Introduction
Hepatocellular carcinoma (HCC), also known as liver
cancer, is the sixth most common malignant tumor worldwide. Each
year, ~748,000 patients are diagnosed with liver cancer, and
~696,000 of these succumb to the disease; liver cancer accounts for
≤1/3 of various malignant tumors. In China, the number of patients
with liver cancer is >50% larger than the total number of
patients that develop liver cancer worldwide (1). Spontaneous rupture of HCC hemorrhage is
a severe complication of HCC; the incidence of spontaneous rupture
in Western countries is ~3%, and the mortality rate in Asian
countries is 12–14% (2). As a result
of its acute onset, the spontaneous rupture of HCC hemorrhages
often leads to hemorrhagic shock, and if timely and reasonable
treatment methods are not provided, the lives of the patients are
put at risk (3–7).
Surgical resection, transarterial chemoembolization
(TACE) and transcatheter arterial embolization (TAE) are common
methods used in the treatment of spontaneous rupture of HCC
hemorrhage (8–10). Recently, a novel method combining
surgery and radio frequency ablation was reported for the treatment
of spontaneous rupture of HCC hemorrhage (11). However, despite the presence of
numerous positive treatment methods, a large number of patients are
not successfully treated, and the mortality rate within 30 days is
as high as 31–67% (8,12–15).
Common embolic agents currently used in the clinical treatment of
acute spontaneous rupture of HCC hemorrhage by TACE or TAE are
iodized oil, gelatin sponge particles (Gelfoam), stainless steel
rings and polyvinyl alcohol (16,17); to
date, gelatin sponge microparticles (GSMs) combined with
chemotherapy for the treatment of this disease has not been
reported.
Embolization materials can be classified into three
groups by the duration of embolization effect: Short-term,
medium-term, and long-term. GSMs are medium-term embolic agents
produced in China. A previous study using animal experimentation,
performed at the Affiliated Zhongshan Hospital of Dalian University
(Dalian, China), demonstrated the safety of GSMs (18). Clinical application studies have
suggested that GSM-TACE in the treatment of HCC results in tumor
necrosis and a reduction in tumor size, and has good clinical
curative effects (19–21). The present study aimed to summarize
the clinical hemostatic effect of GSM-TACE in the treatment of HCC,
and to investigate the safety and efficacy of the clinical
application of GSMs.
Materials and methods
Clinical materials
Data from a total of 13 cases of HCC combined with
spontaneous rupture of HCC hemorrhage, who were treated between
August 2010 and June 2014, were collected at the Affiliated
Zhongshan Hospital of Dalian University (Dalian, China). The 13
patients were admitted to hospital 1 h to 2 days after suddenly
developing acute abdominal pain or liver region pain, and 8
patients exhibited signs of peritoneal irritation. Imaging
examinations, including computed tomography (CT), B ultrasound and
magnetic resonance imaging, combined with the recording of clinical
manifestations or diagnostic abdominal puncture, confirmed that the
patients had a rupture of HCC (Table
I). Baseline liver enzymes, including aspartate transaminase
(AST), alanine aminotransferase (ALT), total bilirubin (TBIL) and
albumin (ALB), were obtained prior to the GSM-TACE. The present
study was approved by the Ethical Committee of the Affiliated
Zhongshan Hospital of Dalian University (Dalian, China). Written
informed consent was obtained from the patients or the patient's
family.
 | Table I.General information of the
patients. |
Table I.
General information of the
patients.
| Parameter | n |
|---|
| Age range (mean) | 43–77
(58.07±10.41) |
| Gender |
|
| Male | 13 |
|
Female | 0 |
| Etiology |
|
| Hepatitis
B | 12 |
| Hepatitis
C | 1 |
| Child-Pugh grading,
A/B | 9/4 |
| ECOG score,
0/1/2 | 12/1/0 |
| BCLC stage,
A/B/C/D | 0/13/0/0 |
| Tumor size range, cm
(mean) | 4.2–10
(6.21±2.18) |
| <5
cm | 2 |
| ≥5
cm | 11 |
| Tumor number,
<2/>2 | 9/4 |
| Tumor light out liver
surface | 11 |
| AFP, <400/>400
ng/ml | 9/4 |
| GSM-TACE cycles,
1/2-3/>3 | 5/8/0 |
GSM-TACE technique
The Seldinger method (22) was used to puncture the right femoral
artery, a 5F-RH catheter (Terumo, Tokyo, Japan) was implanted into
the hepatic duct, and routine celiac artery and hepatic artery
angiography was subsequently performed (22). Heterotopic feeding artery
angiography, including the superior mesenteric artery, phrenic
artery, right renal artery and left gastric artery angiography, was
conducted according to tumor location, size, tumor staining
integrity and contrast extravasation, in order to confirm the tumor
feeding arteries. Digital subtraction angiography (DSA) was
performed to map the vascular liver anatomy to determine the
presence of tumor staining and to identify the arterial feeders of
the tumor. Tumor stains were specific findings of the HCC in DSA.
