Introduction
Pyogenic spondylitis (PS) is regarded as a serious
threat to human health worldwide (1); the disease accounts for 2–7% of all
bone and joint infections, with an annual incidence of 0.2–2
cases/10 million people (2). In
China, due to the increasing clinical use of antibiotics, typical
early cases of PS are rare, thus increasing the difficulty of
obtaining an early diagnosis (1).
Brucella spondylitis (BS) is primarily induced by infection with
the Brucella species, which accounts for 2–5% of all BS cases
(3). Brucellosis is a common
infectious disease in the Middle East, North America and
Mediterranean region (4). According
to previously published statistics, there are 5–6 million cases of
brucellosis worldwide, and 500,000 new cases are reported each year
(5,6). In China, brucellosis primarily occurs
in the northeast and northwest areas, where animal husbandry
industry is well developed (6).
However, as the consumption of the dairy products increases, the
incidence of the disease in cities and towns is increasing
(7). Tuberculous spondylitis (TS) is
the most dangerous and prevalent form of skeletal tuberculosis.
Tuberculosis is caused by Mycobacterium tuberculosis, 3% of
which is skeletal tuberculosis (8).
Tuberculosis has been recognized as the leading cause of mortality
from a curable infectious disease, and the WHO African region has
the highest estimated incidence rate; however, the majority of
patients with tuberculosis live in the most populated countries of
Asia (9).
Early diagnosis of spondylitis is difficult in
clinic due to its unusual signs and symptoms of fever and pain.
There are numerous similarities in the imaging and clinical
manifestations between PS, BS and TS; however, different treatments
are required for each disease (10,11).
Therefore, the early and correct diagnosis of spondylitis is
important for timely and effective intervention, thereby reducing
the occurrence of spinal deformity and dysfunction (12). Currently, histopathology and magnetic
resonance imaging (MRI) are widely used examination methods for
spondylitis in the clinic (13).
Numerous investigators are identifying ways to improve the
specificity and accuracy of diagnosing spondylitis according to
clinical symptoms, laboratory tests (including white blood cell,
C-reactive protein and erythrocyte sedimentation rate analysis) and
radiographic analysis (including X-ray, computed tomography (CT),
positron emission tomography-CT and MRI). However, there are few
studies focusing on the combination diagnosis with
histopathological and MRI examinations for spondylitis. In the
present study, the histopathological and MRI features of
spondylitis are retrospectively reviewed, and the application and
value of the combination diagnosis is discussed.
Materials and methods
Subjects
The study included 22 patients with PS (gender, 12
male and 10 female; age, 26–69 years; average age, 53 years), 20
patients with BS (gender, 11 male and 9 female; aged 24–62 years,
with an average age of 49 years), and 20 TS patients (10 males and
10 females, aged 22–57 years, with an average age of 45 years).
Patients were admitted to the Provincial Hospital Affiliated to
Shandong University (Jinan, China) between February 2012 and April
2014. Written informed consent was obtained from each patient, and
the study was approved by the ethics committee of the Provincial
Hospital Affiliated to Shandong University. Patients were divided
into groups according to their disease: PS, BS and TS.
Patient inclusion criteria for the study were as
follows: i) Patients diagnosed as spondylitis. Patients with PS
were diagnosed by positive blood culture or positive bacterial
culture of a biopsy specimen, and diagnosis was confirmed with
clinical follow-ups. Patients with BS were diagnosed by positive
blood culture, positive bacterial culture of a biopsy specimen, or
a titer >1:160 in the brucellosis agglutination test (14), and diagnosis was confirmed with
clinical follow-ups. Patients with TS were diagnosed by positive
blood culture, positive bacterial culture of a biopsy specimen, or
the detection of acid-fast bacilli by acid-fast staining, and
diagnosis was confirmed with clinical follow-ups. ii) Adults (age,
>18 years). iii) Patients with early spondylitis, with slight
spinal lesions and early clinical symptoms. iv) Patients from whom
the biopsy specimen was subjected to histopathological examination
and bacterial culture. v) Patients who underwent MRI of the spinal
lesions. vi) Patients with a complete date and follow-up period of
>6 months. Patient exclusion criteria for the study were: i)
Patients with autoimmune spondylitis. ii) Chronic cases confirmed
at admission into hospital. iii) Patients suffering from spinal
infection following surgery, or patients with advanced spondylitis.
iv) Dropouts due to other reasons, or patients who did not complete
the follow-up period.
Histopathological examination
Specimens were obtained by CT-guided percutaneous
vertebral biopsy. The tissue was fixed with 10% formaldehyde,
followed by decalcification with edathamil disodium. Once
dehydrated, the tissue was embedded in paraffin and cut into
sections (3–4 µm) using a microtome. The sections were then
subjected to the hematoxylin-eosin staining, and observed under a
microscope (BX51; Olympus Corporation, Tokyo, Japan).
MRI examination
MRI examination was performed using a medical Signa
HDx1.5T scanner (GE Healthcare Life Sciences, Chalfont, UK) and a
spine quadrature coil. The patient was laid in a supine position,
with the head towards the scanner. Conventional T1-weighted images
(T1WI) [repetition time (TR), 550 msec; echo time (TE), 14.2 msec;
section thickness, 3 mm; intersection gap, 0.5 m; matrix, 256×256;
number of excitations (NEX), 4; field of view (FOV), 33×33 cm] and
T2-weighted images (T2WI) (TR, 3000 msec; TE, 120.0 msec; section
thickness, 3 mm; intersection gap, 0.5 m; matrix, 256×256; NEX, 2;
FOV, 32×32 cm) were obtained in the sagittal, coronal and
horizontal planes. Gadolinium-diethylenetriamine pentaacetic acid
(Jinan Luxin Chemical Technology Co., Ltd., Jinan, China) was
injected to enhance imaging when necessary.
Statistical analysis
Data are presented as the mean ± standard deviation.
SPSS version 17.0 (IBM SPSS, Amronk, NY, USA) was used for
statistical analysis. One-way analysis of variance was used for
group comparisons. P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline characteristics
The baseline characteristics of all patients with
spondylitis are summarized in Table
I. No significant differences were observed in the gender, age
and body mass index between patients in the PS, and BS and TS
groups (P>0.05), indicating the patients were suitable for the
investigation.
 | Table I.Baseline characteristics of patients
with PS, BS and TS. |
Table I.
Baseline characteristics of patients
with PS, BS and TS.
|
| Group |
|
|---|
|
|
|
|
|---|
| Parameter | PS | BS | TS | P-value |
|---|
| Gender,
male:female | 12:10 | 11:9 | 10:10 | 0.283 |
| Age, years
(±SD) | 53.24±1.97 | 49.13±2.02 | 45.43±1.82 | 0.262 |
| Body mass index,
kg/m2 (±SD) | 23.15±3.49 | 24.23±4.17 | 23.23±3.75 | 0.299 |
Histopathological findings
The analysis of results from the histopathological
examinations of patients with PS, BS, and TS were retrospectively
reviewed by five senior spine surgeons blinded to the study. The
results demonstrated that there were no significant differences
observed in the plasmocyte infiltration between the PS, BS and TS
groups (P>0.05; Table II).
