Introduction
The arterial catheter is located between the
descending part of aortic arch and the pulmonary artery
bifurcation, approaching the arteriae pulmonalis sinistra and it is
an important channel for fetal circulation. Normally, the function
of arterial catheter would close between 10–15 h after birth. The
arterial catheter that continues to open after 10–15 h is defined
as patent ductus arteriosus (PDA). The arterial ducts of premature
infants due to the maldevelopment of arterial duct wall and the
abnormal secretion of prostaglandin, always fail to close in time,
thus resulting in left-to-right shunt. Due to their poor left
ventricular systolic functions, premature infants are vulnerable to
heart failure and pulmonary edema, and even symptomatic PDA (sPDA),
which is also known as hemodynamically significant PDA (hsPDA)
(1,2). Oral administration of indomethacin or
ibuprofen to premature infants could significantly lower the level
of prostaglandin E2 (PGE2), and promote
constriction and closure of the arterial duct (3–5).
Hammerman et al (6) reported
that, acetaminophen caused arterial duct closure in 5 premature
hsPDA infants that were not successfully treated with ibuprofen. In
this context, to understand the effect of acetaminophen treatment
on premature sPDA infants, we designed prospective randomized
controlled trials (RCTs), aiming to utilize and develop plasma and
urinary PGE2 levels as indicators of progress of
arterial duct closure in a non-invasive manner.
Patients and methods
Patients
The patients of this RCT were premature infants who
were admitted to the Neonatal Ward of Pediatrics Division of the
Affiliated Xuzhou Hospital of Medical College of Southeast
University between October, 2012 and June, 2015.
Sample size estimation
The sample size for this RCT was calculated based on
the results of a previous study (5)
and literature (4). Efficacy
(1-false negative rate β) was set at 80% and the false-negative
rate at α=0.05. According to our estimation, the sample size for
each group was 39 patients.
Inclusion and exclusion criteria
The patients satisfying the following criteria were
included in the presen study: i) gestational age, <37 weeks; ii)
admitted to hospital within 24 h after birth; iii) sPDA diagnosis
was made between 15 h to 10 days after birth and confirmed through
echocardiogram to be sPDA if the patient showed at least three of
the six clinical manifestations. These were: i) systolic or
consecutive murmur in left border of sternum; ii) strengthened beat
of anterior thorax; iii) locomotive pulse; iv) tachycardia in quiet
state; v) unexplainable deterioration of respiratory condition; and
vi) increased pulmonary vasculature shadows and enlarged heart or
signs of pulmonary edema under chest X-ray examination. Diagnostic
criteria of echocardiography was: i) left atrial: aortic root
diameter ratio, (LA:Ao) >1.4; ii) pulmonary artery diastolic
back flow (reflux); and iii) PDA catheter diameter >1.4 mm
(1,7).
The patients were excluded from the study if: i)
patients presented with any of the following medication
contraindications such as thrombocytopenia (blood platelet count
<50×109/l), hemorrhagic disease, oliguria (urine
volume per 8 h <8 ml/kg), necrotizing colitis, intestinal
perforation, high serum creatinine (>159.1 µmol/l), and alanine
aminotransferase (>40 U/l) levels (1,2); ii)
patients with congenital heart diseases such as ventricular septal
defect, complex heart disease; and iii) patients with incomplete
treatment or willing to depart from the study due to personal
reasons.
A total of 95 patients met the inclusion criteria,
of whom 8 patients were excluded for various reasons (reduced
platelet count in 2 patients, 1 patient had sepsis with
disseminated intravascular coagulation, 1 patient had oliguria, 1
patient had necrotizing colitis, 1 patient had complex heart
disease and lack of required data for this study in 2 patients).
Subsequently, 87 patients were included in the study.