The operational approach employed, GSM-TACE, was similar to routine
TACE technique (22), aside from the
use of GSMs [Hangzhou Aili Kang Pharmaceutical Technology Co, Ltd.
(Hangzhou, China); size, 100 mg] with various diameters (350–560,
560–710 and 710–1,000 µm) and dosages (30–150 mg), according to
tumor size and intraoperative blood flow velocity. GSMs were mixed
with 10 mg lobaplatin injection (Hainan Chang'an International
Pharmaceutical Co., Ltd., Chang'an, China; 10 mg) to make the
particle suspension. The GSMs and chemotherapeutic drug suspension
were slowly infused via the transcatheter into the feeding artery
in the tumor region, and the infusion was continued until the
regional intra-arterial blood stagnation and tumor staining
disappeared completely. Intraoperative angiography can be used to
determine whether embolization should be performed. Following
thoroughly embolization, the catheter was placed in the celiac
artery, and once arteriography revealed the splenic artery, liver
protection therapy was performed; 15 ml polyene phosphatidylcholine
injection and 1.8 g glutathione (Fudan Fuhua Pharmaceutical Co.,
Ltd., Shanghai, China) were mixed with 150 ml glucose to a
concentration of 5%, and slowly infused.
Post-operative management
Patients were fasted for 1–2 days and remained on
bed rest. Fluid infusion with saline and glucose was performed for
3–5 days (1,500–2,500 ml/day). In addition, the patients received
the following: Intravenous injection of 2 g cefazolin sodium (Le Pu
Pharmaceutical Co., Ltd., Henan, China), twice daily; intravenous
injection of coenzyme complex 1 + 100 ml glucose with a
concentration of 5% (Shuanglu Pharmaceutical Co., Ltd., Beijing,
China), once daily; intravenous injection of 15 ml polyene
phosphatidylcholine injection + 100 ml glucose with a concentration
of 5% (Tiantai Mountain Pharmaceutical Co., Ltd., Sichuan, China),
once daily; intravenous injection of 1.8 g glutathione + 100 ml
sodium chloride with a concentration of 0.9%, once daily;
intravenous injection of 40 mg esomeprazole (AstraZeneca
Pharmaceutical Co., Ltd., Jiangsu, China) + 0.9% sodium chloride
100 ml, once daily; intravenous injection of 5 mg tropisetron
(Yikang Pharmaceutical Co., Ltd., Shandong, China) + 0.9% sodium
chloride 100 ml, once daily; intramuscular injection of 1 KU
hemocoagulase (Aohong Pharmaceutical Co., Ltd., Liaoning, China),
once daily; and intramuscular injection of 10 mg vitamin K1 (Yikang
Pharmaceutical Co., Ltd., Shandong, China), once daily.
Post-operative fever occurred in seven patients, and symptomatic
treatment [compound aminophenazone (Shuanghe Pharmaceutical Co.,
Ltd., Shanxi, China)] was administered via intramuscular injection
when the temperature of a patient was >38.5°C. Post-operatively,
all patients had right upper abdominal pain, and were treated
according to WHO analgesic three principles (23).
Evaluation of the curative effects and
observation of adverse effects
Evaluation was performed based on the Response
Evaluation Criteria In Solid Tumors (mRECIST 1.1) (24). Target lesions were scored as follows:
Complete response (CR), all target lesions developed during the
arterial enhancement period ceased to exist, and all lymph nodes
(pathological) were <10 mm; partial response (PR), total target
lesion arterial enhancement length diameter was reduced ≥30%;
progressive disease (PD), total baseline lesion diameter was
increased ≥20%, or new lesions occured; and stable disease (SD),
total baseline lesion diameter was reduced but did not reach the
level of PR, or the level was increased but not as high as in
PD.
Non-target lesions were scored as follows: CR, all
non-target lesions developed during the arterial phase ceased to
exist and the tumor marker levels were normal (normal AFP, 0–20
ng/ml); SD, ≥1 non-target lesions developed during the arterial
phase remained, or tumor marker levels were higher than normal
levels; and PD, the appearance of ≥1 new lesions and/or the
existence of non-target lesions. The tumor objective response rate
(ORR; ORR = CR + PR / total number of patients in each time
segment) of each time segment was calculated. The time segment was
the time from the initial GSM-TACE to the evaluation of the
curative effects. At 4 days after surgery, a review CT scan was
performed to evaluate the hemostasis effect and tumor necrosis
degree following GSM-TACE. Routine blood, liver and kidney function
tests, and α-fetoprotein (AFP) examination, were conducted at 4 and
7 days and every month after surgery. An enhanced CT examination
was performed every month after surgery in order to evaluate
whether there was re-bleeding or new lesions; if there was no
re-bleeding, subsequent GSM-TACE treatment was performed to control
tumor growth. The purpose of the treatment was to prolong the
survival of patients.
