Introduction
Severe acute pancreatitis (SAP) is an acute
inflammatory process with variable involvement of local tissues and
remote organs (1). The
overexpression of inflammatory cytokines, such as interleukin
(IL)-1, IL-6, IL-8 and tumor necrosis factor (TNF)-α, can seriously
damage the microcirculatory system's endothelium and subsequently
increase capillary permeability (2,3).
Additionally, the persistent inflammatory state aggravates the
existing hypoxia condition and systemic inflammatory response
syndrome (SIRS), which eventually result in an increase in the
mortality rate associated with SAP (4,5).
In addition to the cytokine cascade, the activation
of the adaptive immune system, including
CD4+CD8+ T lymphocytes is crucial in the
development of SIRS and organ failure in SAP patients (6,7). Results
obtained from prior studies reported a significant reduction in
peripheral blood T-cell subgroups in the early phase of AP, which
may correspond with patients' clinical outcome and disease severity
(8,9). In a previous study, we reported that
the reduction in CD4+ T lymphocytes in peripheral blood
was linked to organ failure and may act as a potential predictor of
severity in AP patients (10).
Effective fluid resuscitation and immune regulation therapy is
significant for the prognosis of SAP in the early phase.
Among patients with AP, early fluid resuscitation is
often associated with a reduced incidence of SIRS and organ failure
(11,12). Currently, two types of fluids are
frequently used for active resuscitation: Crystalloid and colloid
fluids with large molecules that maintain the fluid
intravascularly. Hydroxyethyl starch (HES) is a widely used colloid
fluid in volume expansion and is a priming fluid in the early stage
of AP (13,14). Previous findings have shown that HES
resuscitation in the early stages of SAP can decrease the acute
physiology and chronic health evaluation II (APACHE II) score,
reduce the need for mechanical ventilation, reduce the risk of
intra-abdominal hypertension, and shorten the duration of positive
fluid balance (FB) (15,16). However, recent studies indicated that
HES may not provide a clinical benefit and may even cause a higher
mortality rate as well as higher acute kidney injury rate in
critically ill patients (17–20).
This controversy aroused concerns regarding the safety of using HES
resuscitation during the early phase of SAP. By contrast, other
studies have shown that HES 130/0.4 can reduce the pro-inflammatory
responses and regulate the CD4+CD8+ T
lymphocyte subgroup ratio in cardiac surgery (21,22).
However, whether HES 130/0.4 is effective for the reduction of
pro-inflammatory cytokines and safe for renal function was the
focus of the present study.
Materials and methods
Data source
All relevant clinical data were extracted from the
database of a multi-center, randomized controlled trial (RCT)
study, which was designed to observe the effects of early
goal-directed fluid therapy with HES 130/0.4 on intra-abdominal
hypertension (IAH), multiple organ dysfunction and FB in SAP
patients. This RCT study was conducted from October, 2007 to
November, 2008 and a total of 120 SAP patients from four sites were
enrolled in the present study. There were no significant
differences between the groups regarding demographic data
(P>0.05) (Table I).
 | Table I.Demographic information and baseline
clinical characteristics in the 2 groups. |
Table I.
Demographic information and baseline
clinical characteristics in the 2 groups.
|
| HES group | Control group | P-value |
|---|
| No. (n) | 59 | 61 | – |
| Age (years) | 47.98±12.48 | 46.43±11.54 | 0.479 |
| Gender [n,
(%)] |
|
| 0.741 |
|
Male | 36 (61.00%) | 39 (63.90%) |
|
Female | 23 (39.00%) | 22 (36.10%) |
| Height (cm) | 165.85±7.73 | 167.05±7.00 | 0.374 |
| CT grade [n,
(%)] |
|
| 0.991 |
| 3 | 35 (59.30%) | 35 (58.30%) |
| 4 | 5 (8.50%) | 5 (8.30%) |
| 5 | 19 (32.20%) | 20 (33.30%) |
| APACHE II
score | 13.03±5.18 | 12.87±5.41 | 0.865 |
| IAP (mmHg) | 9.26±2.15 | 9.68±2.70 | 0.433 |
| CVP
(cmH2O) | 10.44±3.28 | 9.92±3.23 | 0.379 |
| WBC
(×109/l) | 14.51±4.43 | 14.13±4.67 | 0.646 |
| ALT (U/l) | 61.49±90.44 | 56.92±82.57 | 0.773 |
| AST (U/l) | 69.43±118.66 | 49.70±63.61 | 0.257 |
| BUN (mmol/l) | 5.59±3.64 | 6.43±3.52 | 0.201 |
| Cr (µmol/l) | 89.68±53.50 | 88.31±61.41 | 0.897 |
| Ca2+
(mmol/l) | 1.91±0.28 | 1.86±0.29 | 0.377 |
| CRP (µg/ml) | 197.56±108.96 | 190.57±92.24 | 0.718 |
| Serum amylase
(U/l) | 789.69±661.13 | 696.23±594.54 | 0.417 |
| Peritoneal drainage
[n, (%)] |
|
| 0.864 |
|
Yes | 9 (15.3%) | 10 (16.4%) |
|
Not | 50 (84.7%) | 51 (84.6%) |
| IL-1 (pg/ml) | 21.34±11.90 | 25.14±16.78 | 0.160 |
| IL-6 (pg/ml) | 51.89±44.55 | 57.85±68.09 | 0.576 |
| IL-8 (pg/ml) | 32.04±34.02 | 32.87±33.12 | 0.894 |
| TNF-α (pg/ml) | 45.52±29.78 | 40.27±16.12 | 0.234 |
| CD4+ T
cell (%) | 31.53±12.09 | 32.56±9.08 | 0.742 |
| CD8+ T
cell (%) | 21.00±8.01 | 19.82±6.74 | 0.590 |
Patients
Participants were adult patients (aged 18–65 years)
admitted within 3 days of disease onset. The diagnostic and
classification criteria included two of the following features: i)
Abdominal pain consistent with AP; ii) amylase activity at least
3-fold greater than the upper limit of normal; and iii)
characteristic findings of AP on contrast-enhanced computed
tomography CT) and, less commonly, on magnetic resonance imaging or
transabdominal ultrasonography. Patients with confirmed SAP were
considered eligible. The patients had at least one of the following
criteria: i) Failure in at least one organ as defined by the
Atlanta classification; ii) an APACHE II score ≥8; and iii) a
Balthazar's CT grade classification score ≥7 (23). Patients with the following conditions
were excluded: i) History of allergy to HES 130/0.4; ii) serious
cardiac or renal failure; iii) serum albumin value <25 g/l; iv)
blood coagulation dysfunction with international normalized ratio
>3; v) history of other colloid intravascular volume-replacement
regimens within 3 months prior to their enrollment in this study;
vi) pregnant or lactating female patients; and vii) MOF needing
continuous renal replacement treatment after admission.