However, significant differences were observed in the
histopathological features across the PS, BS and TS groups
(P<0.05). These features were sequestrum, new bone formation,
epithelioid granuloma, Langerhans giant cells, caseous necrosis,
neutrophil infiltration, and lymphocyte infiltration (Table II).
 | Table II.Histopathological features of
patients with PS, BS and TS. |
Table II.
Histopathological features of
patients with PS, BS and TS.
|
| Group |
|
|---|
|
|
|
|
|---|
| Parameter | PS (%)a | BS (%)b | TS (%)b | P-value |
|---|
| Sequestrum |
0.0 | 20 | 50 | 0.000 |
| New bone
formation |
0.0 | 20 | 0 | 0.012 |
| Epithelioid
granuloma |
0.0 | 40 | 25 | 0.023 |
| Langerhans giant
cells |
0.0 | 0 | 25 | 0.010 |
| Caseous
necrosis |
0.0 | 0 | 25 | 0.010 |
| Predominant
neutrophil infiltration | 91.0 | 5 | 0 | 0.000 |
| Predominant
lymphocyte infiltration |
4.5 | 85 | 80 | 0.000 |
| Predominant
plasmocyte infiltration |
4.5 | 10 | 5 | 0.147 |
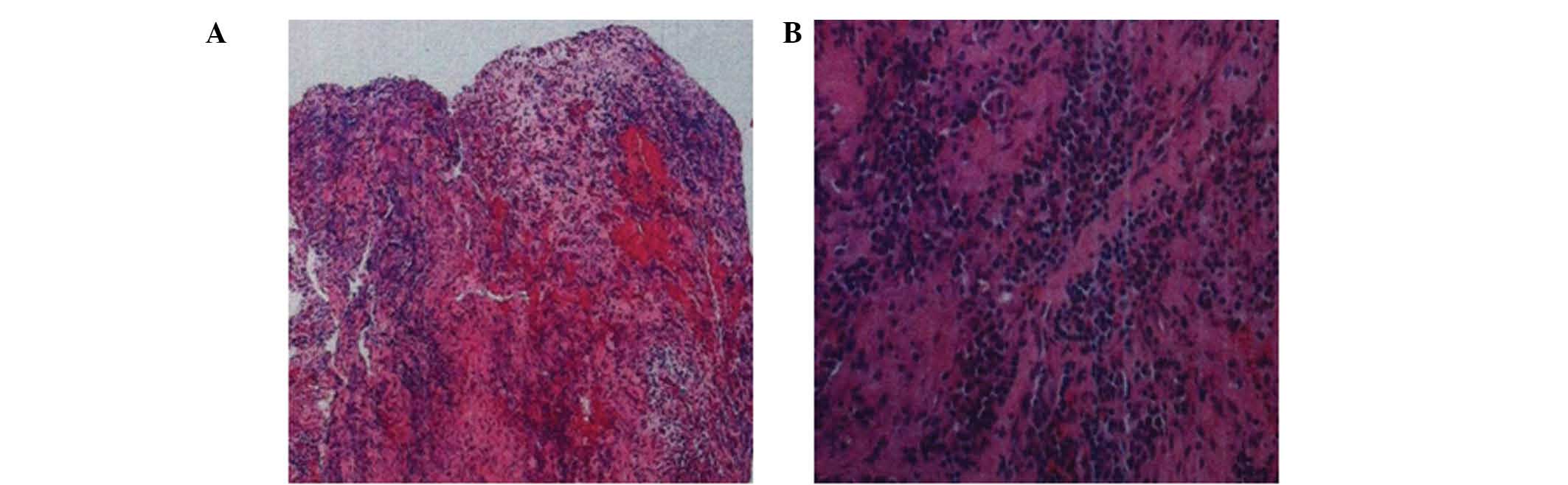
In particular, PS was characterized by predominant
neutrophil infiltration, the incidence of which was significantly
higher than that in the BS and TS groups (P<0.01; Fig. 1 and Table
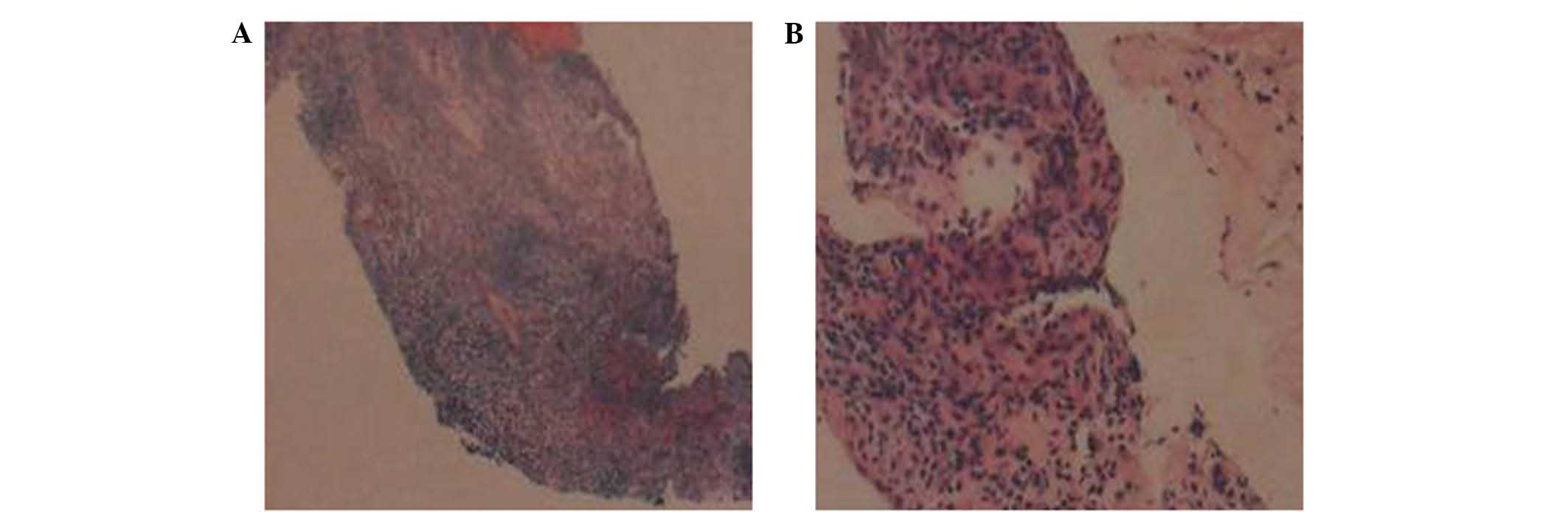
II). In addition, BS was characterized by histopathological
features including new bone formation, epithelioid granuloma, and
predominant lymphocyte infiltration, the incidences of which were
significantly higher than those in PS and TS groups (P<0.01;
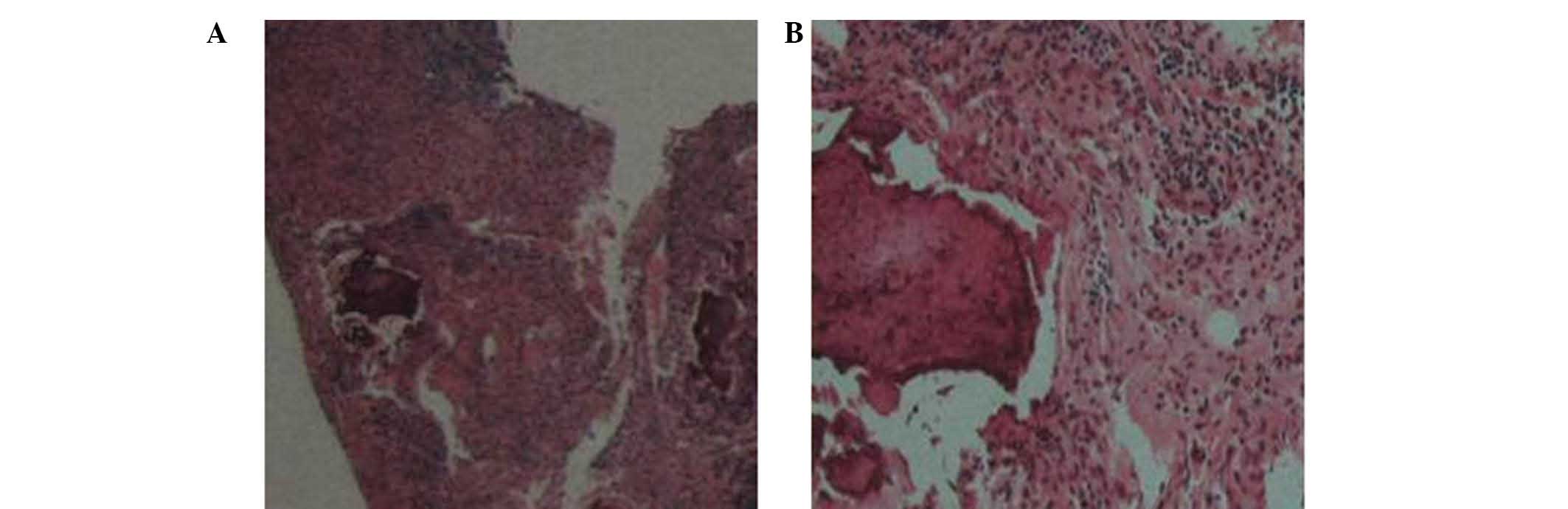
Fig. 2 and Table II). Furthermore, TS was
characterized by histopathological features including Sequestrum,
Langerhans giant cells, and caseous necrosis, which were
significantly different to the BS and PS groups (P<0.01;
Fig. 3 and Table II). These results suggested that
significant differences can be identified in the histopathological