Collection of data and analyses of
parameters prior to treatment
Once the premature infants were admitted to
hospital, information was collected and recorded including: i)
gender, with or without use of a full course of hormone of the
pregnant mother 7 days to 24 h before delivery; ii) presence or
absence of infection in the pregnant mother; iii) premature rupture
of membrane >18 h or less; iv) gestational age; v) delivery
mode; vi) birth weight; vii) 5-min Apgar scoring <8 or >8;
viii) with or without respiratory distress syndrome; and ix) number
of days of positive pressure ventilation.
Tests such as platelet count, serum creatinine
glutamic-pyruvic transaminase, and fecal occult blood were also
carried out in patients.
Treatment of patients and analysis of
parameters
The patients were randomly divided into the
ibuprofen group (n=43) and acetaminophen group (n=44) based on a
computer-generated random number table. The patients in the
ibuprofen group were treated by oral administration of 10 mg/kg
ibuprofen suspension initially, followed by 5 mg/kg during first 24
and 48 h later. Patients in the acetaminophen group were treated
with oral administration of 15 mg/kg acetaminophen orally once in
every 6 h for a total of 3 days. On the completion of 3 days,
ultrasonic cardiogram, platelet count, serum creatinine, glutamic
pyruvic transaminase, and fecal occult blood were re-examined. The
incidence of intraventricular hemorrhage (IVH), neonatal
necrotizing enterocolitis (NEC) and bronchopulmonary dysplasia
(BPD) were also recorded.
Detection of PGE2 in blood
and urine
The PGE2 level was estimated using a
commercially availed ELISA kit following the manufacturer's
instructions (VICMED Bioengineering Co., Ltd., China).
The present study conformed to ethical requirements
of the Affiliated Xuzhou Hospital of Medical College of Southeast
University. The parents of the patients were aware of the treatment
and signed informed consent.
Statistical analysis
The χ2 test was applied to compare the
collected information between the two groups. The t-test was
applied to compare data having normal distribution, whereas, the
Mann-Whitney U test method was utilized to compare data having
skewed distribution between the groups. The paired-samples
Student's t-test was used for intra-group comparison of the data
having normal distribution before and after treatment. The Pearson
correlation coefficient test was applied in the correlation
analysis of the bivariate normal distribution data. Statistical
analyses were carried out using IBM SPSS 20.0 software (Armonk, NY,
USA). P<0.05 was considered of statistical significance.
Results
Clinical characteristics of sPDA
infants of the ibuprofen and acetaminophen groups
The various clinical characteristics including
weight at birth, arterial catheter diameter, and gestational week
between the two groups of sPDA infants were not significantly
different (P>0.05; Table I).
 | Table I.Clinical characteristics of sPDA
infants of the ibuprofen and acetaminophen groups. |
Table I.
Clinical characteristics of sPDA
infants of the ibuprofen and acetaminophen groups.
| Characteristics | Ibuprofen group
(n=43) | Acetaminophen group
(n=44) |
χ2/t/Z | P-value |
|---|
| Male, n (%) | 25 (58.1) | 27 (61.4) |
χ2=0.094 | 0.759 |
| Hormone in full
pregnancy course, n (%) | 28 (65.1) | 25 (56.8) |
χ2=0.629 | 0.428 |
| Maternal infection, n
(%) | 4 (9.3) | 6 (13.6) |
χ2=0.089 | 0.766 |
| Premature rupture of
membrane >18 h, n (%) | 8 (18.6) | 10 (22.7) |
χ2=0.225 | 0.635 |
| Gestational age
(weeks) | 33.4±2.1 | 33.6±2.1 | t=−0.491 | 0.625 |
| Cesarean delivery, n
(%) | 24 (55.8) | 28 (63.6) |
χ2=0.553 | 0.457 |
| Birth weight (g) | 2,091±657 | 2,219±606 | t=−0.946 | 0.347 |
| SGA, n (%) | 9 (20.9) | 6 (13.6) |
χ2=0.811 | 0.368 |
| 5 min Apgar scoring
<8, n (%) | 15 (34.9) | 18 (40.9) |
χ2=0.335 | 0.563 |
| RDS, n (%) | 14 (32.6) | 12 (27.3) |
χ2=0.290 | 0.590 |
| Positive pressure
ventilation (days)a | 3.7 (1.9, 6.1) | 4.5 (3.0, 6.7) | Z=1.277 | 0.201 |
| Age at ultrasonic
cardiogram examination (days) | 5.8±2.0 | 6.4±1.8 | t=−1.527 | 0.131 |
| Urine amount
(ml/kg•h) | 2.52±0.54 | 2.48±0.76 | t=0.222 | 0.825 |
| Pulse pressure
difference (mmHg) | 24.2±3.9 | 23.3±4.7 | t=0.880 | 0.381 |
| LA:Ao | 1.55±0.31 | 1.53±0.31 | t=0.323 | 0.748 |
| Arterial catheter
diameter (mm) | 1.84±0.43 | 2.09±0.46 | t=−1.491 | 0.140 |
Effect of treatment in sPDA infants of
the ibuprofen and acetaminophen groups
PDA closure rate, fecal occult blood positive rate,
IVH, NEC, and BPD incidence rates were similar in the patients of
the two groups (P>0.05). Oliguria was less frequent in the
acetaminophen group than in the ibuprofen group, but this
difference was insignificant (P=0.108; Table II).