Statistical analysis
Statistical analyses were performed using SPSS 17.0
software (SPSS, Inc., Chicago, IL, USA). P<0.05 was considered
to indicate a statistically significant difference.
Results
Patient characteristics
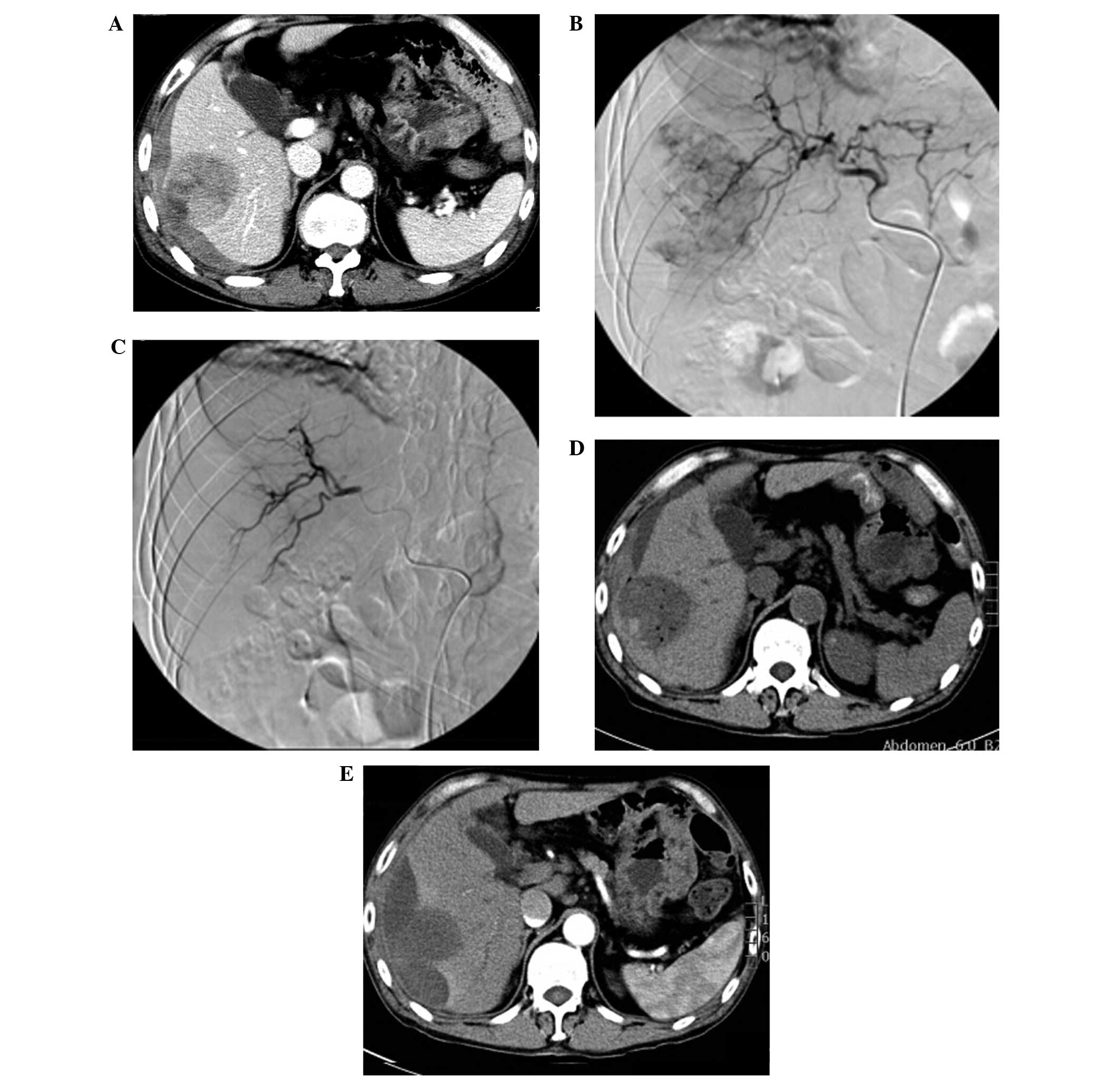
Among the 13 cases of patients with HCC, 11 cases
had tumors located in the right lobe and 2 cases had tumors located
in the left lobe. A total of 11 cases had tumors protruding from
the surface of the liver capsule, and various degrees of blood
accumulation could be observed in the inferior liver capsule and
abdominal cavity (Fig. 1A). Baseline
liver enzymes were obtained prior to the GSM-TACE as follows: AST,
48.31±15.88 IU/l; ALT, 44.77±13.25 IU/l; TBIL, 24.46±5.53 µmol/l;
and ALB, 39.69±4.36 g/l. Prior to GSM-TACE, DSA showed that all 13
cases had hypervascular tumors with strong tumor staining (Fig. 1B). Following GSM-TACE surgery, all 13
cases in the group achieved successful hemostasis, and the tumor
staining disappeared (Fig. 1C). At 4
days after GSMs-TACE, a review CT scan was conducted and the
results showed that 13 cases had no significant increase in hepatic
subcapsular hematoma and hemoperitoneum, and different degrees of
‘honeycomb’ necrosis could be seen in lesions (Fig. 1D). Among the 13 cases, review CT
showed that 2 cases had tumors located in the liver V segment and
VI segment edge with significant necrosis, and no re-bleeding.