features between different types of spondylitis.
Lesion locations
The lesion locations were determined and analyzed in
patients with PS, BS and TS. As shown in Table III, there were no significant
differences observed between the PS, BS and TS groups in the
cervical and sacral regions (P>0.05). However, for the thoracic
and lumbar regions, significant differences were observed between
the BS, PS and TS groups in the thoracic and lumbar regions
(P<0.05).
 | Table III.Lesion locations in patients with PS,
BS and TS. |
Table III.
Lesion locations in patients with PS,
BS and TS.
|
| Group |
|
|---|
|
|
|
|
|---|
| Lesion
location | PS (%)a | BS (%)b | TS (%)b | P-value |
|---|
| Cervical
vertebrae | 9 | 5 | 5 | 0.232 |
| Thoracic
vertebrae | 14 | 10 | 60 | 0.015 |
| Lumbar
vertebrae | 68 | 75 | 35 | 0.023 |
| Sacral
vertebrae | 9 | 10 | 0 | 0.269 |
The results showed that the majority of TS lesions
were located in the thoracic region (60%), the incidence of which
was significantly higher than that in the PS (14%) and BS (10%)
groups (P<0.01). In addition, 75% of the BS lesions were located
in the lumbar region, which was significantly higher than that in
the PS (68%) and TS (35%) groups (P<0.01). These results
suggested that significant differences can be identified in the
location of lesions in different types of spondylitis.
MRI features
The MRI results of patients with PS, BS and TS
patients were reviewed and analyzed. The results showed that no
significant differences were observed between the following MRI
features between the PS, BS and TS groups: Hypointense signal on
T1-weighted images, hyperintense signal on T2-weighted images,
presence of epidural abscesses, and involvement of multiple
vertebral bodies (P>0.05, Table
IV). However, significant differences were observed in the
