Introduction
Synovitis, acne, palmoplantar pustulosis,
hyperostosis, and osteitis (SAPHO) syndrome was initially described
as a disease of aberrant bones, joints and skin lesions in 1987 by
Chamot et al (1). SAPHO
syndrome can occur at any age and is characterized by repeated
remission and recurrence, and it rarely occurs in individuals aged
>60 years (2). Although a wide
spectrum of clinical hallmarks have been previously described for
SAPHO syndrome, the osteoarticular and/or dermatological lesions
are the most important manifestations. Most patients present with
local inflammatory pain, swelling, and limited movement at the site
of the active lesions, particularly at the anterior chest wall
(ACW) (3). The prevalence of SAPHO
is <1/10000 (4). However, its
actual prevalence may be underestimated due to incorrect diagnosis.
High incidence rates of SAPHO syndrome have been reported in the
European population (5), whereas
only occasional cases are reported in Chinese individuals (6–8).
Osteitis and hyperostosis are striking features that can be
observed in any involved skeletal segments (9). It has been demonstrated that skin
manifestations are detected in 63.5% of patients (4), whereas at least 15% adults never
experience skin manifestations (10). Therefore, diagnosis of SAPHO syndrome
may be difficult in certain cases, particularly if the
dermatological manifestations are absent (10). The pathogenesis is poorly understood.