Treatments
All the patients received specialized medical
therapy for AP according to the United Kingdom, Chinese Medical
Association, and International Association of Pancreatology
guidelines (24–26). After admission, patients were
randomly divided into 2 groups. One group received crystalloid (the
control group) and the other group received crystalloid plus HES
130/0.4 resuscitation (the HES group). Patients in the two groups
were infused with lactated Ringer's solution at a basic rate of 1–2
ml/kg/h. The control group received only Ringer's lactate and
saline solution for resuscitation. In the treatment group, 6% HES
130/0.4 (Voluven; Fresenius Kabi, Bad Homburg, Germany) was infused
at a volume ratio of 1:3 compared with saline solution. The volume
of HES was maintained at <50 ml/kg. The total rate and volume of
intravenous fluid was controlled to maintain hemodynamic stability.
A stable hemodynamic status was defined as a central venous
pressure (CVP) of 8–15 mmHg (1 mmHg=0.133 kPa), a urine output
>0.5 ml/kg/h, a mean blood pressure >65 mmHg, a heart ratio
of 80–100/min, a hematocrit >0.3 or a SpO2 of CVP
>0.7. Medication was planned to be administered for 7 days.
After a negative FB emerged, the HES was disabled according to the
patient's condition.
The study was approved by the Medical Ethics
Committee of Union Hospital (Wuhan, China). The need for informed
consent was waived by the Medical Ethics Committee because the
study was a retrospective study using a database from which
patients' identification information had been removed.
Measurement of parameters and
detection methods
Factors included in this study were: Age, gender,
height, CT grade, APACHE II scores, white blood cell counts, serum
ALT, AST, BUN, Cr, Ca2+, CRP and amylase. The
intra-abdominal pressure (IAP) and CVP was measured at 10:00 a.m.,
12:00 and 2:00 p.m. on the 1st day after admission according to the
standard techniques established by the World Society of Abdominal
Compartment Syndrome in 2006 (27).
The mean IAP value was calculated and the CVP measurement protocols
were defined as previously described (28).
Blood samples were obtained on days 1, 2, 4 and 8
after hospitalization and serum pro-inflammatory mediators
including IL-1, IL-6, IL-8 and TNF-α levels were measured using
enzyme-linked immunosorbent assays (R&D Systems, Inc.,
Minneapolis, MN, USA) according to the manufacturer's instructions.
Additionally, patients' blood samples on days 1, 4 and 8 were used
to detect the rate of CD4+CD8+ T lymphocytes.
The measurement protocols were described in a previous study
(10).
Statistical analysis
Empower (R) (www.empowerstats.com; X&Y Solutions, Inc., Boston,
MA, USA) and R (http://www.R-project.org) software were used for the
statistical analysis. Missing data were described as ‘NA’ as per
Empower (R) requirements. Data were presented as mean ± SD or
proportions. Comparisons between groups were performed using the
Chi-square test for categorical variables and two-sample t-test for
continuous variables. P<0.05 was considered to indicate a
statistically significant difference.