 | Table II.Effect of ibuprofen and acetaminophen
treatment in sPDA infants. |
Table II.
Effect of ibuprofen and acetaminophen
treatment in sPDA infants.
|
| Ibuprofen group
(n=43), n (%) | Acetaminophen group
(n=44), n (%) | χ2 | P-value |
|---|
| PDA occlusion | 33 (76.7) | 31 (70.5) | 0.442 | 0.506 |
| Oliguria | 6
(14.0) | 1 (2.3) | 2.587 | 0.108 |
| Positive stool
OB | 4 (9.3) | 2 (4.5) | 0.205 | 0.651 |
| IVH | 4 (9.3) | 5
(11.4) | 0.000 | 1.000 |
| NEC | 5
(11.6) | 4 (9.1) | 0.001 | 0.971 |
| BPD | 6
(14.0) | 5
(11.4) | 0.132 | 0.716 |
PGE2 level in sPDA infants
of the ibuprofen and acetaminophen groups
The treatment of sPDA infants with ibuprofen or
acetaminophen resulted in a significant decrease of plasma and
urinary PGE2 levels compared with their levels before
treatment (P<0.05). Furthermore, plasma and urinary
PGE2 levels were significantly lower among ibuprofen
group patients than the acetaminophen group (P<0.05; Table III). However, the descent range of
the plasma [avg.12.6 (5.7, 19.5) ng/l] PGE2 level in the
acetaminophen group [avg.12.6 (5.7, 19.5) ng/l] was significantly
lower than that of the ibuprofen group [avg.18.5 (10.1, 33.8)
ng/l], and the difference was statistically significant (Z=−2.158,
P=0.031), and the descent range of urinary PGE2 of the
acetaminophen group (45.0±36.9 ng/l) was lower than that of the
ibuprofen group (73.5±44.8 ng/l) and the difference was
statistically significant (t=3.244, P=0.002).
 | Table III.PGE2, platelet,
creatinine, and glutamic-pyruvic transaminase before and after
treatment (mean ± standard deviation). |
Table III.
PGE2, platelet,
creatinine, and glutamic-pyruvic transaminase before and after
treatment (mean ± standard deviation).
