Introduction
Moist diaper with urine and stool may irritate the
buttock skin around the diaper, cause diaper rash, redness and
hyperemia in the skin of buttock and perineum, erythema and
papules, even excoriation and erosion (1). Infants with diaper rash may be crying,
agitated and sleepless due to redness in the diaper area.
Prophylactics are important in the clinical management of infant
diaper rash. Parents should pay attention to the redness around the
buttock of the infant and provide immediate treatment (2,3).
In the present study, we selected 210 infants who
received hydrocolloid dressings, mupirocin plaster as well as
topical application of pearl powder and zinc oxide plaster for
diaper rash, and underwent nursing intervention from January, 2015
to December, 2015. The results of the present study showed that
hydrocolloid dressings combined with individualized nursing may
prevent and treat infant diaper rash effectively, decrease the
incidence of adverse reactions significantly, shorten time to
resolution of diaper rash and hospitalization duration, reduce mean
hospitalization cost, improve parent satisfaction and promote
nursing-patient harmony. Therefore, this method of treatment was
worthy of clinical application.
Materials and methods
General
A total of 210 infants who met the diagnostic
criteria of diaper rash, were included in the present study from
January, 2015 to December, 2015. A total of 106 males and 104
females, with a mean age of 5.7±1.2 months (3–12 months), and
disease course of 16.4±2.5 days (2–25 days) were included. Of the
210 cases, there were 82 mild cases, 75 severity grade I cases and
53 severity grade II cases. Admission diagnosis included: 30
infants with neonatal diarrhea, 15 infants with neonatal
hyperbilirubinemia, 15 premature infants, 3 infants with neonatal
hypoxic-ischemic encephalopathy, 3 infants with infective
pneumonia, 2 infants with hyaline membrane disease and 2 infants
with intracranial hemorrhage. The differences in gender, age,
disease course and condition among these infants were not
significant.
Approval for the study was obtained from the Ethics
Committee of the Liaocheng People's Hospital. Informed consent of
patients and relatives was obtained prior to inclusion in the
study.
Treatments
The infants in group A received hydrocolloid
dressings [State Food and Drug Administration (import) 3640809,
2013; Coloplast A/S, Humlebæk, Denmark] with a cycle of 5 days.
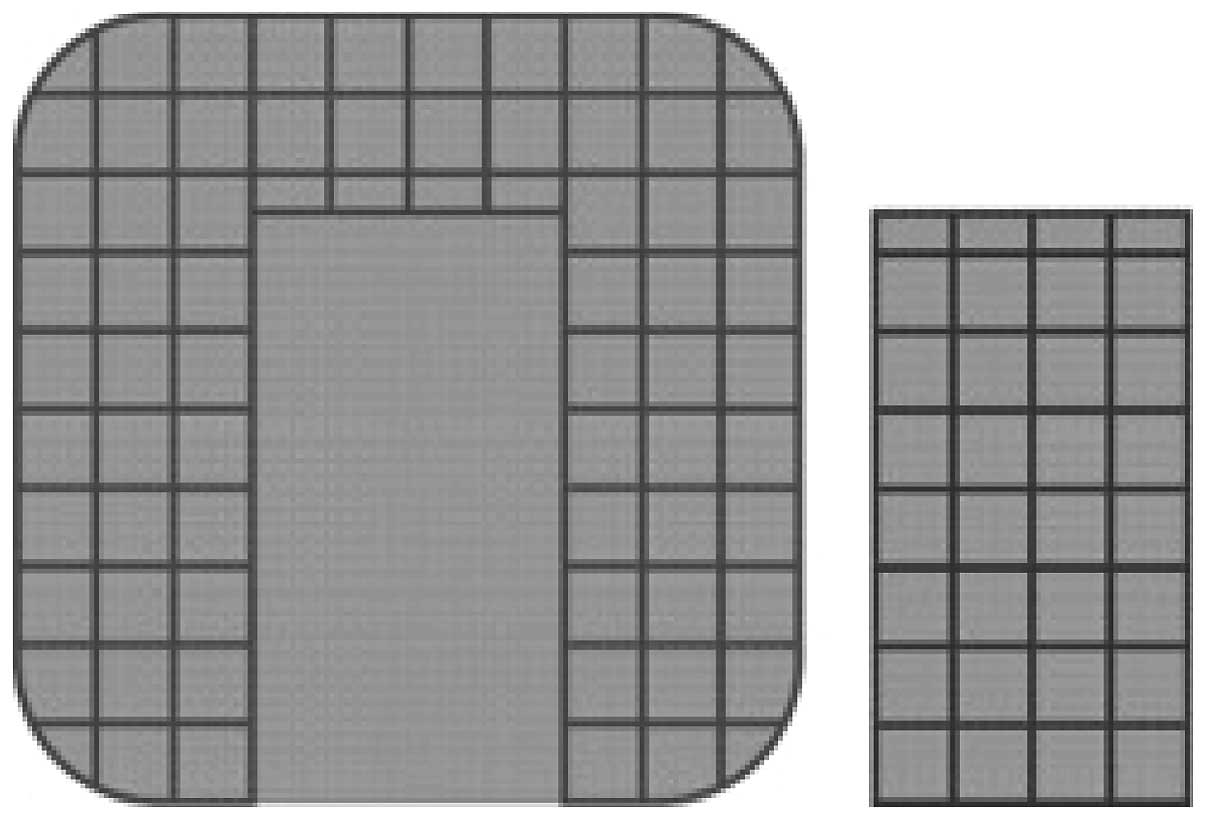
Hydrocolloid dressings (10×10 cm) was cut as Fig. 1, with a left/right margin of 3 cm and
an upper margin of 2.5 cm. The prepared hydrocolloid dressings were
gently applied and fixed on the redness of the affected buttock.
The hydrocolloid dressings were changed based on the actual use.
The hydrocolloid dressings were immediately changed in the case of