following MRI features between the PS, BS and TS groups:
Intervertebral disk abnormality, lesion sites on the vertebral
bodies (ventral and/or lateral sides), vertebral body deformation,
paraspinal soft tissue abnormality, presence of intraosseous or
paraspinal abscesses, appearance of abscess walls, facet joint
involvement, and vertebral osteophyte formation (P<0.05;
Table IV).
 | Table IV.MRI findings for PS, BS, and TS
patients. |
Table IV.
MRI findings for PS, BS, and TS
patients.
|
| Group |
|
|---|
|
|
|
|
|---|
| Parameter | PS (%)a | BS (%)b | TS (%)b | P-value |
|---|
| Hypointense T1WI
signal | 86 | 90 | 85 | 0.2640 |
| Hyperintense T2WI
signal | 86 | 75 | 85 | 0.2270 |
| Abnormal
intervertebral disk signal | 91 | 35 | 15 | 0.0132 |
| Lesion sites on
vertebral bodies |
|
|
|
|
| Ventral
sides | 9 | 55 | 10 | 0.0320 |
| Lateral
sides | 0 | 10 | 50 | 0.0251 |
| Ventral
and lateral sides | 91 | 45) | 40 | 0.0114 |
| Vertebral body
deformation | 59 | 25 | 90 | 0.0213 |
| Abnormal paraspinal
soft tissue signal | 73 | 35 | 90 | 0.0178 |
| Intraosseous or
paraspinal abscess | 55 | 25 | 80 | 0.0021 |
| Thin and smooth
abscess wall | 33 | 0 | 75 | 0.0013 |
| Thick and irregular
abscess wall | 66 | 0 | 0 | 0.0013 |
| Thin and irregular
abscess wall | 0 | 100 | 25 | 0.0079 |
| Epidural
abscess | 14 | 10 | 10 | 0.1612 |
| Involved multiple
vertebral bodies (≥3) | 9 | 5 | 5 | 0.0732 |
| Facet joint
involvement | 0 | 20 | 5 | 0.0071 |
| Vertebral
osteophyte formation | 0 | 40 | 0 | 0.0000 |
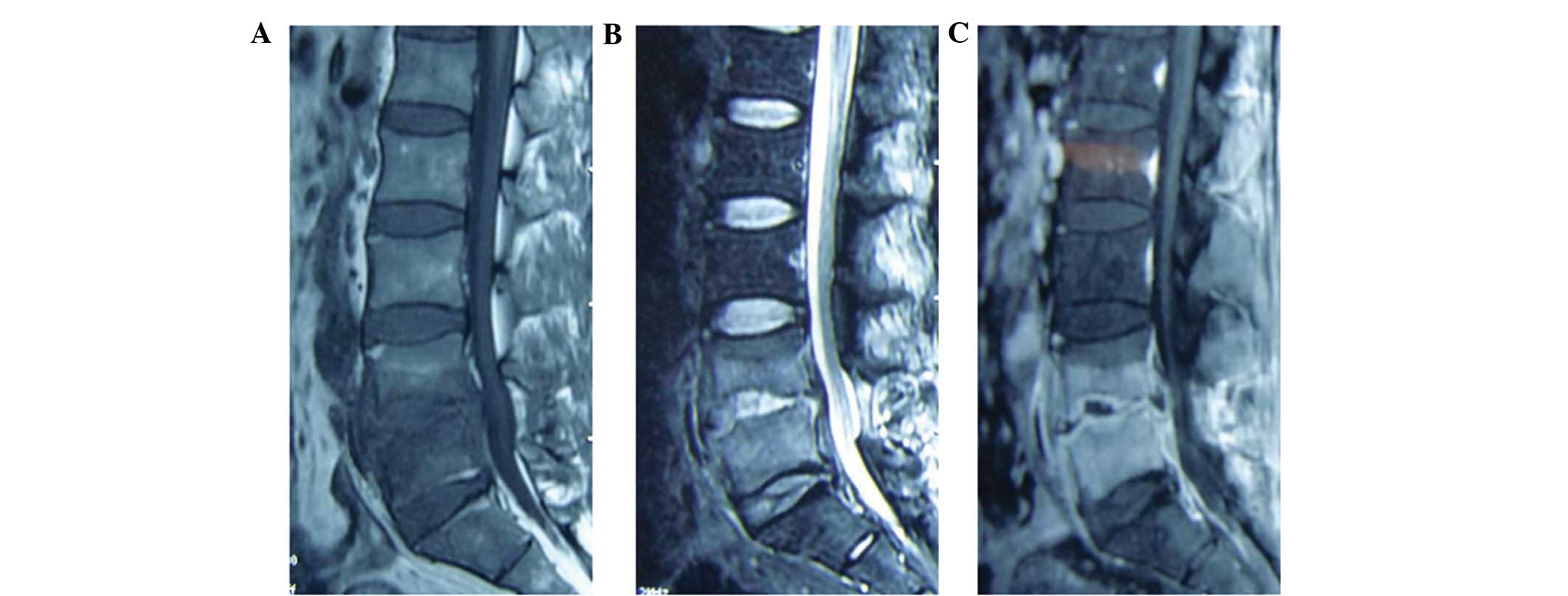
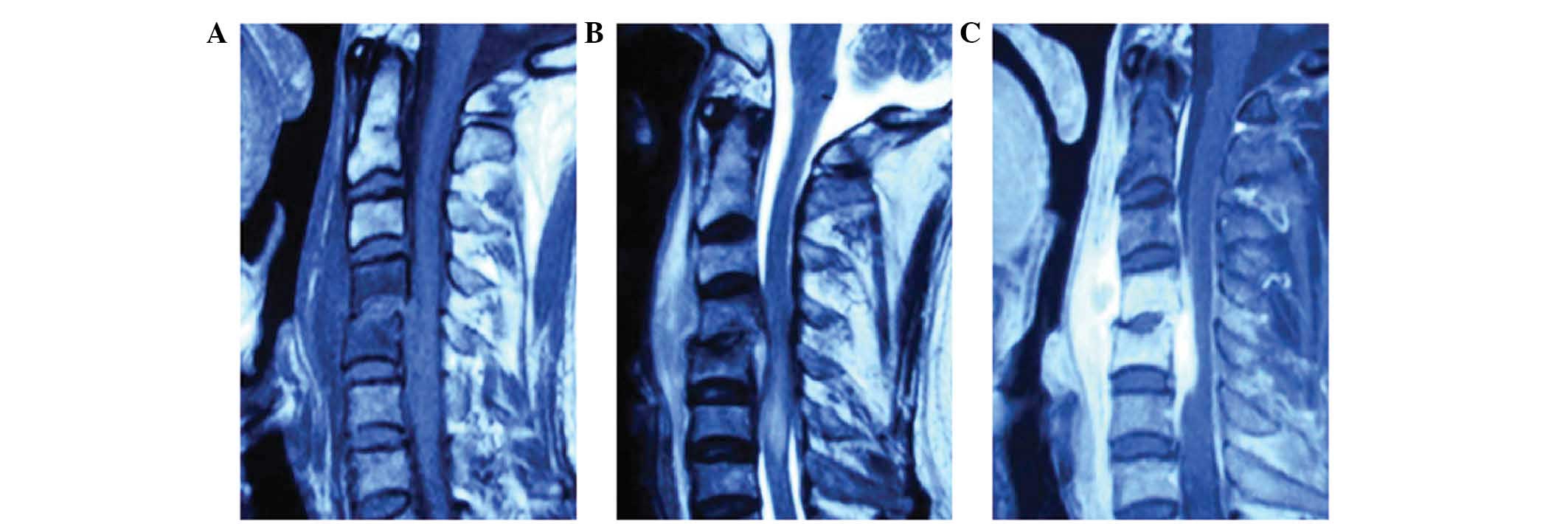
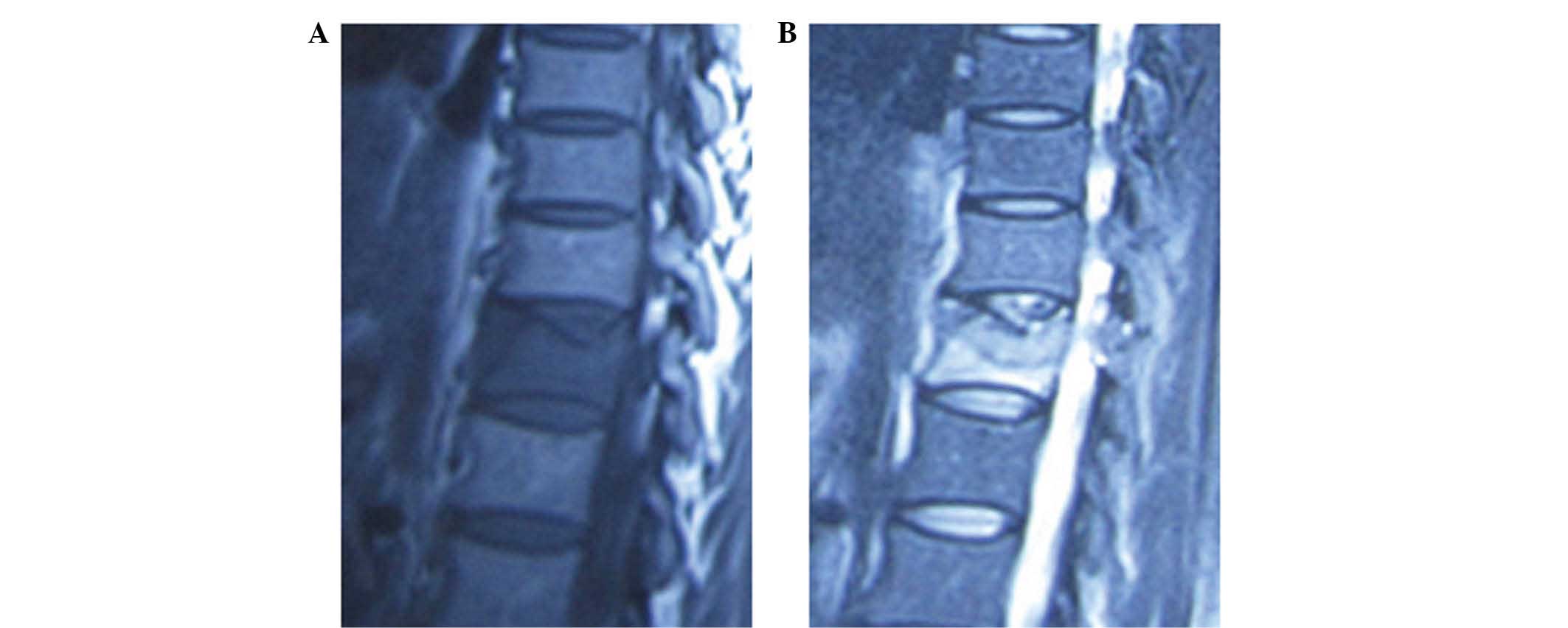
The incidence of the following MRI features was
significantly higher in the PS group in comparison with the BS and
TS groups, as indicated by the well-defined abnormal intervertebral