|
| Ibuprofen group
(n=43) | Acetaminophen group
(n=44) |
|---|
|
|
|
|
|---|
| Indicators | Before
treatment | After
treatment | t | P-value | Before
treatment | After
treatment | t | P-value |
P-valuea |
|---|
| Plasma
PGE2 (ng/l) | 70.0±35.7 | 47.3±24.7 | 7.091 | 0.000 | 74.2±35.5 | 59.9±32.9 | 7.298 | 0.000 | 0.046 |
| Urine
PGE2 (ng/l) | 189.0±62.4 | 115.4±46.3 | 10.765 | 0.000 | 184.4±73.8 | 139.3±54.0 | 8.100 | 0.000 | 0.030 |
| Platelet
(×109/l) | 192.4±94.6 | 224.4±88.0 | 1.807 | 0.078 | 183.8±107.7 | 195.0±84.3 | −0.506 | 0.615 | 0.115 |
| Serum creatinine
(µmol/l) | 69.0±33.6 | 74.1±35.7 | 0.747 | 0.459 | 67.0±33.2 | 60.9±30.9 | 0.874 | 0.387 | 0.068 |
| Glutamic-pyruvic
transaminase (U/l) | 15.4±7.4 | 16.8±4.9 | 1.309 | 0.198 | 15.9±11.2 | 17.4±6.6 | −0.815 | 0.419 | 0.635 |
The comparison on platelets, serum creatinine and
glutamic-pyruvic transaminase between the two groups of patients
before treatment (P>0.05) and after treatment (P>0.05)
revealed no significant difference (Table III).
Descent range of PGE2 in
PDA closed and PDA unclosed, oliguria and non-oliguria patients
after treatment
The descent range of plasma and urinary
PGE2 between PDA closed and PDA unclosed patients was
not significantly different (P>0.05; Table IV). However, the descent range of
plasma and urinary PGE2 in oliguria patients was higher
than non-oliguria patients (P<0.05; Table IV).
 | Table IV.Descent range of PGE2 in
PDA closed and PDA unclosed, oliguria and non-oliguria
patients. |
Table IV.
Descent range of PGE2 in
PDA closed and PDA unclosed, oliguria and non-oliguria
patients.
| Descent range of
PGE2 after treatment (ng/l) | PDA closed group
(n=64) | PDA unclosed group
(n=23) | Z/t | P-value | Oliguria group
(n=7) | Nonoliguric group
(n=80) | Z/t | P-value |
|---|
| Plasmaa | 13.7 (7.3,
25.6) | 15.7 (9.1,
25.3) | Z=0.067 | 0.946 | 35.0 (26.3,
49.8) | 13.3 (6.7,
20.8) | Z=−3.326 | 0.001 |
| Urineb | 61.1±44.7 | 53.7±39.2 | t=0.708 | 0.481 | 135.0±38.0 | 52.5±37.0 | t= 5.649 | 0.000 |
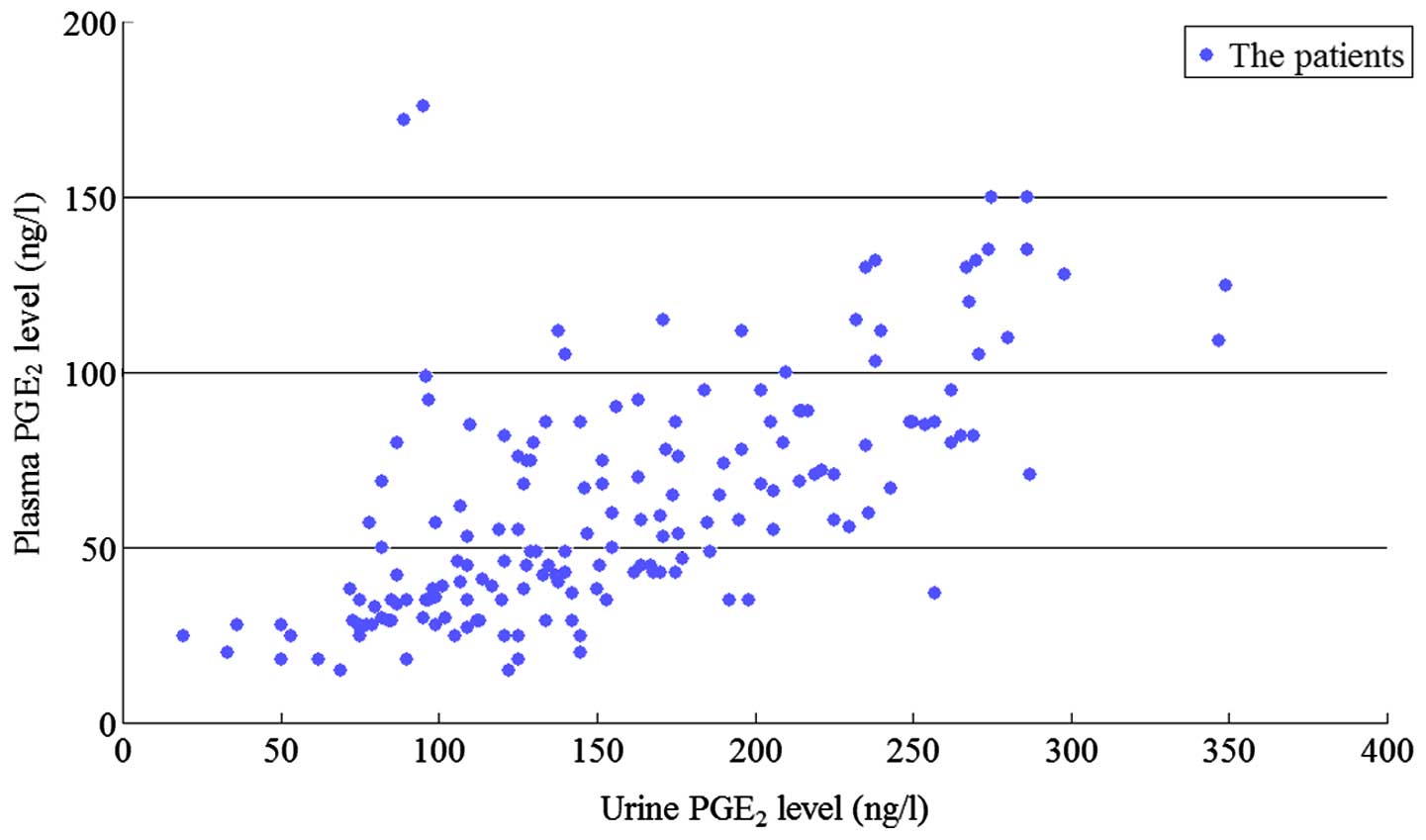