ivory-white bubble or stool/urine on hydrocolloid dressings.
The infants in group B received mupirocin plaster
(SFDA approval no. H10930064, a cycle of 5 days; American Tianjin
Smith Kline Pharmaceutical Co., Ltd., Tianjin, China), and topical
application of pearl powder (SFDA approval no. Z51020812; Sichuan
Kelun Pharmaceutical Co., Ltd., Sichuan, China).
The infants in group C received zinc oxide plaster
(SFDA approval no. H11022229; Beijing Shuangji Pharmaceutical Co.,
Ltd., Beijing, China).
Nursing measures
Individualized nursing was provided in group A: i)
The buttock was cleaned with warm water after defecation and dried
with gauze, and the diaper was changed timely. ii) The trauma was
disinfected with iodophor, cleaned with normal saline, and dried
with a dry towel. Hydrocolloid dressings film was pasted on the
trauma. The nurse avoided direct contact with the inner side of
hydrocolloid dressings film via hands, and ensure no air bubbles
between the film and skin, leaving plain and closed interface
between the film and skin. The hydrocolloid dressings film were
immediately changed in the cases of fluid or feces/urine. The
hydrocolloid dressings film was very gently removed to ensure no
damage occurred to the delicate skin. iii) The induction of diaper
rash was prevented to ensure clean and dry buttock skin (4). iv) The nurse changed the diaper timely,
cleaned the buttock with warm water after defecation (soap was
prohibited) and dried gently with a towel to prevent skin injury.
v) Baby powder was not recommended during treatment, while paper
diaper with good air permeability or soft cotton diaper was
recommended, albeit plastic diaper or rubber diaper was prohibited.
vi) When ulcerate or erosion occurred in buttock skin, sterile
gauze was applied on the trauma, the frequency of changing sterile
gauze was dependent on the actual condition of trauma. vii)
Appropriate temperature and humidity was maintained to avoid low
room temperature, which would impact the healing and recovery of
trauma. viii) The nurse was required to educate the child's parents
regarding the diaper rash, explain any problems patiently,
communicate with parents, provide psychological intervention and
ease negative sentiment.
Observational measurements
The clinical healing, incidence of adverse events,
time to resolution of diaper rash, hospitalization duration, mean
cost and satisfaction of nursing were compared between the 3
groups.
Statistical analysis
SPSS 20.0 software (IBM SPSS, Armonk, NY, USA) was
used for statistical analysis. Measurement data were presented as
mean ± standard deviation and analyzed by t-test. Enumeration data
were presented as cases and analyzed using the Chi-square test.
Non-parametric data were analyzed by the rank-sum test, and
multi-samples were analyzed using ANOVA. P<0.05 was considered
to indicate a statistically significant difference.