However, it has been shown that persistent infection with
low-virulence pathogens and the autoimmune process triggered by a
bacterial or viral pathogen may be associated with SAPHO syndrome
(10).
The present case study described the imaging
features of three cases of SAPHO with sternoclavicular joint
arthritis but without skin manifestations using multiple imaging
modalities, including computed tomography (CT), magnetic resonance
imaging (MRI) and bone scintigraphy. This study was approved by the
Institutional Review Board of the Affiliated Hospital of Nanjing
University of Chinese Medicine (Nanjing, China) with waiver of
informed consent.
Case reports
Case 1
A 52-year-old male patient was admitted to the
Affiliated Hospital of Nanjing University of Chinese Medicine due
to progressive pain at the ACW in March 2008. Over the past 2 years
he had recurrently suffered from sternoclavicular arthritis.
Initially, the symptoms included swelling, pain, and muscle
stiffness with no apparent causes. He was referred to another
hospital, but no diagnosis was made and no treatment was
administered. As the swelling did not recover and became more
severe, the patient consulted our institution for further
evaluation.
Physical examination indicated swelling and
tenderness at the sternoclavicular joint and his body temperature
was 37.5°C. Erythrocyte sedimentation rate (ESR) was 37 mm/h
(reference range in males, 0–15 mm/h) and C-reactive protein level
was 0.83 mg/dl (reference range, <1.0 mg/dl), which indicated