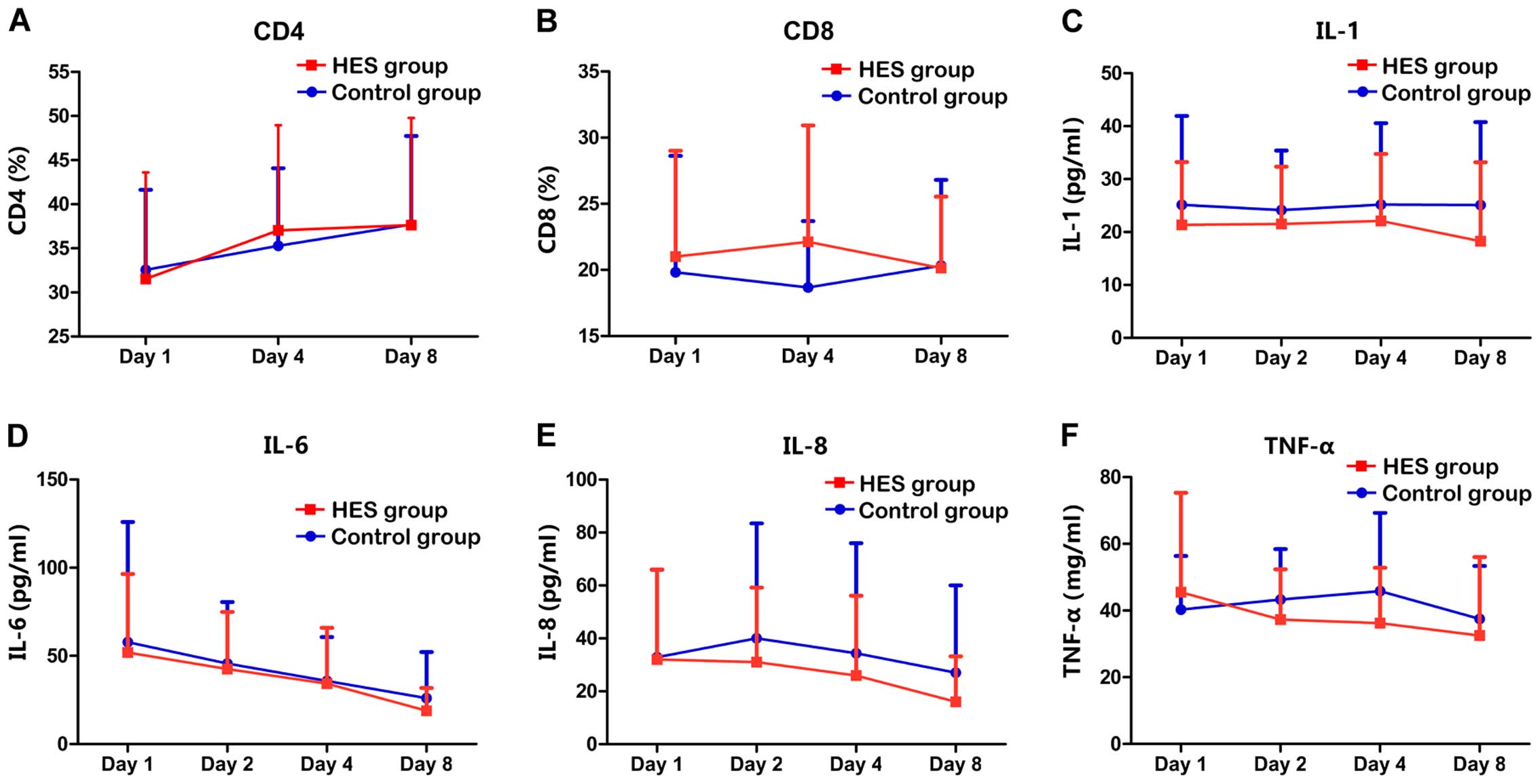
We compared the inter-group differences with regard
to the patients' general condition, CT grade, APACHE II score, IAP
value after admission, peritoneal drainage rate, inflammatory
cytokine value, lymphocyte subsets rates and other biochemical
values. In order to obtain a clear description of changes, we made
line charts using the inflammatory cytokine values (including IL-1,
IL-6, IL-8 and TNF-α) on days 1, 2, 4, and 8 after admission. Line
charts were also made using lymphocyte subset rates (including
CD4+CD8+) on days 1, 4, and 8 after
admission.
We evaluated the effect of the treatment on
inflammatory cytokine levels and lymphocyte subset rates with
regression analyses in the two groups. Additionally, a model
adjusted for potential confounders [gender, age and peritoneal
drainage (yes or not)] was established simultaneously. The
longitudinal changes in inflammatory cytokine values and lymphocyte
subset rates were analyzed with linear mixed-effects regression
models in the two groups. We also calculated the effect of HES
130/0.4 on the serum BUN and Cr values based on the abovementioned
model.
Changes in the inflammatory cytokine levels and
lymphocyte subset rates were dependent on the treatment options and
curing time. To reveal whether the effect of HES 130/0.4 was
critical for the longitudinal changes in the inflammatory cytokine
values and lymphocyte subset rates, a mixed-effects model was
set-up to estimate the interaction between a fixed effect variable
and hospital stay. First, the variable data were transformed into
multiple records based on the admission time. Potential confounders
[gender, age and peritoneal drainage (yes or not)] were also
adjusted in these models. Then, the treatment effect (crystalloid
plus HES 130/0.4 resuscitation or only crystalloid resuscitation),
time effect (hospital stay) and the interaction between the
treatment and time effects in both groups were evaluated in
multiple regression models. Statistical analysis (P) elicited
whether the fixed effect variable of the HES group was significant
for the inflammatory cytokine values and lymphocyte subset rates
when compared with the control group. We also calculated the effect
of HES 130/0.4 on the serum BUN and Cr values based on the above
model.
Results
Scatter plots of
CD4+CD8+ T lymphocyte rates and inflammatory
cytokine value
Fig. 1 shows the
difference in the lymphocyte subset rates and inflammatory cytokine
levels between the two groups. CD4+CD8+
T-cell rates were comparable on days 1 and 8 after hospitalization,
whereas the CD4+CD8+ T rate was higher on day
4 after hospitalization (Fig. 1A and
B). Lower levels of IL-1, IL-6 and IL-8 were detected in the
HES group compared with the control group on days 1, 2, 4 and 8
after hospitalization (Fig. 1C-E).
Higher TNF-α level was detected in the HES group on day 1 (Fig. 1F). We also observed lower level of
TNF-α on days 2, 4 and 8 in the HES group compared with the control
group (Fig. 1F).