These 2 cases received selective tumor resection at 10 days
post-operation and 1 month post-operation, respectively. During the
surgery, the tumor invaded the liver capsule which resulted in
tumor ulceration, and obvious necrosis tissues could be observed.
One case had a re-rupture of the hepatocellular carcinoma
hemorrhage at 3 months after surgery, and received a second
GSM-TACE for successful hemostasis. All the cases had a review CT
scan at 1 month after surgery, and these showed that the
intrahepatic tumor size of 7 cases (53.8%) was reduced compared
with baseline lesions (Fig. 1E).
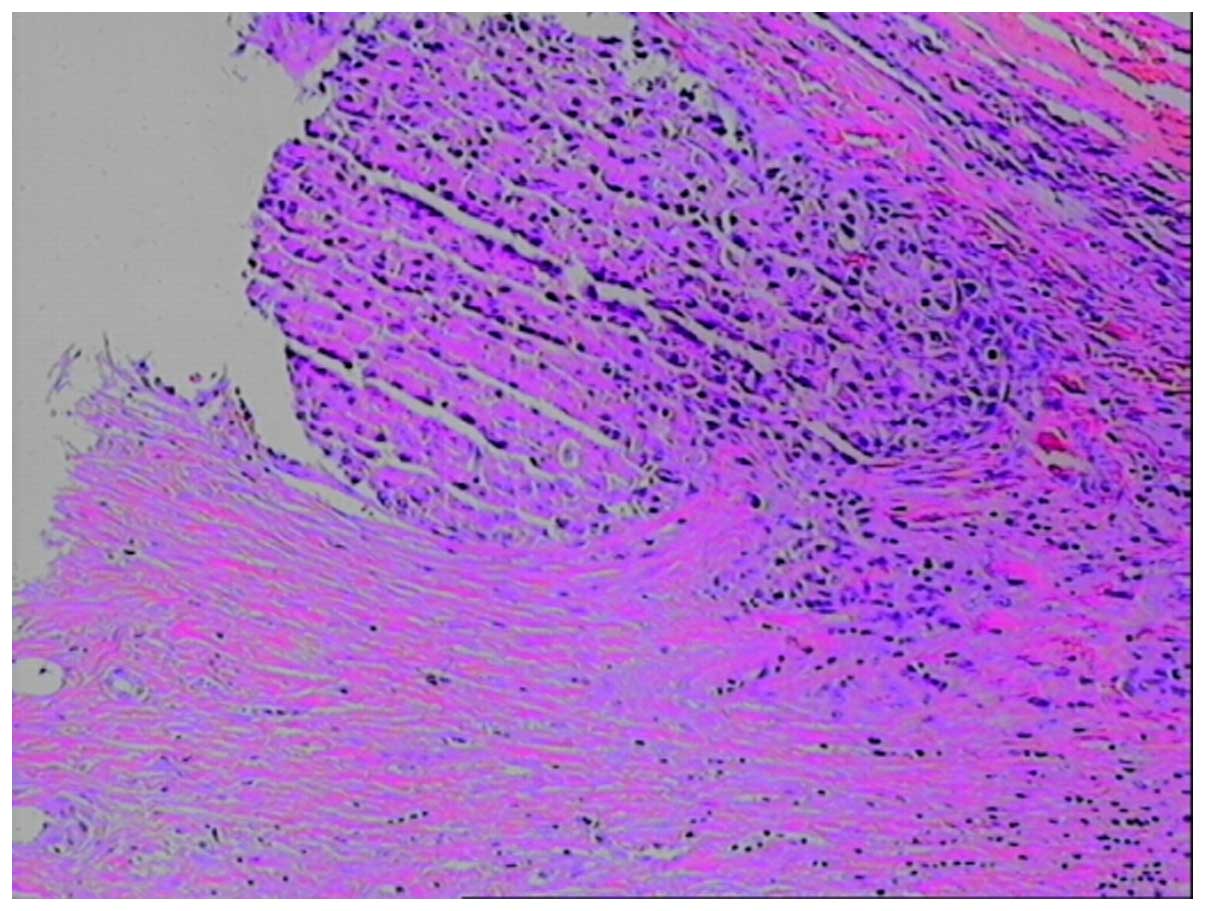
Post-operative pathological examination confirmed that the tumor
was a moderately differentiated hepatocellular carcinoma (Fig. 2).