that there was slight inflammatory reaction. Other laboratory data,
such as rheumatoid factor and anti-nuclear antibody tests, were
negative.
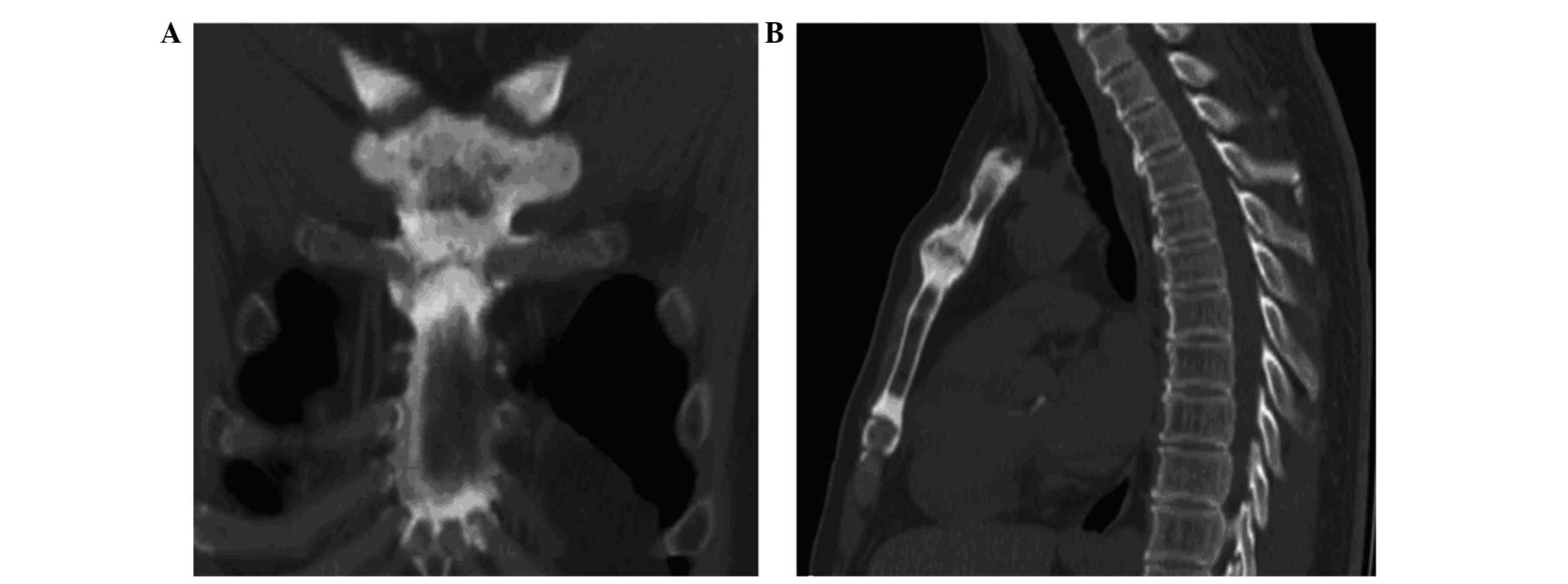
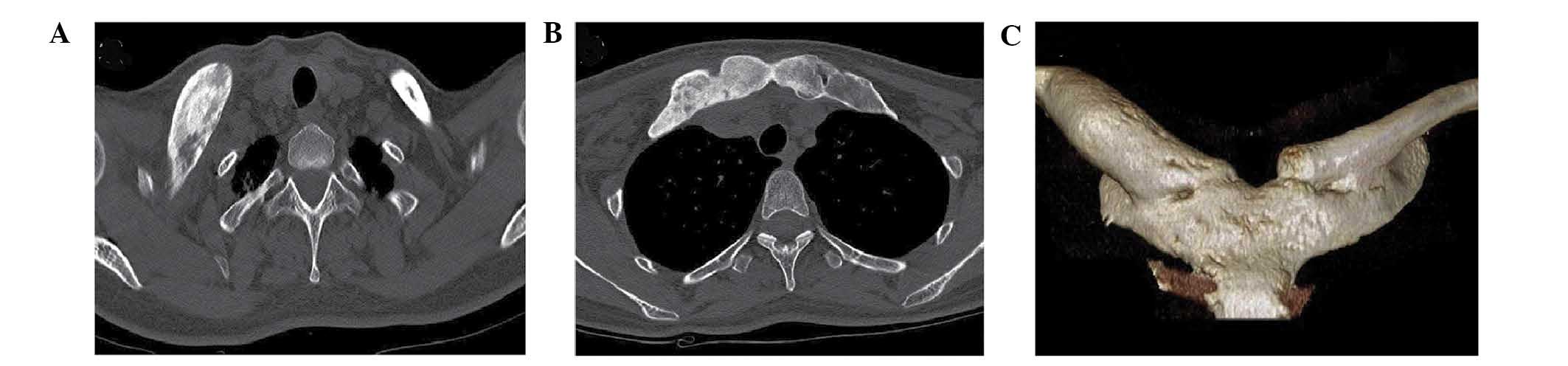
CT scanning demonstrated sclerosis and hyperostosis
with subchondral erosions in the sternocostoclavicular joints, the
medial end of clavicle, sternum, first rib and costal cartilage
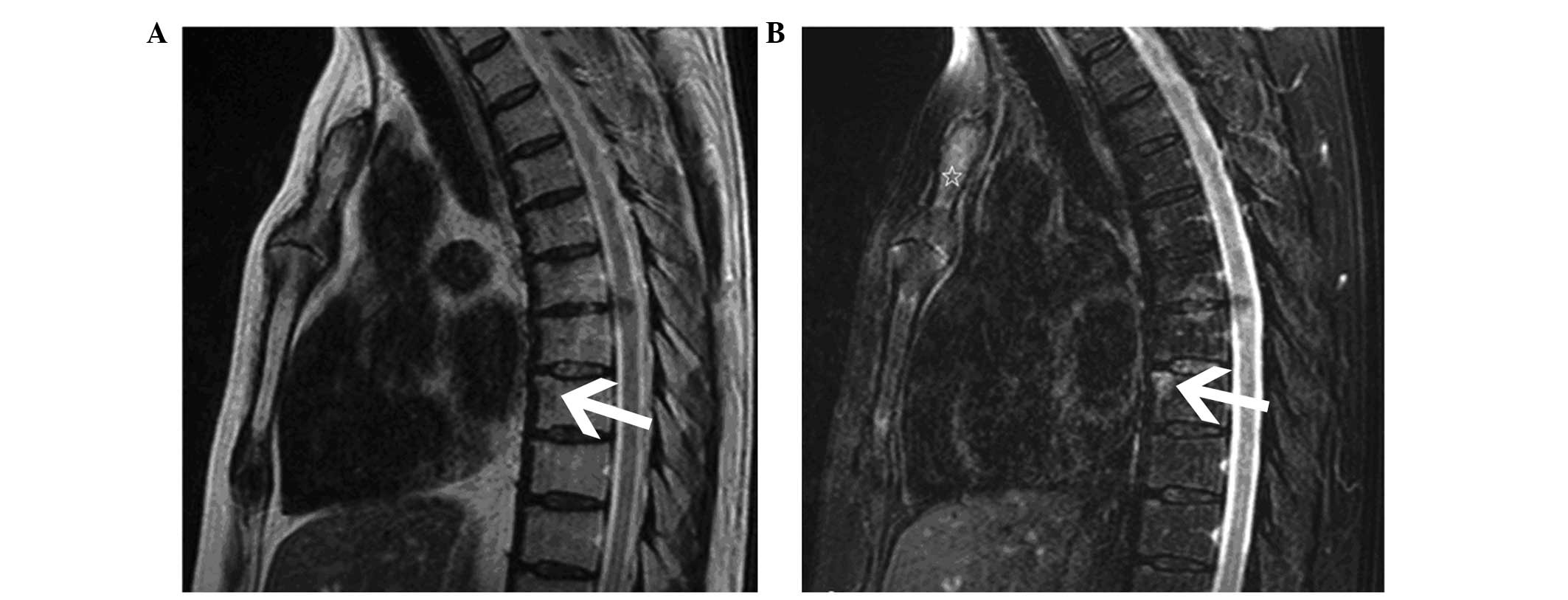
(Fig. 1). MRI indicated bone marrow
oedema in the manubrium and the eighth thoracic vertebral corner on
T1- (Fig. 2A) and T2-weighted
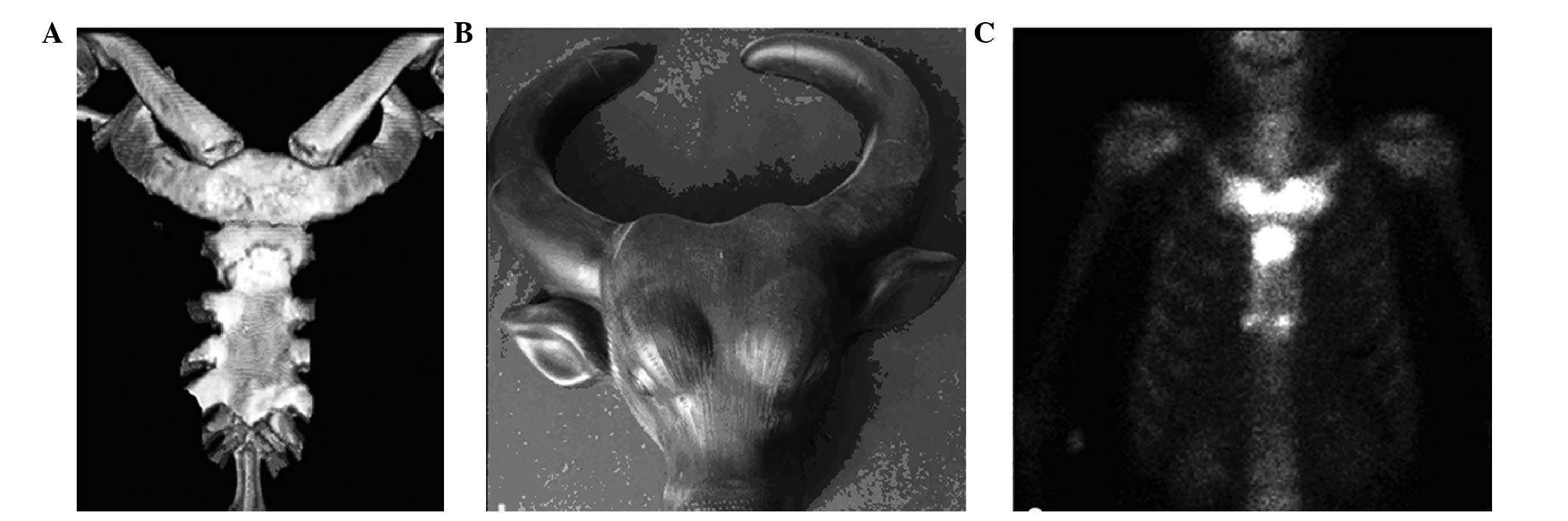
(Fig. 2B) imaging. Bone scintigraphy
with 99mTc-methylene diphosphonate showed an
accumulation of tracer in the sternoclavicular and manubriosternal
joints. The typical ‘bulls head’ sign was observed, and was also
detected by helical CT imaging with a volume rendering technique
(Fig. 3). Treatment with ibuprofen
[100 mg orally, twice daily (bid); Taicheng Pharmaceutical Co.,
Ltd., Guangdong, China] and prednisone (30 mg orally, once daily;
Xinyi Pharmaceutical Co., Ltd., Shanghai, China) was initiated. The
patient reached full remission at the end of a 3-month
follow-up.
Case 2
A 62-year-old female was admitted to the Affiliated
Hospital of Nanjing University of Chinese Medicine with pain in the
right thoracic area with no apparent cause in May 2009. She had
suffered from pain for 5 years with repeated remission and relapse.