Regression analyses of the changes of
CD4+CD8+ T lymphocyte rates, inflammatory
cytokine and renal function values based on basic and adjusted
models. To investigate the impact of different methods of fluid
resuscitation on the CD4+CD8+ T lymphocyte
rates, pro-inflammatory cytokine values and renal function,
mixed-effects regression models were established. Model I (not
adjusted for related risk factors) and model II [adjusted for year,
gender and peritoneal drainage (yes or no)] were established
simultaneously. Our results demonstrated the different fluid
resuscitation methods elicited significantly elevated
CD4+ T-cell rates for model I (in the HES group:
Coefficient=0.78, 95% CI=0.40 to 1.16, P-<0.001; and in the
control group: Coefficient=0.71, 95% CI=0.35 to 1.07, P<0.001)
(Table II). Correlation between
fluid resuscitation and the CD8+ T-cell rate in the HES
group was significantly negative in model I (coefficient =−0.25,
95% CI=−0.47 to −0.04, P-value, 0.027), whereas the relationship
was positive and not significant in the control group
(coefficient=0.04, 95% CI=−0.27 to 0.35, P=0.813). Additionally,
there was a similar tendency for the CD4+CD8+
T lymphocyte rates in models I and II.
 | Table II.Regression analyses of the changes of
CD4+CD8+ T lymphocyte rates, inflammatory
cytokine and renal function values based on different analysis
models. |
Table II.
Regression analyses of the changes of
CD4+CD8+ T lymphocyte rates, inflammatory
cytokine and renal function values based on different analysis
models.
|
| Model I | Model II |
|---|
|
|
|
|
|---|
|
| Coefficient | 95% CI | P-value | Coefficient | 95% CI | P-value |
|---|
| CD4+ T
cell (%) |
|
|
|
|
|
|
| HES
group | 0.78 | 0.40 to 1.16 | <0.001 | 0.77 | 0.40 to 1.15 | <0.001 |
| Control
group | 0.71 | 0.35 to 1.07 | <0.001 | 0.72 | 0.36 to 1.08 | <0.001 |
| CD8+ T
cell (%) |
|
|
|
|
|
|
| HES
group | −0.25 | −0.47 to −0.04 | 0.027 | −0.25 | −0.47 to −0.04 | 0.027 |
| Control
group | 0.04 | −0.27 to 0.35 | 0.813 | 0.04 | −0.27 to 0.35 | 0.798 |
| IL-1 (pg/ml) |
|
|
|
|
|
|
| HES
group | −0.46 | −0.71 to −0.20 | <0.001 | −0.46 | −0.71 to −0.20 | <0.001 |
| Control
group | −0.05 | −0.34 to 0.24 | 0.741 | −0.05 | −0.34 to 0.24 | 0.733 |
| IL-6 (pg/ml) |
|
|
|
|
|
|
| HES
group | −4.03 | −5.01 to −3.05 | <0.001 | −4.03 | −5.01 to −3.04 | <0.001 |
| Control
group | −3.77 | −5.13 to −2.41 | <0.001 | −3.76 | −5.13 to −2.40 | <0.001 |
| IL-8 (pg/ml) |
|
|
|
|
|
|
| HES
group | −2.08 | −2.87 to −1.29 | <0.001 | −2.08 | −2.87 to −1.29 | <0.001 |
| Control
group | −0.93 | −1.78 to −0.08 | 0.034 | −0.93 | −1.78 to −0.08 | 0.034 |
| TNF-α (pg/ml) |
|
|
|
|
|
|
| HES
group | −1.64 | −2.40 to −0.87 | <0.001 | −1.64 | −2.41 to −0.87 | <0.001 |
| Control
group | −0.46 | −1.00 to 0.07 | 0.093 | −0.47 | −1.00 to 0.07 | 0.090 |
| BUN (mmol/l) |
|
|
|
|
|
|
| HES
group | −0.12 | −0.25 to −0.02 | 0.090 | −0.12 | −0.25 to 0.02 | 0.090 |
| Control
group | −0.19 | −0.27 to −0.12 | <0.001 | −0.19 | −0.27 to −0.12 | <0.001 |
| Cr (µmol/l) |
|
|
|
|
|
|
| HES
group | −1.91 | −3.43 to −0.39 | 0.015 | −1.91 | −3.43 to −0.39 | 0.015 |
| Control
group | −3.26 | −4.54 to −1.98 | <0.001 | −3.28 | −4.56 to −2.00 | <0.001 |
In model I, IL-1, IL-6, IL-8 and TNF-α levels were
reduced significantly in the HES group, while IL-6 and IL-8 levels
decreased significantly in the control group (P<0.05). In the
control group, IL-1 and TNF-α levels were also reduced, but the
reduction was not significant. Inflammatory cytokine distribution
in model II was similar to that in model I. The Cr level decreased
significantly in the two groups based on models I and II
(P<0.001), while no obvious change in BUN value was detected in
either group (P>0.05).
Regression analyses of the impact of
hospital stay, resuscitation methods and the interaction between
hospital stay and different fluid resuscitation methods for the
changes of CD4+CD8+ T lymphocyte rates,
inflammatory cytokines and renal function value
To investigate whether crystalloid plus HES 130/0.4
resuscitation is a critical factor for the reduction of the
lymphocyte subset rates, inflammatory cytokines and renal function
values compared in 2 groups. New multiple regression models were
established to evaluate the impact of hospital stay, resuscitation
methods and the relation between hospital stay and different fluid
resuscitation methods. Additionally, its impact on the changes in
the BUN and Cr values was analyzed in this model. Potential
confounders, including gender, age and peritoneal drainage (yes or
no), were also adjusted in this model.
As shown in Table
III, there was a significant elevation in the CD4+ T
lymphocyte rates [risk ratio (RR) difference = 0.725, P<0.001]
and reduction in the IL-6, BUN and Cr levels (P<0.001) in the
HES group compared with the control group. The use of crystalloid
plus HES 130/0.4 resuscitation had no significant effect on the
CD4+CD8+ T lymphocyte rates, inflammatory
cytokines and renal function. The interaction between hospital stay
and different fluid resuscitation methods was analyzed in this
model, and results revealed the presence of cumulative effects in
the impact of crystalloid plus HES 130/0.4 resuscitation. The RR
difference of the observed variables with changes over time between
the HES and control groups was significantly lower for IL-1
(RR=0.406, P=0.041) and TNF-α (RR=−1.189, P=0.013). It showed a
marginally significant difference in case of IL-8 (RR=−1.149,
P=0.054). The curve's RR difference was not significant for IL-6,
the CD4+CD8+ T lymphocyte rate, BUN and Cr
values (P>0.05).
 | Table III.Regression analyses of the impact of
hospital stay, treatments and the interaction between hospital stay
and different fluid resuscitation methods for the changes of
CD4+CD8+ T lymphocyte rates, inflammatory
cytokine and renal function value. |
Table III.