Adverse reactions following
GSM-TACE
Patients had various degrees of right upper
abdominal pain and nausea and vomiting following surgery, and this
may be related to tumor rupture and reactions following embolism.
Following surgery, 7 patients experienced symptoms of fever, and
body temperature fluctuated of 37.1–38.9°C. Liver enzymes were
measured four days after the GSM-TACE as follows: AST, 60.85±13.53
IU/l (P=0.037); ALT, 54.23±12.72 IU/l (P=0.001); TBIL, 38.77±4.67
µmol/l (P=0.011); and ALB, 37.77±3.61 g/l (P=0.001). Although these
results were significantly increased and indicative of mild
impaired liver function, this was only transient and liver function
indices recovered to the normal levels (AST, 37.51±13.84 IU/l; ALT,
35.47±12.41 IU/l; TBIL, 21.86±3.84 µmol/l; and ALB, 43.77±11.38
g/l) after ~7 days of supportive liver protection therapy. A total
of 13 cases had I–II degree adverse reactions following surgery
(Table II).
 | Table II.Adverse reactions and complications
following gelatin sponge microparticle-transcatheter arterial
chemoembolization treatment. |
Table II.
Adverse reactions and complications
following gelatin sponge microparticle-transcatheter arterial
chemoembolization treatment.
| Complications | n (%) |
|---|
| I–II degree |
|
| Upper
abdominal pain | 13 (100.0) |
| Nausea
and vomiting | 9 (69.2) |
|
Fever | 7 (53.8) |
|
Neutropenia | 0 (0.0) |
| III degree |
|
|
Cholecystitis | 0 (0.0) |
| Liver
abscess | 0 (0.0) |
| Tumor
recurrent rupture and bleeding | 1 (7.6) |
| Hepatic
failure | 1 (7.6) |
| Renal
failure | 1 (7.6) |
| Hepatic
encephalopathy | 1 (7.6) |
| Upper
gastrointestinal bleeding | 1 (7.6) |
Therapeutic evaluation
The survival rates at 1, 3 and 6 months after
surgery were 76.9 (10/13), 61.5 (8/13) and 53.8% (7/13),
respectively. Until June 2014, the follow-up time was 3 years and
10 months, during which 4 cases did not survive (30.7%), including
1 case who succumbed to hepatic encephalopathy, 2 cases who
succumbed to renal failure and 1 case who succumbed to upper
gastrointestinal hemorrhage (Table
III).
 | Table III.Tumor response after gelatin sponge
microparticle-transcatheter arterial chemoembolization
treatment. |
Table III.
Tumor response after gelatin sponge
microparticle-transcatheter arterial chemoembolization
treatment.
| Months after
surgery | n | Complete
responsea | Partial
responsea | Stable
diseasea | Progressive
diseasea | ORRa |
|---|
| 1 | 12 | 3 (23.1) | 5 (38.5) | 2 (15.4) | 2
(15.4) | 8 (61.6) |
| 3 | 10 | 2 (15.4) | 5 (38.5) | 2 (15.4) | 1 (7.6) | 7 (53.9) |
| 6 | 9 | 2 (15.4) | 3 (23.1) | 2 (15.4) | 2
(15.4) | 5 (38.5) |
Discussion
Interventional embolization is the first choice of
emergency treatment for HCC rupture hemorrhage (25,26). A
previous meta-analysis (16)
revealed that the success rate of TAE hemostatic therapy for the
treatment of HCC rupture hemorrhage in the acute stage was 53–100%
(16); the 30-day mortality of TAE
treatment (0–37%) was lower than that of surgical resection
(28–75%), suggesting that regardless of whether patients with HCC
have bleeding or not, the survival rate will be similar following
treatment (16). Kirikoshi et
al (14) demonstrated that the
post-operative survival rate of TAE treatment was significantly
higher compared with surgical resection; mortality rates following
surgical resection within 30 days of surgery were 30–70%, and the
mortality rates following TAE treatment within 30 days of surgery
were <10%. Tumor resection following TACE or TAE for the
treatment of patients with HCC greatly increased the survival rate
of the patients (27). The long-term
outcomes of surgical resection were improved compared with TACE
treatment for HCC, and resection was able to remove the tumor
completely (28–30). All 13 patients with rupture of
hepatocellular carcinoma hemorrhage received GSM-TACE treatment
between 1 h and 2 days after bleeding; among them, 2 cases received
surgical resection following GSM-TACE treatment. After follow-up
between 4 and 6 months, the results demonstrated that no recurrence
or metastatic lesions were observed among the patients who received
surgical resection. It is believed that TACE is preferable in the
treatment of spontaneous rupture of hepatocellular carcinoma
hemorrhage, and elective surgical resection may help to improve the
long-term curative effect.