disk signal, lesions on the ventral and lateral sides of the
vertebral bodies, and thick and irregular abscess walls (P<0.05;
Figs. 4 and 5; Table
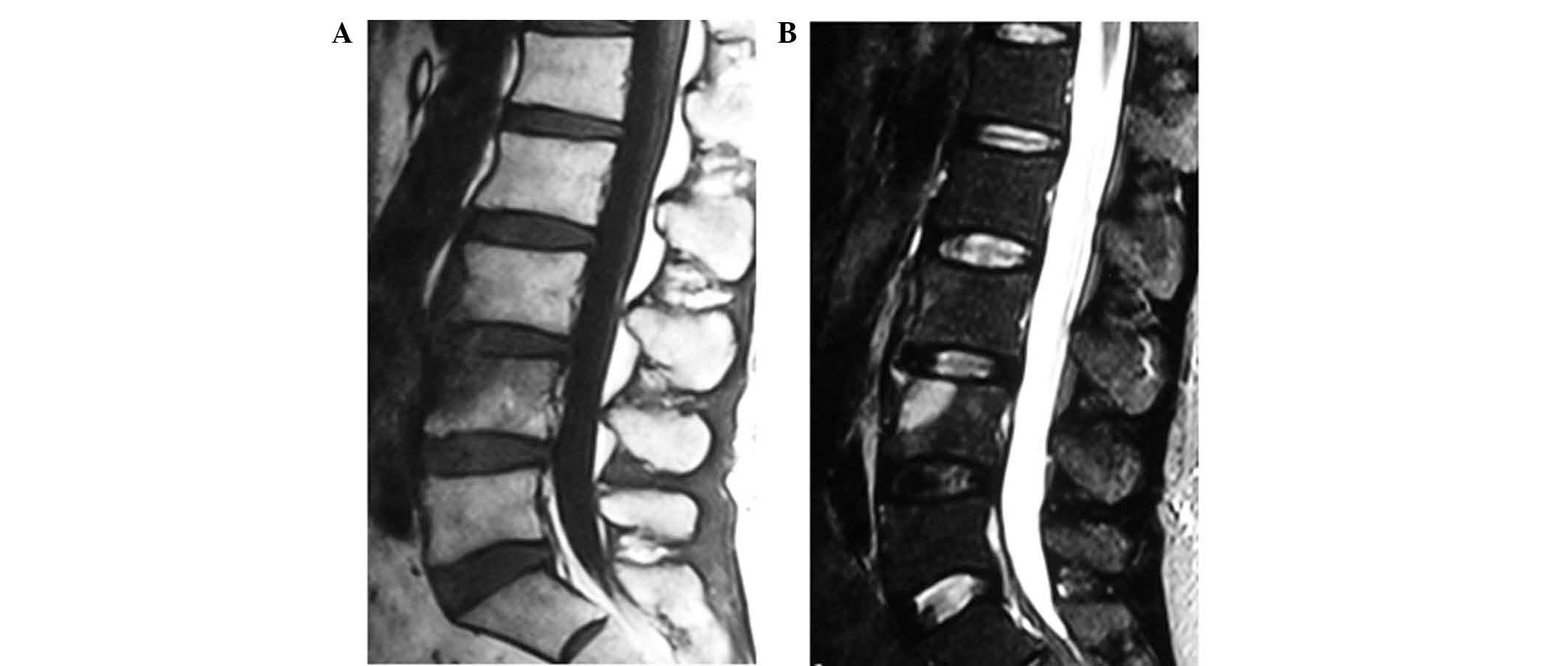
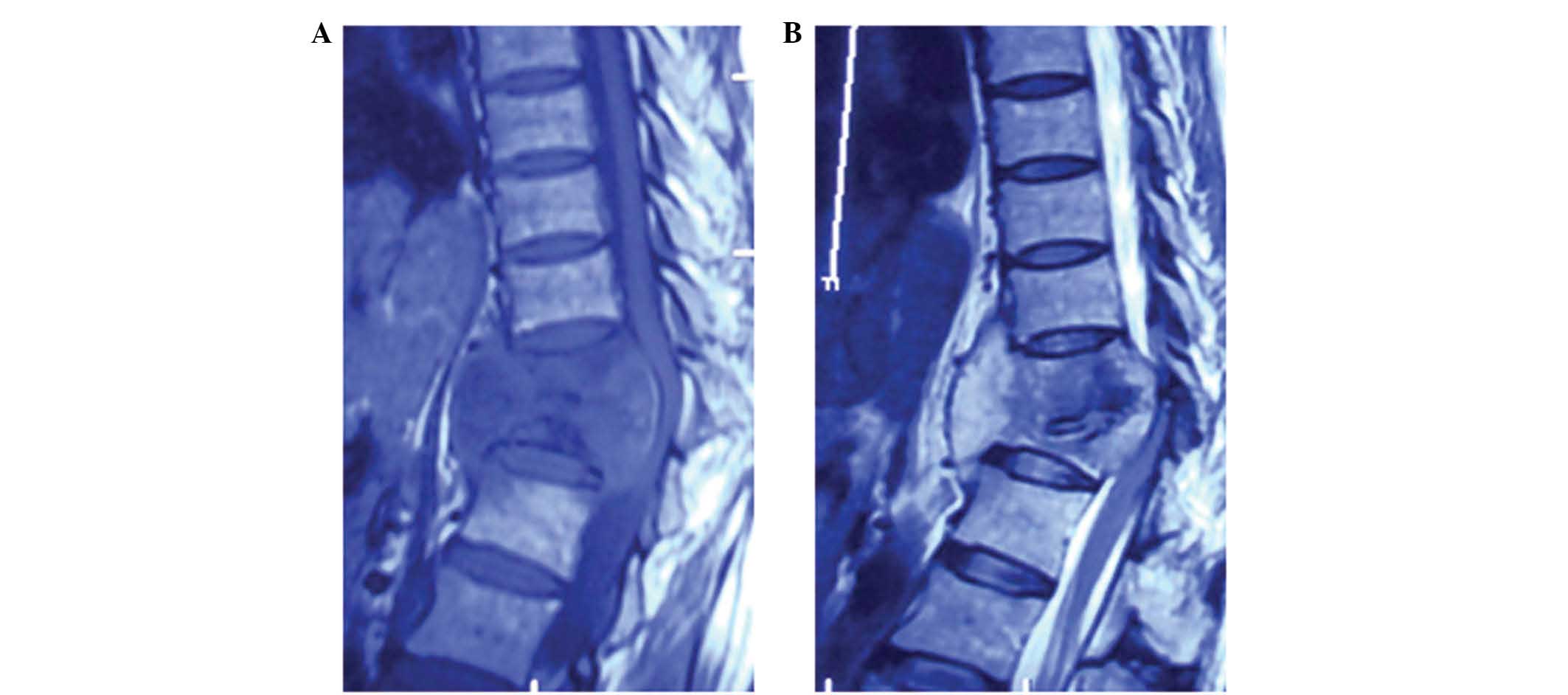
IV). In the BS group, the incidences of the following MRI
features were significantly higher than those in the PS and TS
groups: Lesions on the ventral sides of the vertebral bodies, no,
or very mild, vertebral body deformation, normal paraspinal soft
tissue signal, thin and irregular abscess walls, facet joint
involvement, and vertebral osteophyte formation (P<0.05;
Figs. 6 and 7; Table
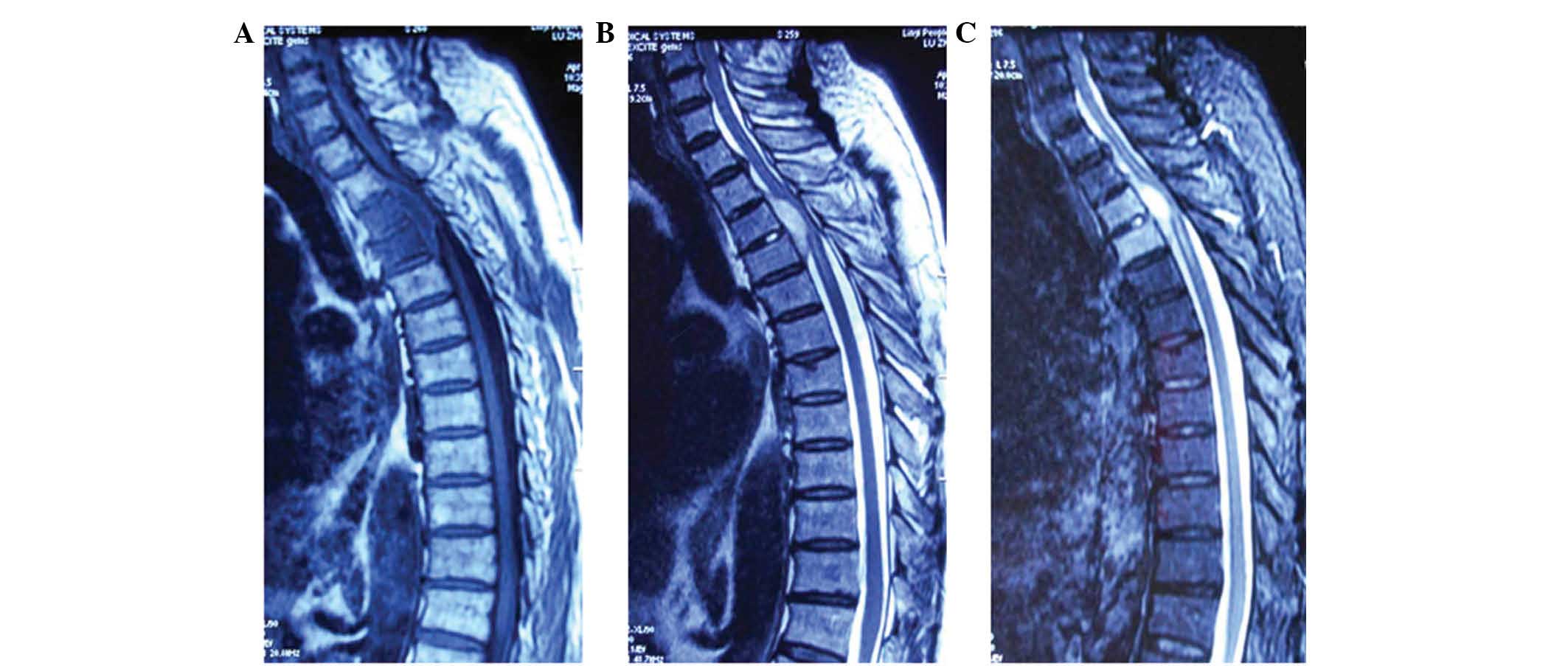
IV). In the TS group, the incidences of the following MRI
features were significantly higher than those in the PS and BS
groups: No obvious abnormal intervertebral disk signal, lesions on
the lateral sides of the vertebral bodies, obvious vertebral body
deformation, abnormal paraspinal soft tissue signal, presence of
intraosseous or paraspinal abscesses, and thin and smooth abscess
walls (P<0.05; Figs. 8 and
9; Table
IV). These results suggested that significant differences are
present in the MRI features between different types of
spondylitis.
Discussion
Diagnosing spondylitis in the early stages is
difficult due to its unusual signs and symptoms. However, the
disease can develop and progress into chronic inflammation without
a timely diagnosis and appropriate treatment (15–17). In
the present study, the histopathological and MRI features of
different types of spondylitis were analyzed and compared.
The analysis of results from the histopathological
examinations showed that the sequestrum and bone repairing process
is rarely observed in the early bone destruction experienced in PS,
however, the sequestrum and new bone formation were simultaneously