Plasma and urinary PGE2
levels are highly correlated
The plasma and urinary PGE2 levels were
highly correlated (Pearson correlation coefficient r=0.648, P=0.01)
as shown in Fig. 1 and the variable
coefficient of urinary PGE2 (67.1/157.1=0.427) level was
lower than the plasma PGE2 (33.9/62.9=0.539) level.
Incidence of adverse reactions among
sPDA infants of acetaminophen and ibuprofen groups
The various incidences of adverse reactions
including PDA occlusion, oliguria, and fecal occult blood observed
are shown in Table II. None of the
adverse reactions showed a significant association with
administration of either acetaminophen or ibuprofen (P>0.05).
Additionally, no significant changes were observed on the
transcutaneous oxygen saturation, pulse rate, blood pressure,
peripheral blood glucose, transcutaneous bilirubin, temperature,
feeding, and bleeding tendency during the treatment period. The
incidence of NEC that occurred several days later could not be
confirmed to be associated with the drugs.
Discussion
General
Inside the uterus, low arterial oxygen partial
pressure, prostaglandin and nitric oxide are the major factors that
maintain the opening of the arterial catheter, of which
PGE2 plays the key role (1,2).
Cyclooxygenase (COX) is a key rate-limiting enzyme synthesized by
prostaglandin, which has the active sites of COX and peroxidase.
COX can catalyze arachidonic acid to transform into prostaglandin
via its COX activity, and then catalyze the prostaglandin to
transform into active PGE series via the activity of peroxidase.
COX has two types of isozymes, COX-1 and COX-2. COX-3 has been
quite widely used in recent years after first discovered by
Chandrasekharan et al (8) in
their study on the mechanism of action of acetaminophen. COX-3 was
quite sensitive to the inhibiting effect of acetaminophen, thus
being deemed as the effector target of acetaminophen. Ibuprofen, as
the non-selective inhibitor of COX-1 and COX-2 could play the
inhibiting role by blocking or modifying the COX active sites.