Tumor rupture hemorrhage is one of the severe
complications of primary hepatocellular carcinoma, and the
underlying mechanisms remain unclear. A number of investigators
believe that tumor invasion in hepatic veins may cause congestion,
and increased tumor growth speed could cause central necrosis
combined with coagulation disorders, and the tumor tissue edge is
vulnerable, so trauma or a sudden increase in intra-abdominal
pressure and the friction between the diaphragmatic muscle and the
tumor, caused by respiratory motion could result in rupture and
bleeding (26,31). In the present study, 11 cases had a
tumor protruding from the liver surface, and 9 cases had a tumor
protruding from the liver surface >1 cm. The results of the
current study demonstrate that tumor size >5 cm and tumors
protruding from the liver surface are one of the primary risk
factors of HCC rupture and bleeding. In the present study, 1 case
had a rupture of HCC hemorrhage, and no follow-up was conducted
following emergency GSM-TACE embolization; after 3 months,
re-bleeding occurred and hemostasis was achieved after treatment
with the same embolization therapy. To date, the patient is in a
stable condition according to mRECIST; stable disease and the
diameter of the tumor were reduced but a partial response was not
achieved. Bleeding following GSM-TACE treatment may be associated
with the following factors: i) The tumor protruding into the liver
surface; ii) excessive embolism therapy dosages; iii) a large tumor
with internal liquefaction necrosis and increasing pressure; and
iv) tumor progression. In the present study, the patients underwent
hemostasis following GSM-TACE treatment, and the tumor growth was
effectively inhibited during follow-up the period.
In the current study, the clinical characteristic of
TACE in the treatment of HCC rupture and bleeding were assessed
following the application of particulate embolic agent-GSM in
regional tumor arterial embolization. Worldwide, embolic agents for
the treatment of HCC rupture and bleeding typically include iodized
oil, gelatin sponge particles, polyvinyl alcohol and stainless
steel ring (17,29), and each agent has its advantages and
disadvantages. The agents using iodized oil as the primary embolic
agent after years of clinical precipitation are used widely, but
during the treatment of HCC by TACE, the necrotic rate of tumors is
only 0–4.8% (32,33), and it may lead to severe
complications, such as pulmonary embolism (34). However, the application of iodized
oil embolization agent is considered to be one of the factors that
cause tumor rupture (35,36).
The application of permanent embolic agents and
steel rings is not conducive to the future treatment of HCC. The
GSMs used in the present study were particle-type mid-embolic
agents made in China, and preliminary animal experiments and
clinical studies have confirmed their safety and efficacy, which is
suitable for the treatment of large HCCs and combined arteriovenous
fistula and portal vein thrombosis; in the present study, tumor
necrosis could be observed at 3 h after surgery with few
complications (18,19). In addition, in the current study, no
re-bleeding occurred in 13 cases (100%) 1 month after GSM-TACE.
Grade I–II adverse reactions, such as fever, right upper abdominal
pain, nausea and vomiting, are common complications following
GSM-TACE (37); in the present
study, the liver and kidney functions were recovered to the
pre-operative levels 7–10 days after surgery, tumor growth was
effectively controlled, and the ORR at 1, 3 and 6 months after
surgery was 61.6, 53.9 and 38.5%, respectively, leading to the
conclusion that the survival rate of the patients was prolonged.
The occurrence of the above-mentioned complications may be
associated with tumor necrosis. In the current study, 4 cases
succumbed to complications, such as tumor progression complicated
with multiple organ failure, gastrointestinal bleeding and hepatic
encephalopathy; however, patient mortality showed no direct
correlation with GSM-TACE. The results of the present study were
concordant with those of previous studies with regards to the
safety and clinical efficacy of GSMs for the treatment of HCC
(19–21).
Pre-operative shock, low hemoglobin and albumin
expression levels, prolonged prothrombin time, increased serum
creatinine expression levels, hepatic encephalopathy, severe
ascites, portal vein tumor thrombus and multinodular tumors in the
left and right lobe are the primary factors that affect the
treatment of HCC rupture hemorrhage. Liver function is one of the
prognostic factors for survival time in TAE and TACE (25). According to the Barcelona clinic
liver cancer (BCLC) standard, all of the patients in the present
study were suitable for GSM-TACE treatment. During surgery, the
dosage was personalized for each individual according to patients'
conditions, as suitable quantity of embolism is a key factor in
achieving good clinical efficacy. In addition, the protection of
liver function during and following TACE is important.