observed in BS. In TS, 50% of cases were accompanied with the
sequestrum, but no evidence of new bone formation was observed,
indicating the presence of severe bone destruction in the
development of the disease. In addition, PS was characterized by
the purulent exudates, without nodules. The histopathological
characteristics of BS included granulomatous inflammation, but no
caseous necrosis. These findings are in accordance with those
observed in Yang et al (18).
Granulomatous inflammation was also observed in TS; however, other
histopathological changes, such as exudation, hyperblastosis and
necrosis, may be expected, depending on the bacterial virulence and
patient resistance. Notably, the typical histopathological changes
of TS were observed to be the tuberculosis nodules, including
caseous necrosis, epithelioid tissue and Langerhans giant cells,
which may be used as markers for determining between different
types of spondylitis (19).
Neutrophils are the predominant infiltrating cell type in PS, and
these cells are important in resisting pyogenic bacterial infection
(20). However, BS samples are
primarily infiltrated with lymphocytes, which may be attributed to
the involvement of the humoral immune response in the early
development of the disease (21).
The predominant infiltrating cell type in TS was also the
lymphocyte.
From the analysis of lesion locations in patients
with spondylitis, 68.2% of the PS lesions were located in the
lumbar region, findings that are consistent with those in Colmenero
et al (10) and Antunes
(18). In addition, 85% of BS cases
were located in the lumbosacral region, also in agreement with
previous studies (3,22–26).
However, the majority of TS cases (60%) were located in the lower
thoracic region, similar to results obtained by Turunc et al
(27) and Jung et al
(28).