Subsequent to her admission, hypesthesia and muscle weakness of
upper chest wall on the right side appeared and gradually
deteriorated. Pain persisted and was not associated with any
noticeable early morning stiffness. The patient did not have a
history of skin lesions. Physiotherapy could not relieve her pain;
therefore, she underwent therapy for rheumatoid arthritis, but no
obvious amelioration was detected. Physical examination indicated
that she had no remarkable neuronal responses and tenderness was
detected on both knees, her right shoulder, and right
sternoclavicular joint with conspicuous swelling.
ESR was 21 mm/h (reference range in females, 0–20
mm/h) and C-reactive protein level was 7.22 mg/dl (reference range,
<1.0 mg/dl), which indicated the presence of a slight
inflammatory reaction. Results of routine blood testing were
normal. Tumor marker [carcinoembryonic antigen (CEA), CA125 and
alkaline phosphatase (ALP)] and tuberculin tests were negative.
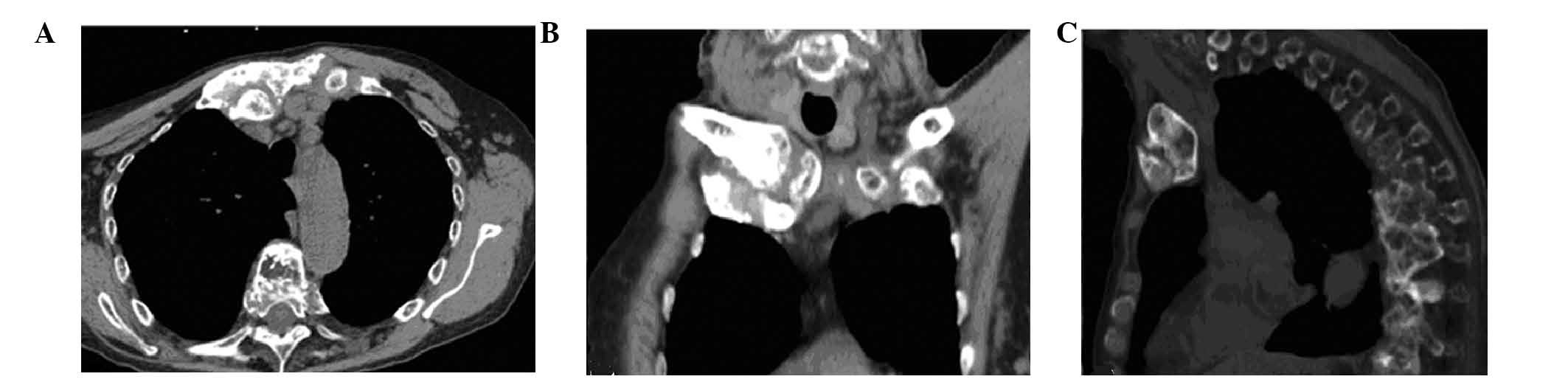
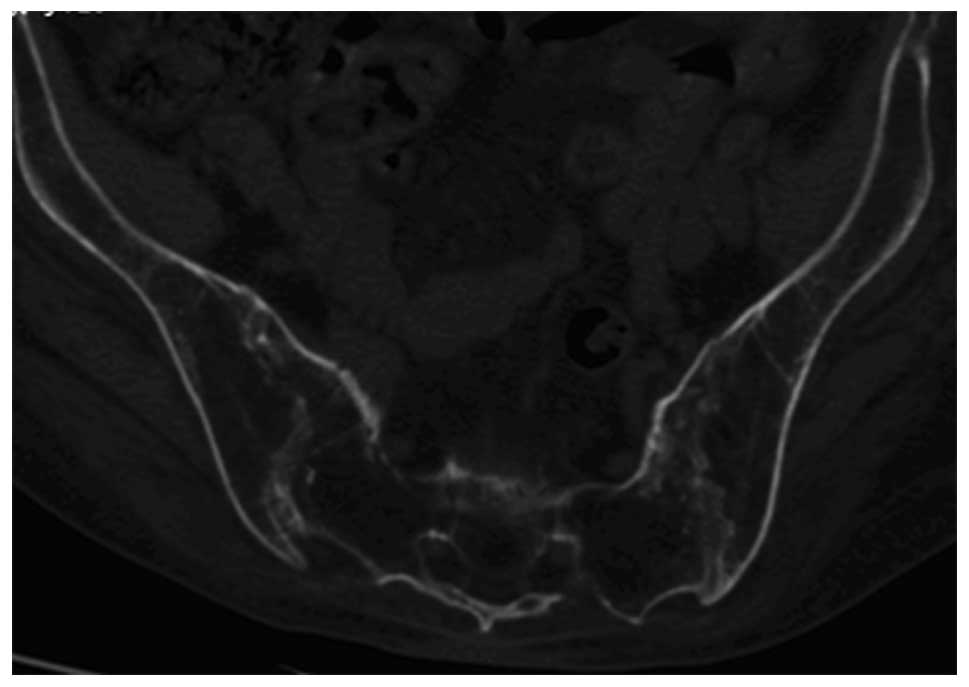
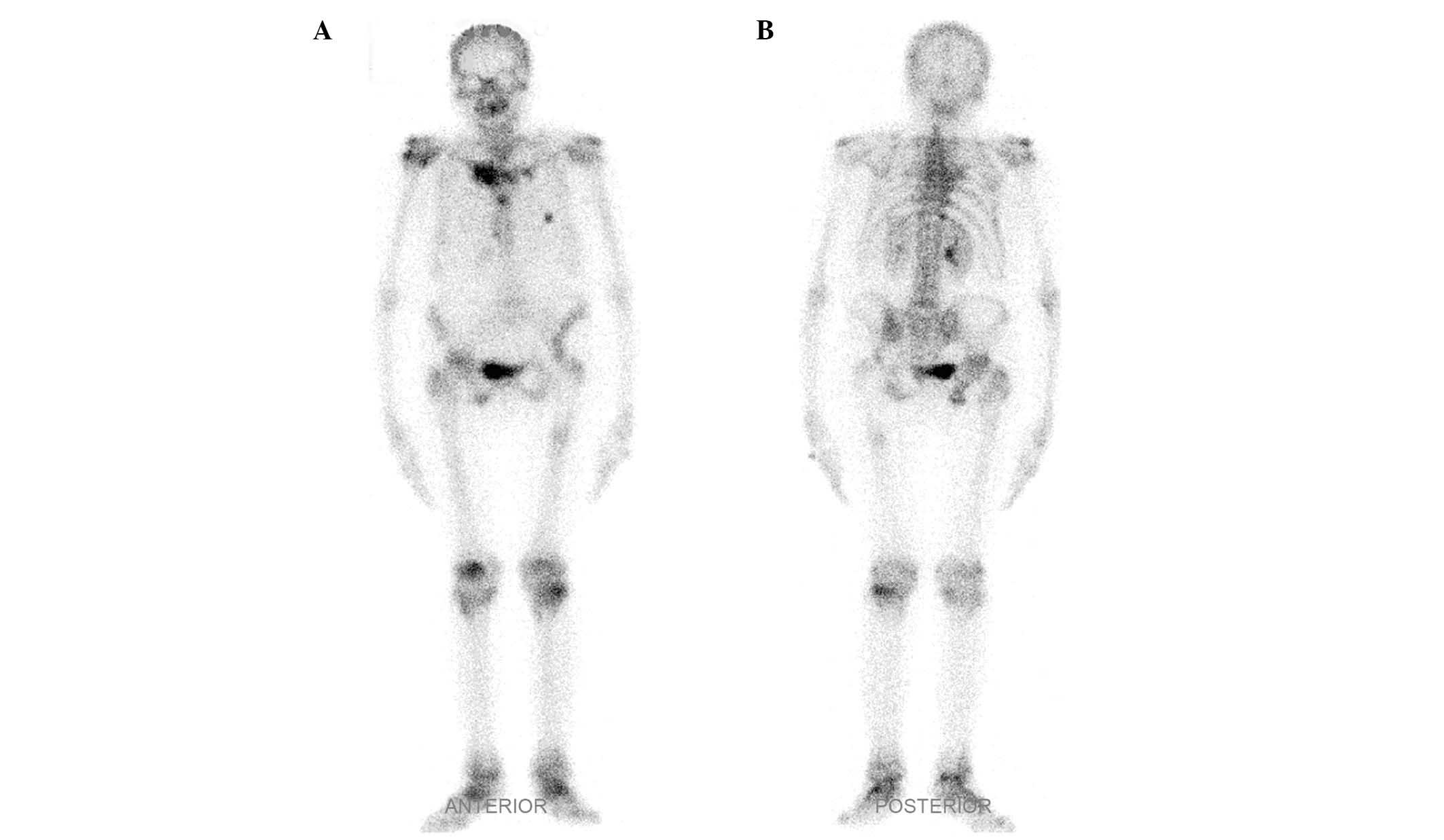
CT imaging revealed hyperostosis at the right
sternocostoclavicular joints and severe destruction with marginal
sclerosis at multiple thoracic vertebras (Fig. 4). Joint space narrowing and erosive
damage at the bilateral sacroiliac joints (Fig. 5) was also observed. Whole-body bone
scintigraphy with 99mTc-methylene diphosphonate
indicated increased tracer uptake in the sternoclavicular joint,
upper thoracic vertebra, shoulders, and the knee and ankle joints
(Fig. 6). Treatment with ibuprofen
(100 bid, orally) and sulfasalazine (500 mg orally, four times
daily; Xinyi Pharmaceutical Co., Ltd.).was initiated. The patient
reached partial remission at the end of a 3-month follow-up.