Regression analyses of the impact of
hospital stay, treatments and the interaction between hospital stay
and different fluid resuscitation methods for the changes of
CD4+CD8+ T lymphocyte rates, inflammatory
cytokine and renal function value.
|
| Time | Treatment | Time:treatment |
|---|
|
|
|
|
|
|---|
|
| RR difference | SE | P-value | RR difference | SE | P-value | RR difference | SE | P-value |
|---|
| CD4 (%) | 0.725 | 0.196 | <0.001 | −1.195 | 2.684 | 0.658 | 0.051 | 0.267 | 0.849 |
| CD8 (%) | 0.024 | 0.141 | 0.867 | 2.863 | 1.769 | 0.111 | −0.251 | 0.192 | 0.193 |
| IL-1 (pg/ml) | −0.050 | 0.139 | 0.718 | −2.665 | 2.465 | 0.282 | −0.406 | 0.197 | 0.041 |
| IL-6 (pg/ml) | −3.761 | 0.604 | <0.001 | −3.698 | 6.249 | 0.555 | −0.269 | 0.861 | 0.755 |
| IL-8 (pg/ml) | −0.931 | 0.416 | 0.026 | −3.360 | 5.760 | 0.561 | −1.149 | 0.593 | 0.054 |
| TNF-α (pg/ml) | −0.460 | 0.333 | 0.168 | 1.185 | 3.455 | 0.732 | −1.189 | 0.474 | 0.013 |
| BUN (mmol/l) | −0.192 | 0.055 | <0.001 | −0.489 | 0.589 | 0.408 | 0.076 | 0.078 | 0.328 |
| Cr (µmol/l) | −3.268 | 0.717 | <0.001 | 2.707 | 8.910 | 0.762 | 1.360 | 1.013 | 0.181 |
Percentage of patients with negative
FB at 8 days
We calculated the number of patients with negative
FB(−) on a daily basis. Patients with peritoneal drainage were not
included in this analysis. After excluding those patients with
peritoneal drainage, 50 cases remained in the HES group and 51
cases in the control group. As shown in Table IV, there was a significantly higher
number of patients with a negative FB from day 4 to 8 in the HES
group (P<0.05).
 | Table IV.Percentage of patients with negative
fluid balance within 8 days. |
Table IV.
Percentage of patients with negative
fluid balance within 8 days.
| Negative FB [n,
(%)] | HES group
(n=50) | Control group
(n=51) | P-value |
|---|
| Day 1 | 11 (22%) | 7 (13.7%) | 0.277 |
| Day 2 | 14 (28%) | 14 (27.5%) | 0.95 |
| Day 3 | 17 (34%) | 12 (23.5%) | 0.244 |
| Day 4 | 13 (26%) | 16 (31.4%) | 0.55 |
| Day 5 | 21 (42%) | 12 (23.5%) | 0.047 |
| Day 6 | 36 (72%) | 14 (28.6%) | <0.001 |
| Day 7 | 36 (72%) | 20 (40.8%) | <0.001 |
| Day 8 | 38 (77.6%) | 17 (35.4%) | <0.001 |
Discussion
In the early phase of SAP, activation of
inflammatory cells leads to the release of pro-inflammatory
mediators which lie at the heart of the pathologic process and are
involved in all aspects of the cascade leading to SIRS and multiple
organ dysfunction syndrome (29). It
has been established that the excessive production of inflammatory
mediators is responsible for the escalation of localized pancreatic
inflammation into a generalized systemic inflammatory response,
irrespective of the initiating stimulus (30). Many studies have shown that plasma
levels of pro-inflammatory cytokines are usually elevated early in
the course of AP and are associated with severity of the disease
(2,31–34).
Thus, resolving the inflammatory status by downregulating the
pro-inflammatory cytokines significantly improves the
prognosis.
HES is a type of colloid solution that is widely
used for fluid resuscitation in intensive care units. HES has the
advantages of minimizing resuscitation volumes and the potential to
sustain the intravascular volume for longer periods (35). Results obtained from our previous
studies suggested that fluid resuscitation with HES in the early
stages of SAP could improve the prognosis (16,36).
Additionally, a recent study has indicated that HES resuscitation
may attenuate SIRS by downregulating pro-inflammatory cytokine
(21). However, the exact mechanism
for the HES effect on cytokines is not well understood. Working on
rat sepsis models, Feng et al reported that HES 130/0.4
inhibited the activation of nuclear factor-κB and neutrophil
adhesion and migration, thus inhibiting cytokine production
(37). Schäper et al
demonstrated that HES prevented the inflammatory reaction by
relieving ischemia reperfusion injury in the intestine (38). In the present study, we have shown
that HES combined with crystalloid fluid resuscitation decreased
IL-1 and TNF-α levels in peripheral blood.