The results of the MRI examinations in the present
study demonstrated that no significant differences were present in
the hypointense T1WI, and the hyperintense T2WI, between the PS, BS
and TS groups. The MRI features of early PS included abnormal
intervertebral disk signals (91%), which was not obvious in the MRI
results of patients with BS. This finding of the abnormal
intervertebral disk signal in MRI features of PS is in accordance
with those of previous studies (29,30),
which may be due to the fact that the lymphocyte infiltration was
predominantly observed in the BS cases, suggesting the presence of
cell immune responses (21), which
would contribute to the lower incidence of intervertebral disk
abnormalities in the disease pathogenesis. The incidence of
intervertebral disk abnormalities in the TS group in the present
study was 15%, and this low percentage may be attributed to the
fact that Mycobacterium tuberculosis did not effectively
decompose the intervertebral disk, which is in accordance with a
previous study (31). Of note, the
abnormal intervertebral disk signal was observed in the MRI results
of three TS cases, in which Mycobacterium tuberculosis would
destroy the endplate and then infiltrate into the intervertebral
disk (31). In addition, uniform
signals in the abnormal intervertebral disk were observed, with
normal height but intense spot-like cystic signals, indicative of
the suspected formation of a tuberculosis abscess that was
identified to be a typical MRI feature for TS, which is in
accordance with findings from Zhou et al (32).
In patients with PS, lesions were located on the
ventral and lateral sides of the vertebral bodies, with an
incidence of 91% in the present study. This phenomenon may be
because PS is primarily caused by non-specific bacteria, and,
therefore, the edema may quickly spread to the entire vertebral
body; this could be used as a marker for the disease (1). In patients with BS, the lesions were
mainly observed on the ventral sides of the vertebral bodies, with
an incidence of 55%, which is in accordance with previous findings
(29,33). These lesions in BS may be explained
by the fact that the disease originates from the upper endplate
with adequate blood supply, and the lesion may be limited within
the ventral side of the vertebral body as a result of the
non-invasive disease progression (29). In addition, consistent with previous
findings from Turunc et al (27), the lesions in the TS group were
primarily located on the lateral sides of the vertebral bodies,
with an incidence of 50%, which may be regarded as a typical
feature of the disease. However, Currie et al (13) demonstrated that TS may originate from
the ventral side of the vertebral body near the endplate, and
therefore the MRI feature of early TS may be edema within the
endplate. Further in-depth studies are required to resolve this
contradiction.
A total of 59% (13 cases) of the patients with PS
experienced vertebral body deformation, including 10 cases of
endplate destruction and 3 cases of vertebral bone destruction. In
addition, 25% (5 cases) of patients with BS experienced vertebral
body deformation, including 4 cases of wedge-shaped vertebral
bodies with bone hyperplasia, and 1 case of moderate endplate and
vertebral destruction. Furthermore, 90% (18 cases) of patients with
TS experienced vertebral body deformation, including 12 cases of
vertebral defect, 2 cases of wedge-shaped vertebral bodies, and 4
cases of moderate endplate and vertebral destruction. From these
results, it is evident that PS is associated with diffuse lesions
and bone destruction, while obvious bone destruction and spinal
kyphosis deformity is associated with TS. On the other hand,
lesions were limited in patients with BS, and new bone formation
was observed during the bone destruction, resulting in non-altered
or mild wedging morphology without obvious endplate damage
(34). The results from the present
study show that 40% of patients with BS experienced osteophytes due
to hyperosteogeny, which was in accordance with previous findings
(29).
The results from the present study show that
abnormal signals with unclear boundaries were observed in the
paraspinal soft tissue in early PS cases. Multiple small abscess
cavities within the large abscess, which may be associated with the
inflammation induced by the neutrophil proteolytic enzymes
(35), were observed. In 66% (8
cases) of patients with PS, thick and irregular abscess walls were
observed, a finding that is in accordance with Jung et al
(28). Paraspinal soft tissue
abnormality and abscesses were observed in 5 patients with early
BS, the majority of which were single lesions with a small lesion
area, and thin and irregular abscess walls, findings that are in
accordance with those in Yang et al (36). It has been demonstrated that the
paraspinal soft tissue and the psoas abscesses are involved in the
development of TS (37). In the
present study, the incidence of paraspinal soft tissue abnormality
was 90% in the TS group, with an abscess incidence of 80%. In
addition, 75% of TS cases were associated with the thin and smooth
abscess walls, which is in accordance with previous findings
(29,38). Furthermore, in the present study, the
incidence of the involvement of multiple vertebral bodies in the
PS, BS, and TS groups was 9, 5 and 5%, respectively. These
incidences are slightly lower than previously published results
(3,25,28). In
the present study, epidural abscesses were rarely observed in the
early stages of PS, BS and TS, which is in agreement with previous
findings (13,33,38).
In conclusion, the results from the present study
show that PS is histopathologically characterized by predominant
neutrophil infiltration with no sequestrum, new bone formation,
Langerhans giant cells and caseous necrosis. From the MRI features,
PS lesions were primarily identified in the lumbar region, which
may be characterized by the well-defined abnormal intervertebral
disk signal, lesions on the ventral and lateral sides of the
vertebral bodies, vertebral body deformation, paraspinal soft
tissue abnormality with large and unclear boundaries, thick and
irregular abscess walls, and multiple small abscess cavities,
without the involvement of facet joints or the formation of
osteophytes. In addition, the histopathological features of BS
included predominant lymphocyte infiltration, sequestrum, new bone
formation, and epithelioid granuloma, without Langerhans giant
cells or caseous necrosis. Furthermore, the MRI features of BS were
lesions, primarily in the lumbar region, mild intervertebral disk
destruction, lesions on the ventral sides of the vertebral bodies,
facet joint involvement, and vertebral osteophyte formation, with
no, or very mild, vertebral body deformation and abnormal
paraspinal soft tissue signal (the majority of which are single
lesions with a small area, and thin and irregular abscess walls).
The histopathological features of TS included predominant
lymphocyte infiltration, sequestrum without new bone formation,
epithelioid granuloma, Langerhans giant cells and caseous necrosis.
The MRI features of TS were lesions, primarily in the thoracic
region, very mild intervertebral disk damage, lesions on the
lateral sides of the vertebral bodies, vertebral body deformation,
abnormal paraspinal soft tissue signal (with a large area, and thin
and smooth abscess walls), and rare involvement of facet joints and
formation of osteophytes. These results suggest that
histopathological and MRI analysis can distinguish between PS, BS
and TS pathogenesis, which may contribute towards the ability to
distinguish between PB, BS and TS during the diagnosis of
spondylitis.
Acknowledgements
The authors thank Dr Chen Liang of the Department of
Spinal Surgery, Provincial Hospital Affiliated to Shandong
University (Jinan, China) for the kind assistance in the collection
of data.
References
|
1
|
Cheung WY and Luk KD: Pyogenic
spondylitis. Int Orthop. 36:397–404. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sapico FL and Montgomerie JZ: Pyogenic
vertebral osteomyelitis: Report of nine cases and review of the
literature. Rev Infect Dis. 1:754–776. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Solera J, Lozano E, Martínez-Alfaro E,
Espinosa A, Castillejos ML and Abad L: Brucellar spondylitis:
Review of 35 cases and literature survey. Clin Infect Dis.
29:1440–1449. 1999. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Colmenero JD, Cisneros JM, Orjuela DL,
Pachón J, Garcia-Portales R, Rodriguez-Sampedro F and Juarez C:
Clinical course and prognosis of Brucella spondylitis. Infection.
20:38–42. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang Dali and Zhang Shiyi: Advances in
treatment of acute brucellosis. Zhong Guo Gan Ran Kong Zhi Za Zhi.