Results
Healing rate
After 1 cycle of treatment and nursing, the healing
rate of diaper rash in infants between groups A, B and C was
significantly different (P<0.05), with the highest healing rate
in group A (96.3%). As shown in Table
I, the healing rate of severity grade I diaper rash in infants
between groups A, B and C was significantly different (P<0.05),
with highest healing rate in group A (92.0%). The healing rate of
severity grade II diaper rash in infants between groups A, B and C
was significantly different (P<0.05), with the highest healing
rate in group A (72.2%). Classical severity grade I cases: one
child was diagnosed as severity grade I before treatment (Fig. 2A), 24 h after treatment, the symptoms
were relieved (Fig. 2B), and 5 days
after treatment, the child recovered (Fig. 2C).
 | Table I.The healing of infants after 1
cycle. |
Table I.
The healing of infants after 1
cycle.
|
|
| Mild | Severity grade I | Severity grade
II |
|---|
|
|
|
|
|
|
|---|
| Groups | No. | No. | Healing | Healing rate (%) | No. | Healing | Healing rate (%) | No. | Healing | Healing rate (%) |
|---|
| A | 70 | 27 | 26 | 96.3 | 25 | 23 | 92.0 | 18 | 13 | 72.2 |
| B | 70 | 27 | 22 | 81.5 | 25 | 18 | 72.0 | 18 | 9 | 50.0 |
| C | 70 | 28 | 20 | 71.4 | 25 | 15 | 60.0 | 17 | 6 | 35.3 |
| P-value |
|
| <0.05 |
|
| <0.05 |
|
| <0.05 |
|
Factors
After treatment and nursing, the incidence of
adverse events in infants between groups A, B and C was
significantly different (P<0.05), with the lowest incidence in
group A (2.9%) (Table II). As shown
in Table III, after treatment and
nursing, the time to resolution of diaper rash, hospitalization
duration and cost in infants were not significantly different
(P<0.05), with the shortest time to resolution of diaper rash
and hospitalization duration as well as lowest mean hospitalization
cost in group A. The satisfaction rate of nursing for the parents
of groups A, B and C was 98.6, 87.1 and 80.0%, respectively, and
the difference was significant (P<0.05; Table IV).
 | Table II.The incidence of adverse events in
infants. |
Table II.
The incidence of adverse events in
infants.
| Groups | No. | Skin allergies | Pustule | Itching | Yellow exudate | Incidence of adverse
events (%) | P-value |
|---|
| A | 70 | 0 | 1 | 1 | 0 | 2.9 | <0.05 |
| B | 70 | 1 | 2 | 2 | 1 | 8.6 | <0.05 |
| C | 70 | 1 | 4 | 2 | 1 | 11.4 | <0.05 |
 | Table III.Time to resolution of diaper rash,
hospitalization duration and cost in infants (mean ± standard
deviation). |
Table III.
Time to resolution of diaper rash,
hospitalization duration and cost in infants (mean ± standard
deviation).
| Groups | No. | Time to resolution
(h) | Hospitalization
duration (day) | Hospitalization cost
(RMB) |
|---|
| A | 70 |
71.64±16.72 | 5.4±1.3 | 2564.7±367.2 |
| B | 70 |
86.81±18.43 | 7.1±2.2 | 3637.5±412.8 |
| C | 70 | 107.53±21.43 | 9.6±2.7 | 4484.6±533.4 |
| P-value |
|
<0.05 | <0.05 | <0.05 |
 | Table IV.Satisfaction rate of nursing in
parents. |
Table IV.
Satisfaction rate of nursing in
parents.
| Groups | No. | Very satisfied | Satisfied | Dissatisfied | Total satisfaction
(%) | P-value |
|---|
| A | 70 | 41 | 28 | 1 | 98.6 | <0.05 |
| B | 70 | 34 | 27 | 9 | 87.1 | <0.05 |
| C | 70 | 29 | 27 | 14 | 80.0 | <0.05 |
Discussion
Diaper rash in infants is also known as red buttock,
and was a common disease of skin injury in infants (5). The induction factors of diaper rash
include: i) Infant skin was delicate, if the diaper had not been
changed immediately, the urea in urine were metabolized into
ammonia, which may irritate infant buttock skin and cause
inflammation. ii) The moist and warm diaper region of infants was
susceptible to maceration of stratum corneum, leading to gradual
degeneration of the barrier function of epidermis, and as a result,
fungi penetrated the skin and caused fungal infection. iii) Infant
was of poor immunity and susceptible to diseases, thus the
administration of antibiotics may have caused secondary infection,
and prototype antibiotics were excreted with feces and urine.
Consequently, flora imbalance occurred in the skin and feces in the
diaper region, leading to diaper rash (6–9).