However, the exact mechanism for the effect of acetaminophen on COX
activity remains controversial. At present, two theories are quite
prevalent: i) acetaminophen could selectively inhibit COX-3; and
ii) acetaminophen has no affiliation to the active sites of COX,
but it may restore the active oxydic COX into non-active COX and
then obstruct its biological activity (9).
Influence of ibuprofen and
acetaminophen treatment on PGE2 of premature infants
with sPDA
In the current study, ibuprofen and acetaminophen
treatment reduced the level of plasma and urinary PGE2.
From this it could be inferred that the two drugs may reduce the
PGE2 levels and promote the closure of sPDA. The present
study has also shown that, the descent range of plasma and urinary
PGE2 levels of the acetaminophen group was lower than
those of the ibuprofen group. This may be because COX3 was
selectively inhibited by acetaminophen activity of COX and
peroxidase, although the activity was only 20% of COX-1 (9). Shetty et al (10) showed that, ibuprofen reduced the
level of PGE2 in gingival crevicular fluid, but
acetaminophen had no significant effect on the level of
PGE2. No reports are available at present on the
influence of acetaminophen on PGE2 level in premature
infants with sPDA.
The action mechanisms of ibuprofen and acetaminophen
on COX activity are different, the descended ranges of plasma and
urinary PGE2 levels due to the drugs were different in
this study, but their curative effects on promoting sPDA closure
were similar and this curative effect was not related to the
descent range of PGE2 level. A possible explanation for
this may be that although the plasma prostaglandin level is an
important factor in inhibiting the contraction of arterial duct,
the closure of arterial catheter is affected by multiple factors
including the maturity of arterial catheter, family genetic
background and other unknown factors promoting and inhibiting the
arterial duct contraction (1).
Association of ibuprofen and
acetaminophen with adverse reactions and the descent range of
PGE2 levels
Antonucci et al (4) in an earlier study reported that,
ibuprofen treatment reduced the urinary PGE2 level and
caused acute renal failure in 3 of 20 hsPDA patients. Antonucci
et al (4) suggested that,
ibuprofen inhibited COX thereby lowering the PGE2 level
and this resulted in reduced peripheral blood vessel flow,
increased oliguria, acute renal failure and NEC. In our study, the
incidence of oliguria in acetaminophen group was significantly
lower than that of the ibuprofen group. This may be because of the
descending ranges of plasma and urinary PGE2 levels of
acetaminophen group being lower than the ibuprofen group.
Additionally, the descent ranges of plasma and urinary
PGE2 levels of the oliguria group were more than those
of the non-oliguria group. Our results substantiated the study of
Antonucci et al (4). Although
the descent range of plasma and urinary PGE2 between
oliguria and non-oliguria patients showed a significant difference
in the absolute values, the incidence of oliguria being very low
among patients of the ibuprofen and acetaminophen groups may be due
to the low sample size (sample size of this study was estimated on
the basis of major research indicator ‘changes of plasma and urine
PGE2 levels before and after treatment’).
Walker et al (11) showed that, indometacin induces NEC
and PEG2 and its receptor plays a key role in regulating the
intestinal blood flow. The more the reduction in the level of PEG2,
the less was the intestinal blood flow. Dang et al (12) reported that, the incidence of
gastrointestinal bleeding in patients administered with
acetaminophen was significantly lower than the patients
administered with ibuprofen. In our study, the incidence of
positive fecal occult blood in the acetaminophen group was
relatively lower than those observed in the ibuprofen group. We
suggest that, acetaminophen selectively inhibited COX-3 and its
inhibiting effect on COX-1 (associated with the synthesis of the
protective prostaglandin in stomach and duodenum) was lower than
that exerted by ibuprofen. Moreover, no COX-3 has been discovered
in the small intestinal epithelial cells of human beings (13).