IL-1 is an important mediator of inflammatory
changes during pancreatitis. During the early phase of AP, IL-1
initiates the inflammatory cascade and activates the endothelium,
allowing the migration of neutrophils into the post-venule and
resulting in neutrophil degranulation, adhesion molecule
expression, and chemokine activity. Additionally, TNF-α derived
from macrophages and monocytes interacts with a number of other
cytokines such as IL-1, IL-6 and platelet activation factor, which
participate in this process simultaneously (39). The present study demonstrated that
IL-1 and TNF-α levels decreased significantly in the HES group
(P<0.05) while the IL-8 level decreased only marginally in this
group compared with the control group (P=0.054). These results
suggested that HES combined with colloid fluid resuscitation
decreased the pro-inflammatory cytokine concentration and improved
the SIRS status.
In addition to the pro-inflammatory cytokine
cascade, the activated adaptive immune system including
CD4+CD8+ T lymphocytes are central to the
development of SIRS and organ failure in AP patients (40,41).
Previous findings have shown that a significant reduction in the
proportion of CD4+ T cells is correlated with the
severity of AP (8,9,42). In a
previous study, we showed that the reduction of peripheral blood
CD4+ T lymphocytes was associated with persistent organ
failure (10). Ozturk et al
reported a higher CD4+ T lymphocyte level and
CD4+:CD8+ T-cell ratio, in coronary surgery
patients, in the HES 130/0.4 group compared with the crystalloid
group (21). Differences in the
CD4+CD8+ lymphocyte subset rates between the
HES and control groups were not significant in this study. This
phenomenon may be explained by the fact that the immune system in
SAP patients is affected by multiple organs and colloid
resuscitation alone is insufficient to influence patients' adaptive
immune system. The mechanism by which HES may affect
CD4+CD8+ lymphocyte subsets is still
unclear.
Early effective fluid resuscitation is recommended
to shorten the duration of SIRS and reduce morbidity and mortality
among AP patients (43). However,
higher capillary permeability results in loss of fluid from the
intravascular space and fluid sequestration into the third space,
which facilitates the deficiency in blood volume. Excess fluids may
be harmful for effective organ perfusion, in critically ill
patients and can increase the mortality rate and cause various
complications, including IAH and abdominal compartment syndrome,
which are associated with a poor prognosis for SAP patients
(44). Previous findings have shown
that FB-positive(+) status was associated with the poor prognosis
of critically ill patients (45,46).
Barmparas et al reported that the early attainment of FB(−)
status was associated with a nearly 70% reduction in the risk of
mortality in critically ill surgical patients (47). Therefore, maintaining colloid osmotic
pressure and achieving FB(−) status earlier are important factors
for the prognosis of SAP patients.
This study presented significantly higher rates of
patients with FB(−) from day 4 to 8 in the HES group after
excluding those patients with peritoneal drainage, which indicated
HES 130/0.4 combined crystalloid resuscitation could significantly
shorten FB(+) duration. This can be explained by the fact that HES
130/0.4 belongs to a family of polydispersed colloid solutions with
polymerized amylopectin molecules which do not leak from capillary
vessels. This characteristic makes HES to sustain its colloid
osmotic pressure longer than crystalloid solutions alone (48). These results also suggested that HES
combined with crystalloid fluid resuscitation could negatively
affect the release of pro-inflammatory cytokines, which may be
another cause for the effect of HES on FB.
Recently, safety concerns for the clinical use of
HES 130/0.4 for acute volume resuscitation have attracted the
attention of the researchers in this field. The most important
concern was the effect of HES 130/0.4 on renal function (17,18,20).
However, we did not observe any HES related effects on renal
function for SAP patients in this study. However, no patients with
renal failure were included in this study. Due to potential acute
kidney injury, HES 130/0.4 should be used with extreme caution for
SAP patients with renal failure.
There are certain limitations to our study. First,
this was an observational study that revealed the effect of HES
130/0.4 on pro-inflammatory cytokines, FB status and renal
function. Whether HES 130/0.4 may provide a better prognosis merits
further investigation. Second, our study only included data
obtained from the first 8 days after hospitalization. Third,
previous studies reported that HES 130/0.4 changed the
CD4+ T lymphocytes and the
CD4+:CD8+ T cell ratio compared with those
patients who only received crystalloid resuscitation after coronary
surgery (21). However, we did not
observe this effect in this study. This may be due to the fact that
HES 130/0.4 was only used in the 1st week, which did not produce
any changes in patient's immune status. The exact mechanism for the
effect of HES 130/0.4 on CD4+:CD8+ T
lymphocytes should be investigated in future.
In conclusion, we identified that HES treatment
could decrease IL-1 and IL-8 levels, shorten the duration of
positive FB, and preserve the patient's immune status and renal
function during the early phase of SAP.
References
|
1
|
Mitchell RM, Byrne MF and Baillie J:
Pancreatitis. Lancet. 361:1447–1455. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang J, Niu J and Yang J: Interleukin-6,
interleukin-8 and interleukin-10 in estimating the severity of
acute pancreatitis: an updated meta-analysis.
Hepatogastroenterology. 61:215–220. 2014.PubMed/NCBI
|
|
3
|
Wang XY, Tang QQ, Zhang JL, Fang MY and Li
YX: Effect of SB203580 on pathologic change of pancreatic tissue
and expression of TNF-α and IL-1β in rats with severe acute
pancreatitis. Eur Rev Med Pharmacol Sci. 18:338–343.
2014.PubMed/NCBI
|
|
4
|
Singh VK, Wu BU, Bollen TL, Repas K,
Maurer R, Mortele KJ and Banks PA: Early systemic inflammatory
response syndrome is associated with severe acute pancreatitis.