Investigators have reported the incidence of diaper
rash at 16–40%, therefore, more attention should be paid to the
prevention and treatment of diaper rash (10–12).
Currently, there are many available medications for infant diaper
rash with varying efficacy. Zinc oxide plaster can repair and
protect skin tissues. However, zinc oxide plaster has some
antibacterial effects, but is slow and inconvenient for topical
application (13). Mupirocin plaster
is a topical antibiotic plaster, and low levels of mupirocin had a
bacteriostatic effect and a high level of mupirocin had
bactericidal effect. With a broad antimicrobial spectrum, mupirocin
is efficacious for gram-positive and -negative bacteria (14). Pearl powder has heat-clearing and
detoxifying effects, and an astringent effect on tissue
regeneration. Mupirocin plaster combined with pearl powder may form
a protective membrane on human skin surface, thus may prevent the
irritation of urine and inhibit bacterial growth.
Active components of hydrocolloid dressings include
sodium carboxymethyl cellulose particles, medical tape and calcium
alginate, and its absorptive capacity has been demonstrated
previously (15). With good
self-adhesion and permeability, hydrocolloid dressings are aslo
convenient in clinical application. Additionally, hydrocolloid
dressings are closed, which can preserve the release of
biologically active substances and form low oxygen tension on the
surface and stimulate the release of interleukins, enhance the
bactericidal effect locally as well as repair and protect damaged
skin. Hydrocolloid dressings allow for the penetration of oxygen
and water into skin while permitting cleaning, drying and
moisturizing effects on human skin (16). Hydrocolloid dressings have been of
great interest and extensively applied. However, clinical
application of hydrocolloid dressings in the treatment of diaper
rash was limited currently.
The present study included 210 infants with diaper
rash who underwent different therapeutic options, and explored the
application of hydrocolloid dressings in the treatment of diaper
rash. The results demonstrated the clinical efficacy, incidence of
adverse events, time to resolution of diaper rash, hospitalization
duration and mean hospitalization cost. The best efficacy, lowest
incidence of adverse events, shortest time to resolution of diaper
rash and hospitalization duration as well as lowest mean
hospitalization cost were observed in the group with hydrocolloid
dressings. Therefore, the efficacy of hydrocolloid dressings in the
treatment of diaper rash was better than mupirocin plaster and
pearl powder combined with zinc oxide plaster.
Infant diaper rash, especially neonatal diaper rash,
may cause pain of infants and increase the burden of nurses.
Nursing should be enhanced for infant diaper rash, otherwise, it
would cause damage or delay healing time, or even induce secondary
infection or erosion (17,18). However, the clinical nursing of
infant diaper rash is difficult. Jing and Xia (19) used moist expose burn ointment to
treat infant diaper rash and obtained good efficacy. Previous
studies summarized the nursing of neonatal buttock erythema and
suggested the importance of frequent cleaning and urination, pure
cotton diapers and breast feeding (20,21).
In the present study, the nursing staff performed
individualized nursing during the treatment of diaper rash with
hydrocolloid dressings in group A. The results showed that the
satisfaction rate of nursing in group A parents was significantly
better than those in groups B and C (P<0.05). This result
indicated that individualized nursing during the treatment with
hydrocolloid dressings was able to relieve infant discomfort
effectively, promote early recovery, improve nursing quality and
achieve parent satisfaction.
Our experience indicated that improvement of nursing
quality and skills, and innovation of nurses were beneficial to the
clinical application of hydrocolloid dressings in the prevention
and treatment of infant diaper rash. Individualized nursing, which
was centered on patients, has been gaining interest recently.
Individualized nursing requires higher quality of nursing staff and
nursing skills. Thus, hospitals should provide more training for
nursing skills, improve comprehensive quality of nursing skills,
and improve nursing quality. Hospitals may conduct seminars on
nursing skills periodically, encourage nurses to communicate
experiences and share precautions and encourage parents to provide
advice on clinical nursing. Nurse-patient harmony is crucial for
individualized nursing. The parents of infants with diaper rash can
be anxious or depressed and nurse-patient disharmony may cause
medical disputes. Therefore, nurses should work in patient-oriented
manner, explain the disease to parents patiently, relieve negative
sentiment of parents, reduce unnecessary medical disputes and
promote nurse-patient harmony (22).
In conclusion, it is crucial to identify the
cause(s) for infant diaper rash, provide treatment and appropriate
nursing measures, to prevent diaper rash from recurring.