Case 3
A 44-year-old male patient was admitted to the
Affiliated Hospital of Nanjing University of Chinese Medicine
complaining of a slight bulge accompanied by pain at the upper ACW
in May 2014. Inadequate attention was paid to the lesion as the
patient had no any other systemic complaints with the exception of
an indolent mass at his left sternocostoclavicular joints for the
past 4 years. The mass had gradually increased in size over the
previous year.
Physical examination showed the there was tenderness
and swelling at the left ACW. ESR and C-reactive protein level were
within the normal ranges. Human leukocyte antigen (HLA) B27 antigen
was positive. Tumor marker (CEA, CA125, prostate-specific antigen
and ALP) and tuberculin test results were normal.
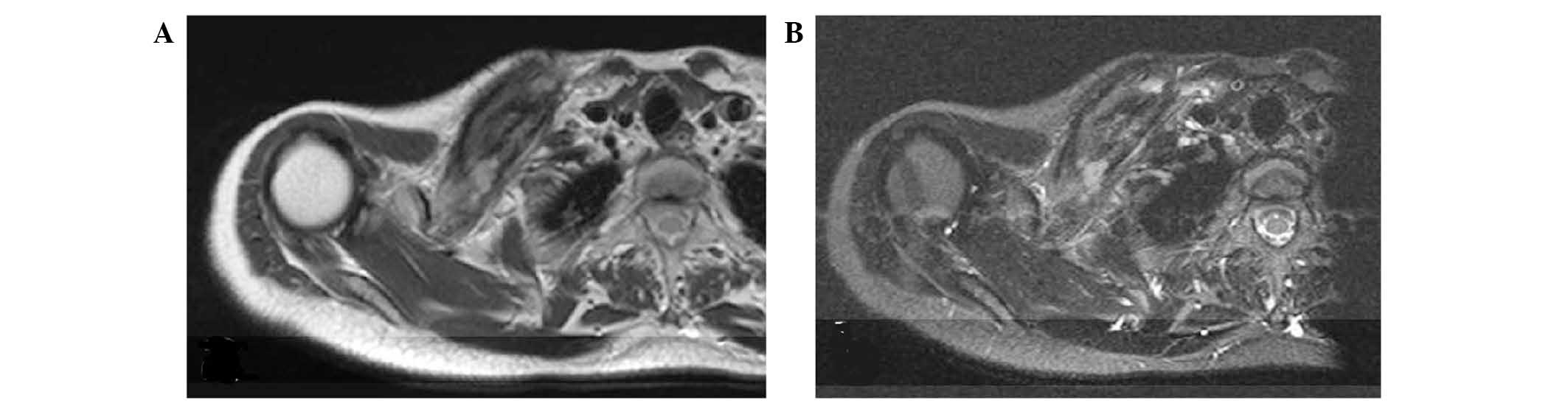
CT scanning revealed subarticular erosions and
regional sclerosis at the sternoclavicular joint (Fig. 7). Bone marrow edema at the right
collarbone was detected by MRI axial T2-weighted imaging and
T2-weighted imaging with fat saturation (Fig. 8). Although no skin lesions developed
during the clinical course, the diagnosis of SAPHO syndrome was
made based on the presence of osteoarthritis at the
sternoclavicular joint. Ibuprofen (200 mg orally, twice daily;
Xiuzheng Pharmaceutical Co., Ltd., Jilin, China) and methotrexate
(7.5 mg orally, once weekly; Xinyi Pharmaceutical Co., Ltd.) were
administered. The patient reached partial remission at the end of a
2-month follow-up.
Discussion
SAPHO syndrome is a well-documented rare chronic
disorder, which is characterized by abnormal osteoarticular
manifestations and a range of chronic dermatosis (11). The majority of published papers in
this field are case reports or small series case studies. The
natural history and long-term evolution of the disease have not
been investigated extensively. Among patients with SAPHO syndrome,
65–90% presented with damage to the anterior chest (9). Involvement of multiple ACW sites such
as the sternoclavicular, manubriosternal, costochondral, and
costosternal junctions should be considered as an important
criterion for diagnosis (10).
Diagnosis of SAPHO syndrome is based on the presence
of at least one of four diagnostic criteria (12): i) Osteoarticular manifestations with
severe acne; ii) osteoarticular manifestations with palmoplantar
pustulosis; iii) hyperostosis involving either the ACW, spine, or
limbs, with or without dermatosis; and iv) recurrent multifocal
chronic osteomyelitis involving the axial or peripheral skeleton,
with or without dermatosis. Skin symptoms. including palmoplantar
pustulosis or/and severe acne, can be helpful for diagnosing SAPHO
syndrome. In addition, other dermatoses associated with SAPHO
include pustular psoriasis, hidradenitis suppurativa, and psoriasis
vulgaris (13). Some researchers
have reported that skin lesions were not observed in 16% of
patients, and the osteoarticular manifestation antedates the skin
manifestation in 32% of patients (2,14,15).