Clin Gastroenterol Hepatol. 7:1247–1251. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sathyanarayan G, Garg PK, Prasad H and
Tandon RK: Elevated level of interleukin-6 predicts organ failure
and severe disease in patients with acute pancreatitis. J
Gastroenterol Hepatol. 22:550–554. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu Y, Wang L, Cai Z, Zhao P, Peng C, Zhao
L and Wan C: The decrease of peripheral blood CD4+ T
cells indicates abdominal compartment syndrome in severe acute
pancreatitis. PLoS One. 10:e01357682015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pezzilli R, Billi P, Gullo L, Beltrandi E,
Maldini M, Mancini R, Incorvaia L and Miglioli M: Behavior of serum
soluble interleukin-2 receptor, soluble CD8 and soluble CD4 in the
early phases of acute pancreatitis. Digestion. 55:268–273. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pezzilli R, Billi P, Beltrandi E, Maldini
M, Mancini R, Labate AM Morselli and Miglioli M: Circulating
lymphocyte subsets in human acute pancreatitis. Pancreas.
11:95–100. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Uehara S, Gothoh K, Handa H, Tomita H and
Tomita Y: Immune function in patients with acute pancreatitis. J
Gastroenterol Hepatol. 18:363–370. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang Z, Zhang Y, Dong L, Yang C, Gou S,
Yin T, Wu H and Wang C: The reduction of peripheral blood
CD4+ T cell indicates persistent organ failure in acute
pancreatitis. PLoS One. 10:e01255292015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lipinski M, Rydzewska-Rosolowska A,
Rydzewski A and Rydzewska G: Fluid resuscitation in acute
pancreatitis: normal saline or lactated Ringer's solution? World J
Gastroenterol. 21:9367–9372. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
de-Madaria E, Soler-Sala G, Sánchez-Payá
J, Lopez-Font I, Martínez J, Gómez-Escolar L, Sempere L,
Sánchez-Fortún C and Pérez-Mateo M: Influence of fluid therapy on
the prognosis of acute pancreatitis: a prospective cohort study. Am
J Gastroenterol. 106:1843–1850. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mao EQ, Tang YQ, Fei J, Qin S, Wu J, Li L,
Min D and Zhang SD: Fluid therapy for severe acute pancreatitis in
acute response stage. Chin Med J (Engl). 122:169–173.
2009.PubMed/NCBI
|
|
14
|
Freitag M, Standl TG, Kleinhans H,
Gottschalk A, Mann O, Rempf C, Bachmann K, Gocht A, Petri S,
Izbicki JR, et al: Improvement of impaired microcirculation and
tissue oxygenation by hemodilution with hydroxyethyl starch plus
cell-free hemoglobin in acute porcine pancreatitis. Pancreatology.
6:232–239. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Du XJ, Hu WM, Xia Q, Huang ZW, Chen GY,
Jin XD, Xue P, Lu HM, Ke NW, Zhang ZD, et al: Hydroxyethyl starch
resuscitation reduces the risk of intra-abdominal hypertension in
severe acute pancreatitis. Pancreas. 40:1220–1225. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yang ZY, Wang CY, Jiang HC, Sun B, Zhang
ZD, Hu WM, Ou JR and Hou BH: Effects of early goal-directed fluid
therapy on intra-abdominal hypertension and multiple organ
dysfunction in patients with severe acute pancreatitis. Zhonghua
Wai Ke Za Zhi. 47:1450–1454. 2009.(In Chinese). PubMed/NCBI
|
|
17
|
Haase N, Perner A, Hennings LI, Siegemund
M, Lauridsen B, Wetterslev M and Wetterslev J: Hydroxyethyl starch
130/0.38-0.45 versus crystalloid or albumin in patients with
sepsis: systematic review with meta-analysis and trial sequential
analysis. BMJ. 346:f8392013. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zarychanski R, Abou-Setta AM, Turgeon AF,
Houston BL, McIntyre L, Marshall JC and Fergusson DA: Association
of hydroxyethyl starch administration with mortality and acute
kidney injury in critically ill patients requiring volume
resuscitation: a systematic review and meta-analysis. JAMA.
309:678–688. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Perner A, Haase N, Winkel P, Guttormsen
AB, Tenhunen J, Klemenzson G, Müller RG, Aneman A and Wetterslev J:
Long-term outcomes in patients with severe sepsis randomised to
resuscitation with hydroxyethyl starch 130/0.42 or Ringer's
acetate. Intensive Care Med. 40:927–934. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Perner A, Haase N, Guttormsen AB, Tenhunen
J, Klemenzson G, Åneman A, Madsen KR, Møller MH, Elkjær JM, Poulsen
LM, et al: 6S Trial Group; Scandinavian Critical Care Trials Group:
Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe
sepsis. N Engl J Med. 367:124–134. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Öztürk T, Onur E, Cerrahoğlu M, Çalgan M,
Nizamoglu F and Çivi M: Immune and inflammatory role of
hydroxyethyl starch 130/0.4 and fluid gelatin in patients
undergoing coronary surgery. Cytokine. 74:69–75. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Choi YS, Shim JK, Hong SW, Kim JC and Kwak
YL: Comparing the effects of 5% albumin and 6% hydroxyethyl starch
130/0.4 on coagulation and inflammatory response when used as
priming solutions for cardiopulmonary bypass. Minerva Anestesiol.
76:584–591. 2010.PubMed/NCBI
|
|
23
|
Balthazar EJ: Acute pancreatitis:
assessment of severity with clinical and CT evaluation. Radiology.
223:603–613. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Working Party of the British Society of
Gastroenterology; Association of Surgeons of Great Britain and
Ireland; Pancreatic Society of Great Britain and Ireland;
Association of Upper GI Surgeons of Great Britain and Ireland, . UK
guidelines for the management of acute pancreatitis. Gut. 54(Suppl
1): i1–i9. 2005.PubMed/NCBI
|
|
25
|
Group of Pancreas Surgery, Chinese Society
of Surgery, Chinese Medical Association, . The guideline of
diagnosis and treatment of severe acute pancreatitis. Zhonghua Wai
Ke Za Zhi. 45:727–729. 2007.(In Chinese). PubMed/NCBI
|
|
26
|
Uhl W, Warshaw A, Imrie C, Bassi C, McKay
CJ, Lankisch PG, Carter R, Di Magno E, Banks PA, Whitcomb DC, et
al: International Association of Pancreatology: IAP guidelines for
the surgical management of acute pancreatitis. Pancreatology.
