, whereas if the
nasal cavity was relatively clean, a review was conducted once at 1
month or 2 months. The treatment interval was <2 weeks. At 2
weeks, if a bubble appeared it was removed by suction drainage. Any
granulation was removed using cutting forceps (452831 or 452832,
Karl Storz, Tuttlingen, Germany). Regular nasal endoscope operative
cavity cleaning with mitomycin anti-adhesion was performed at the
ostium of the frontal sinus and middle turbinate surface until the
sinus and nasal cavity. Briefly, a cotton piece with 0.4 g/l MMC
was placed for 5 min, and then rinsed thoroughly with 200 ml
physiological saline. The operative cavity was reviewed once under
nasal endoscopy (Karl Storz). A cotton piece was placed on the
wound surface with 0.4 g/l MMC for 5 min, and rinsed thoroughly
with 200 ml physiological saline, after 1–2 months of operation.
Inverted papilloma patients were followed up for the period of 6
months to 3 years. The operative cavity was reviewed once under
nasal endoscopy, after 1–2 months of operation, and once each month
in the first 3 months. Subsequent reviews occurred once every 6
months up to 3 years.
Efficacy evaluation
The postoperative efficacy of chronic sinusitis and
nasal polyps was assessed according to the Chinese ENT and Head and
Neck Surgery Journal Editorial Committee of the Sinusitis clinical
diagnosis and treatment guidelines (CPOS2012) standard (4).
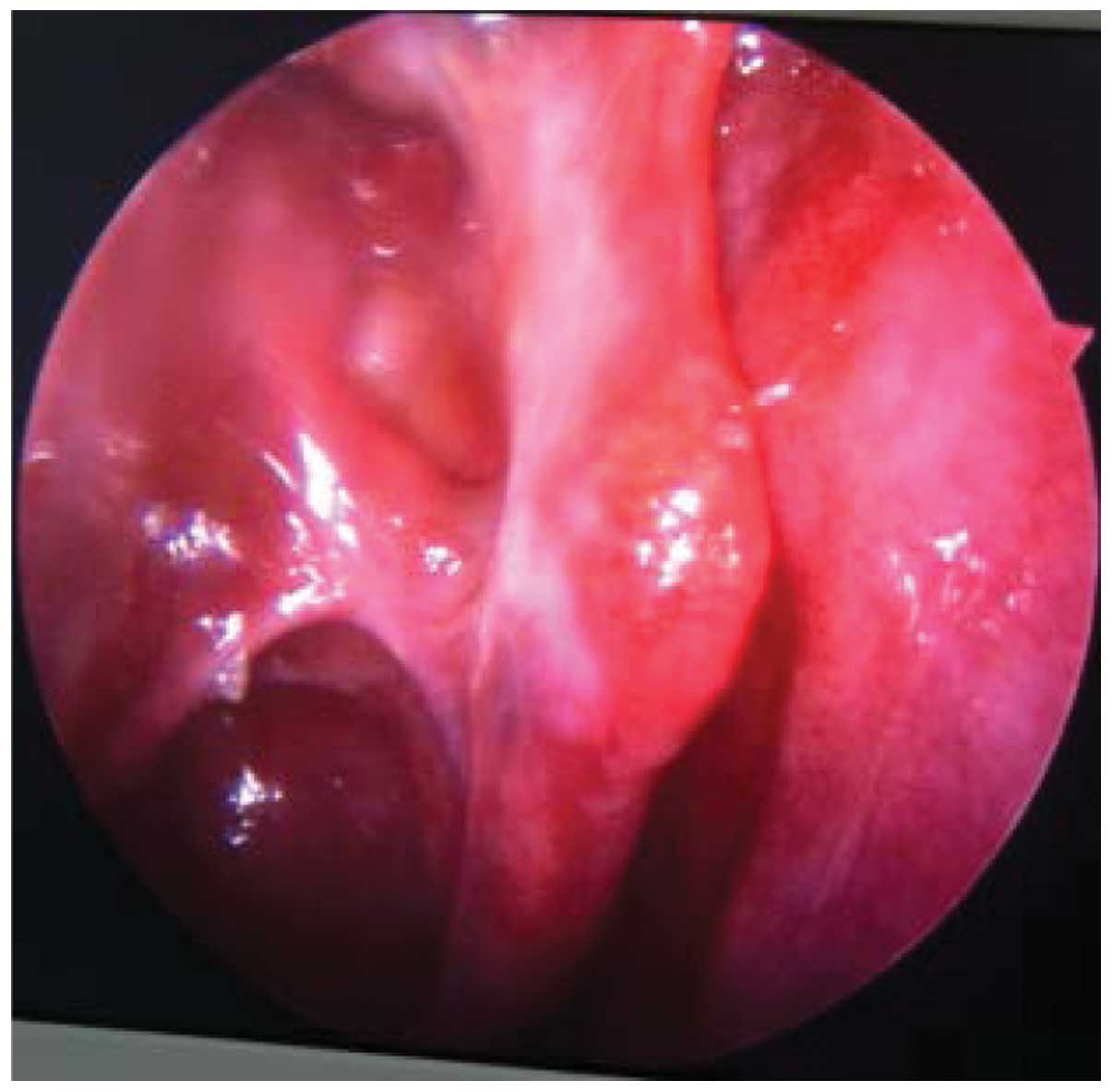
As a complete control of symptoms, the VAS total
score was between 0 and 1 points according to Lund and Kennedy
(5). After endoscopic surgery, the
sinus opening was good, and the mucosal edema disappeared. No
sticky purulent secretions were evident. The epithelium is shown in
Fig. 4. According to the control,
the symptoms improved significantly but did not completely subside.