Skeletal symptoms and skin disease do not always occur in parallel
(8), which has an influence on the
diagnosis. These findings indicate that skin lesions are not a
necessary criteria for SAPHO diagnosis if patients exhibit
hyperostosis or multifocal chronic osteomyelitis. Osteoarticular
manifestations include hyperostosis, osteitis, synovitis and
arthropathy. Osteitis and hyperostosis are striking features that
can be observed in any involved skeletal segments (9). The main affected site is the ACW, but
other bones may also be involved (9). Osteitis or hyperostosis was observed in
the three cases described in the present case report. Therefore,
the three cases in the present report were diagnosed with SAPHO
syndrome with specific osteoarthritic manifestation at certain
sites in the absence of lesions.
The cause and pathogenesis of SAPHO syndrome remains
poorly understood (15). As such,
SAPHO syndrome can be misdiagnosed as a tumor or infectious disease
(16). Misdiagnosed benign tumors
include chronic infectious osteomyelitis, Paget's disease,
spondylarthropathies and osteitis condensans of the clavicle.
Malignant entities that should be considered are multiple myeloma,
extramedullary plasmacytoma, osteosarcoma and bone metastasis. When
radiological findings are confused with these entities, a history
of skin lesions, results of other laboratory tests and examination
with multiple imaging modalities may be helpful for differential
diagnosis. Radiologists should recommend bone scintigraphy or
positron emission tomography-CT to reveal asymptomatic
manifestations. Standard uptake values can be used to differentiate
SAPHO syndrome from malignancies, infections processes and
metastatic diseases (17,18).
There is no specific biomarker for SAPHO syndrome.
ESR and C-reaction protein levels can be moderately elevated, and
it has been shown that HLA-B27 is present in 15–33% (1) or 4–14% (9) of patients. In the present study,
elevation of ESR and C-reaction were detected in two cases (cases 1
and 2) and HLA-B27 was present in one case (case 3).
SAPHO syndrome remains difficult to diagnose. Before
a correct diagnosis is made, patients are often subjected to
multiple imaging examinations and unsuccessful therapy.
Radiologists have a key role in the early diagnosis for SAPHO
syndrome (19,20). Radiographs, bone scintigraphy, CT and
MRI are invaluable diagnostic tools. As a more sensitive imaging
modality, CT has the ability to detect abnormalities in the
sternoclavicular area that are not obvious on radiographs. Bone and
soft-tissue edemas are well recognized on MRI, particularly on
short-tau inversion recovery sequences, which can be useful in
differentiating between active and inactive lesions (21). MRI is radiation-free and is well
suited for patients who require repeated follow-up examinations.
Whole-body bone scintigraphy is a useful investigation technique in
the detection of relatively inactive and subclinical lesions
(22). Predominant high tracer
uptake in the sternoclavicular region appears to mimic a ‘bull
head’, with the manubrium representing the upper skull of the bull
and the horns corresponding to the inflamed sternoclavicular joints
and the adjacent claviculae (23,24). In
the present study, sclerosis or hyperostosis with subchondral
erosions in the sternocostoclavicular joints or manubrium were
observed on CT images. MRI images also showed bone marrow oedema in
case 2. Whole-body bone scintigraphy indicated multiple lesions,
including lesions in the sternoclavicular joint, upper thoracic
vertebra, the shoulders, the knee and ankle joints, and the typical
‘bull's head’ sign in case 2. These findings suggest that multiple
modalities imaging in combination may be helpful for the diagnosis
of SAPHO syndrome.
ACW and sternocostoclavicular joints were the main
regions affected in the present cases. It has been shown that the
lesions of SAPHO syndrome may be age dependent (25). In children, SAPHO syndrome often
affects long bones, followed by the clavicle and spine (15). In adults, sternocostoclavicular
joints and ACW are predominately affected, followed by spine
(19). Sweeney et al
(13) indicated that ribs may also
be involved. Laredo et al (18) showed that vertebral corner erosion
was a consistent MR imaging finding of SAPHO. Involvement of spine
and ribs were also found in our cases (spine, cases 1 and 2; ribs,
cases 2 and 3). Additional regions were affected in case 2, as
detected by whole-body bone scintigraphy, which suggested that
whole-body bone scintigraphy may have a relevant role in the
detection of lesion localizations.
In conclusion, SAPHO syndrome is characterized by
progressive hyperostosis and the eventual destruction of
sternoclavicular joints. Multiple bones may also be involved,
including the spine and ribs. Diagnosis remains challenging in the
absence of skin lesions and multiple imaging modalities may aid the
early and correct diagnosis of SAPHO syndrome.
References
|
1
|
Chamot AM, Benhamou CL, Kahn MF, Beraneck
L, Kaplan G and Prost A: Acne-pustulosishyperostosis-osteitis
syndrome: Results of a national survey. 85 cases. Rev Rhum Mal
Osteoartic. 54:187–196. 1987.(In French).
|
|
2
|
Carneiro S and Sampaio-Barros PD: SAPHO
syndrome. Rheum Dis Clin North Am. 39:401–418. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Judex AG, Freyschmidt J, Feuerbach S,
Schölmerich J and Müller-Ladner U: Sequential combination therapy
leading to sustained remission in a patient with SAPHO syndrome.