Correlation of plasma and urinary
PGE2 levels
The findings of the present study showed that the
plasma and urinary PGE2 levels were highly correlated,
and the variable coefficient of urinary PGE2 level was
lower than that of plasma PGE2. Thus, for monitoring
PGE2 levels in sPDA infants, urine samples are optimal
in the clinical setting, because it can be collected in a
non-invasive manner.
Efficacy and safety of ibuprofen and
acetaminophen in clinical setting
In 2011, Hammerman et al (6) first reported that, oral administration
of 15 mg/kg acetaminophen caused closure of the arterial catheter
in 5 sPDA infants who were unresponsive to ibuprofen treatment
without any significant adverse reactions. Since then, the majority
of studies (14–19) have used oral or intravenous
administration of acetaminophen as a replacement therapy for the
closure of arterial catheter in sPDA patients who were unresponsive
by ibuprofen/indometacin treatments. Additionally, a low
concentration of peroxide activated the activity of peroxidase, but
a higher concentration of peroxide was needed to activate COX.
Therefore, in the hypoxic environment, such as arterial duct
endothelial cells, acetaminophen inhibits COX, rather than
ibuprofen, in a better manner (9).
This may be one of the reasons for the use of acetaminophen as a
replacement therapy for patients who failed in the ibuprofen
treatment. In the present study, we showed that, the effect of
acetaminophen in promoting the closure of sPDA in premature infants
was similar to that of ibuprofen, which was consistent with recent
studies (14,20). A RCTs study which included 80
premature infants with sPDA (gestational age, ≤30 weeks; birth
weight, ≤1,250 g) showed that, the arterial catheter closure rate
among ibuprofen-treated patients was similar to that of
acetaminophen-treated patients (21). Another non-inferiority RCTs study
which included 160 premature infants with sPDA (gestational age,
≤34 weeks) showed that, the arterial catheter closure rate in
acetaminophen-treated patients was not inferior to patients treated
with ibuprofen (81.2 vs. 78.8%) (12).
Previous findings have shown that the tolerance for
acetaminophen is good, and only few patients had their liver
enzymes elevated (14). In this
study, we showed that, oral administration of ibuprofen and
acetaminophen exerted no significant influence on the platelet,
serum creatinine, and glutamic-pyruvic transaminase and also there
was no occurrence of NEC. This indicates that, oral administration
of ibuprofen or acetaminophen at the dosage level described in this
study is safe during a short-term administration of the drug.
Limitations of this study
The present study did not include a placebo control
group and thus, we were not able to estimate the spontaneous
arterial catheter closure rate and physiological changes of plasma
and urinary PGE2 levels.
In conclusion, the clinical efficacy of oral
ibuprofen and acetaminophen in the treatment of preterm infants
with sPDA are relatively similar with low adverse events. Since a
high correlation exists between plasma and urinary PGE2,
the urinary PGE2 level can be used for predicting the
occurrence of drug associated adverse reactions including oliguria,
renal damage and gastrointestinal tract side effects in a
non-invasive manner in preterm infants with sPDA.
References
|
1
|
Clyman RI: Patent ductus arteriosus in the
preterm infantAvery's Diseases of the Newborn. Gleason CA and
Devaskar S: 9th. Saunders; Philadelphia, PA: pp. 751–761. 2012,
View Article : Google Scholar
|
|
2
|
Hamrick SE and Hansmann G: Patent ductus
arteriosus of the preterm infant. Pediatrics. 125:1020–1030. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pacifici GM: Clinical pharmacology of
indomethacin in preterm infants: implications in patent ductus
arteriosus closure. Paediatr Drugs. 15:363–376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Antonucci R, Cuzzolin L, Arceri A, Dessì A
and Fanos V: Changes in urinary PGE2 after ibuprofen
treatment in preterm infants with patent ductus arteriosus. Eur J
Clin Pharmacol. 65:223–230. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gao X, Hei M, Yang B, Zhu H, Zhang QG, Lei
HG and Ren Y: The changes of plasma prostaglandins E2 at
pre- and post-treatment in preterm infants with patent ductus
arteriosus. Chin J Heart Heart Rhythm. 3:102–108. 2015.
|
|
6
|
Hammerman C, Bin-Nun A, Markovitch E,
Schimmel MS, Kaplan M and Fink D: Ductal closure with paracetamol:
a surprising new approach to patent ductus arteriosus treatment.