In conclusion, in patients with acute HCC rupture,
bleeding with stable vital signs, BCLC B stage and Child A-B grade
can be treated with TACE as a first line of treatment. After
reaching a stable condition, treatment with surgery can be
conducted appropriately according to lesion location, size, number,
metastasis status and tumor progression, which is conducive to
improve the long-term curative effect. GSM-TAC for the treatment of
HCC rupture and bleeding has the advantages of a good hemostatic
effect, and good safety and short-term effects; however, due to the
small sample size used in the current study, the long-term effects
need to be verified by investigating a larger sample size.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Battula N, Madanur M, Priest O, Srinivasan
P, O'Grady J, Heneghan MA, Bowles M, Muiesan P, Heaton N and Rela
M: Spontaneous rupture of hepatocellular carcinoma: A Western
experience. Am J Surg. 197:164–167. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Okazaki M, Higashihara H, Koganemaru F,
Nakamura T, Kitsuki H, Hoashi T and Makuuchi M: Intraperitoneal
hemorrhage from hepatocellular carcinoma: Emergency
chemoembolization or embolization. Radiology. 180:647–651. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sato Y, Fujiwara K, Furui S, Ogata I, Oka
Y, Hayashi S, Ohta Y, Iio M and Oka H: Benefit of transcatheter
arterial embolization for ruptured hepatocellular carcinoma
complicating liver cirrhosis. Gastroenterology. 89:157–159. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Corr P, Chan M, Lau WY and Metreweli C:
The role of hepatic arterial embolization in the management of
ruptured hepatocellular carcinoma. Clin Radiol. 48:163–165. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Xu HS and Yan JB: Conservative management
of spontaneous ruptured hepatocellular carcinoma. Am Surg.
60:629–633. 1994.PubMed/NCBI
|
|
7
|
Hsieh JS, Huang CJ, Huang YS, Sheen PC and
Huang TJ: Intraperitoneal hemorrhage due to spontaneous rupture of
hepatocellular carcinoma: Treatment by hepatic artery embolization.
AJR Am J Roentgenol. 149:715–717. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li WH, Cheuk EC, Kowk PC and Cheung MT:
Survival after transarterial embolization for spontaneous ruptured
hepatocellular carcinoma. J Hepatobihary Pancreat Surg. 16:508–512.
2009. View Article : Google Scholar
|
|
9
|
Yang T, Sun YF, Zhang J, Lau WY, Lai EC,
Lu JH, Shen F and Wu MC: Partial hepatectomy for ruptured
hepatocellular carcinoma. Br J Surg. 100:1071–1079. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yeh CN, Lee WC, Jeng LB, Chen MF and Yu
MC: Spontaneous tumour rupture and prognosis in patients with
hepatocellular carcinoma. Br J Surg. 89:1125–1129. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cheung TT, Poon RT, Chok KS, Chan AC,
Tsang SH, Dai WC, Yau TC, Chan SC, Fan ST and Lo CM: Management of
spontaneously ruptured hepatocellular carcinomas in the
radiofrequency ablation era. PLoS One. 9:e944532014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Toshikuni N, Takuma Y, Morimoto Y,
Shimomura H and Yamamoto H: Transarterial embolization for ruptured
hepatocellular carcinoma: Survival predictors.
Hepatogastroenterology. 58:565–569. 2011.PubMed/NCBI
|
|
13
|
Tan FL, Tan YM, Chung AY, Cheow PC, Chow
PK and Ooi LL: Factors affecting early mortality in spontaneous
rupture of hepatocellular carcinoma. ANZ J Surg. 76:448–452. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kirikoshi H, Saito S, Yoneda M, Fujita K,
Mawatari H, Uchiyama T, Higurashi T, Imajo K, Sakaguchi T, Atsukawa
K, et al: Outcomes and factors influencing survival in cirrhotic
cases with spontaneous rupture of hepatocellular carcinoma: A
multicenter study. BMC Gastroenterol. 9:292009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kung CT, Liu BM, Ng SH, Lee TY, Cheng YF,
Chen MC and Ko SF: Transcatheter arterial embolization in the
emergency department for hemodynamic instability due to ruptured
hepatocellular carcinoma: Analysis of 167 cases. Am J Roentgenol.
191:W231–W239. 2008. View Article : Google Scholar
|
|
16
|
Lai EC and Lau WY: Spontaneous rupture of
hepatocellular carcinoma: A systematic review. Acta Radiol.
141:191–198. 2006.
|
|
17
|
Lau WY: Primary hepatocellular
carcinomaDisease of the Liver and Biliary Tract. Blumgart LH and
Fong Y: 3rd edition. WB Saunders Co, Ltd.; London, England: pp.