16:94–95. 2001.(In Chinese).
|
|
6
|
Shang DQ: Research advances in brucellosis
disease. Zhong Guo Gan Ran Kong Zhi Za Zhi. 19:204–212. 2004.(In
Chinese).
|
|
7
|
Lin C and Liu X: Analysis of brucellosis
infection through diet. Zhong Guo Ren Shou Gong Huan Bing Xue Bao.
17:58–59. 2001.(In Chinese).
|
|
8
|
Koh DM, Bell JR, Burkill GJ, Padley SP and
Healy JC: Mycobacterial infections: Still a millennium bug-the
imaging features of mycobacterial infections. Clin Radiol.
56:535–544. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dye C: Global epidemiology of
tuberculosis. Lancet. 367:938–940. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Colmenero JD, Jiménez-Mejías ME,
Sánchez-Lora FJ, Reguera JM, Palomino-Nicás J, Martos F, de las
Heras J García and Pachón J: Pyogenic, tuberculous, and brucellar
vertebral osteomyelitis: a descriptive and comparative study of 219
cases. Ann Rheum Dis. 56:709–715. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yilmaz MH, Mete B, Kantarci F, Ozaras R,
Ozer H, Mert A, Mihmanli I, Ozturk R and Kanbergoglu K:
Tuberculous, brucellar and pyogenic spondylitis: comparison of
magnetic resonance imaging findings and assessment of its value.
South Med J. 100:613–614. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bettini N, Girardo M, Dema E and
Cervellati S: Evaluation of conservative treatment of non specific
spondylodiscitis. Eur Spine J. 18:(Suppl 1). 143–150. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Currie S, Galea-Soler S, Barron D,
Chandramohan M and Groves C: MRI characteristics of tuberculous
spondylitis. Clin Radiol. 66:778–787. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao GM, Li F, Sun TS, Wu J, Guan K and
Zhang ZC: Diagnosis and treatment of Brucella spondylitis. Zhong
Guo Ji Zhu Ji Sui Za Zhi. 17:437–439. 2007.(In Chinese).
|
|
15
|
Yee DK, Samartzis D, Wong YW, Luk KD and
Cheung KM: Infective spondylitis in Southern Chinese: A descriptive
and comparative study of ninety-one cases. Spine. 35:635–641. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fukuda K, Miyamoto H, Uno K and Okada Y:
Indications and limitations of conservative treatment for pyogenic
spondylitis. J Spinal Disord Tech. 27:316–320. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yoon YK, Jo YM, Kwon HH, Yoon HJ, Lee EJ,
Park SY, Pary SY, Choo EJ, Ryu SY, Lee MS, et al: Differential
diagnosis between tuberculous spondylodiscitis and pyogenic
spontaneous spondylodiscitis: A multicenter descriptive and
comparative study. Spine J. 15:1764–1771. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang X, Shi W, Du YK, Meng XY and Zou YW:
Imaging manifestations and pathological characters of the brucellar
spondylitis. Shi Yong Fang She Xue Za Zhi She. 24:522–525. 2008.(In
Chinese).
|
|
19
|
Duan H, Yang H, Zuo J, Chen G, Zhou L and
He Y: Analysis: Pathology of 6 cases spine tuberculosis. Sheng Wu
Gu Ke Cai Liao Yu Lin Chuang Yan Jiu Za Zhi She. 8:1–3. 2011.(In
Chinese).
|
|
20
|
Li Y and Tang J: Pathology. 6th version.
People's Medical Publishing House; Beijing: 2006, View Article : Google Scholar
|
|
21
|
Zhong X, Chen Z and Huang K: Research
advance on Brucellosis virulence factors and treatment. Xu Mu Yu
Shou Yi. 40:96–101. 2008.(In Chinese).
|
|
22
|
Antunes JL: Infections of the spine. Acta
Neurochir (Wien). 116:179–186. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mete B, Kurt C, Yilmaz MH, Ertan G, Ozaras
R, Mert A, Tabak F and Ozturk R: Vertebral osteomyelitis: Eight
years' experience of 100 cases. Rheumatol Int. 32:3591–3597. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Colmenero JD, Ruiz-Mesa JD, Plata A,
Bermúdez P, Martín-Rico P, Queipo-Ortuño MI and Reguera JM:
Clinical findings, therapeutic approach, and outcome of brucellar
vertebral osteomyelitis. Clin Infect Dis. 46:426–433. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ariza J, Gudiol F, Valverde J, Pallarés R,
Fernández-Viladrich P, Rufí G, Espadaler L and Fernández-Nogues F:
Brucellar spondylitis: A detailed analysis based on current
findings. Rev Infect Dis. 7:656–664. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Glasgow MM: Brucellosis of the spine. Br J
Surg. 63:283–288. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Turunc T, Demiroglu YZ, Uncu H, Colakoglu
S and Arslan H: A comparative analysis of tuberculous, brucellar
and pyogenic spontaneous spondylodiscitis patients. J Infect.
55:158–163. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jung NY, Jee WH, Ha KY, Park CK and Byun
JY: Discrimination of tuberculous spondylitis from pyogenic
spondylitis on MRI. Am J Roentgenol. 182:1405–1410. 2004.
View Article : Google Scholar
|
|
29
|
Özaksoy D, Yücesoy K, Yücesoy M,
Kovanlikaya I, Yüce A and Naderi S: Brucellar spondylitis: MRI
findings. Eur Spine J. 10:529–533. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ledermann HP, Schweitzer ME, Morrison WB
and Carrino JA: MR imaging findings in spinal infections: Rules or
myths? Radiology. 228:506–514. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Almeida A: Tuberculosis of the spine and
spinal cord. Eur J Radiol. 55:193–201. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhou J: The early diagnostic value of MRI
on spinal tuberculosis. Zhong Guo Zhong Xi Yi Jie He Ying Xiang Xue
Za Zhi. 4:362–364. 2010.(In Chinese).
|
|
33
|
Çelik AK, Aypak A and Aypak C: Comparative
analysis of tuberculous and brucellar spondylodiscitis. Trop Doct.
41:172–174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wu W, Liu B, Liu Z, Cui SJ and Guo HB: MRI
in the differential diagnosis of brucella spondylitis and spinal
tuberculosis. Zhong Guo Mei Rong Yi Xue. 21:140–141. 2012.(In
Chinese).
|
|
35
|
Zhou S, Wang J, Zhao X and Fan C: MR
imaging manifestations and staging of pyogenic spondylitis. Ying
Xiang Zhen Duan Yu Jie Ru Fang She Xue. 20:218–221. 2011.(In
Chinese).
|
|
36
|
Yang XM, Shi W, Du YK, Meng XY and Zou YW:
Manifestation of clinical imageology and surgical treatment of the
brucellosis spondylitis. Orthop J Chin. 19:1463–1466. 2007.
|
|
37
|
Hong SH, Kim SM, Ahn JM, Chung HW, Shin MJ
and Kang HS: Tuberculous versus pyogenic arthritis: MR imaging
evaluation. Radiology. 218:848–853. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yang JZ, Wang CJ, He FL, Chen SW and Huang
YF: MR imaging of spondylitis (report of 11 cases). Zhong Guo Yi
Xue Ying Xiang Ji Shu. 15:488–489. 2002.(In Chinese).
|