Pediatrics. 128:e1618–e1621. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
El Hajjar M, Vaksmann G, Rakza T, Kongolo
G and Storme L: Severity of the ductal shunt: a comparison of
different markers. Arch Dis Child Fetal Neonatal Ed. 90:F419–F422.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chandrasekharan NV, Dai H, Roos KL,
Evanson NK, Tomsik J, Elton TS and Simmons DL: COX-3, a
cyclooxygenase-1 variant inhibited by acetaminophen and other
analgesic/antipyretic drugs: cloning, structure, and expression.
Proc Natl Acad Sci USA. 99:13926–13931. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Graham GG, Davies MJ, Day RO, Mohamudally
A and Scott KF: The modern pharmacology of paracetamol: therapeutic
actions, mechanism of action, metabolism, toxicity and recent
pharmacological findings. Inflammopharmacology. 21:201–232. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shetty N, Patil AK, Ganeshkar SV and Hegde
S: Comparison of the effects of ibuprofen and acetaminophen on
PGE2 levels in the GCF during orthodontic tooth
movement: a human study. Prog Orthod. 14:62013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Walker KS, Matheson PJ, Galganski LA,
Garrison RN and Downard CD: Application of prostaglandin E2
improves ileal blood flow in NEC. J Pediatr Surg. 49:945–949;
discussion 949. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dang D, Wang D, Zhang C, Zhou W, Zhou Q
and Wu H: Comparison of oral paracetamol versus ibuprofen in
premature infants with patent ductus arteriosus: a randomized
controlled trial. PLoS One. 8:e778882013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wu M and Wan J: COX-3: is it the target of
acetaminophen? Prog Physiol Sci. 41:40–42. 2010.
|
|
14
|
Le J, Gales MA and Gales BJ: Acetaminophen
for patent ductus arteriosus. Ann Pharmacother. 49:241–246. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Allegaert K, Anderson B, Simons S and van
Overmeire B: Paracetamol to induce ductus arteriosus closure: is it
valid? Arch Dis Child. 98:462–466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Oncel MY, Yurttutan S, Uras N, Altug N,
Ozdemir R, Ekmen S, Erdeve O and Dilmen U: An alternative drug
(paracetamol) in the management of patent ductus arteriosus in
ibuprofen-resistant or contraindicated preterm infants. Arch Dis
Child Fetal Neonatal Ed. 98:F942013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nadir E, Kassem E, Foldi S, Hochberg A and
Feldman M: Paracetamol treatment of patent ductus arteriosus in
preterm infants. J Perinatol. 34:748–749. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sinha R, Negi V and Dalal SS: An
interesting observation of PDA closure with oral paracetamol in
preterm neonates. J Clin Neonatol. 2:30–32. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ozdemir OM, Doğan M, Küçüktaşçı K, Ergin H
and Sahin O: Paracetamol therapy for patent ductus arteriosus in
premature infants: a chance before surgical ligation. Pediatr
Cardiol. 35:276–279. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Terrin G, Conte F, Scipione A, Bacchio E,
Conti MG, Ferro R, Ventriglia F and De Curtis M: Efficacy of
paracetamol for the treatment of patent ductus arteriosus in
preterm neonates. Ital J Pediatr. 40:212014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Oncel MY, Yurttutan S, Erdeve O, Uras N,
Altug N, Oguz SS, Canpolat FE and Dilmen U: Oral paracetamol versus
oral ibuprofen in the management of patent ductus arteriosus in
preterm infants: a randomized controlled trial. J Pediatr.
164:510–514, e.1. 2014. View Article : Google Scholar : PubMed/NCBI
|