Hydrocolloid dressings, combined with individualized nursing, are
an effective treatment for infant diaper rash and worthy of future
clinical application.
References
|
1
|
Adib-Hajbaghery M, Mahmoudi M and
Mashaiekhi M: Shampoo-clay heals diaper rash faster than calendula
officinalis. Nurs Midwifery Stud. 3:e14180. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gaunder BN and Plummer E: Diaper rash:
Managing and controlling a common problem in infants and toddlers.
J Pediatr Health Care. 1:26–34. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shimizu M, Sakai S, Tatekawa Y, Ishikawa
S, Miyamoto M and Yachie A: An infant with PELVIS (perineal
hemangioma, external genital malformations, lipomyelomeningocele,
vesicorenal abnormalities, imperforate anus, and skin tag) syndrome
misdiagnosed as diaper rash. J Pediatr. 165:6342014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Umachitra G: Disposable baby diaper - a
threat to the health and environment. J Environ Sci Eng.
54:447–452. 2012.PubMed/NCBI
|
|
5
|
Mohamadi J, Motaghi M, Panahi J, Havasian
MR, Delpisheh A, Azizian M and Pakzad I: Anti-fungal resistance in
candida isolated from oral and diaper rash candidiasis in neonates.
Bioinformation. 10:667–670. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shin HT: Diagnosis and management of
diaper dermatitis. Pediatr Clin North Am. 61:367–382. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li CH, Zhu ZH and Dai YH: Diaper
dermatitis: A survey of risk factors for children aged 1–24 months
in China. J Int Med Res. 40:1752–1760. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ratliff C and Dixon M: Treatment of
incontinence-associated dermatitis (diaper rash) in a neonatal
unit. J Wound Ostomy Continence Nurs. 34:158–161; discussion
161–162. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mak SS, Molassiotis A, Wan WM, Lee IY and
Chan ES: The effects of hydrocolloid dressing and gentian violet on
radiation- induced moist desquamation wound healing. Cancer Nurs.
23:220–229. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Martin FT, O'Sullivan JB, Regan PJ, McCann
J and Kelly JL: Hydrocolloid dressing in pediatric burns may
decrease operative intervention rates. J Pediatr Surg. 45:600–605.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Block SL: Perianal dermatitis: Much more
than just a diaper rash. Pediatr Ann. 42:12–14. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Levy M: Diaper rash syndrome or
dermatitis. Cutis 67 (Suppl 5). 37–38. 2001.
|
|
13
|
Baldwin S, Odio MR, Haines SL, O'Connor
RJ, Englehart JS and Lane AT: Skin benefits from continuous topical
administration of a zinc oxide/petrolatum formulation by a novel
disposable diaper. J Eur Acad Dermatol Venereol 15 (Suppl 1). 5–11.
2001. View Article : Google Scholar
|
|
14
|
Zhang Y: Clinical application of Mupirocin
plaster in the treatment of pediatric diaper rash. Shanxi J Med.
42:2692013.(In Chinese).
|
|
15
|
Tan F, Wang K and Huang Z: The application
of hydrocolloid dressings in the nursing of pressure sores. Nurs J
PLA. 28:41–42. 2011.
|
|
16
|
Michel JM, Couilliet D, Bleicher R, Bloch
B, Bochaton C and Groell S: Membres Du Groupe Plaies et
Cicatrisation Des Hôpitaux Civils de Colmar: Hydrocolloid
dressings. Ann Dermatol Venereol. 129:1326–1327. 2002.(In French).
PubMed/NCBI
|
|
17
|
Lohmann I: Guidelines for treatment and
prevention of diaper rash. Kinderkrankenschwester. 24:481–482.
2005.(In German). PubMed/NCBI
|
|
18
|
Ying L: Sesame oil in the treatment of
infant diaper rash. Nurs Res. 24:5672010.
|
|
19
|
Jing L and Xia L: The treatment and
nursing of 136 cases of infant buttock erythema. Chinese J Misdiag.
10:72352010.(In Chinese).
|
|
20
|
Lin R: Clinical nursing of neonatal
buttock erythema. Adv Med. 5:2732015.(In Chinese).
|
|
21
|
Wan H: The efficacy of Kanghuier
transparent tape in severe neonatal buttock erythema. Chinese J
Prac Nurs. 31:662015.(In Chinese).
|
|
22
|
Yuan Y and Li X: The effect of delicate
nursing in neonatal diaper rash. Chinese Contemp Med. 21:121–122.
2014.(In Chinese).
|