The VAS total score was <3 points or >3 points, and the
Lund-Kennedy total score was >1 point.
Formation of the regional edema through endoscopic
examination was observed. Additionally, hypertrophy or granulation
tissue were evident in the region of the sinus mucosa, and there
was a small amount of adhesive or purulent secretion. If there was
no difference in the VAS score prior to and after the treatment,
and a total score of Lund-Kennedy was not significantly decreased,
patients were examined again. Through endoscopic examination, it
was identified that there was a swelling of the mucus membrane of
the sinus cavity and the formation of polyps or the proliferation
of connective tissue was observed. Additionally, more extensive
adhesion, stenosis or occlusion of the sinus orifice, and sticky
purulent secretion were identified. The curative effect of frontal
sinus inverted papilloma were observed via nasal endoscopic
examination. The granulation tissue was taken for pathology
examination. According to the results of the pathology examination,
recurrence of the frontal sinus was determined.
Results
We successfully performed surgery of the frontal
sinus. Unilateral periorbital edema for chronic sinusitis and nasal
polyp type II phase 3 in 2 cases after the operation were observed.
We performed nasal cavity cleaning and administered packing
material and hormone. The results showed that the edema subsided in
3 days, and there was no visual acuity and diplopia. There was no
cerebrospinal rhinorrhea, anterior ethmoidal artery bleeding, or
other complications.
Nasal endoscopy was performed between 6 and 36
months after the surgery. MMC was used in the patients with nasal
endoscopy after surgery, and the adhesion was not found at
follow-up of 6–36 months. We observed chronic sinusitis and nasal
polyps of type II phase 3 of 7 cases with 13 left or and right
nasal cavities, disease control with 11 left or and right nasal
cavities and diseased partial control with 2 left or and right
nasal cavities. We observed type III for 6 left or and right nasal
cavities in 3 cases, disease control for 4 left or and right nasal
cavities and partial disease control for 2 left or and right nasal
cavities. Chronic sinusitis and nasal polyps were identified in 10
cases with 19 left or and right nasal cavities, disease control
with 15 left or and right nasal cavities and disease partial
control with 4 left or and right nasal cavities. The results of the
VAS and Lund-Kennedy scores obtained are shown in Table I. Frontal sinus inverted papilloma
were observed in 9 cases with 9 left or and right nasal cavities.
Six cases with frontal sinus inverted papilloma underwent further
surgery owing to recurrence. The surgery was successful in 8 cases
and recurrence was identified for 1 case. We also found a
recurrence for pre-operation diagnosis of inverted papilloma and
the postoperative pathological study of inverted papillary
cancer.
 | Table I.VAS and Lund-Kennedy scores with
chronic sinusitis and nasal polyps. |
Table I.