2:565–573. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Malbrain ML, Cheatham ML, Kirkpatrick A,
Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C,
Ivatury R, et al: Results from the international conference of
experts on intra-abdominal hypertension and abdominal compartment
syndrome. I. Definitions. Intensive Care Med. 32:1722–1732. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yang C, Yang Z, Chen X, Liu T, Gou S, Chen
C, Xiao J, Jin X, He Z, Dong L, et al: Inverted U-shaped
relationship between central venous pressure and intra-abdominal
pressure in the early phase of severe acute pancreatitis: a
retrospective study. PLoS One. 10:e01284932015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Makhija R and Kingsnorth AN: Cytokine
storm in acute pancreatitis. J Hepatobiliary Pancreat Surg.
9:401–410. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zyromski N and Murr MM: Evolving concepts
in the pathophysiology of acute pancreatitis. Surgery. 133:235–237.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fink GW and Norman JG: Specific changes in
the pancreatic expression of the interleukin 1 family of genes
during experimental acute pancreatitis. Cytokine. 9:1023–1027.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Park J, Chang JH, Park SH, Lee HJ, Lim YS,
Kim TH, Kim CW and Han SW: Interleukin-6 is associated with
obesity, central fat distribution, and disease severity in patients
with acute pancreatitis. Pancreatology. 15:59–63. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chen CC, Wang SS, Lee FY, Chang FY and Lee
SD: Proinflammatory cytokines in early assessment of the prognosis
of acute pancreatitis. Am J Gastroenterol. 94:213–218. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Exley AR, Leese T, Holliday MP, Swann RA
and Cohen J: Endotoxaemia and serum tumour necrosis factor as
prognostic markers in severe acute pancreatitis. Gut. 33:1126–1128.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bunn F and Trivedi D: Colloid solutions
for fluid resuscitation. Cochrane Database Syst Rev.
7:CD0013192012.PubMed/NCBI
|
|
36
|
Zhao G, Zhang JG, Wu HS, Tao J, Qin Q,
Deng SC, Liu Y, Liu L, Wang B, Tian K, et al: Effects of different
resuscitation fluid on severe acute pancreatitis. World J
Gastroenterol. 19:2044–2052. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Feng X, Yan W, Liu X, Duan M, Zhang X and
Xu J: Effects of hydroxyethyl starch 130/0.4 on pulmonary capillary
leakage and cytokines production and NF-kappaB activation in
CLP-induced sepsis in rats. J Surg Res. 135:129–136. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Schäper J, Ahmed R, Schäfer T, Elster A,
Enigk F, Habazettl H, Mousa S, Schäfer M and Welte M: Volume
therapy with colloid solutions preserves intestinal microvascular
perfusion in endotoxaemia. Resuscitation. 76:120–128. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lane JS, Todd KE, Gloor B, Chandler CF,
Kau AW, Ashley SW, Reber HA and McFadden DW: Platelet activating
factor antagonism reduces the systemic inflammatory response in a
murine model of acute pancreatitis. J Surg Res. 99:365–370. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Oiva J, Mustonen H, Kylänpää ML, Kyhälä L,
Kuuliala K, Siitonen S, Kemppainen E, Puolakkainen P and Repo H:
Acute pancreatitis with organ dysfunction associates with abnormal
blood lymphocyte signaling: controlled laboratory study. Crit Care.
14:R2072010. View
Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nakayama S, Nishio A, Yamashina M, Okazaki
T, Sakaguchi Y, Yoshida K, Fukui T, Uchida K and Okazaki K:
Acquired immunity plays an important role in the development of
murine experimental pancreatitis induced by alcohol and
lipopolysaccharide. Pancreas. 43:28–36. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Curley PJ, McMahon MJ, Lancaster F, Banks
RE, Barclay GR, Shefta J, Boylston AW and Whicher JT: Reduction in
circulating levels of CD4-positive lymphocytes in acute
pancreatitis: relationship to endotoxin, interleukin 6 and disease
severity. Br J Surg. 80:1312–1315. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Warndorf MG, Kurtzman JT, Bartel MJ, Cox
M, Mackenzie T, Robinson S, Burchard PR, Gordon SR and Gardner TB:
Early fluid resuscitation reduces morbidity among patients with
acute pancreatitis. Clin Gastroenterol Hepatol. 9:705–709. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Al-Bahrani AZ, Abid GH, Holt A, McCloy RF,
Benson J, Eddleston J and Ammori BJ: Clinical relevance of
intra-abdominal hypertension in patients with severe acute
pancreatitis. Pancreas. 36:39–43. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Cunha AR and Lobo SM: What happens to the
fluid balance during and after recovering from septic shock? Rev
Bras Ter Intensiva. 27:10–17. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lee J, de Louw E, Niemi M, Nelson R, Mark
RG, Celi LA, Mukamal KJ and Danziger J: Association between fluid
balance and survival in critically ill patients. J Intern Med.
277:468–477. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Barmparas G, Liou D, Lee D, Fierro N,
Bloom M, Ley E, Salim A and Bukur M: Impact of positive fluid
balance on critically ill surgical patients: a prospective
observational study. J Crit Care. 29:936–941. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Boldt J: Hydroxyethyl starch:
pharmaceutical and clinical profile. Minerva Anestesiol.
65:305–309. 1999.PubMed/NCBI
|