1423–1450. 2000
|
|
18
|
Zhang YW, Ao J, Liu Y, Qiao MX, Yang XL,
Tang SX, Li C and Xu K: Pharmacokinetics of gelatin sponge
microparticles in a rabbit VX2 liver tumor model of hepatic
arterial chemoembolization. Tumour Biol. 35:10905–10910. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang YW and Liu Y: Transcatheter arterial
chemoembolization of hepatocellular carcinoma with 350-560 µm
gelatin sponge particles: Efficacy, tumour response and survival.
Zhonghua Gan Zang Bing Za Zhi. 21:637–638. 2013.(In Chinese).
PubMed/NCBI
|
|
20
|
Kamran AU, Liu Y, Li FE, Liu S, Wu JL and
Zhang YW: Transcatheter arterial chemoembolization with gelatin
sponge microparticles treated for BCLC stage B hepatocellular
carcinoma: A single center retrospective study. Medicine
(Baltimore). 94:e21542015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu Y, Zhang Y, Bautista D, Tang S, Zhou
J, Li C and Zhao G: Trans-arterial p53-gene-embolization with
gelatin sponge microparticles for hepatocellular carcinoma with
BCLC stage B: Single-centre experience. Cell Biochem Biophys.
71:99–104. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ramsey DE, Kernagis LY, Soulen MC and
Geschwind JF: Chemoembolization of hepatocellular carcinoma. J Vasc
Interv Radiol. 13:S211–S221. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
World Health Organization, . Cancer Pain
Relief and Palliative Care. Report of a WHO Expert Committee;
Geneva: 1990, pp. 7–21
|
|
24
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shin BS, Park MH and Jeon GS: Outcome and
prognostic factors of spontaneous ruptured hepatocellular carcinoma
treated with transarterial embolization. Acta Radiol. 52:331–335.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhu LX, Wang GS and Fan ST: Spontaneous
rupture of hepatocellular carcinoma. Br J Surg. 83:602–607. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jin YJ, Lee JW, Park SW, Lee JI, Lee DH,
Kim YS, Cho SG, Jeon YS, Lee KY and Ahn SI: Survival outcome of
patients with spontaneously ruptured hepatocellular carcinoma
treated surgically or by transarterial embolization. World J
Gastroenterol. 19:4537–4544. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Liu CL, Fan ST, Lo CM, Tso WK, Poon RT,
Lam CM and Wong J: Management of spontaneous rupture of
hepatocellular carcinoma: Single-center experience. J Clin Oncol.
19:3725–3732. 2001.PubMed/NCBI
|
|
29
|
Tarantino L, Sordelli I, Calise F, Ripa C,
Perrotta M and Sperlongano P: Prognosis of patients with
spontaneous rupture of hepatocellular carcinoma in cirrhosis.
Updates Surg. 63:25–30. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fujii M, Miyake H, Takamura K and Tashiro
S: Management of spontaneous ruptured hepatocellular carcinoma.
Nihon Geka Gakkai Zasshi. 105:292–295. 2004.(In Japanese).
PubMed/NCBI
|
|
31
|
Tanaka T, Yamanaka N, Oriyama T, Furukawa
K and Okamoto E: Factors regulating tumor pressure in
hepatocellular carcinoma and implications for tumor spread.
Hepatology. 26:283–287. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Llovet JM and Bruix J: Systematic review
of randomized trials for unresectable hepatocellular carcinoma:
Chemoembolization improves survival. Hepatology. 37:429–442. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cammà C, Schepis F, Orlando A, Albanese M,
Shahied L, Trevisani F, Andreone P, Craxì A and Cottone M:
Transarterial chemoembolization for unresectable hepatocellular
carcinoma: Meta-analysis of randomized controlled trials.
Radiology. 224:47–54. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kim YJ, Lee HG, Park JM, Lim YS, Chung MH,
Sung MS, Yoo WJ and Lim HW: Polyvinyl alcohol embolization adjuvant
to oily chemoembolization in advanced hepatocellular carcinoma with
arterioportal shunts. Korean J Radiol. 8:311–319. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Miyoshi A, Kitahara K, Kohya N, Noshiro H
and Miyazahi K: Outcomes of patients with spontaneous rupture of
hepatocellular carcinoma. Hepatogastroenterology. 58:99–102.
2011.PubMed/NCBI
|
|
36
|
Liu CL, Ngan H, Lo CM and Fan ST: Ruptured
hepatocellular carcinoma as a complication of transarterial oily
chemoembolization. Br J Surg. 85:512–514. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
National Cancer Institute. Common
Terminology Criteria for Adverse Events (CTCAE) version 4. United
States Department of Health and Human Services. 2009, http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7pdfAccessed
February 22, 2012.
|