VAS and Lund-Kennedy scores with
chronic sinusitis and nasal polyps.
|
| VAS score
(points) |
|
|---|
|
|
|
|
|---|
| Side no. (side) | Preoperative | After operation | Lund-Kennedy
(points) |
|---|
| 15 |
9.05±0.705 | 0 | 0 |
| 4 |
9.22±0.667 | 5.11±0.782 | 2.33±0.500 |
Discussion
There are two basic ways of endoscopic frontal sinus
operation for the frontal recess. The first is from front to back,
and the second way is from bottom-up, respectively. The hook
process and the nasal dome are important anatomic signs (6). The bottom-up method is mainly for the
upper attachment of the uncinate process to sinus location. When
the upper end of the uncinate process is attached to the skull base
or middle turbinate, the mouth of the frontal sinus in the uncinate
process of the outer side of the upper end is explored, whereas
when the uncinate process of the upper attachment to the lamina
papyracea occurs, the frontal sinus mouth in the inner side of the
uncinate process is explored first (7). We observed severe mucosal edema and
local formation of polyps in patients with a history of nasal
surgery. In those patients, anatomical landmarks are difficult to
identify. Furthermore, the operation is difficult because the angle
lens device cannot reach the lesion site. In this situation,
complete removal of the lesion is difficult, and this can easily
damage the nasal cavity and sinus mucosa.
Agger nasi is the gas in the front room of frontal
recess, at the top of the front of the ethmoid bone on the lateral
wall of the nasal cavity, located in the front of the uncinate
process, and upper section of the attachment middle turbinate and
nasal lateral wall (8). At the top
is the frontal recess and frontal sinus, the front section is the
process of the maxilla, the rear is the frontal recess and
ethmoidal infundibulum, which is in the uncinate process, and
laterally is the nasal and lachrymal bone (8). Bolger et al observed that the
occurrence rate of agger nasi was 98.5% (9). Thus, the agger nasi is the constant
volume recess air real.
Schaefer and Close (10) first reported the agger nasi approach
of frontal sinus operation and its theoretical basis is that the
posterior wall of the nasal dome is the anterior wall of the
frontal recess. On the bottom wall of the frontal sinus, the top
posterior wall of a nasal dome is opened, which then opens the
frontal recess. Wormald (11)
improved this process further. According to Wormald's process, the
basic characteristic is at 0° endoscopy between the middle
turbinate and lateral nasal wall which forms a cutaneous, mucosal
flap whereby the pedicle is in the medial. This process facilitates
removal of the agger nasi anterior, medial wall, posterior wall and
the top wall of the frontal sinus openings. In addition, the amount
of root of the middle turbinate mucosa flap repairs the anterior
frontal recess of the exposed bone surface. The utility model has
the advantages of 0° endoscopic surgery. The operation is
relatively convenient, and the operative field is also well
exposed. Furthermore, anatomical structure recognition is
relatively simple because of the frontal recess which is relatively
narrow and a nasal process of frontal bone dysplasia (12). The ostium frontal sinus stenosis in
most cases is due to postoperative mucus membrane edema or
hyperplasia of frontal recess stenosis and adhesion. In the agger
nasi diameter open frontal sinus (13), middle turbinate upper and frontal
recess or agger nasi real gas adhesion was caused by frontal sinus
ostium stenosis or atresia.
In the study of Wormald (14), 64 patients underwent surgery for
frontal sinus and 6 patients had middle turbinate front and lateral
nasal wall adhesion. In the present study, there was no operative
cavity adhesion following surgery, and previous findings (13,15) have
identified that the difference is mainly because of the application
of mitomycin C after the operation of endoscopic nasal surgery.
Mitomycin C acts as an anti-drug metabolism that can cross-link
with DNA double helix molecules and destroys the structure and
function of DNA (16). This
ultimately inhibits cell proliferation and DNA replication. This
process prevents fibroblasts from producing collagen material and
reduces scar formation and granulation tissue hyperplasia and
prevents tissue adhesion. In the present study mitomycin cotton
with 0.4 g/l was placed in the middle turbinate upper and frontal
recess or agger nasi to prevent postoperative cavity adhesion. The
mitomycin treatment was useful in wound healing. The results showed
that use of 0.4 g/l mitomycin 4 min after endoscopic nasal surgery
significantly reduced the incidence of postoperative adhesions.
Patients were followed up for 4 months after surgery and no side
effect was observed (17). In the
present study, two left or and right nasal cavities orbital edema
appeared in two days and then five days after surgery; however, the
edema gradually disappeared. This observation may be associated
with the orbital board minor injury. One case of recurrence was
found to be stage III frontal sinus inverted papilloma. In the
present study, inverted papillary adenocarcinoma was identified
after the postoperative pathology study. Through endoscopic
resection, a case of recurrence was identified three months after
surgery and then comprehensive treatment was followed up. The
present study employed the agger nasi approach Draf IIb frontal
sinus surgery. The mucosal flap was not preserved and resection of
the fornix position (height, 10–12 mm) and excision of the frontal
process of the upper maxilla were performed to allow entrance to
the path of a more widened frontal sinus. Resection of the upper
end of the middle turbinate and medial frontal sinus wall easily
exposed the medial frontal sinus wall.