Open Rheumatol J. 3:18–21. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Govoni M, Colina M, Massara A and Trotta
F: SAPHO syndrome and infections. Autoimmun Rev. 8:256–259. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sallés M, Olivé A, Perez-Andres R, Holgado
S, Mateo L, Riera E and Tena X: The SAPHO syndrome: A clinical and
imaging study. Clin Rheumatol. 30:245–249. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang LL, Zhao JX and Liu XY: Successful
treatment of SAPHO syndrome with severe spinal disorder using
entercept: A case study. Rheumatol Int. 32:1963–1965. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhao Z, Li Y, Li Y, Zhao H and Li H:
Synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO)
syndrome with review of the relevant published work. J Dermatol.
38:155–159. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Song X, Sun W, Meng Z, Gong L, Tan J, Jia
Q, Yu C and Yu T: Diagnosis and treatment of SAPHO syndrome: A case
report. Exp Ther Med. 8:419–422. 2014.PubMed/NCBI
|
|
9
|
Colina M, Govoni M, Orzincolo C and Trotta
F: Clinical and radiologic evolution of synovitis, acne,
pustulosis, hyperostosis, and osteitis syndrome: A single center
study of a cohort of 71 subjects. Arthritis Rheum. 61:813–821.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nguyen MT, Borchers A, Selmi C, Naguwa SM,
Cheema G and Gershwin ME: The SAPHO syndrome. Semin Arthritis
Rheum. 42:254–265. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Takigawa T, Tanaka M, Nakahara S, Sugimoto
Y and Ozaki T: SAPHO syndrome with rapidly progressing destructive
spondylitis: Two cases treated surgically. Eur Spine J. 17 Suppl
2:331–337. 2008. View Article : Google Scholar
|
|
12
|
Benhamou CL, Chamot AM and Kahn MF:
Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome
(SAPHO) A new syndrome among the spondyloarthropathies? Clin Exp
Rheumatol. 6:109–112. 1988.PubMed/NCBI
|
|
13
|
Sweeney SA, Kumar VA, Tayar J, Weber DM,
Safdar A, Alonso C and Hymes S: Case 181: Synovitis acne pustulosis
hyperostosis osteitis (SAPHO) syndrome. Radiology. 263:613–617.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Depasquale R, Kumar N, Lalam RK, Tins BJ,
Tyrrell PN, Singh J and Cassar-Pullicino VN: SAPHO: What
radiologists should know. Clin Radiol. 67:195–206. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Earwaker JW and Cotten A: SAPHO: Syndrome
or concept? Imaging findings. Skeletal Radiol. 32:311–327. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Freyschmidt J and Sternberg A: The
bullhead sign: Scintigraphic pattern of sternocostoclavicular
hyperostosis and pustulotic arthroosteitis. Eur Radiol. 8:807–812.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fritz P, Baldauf G, Wilke HJ and Reitter
I: Sternocostoclavicular hyperostosis: Its progression and
radiological features. A study of 12 cases. Ann Rheum Dis.
51:658–664. 1992. View Article : Google Scholar
|
|
18
|
Laredo JD, Vuillemin-Bodaghi V, Boutry N,
Cotten A and Parlier-Cuau C: SAPHO syndrome: MR appearance of
vertebral involvement. Radiology. 242:825–831. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van Doornum S, Barraclough D, McColl G and
Wicks I: SAPHO: Rare or just not recognized? Semin Arthritis Rheum.
30:70–77. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pahlavan PS and Leslie WD: Multiple
imaging findings in SAPHO syndrome. Clin Nucl Med. 33:912–915.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Patel CN, Smith JT, Rankine JJ and
Scarsbrook AF: F-18 FDG PET/CT can help differentiate SAPHO
syndrome from suspected metastatic bone disease. Clin Nucl Med.
34:254–257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Boutin RD and Resnick D: The SAPHO
syndrome: An evolving concept for unifying several idiopathic
disorders of bone and skin. AJR Am J Roentgenol. 170:585–591. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zemann W, Pau M, Feichtinger M,
Ferra-Matschy B and Kaercher H: SAPHO syndrome with affection of
the mandible: Diagnosis, treatment, and review of literature. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod. 111:190–195. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shikino K, Ikusaka M and Hirota Y:
Magnetic resonance imaging of sternoclavicular joint arthritis due
to SAPHO syndrome. Int J Case Rep Images. 5:462–464. 2014.
View Article : Google Scholar
|
|
25
|
Rodríguez M Quirico, Casáns Tormo I, Redal
Peña MC and López Castillo V: The importance of bone scintigraphy
in the diagnosis of SAPHO syndrome. Rev Esp Med Nucl. 29:127–130.
2010.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|