Resection of part of the nasal process of the
frontal bone allows the frontal sinus and frontal recess increased
unobstructed drainage without the production of a mucosal flap.
This process is time efficient with regard to surgery and reduces
the bleeding. By contrast, the production of a mucosal flap in
nasal endoscopy causes bleeding, which leads to blood pollution
causing the operation field to become unclear. The operation time
is also prolonged. This process also reduces postoperative adhesion
and cause obstruction in dressing and inspection of the frontal
sinus. To avoid intracranial and intraorbital complications, the
anterior cranial base and the anterior artery should be
cleared.
In conclusion, the agger nasi approach Draf IIb
frontal sinus surgery for frontal sinus disease rarely uses the
angled endoscope and equipment. The operation is convenient with
clear operation visual field and less bleeding. Operation time is
also short with fewer complications. This approach of surgery is
worthy of clinical application.
References
|
1
|
Han JK, Ghanem T, Lee B and Gross CW:
Various causes for frontal sinus obstruction. Am J Otolaryngol.
30:80–82. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
China Medical Branch Department of
Otolaryngology Otorhinolaryngology Medicine Editorial Board.
Clinical classification of chronic sinusitis and nasal polyp stage
and the evaluation standard endoscopic sinus surgery: Haikou. Chin
J Otorhinolaryngol. 33:1341998.
|
|
3
|
Krouse JH: Development of a staging system
for inverted papilloma. Laryngoscope. 110:965–968. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chinese Otolaryngology Head and neck
surgery Magazine Editorial Committee of Rhinology Group, Chinese
medical Association of Otolaryngology - head and neck surgery,
nasal science group, chronic nasal. Sinusitis diagnosis and
treatment guidelines (as of 2012, Kunming). Chin Otorhinolaryngol
Head Neck Surg. 48:92–94. 2013.
|
|
5
|
Lund VJ and Kennedy DW: Staging for
rhinosinusitis. Otolaryngol Head Neck Surg. 117:S35–S40. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Luo Zhang, Bing Zhou Wen Tong Ge, et al:
Endoscopic frontal sinus surgery through agger nasi cell approach.
Chin Otolaryngol Head Neck Surg. 40:493–497. 2005.(In Chinese).
|
|
7
|
Friedman M, Bliznikas D, Vidyasagar R, et
al: Frontal sinus surgery 2004: Update of clinical anatomy and
surgical techniques. Op Tech Otolaryngol Head Neck Surg. 15:23–31.
2004. View Article : Google Scholar
|
|
8
|
Stammberger HR and Kennedy DW: Anatomic
Terminology Group. Paranasal sinuses: anatomic terminology and
nomenclature. Ann Otol Rhinol Laryngol Suppl. 167:7–16.
1995.PubMed/NCBI
|
|
9
|
Bolger WE, Butzin CA and Parsons DS:
Paranasal sinus bony anatomic variations and mucosal abnormalities:
CT analysis for endoscopic sinus surgery. Laryngoscope. 101:56–64.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schaefer SD and Close LG: Endoscopic
management of frontal sinus disease. Laryngoscope. 100:155–160.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wormald PJ: The agger nasi cell: the key
to understanding the anatomy of the frontal recess. Otolaryngol
Head Neck Surg. 129:497–507. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shi J and Lai Y: Frontal sinus, the key
stone in current endoscopic period, needs more focus surgery. Chin
J Ophthalmol Otorhinolaryngol. 12:75–77. 2012.
|
|
13
|
Loury MC: Endoscopic frontal recess and
frontal sinus ostium dissection. Laryngoscope. 103:455–458. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wormald PJ: The axillary flap approach to
the frontal recess. Laryngoscope. 112:494–499. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Metson R: Endoscopic treatment of frontal
sinusitis. Laryngoscope. 102:712–716. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gutierrez T and Hopkins C: Safe
application of mitomycin C within the nasal cavity. J Laryngol
Otol. 125:309–310. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chung JH, Cosenza MJ, Rahbar R and Metson
RB: Mitomycin C for the prevention of adhesion formation after
endoscopic sinus surgery: a randomized, controlled study.
Otolaryngol Head Neck Surg. 126:468–474. 2002. View Article : Google Scholar : PubMed/NCBI
|