Introduction
Tuberculous meningitis (TBM) is the most lethal form
of tuberculosis. A higher proportion of sufferers succumb to
mortality as a result of TBM compared with any other form of
tuberculosis (1). Rapid diagnosis
and early treatment should enable the mortality to be reduced. The
ideal tuberculosis screening test should be cost-effective, robust
and easy to perform, require little infrastructure or reagents and
provide results within a short span of time (2). Of the current diagnostic methods, smear
microscopy remains the most convenient gold standard for detecting
acid-fast bacilli (AFB), especially in developing countries
(3). An international TBM workshop
has reported a definite diagnosis criteria for TBM, which is the
detection of AFB in the cerebrospinal fluid (CSF) (4). However, the sensitivity of conventional
Ziehl-Neelsen (Z-N) staining for CSF specimens is rarely >60%
(5–10). Modified Z-N staining is advocated as
a good technique with high sensitivity and specificity (6). However, a mycobacterium is thin with an
approximate length of 1–4 µm, and the density of mycobacteria in
the CSF is low (11). Typically, ≥5
min is required for the reading of a negative smear with light
microscopy (12), and further time
is required to examine all the visual fields, which increases the
workload of the microscopist. Therefore, rapid and simple diagnosis
methods are urgently required for the diagnosis of TBM.
In the present study, two observational methods were
employed for modified Z-N staining in the same smear. The smears
were firstly observed under transmitted light, and then observed by
fluorescence directly, without auramine O or auramine-rhodamine.
The aim of the present study was to compare the practicality of the
two observational methods and provide a more effective method for
the diagnosis of TBM.
Materials and methods
Subjects
Ethical approval for the present study was granted
by the Research Ethics Committees of the Second Hospital of Hebei
Medical University (Shijiazhuang, China), and written informed
consent was obtained from all patients or their direct relatives. A
total of 155 patients from the Second Hospital of Hebei Medical
University were enrolled in the study, and 223 CSF specimens were
collected from them between March 2011 and March 2013. Among the
enrolled patients, 99 patients with 167 specimens were clinically
diagnosed with TBM according to the uniform case definition for use
in clinical research (4). A
definitive diagnosis of TBM was made if there was evidence of AFB
in the CSF smear, culture or on histological specimens from the
brain or spinal cord. According to the point-scoring system
reported by a previous study (4), a
probable diagnosis was established if the total score was >10
points and no imaging data was available for patients, or >12
points if imaging was used. A possible diagnosis was made on the
basis of scores between 6 and 9 points without imaging or between 6
and 11 points with imaging. Patients were excluded if their
diagnostic score was <6. The patients were classified as
definite, probable and possible TBM and 56 patients with 56 samples
in which CSF was found to be the pathogen served as negative
controls. Meningeal carcinomatosis was confirmed according to the
detection of malignant cells from the CSF. Cryptococcal meningitis
was confirmed according to the detection of Cryptococcus
neoformans or culture isolation of Cryptococcus
neoformans from CSF. Viral encephalitis was confirmed according
to etiological diagnosis (CSF had a positive antigen screening).
Leukemia with central nervous system involvement was confirmed by
the detection of leukemia cells in CSF. Purulent meningitis was
identified through the culturing of CSF and neurocysticercosis was
diagnosed based upon clinical characteristics, imaging findings and
histological changes.
In order to analyze the changes of the positive rate
of modified Z-N staining over time, all patients were classified
into two stages according to the duration of symptoms prior to
admission to the Second Hospital of Hebei Medical University (stage
1, <1 month prior to admission to the hospital; stage 2, ≥1
month prior to admission to the hospital).
Modified Z-N staining and GeneXpert
test
Standard procedures were performed upon each of the
CSF smears: A poly-l-lysine-coated slide was used to collect the
cells in 0.5 ml CSF specimen by centrifugation at 150 × g for 5
min, followed by air drying and fixation with 4% paraformaldehyde
(pH 7.4) for 10 min. The smears were then subjected to Z-N staining
subsequent to permeabilization with 0.3% Triton X-100 (Fuzhou
Maixin Biotechnology Development Co., Ltd., Fuzhou, China) for 30
min. The smears were flooded with carbol fuchsin solution (Shanghai
Sangon Biological Engineering Co., Ltd., Shanghai, China) for 20
min, then rinsed with sterile water, decolorized twice with
acid-alcohol for 2 min, then rinsed with sterile water,
counterstained with methylene blue (Shanghai Sangon Biological
Engineering Co., Ltd.) for 2 min, rinsed with sterile water and
allowed to air dry. The GeneXpert test was performed to detect TBM
according to the reported method (13).
Microscopic observation
The well-stained smears of each CSF specimen were
observed successively using an Olympus BX-51 light microscope
(Olympus Corporation, Tokyo, Japan) under transmitted light
(magnification, ×1,000) and under fluorescence with the
green-excitation wavelength (546–590 nm; magnification, ×1,000).
AFB were observed as red, thin and slightly curved structures under
transmitted light. Fuchsin-stained AFB were also directly
detectable by green-excitation wavelength under a fluorescent
microscope, and orange-red emission could be observed without the
use of a fluorescent dye, for example, auramine O or
auramine-rhodamine.
Recording and reporting of
results
The results were reported according to the Revised
National Tuberculosis Control Programme guidelines (14). All smears were read and classified as
positive or negative by two types of observational methods. A
single acid-fast bacillus was considered as a cutoff point for a
positive result. For each smear, 100 fields were examined by two
experienced observers prior to declaring a smear negative or
positive.
Statistical analysis
SPSS statistical software (version 14.0; SPSS, Inc.,
Chicago, IL, USA was employed for statistical analysis. Subsequent
to reading of the smears under transmitted light and fluorescence,
the results were compared through use the two types of
observational methods. The χ2 test was used to compare
the detection rate of the two methods. P<0.05 was considered to
indicate a statistically significant difference.
Results
Characteristics of patients
Twenty-seven definitive TBM cases with 52 smears
were identified, among which 15 CSF samples tested positive by
isolation of the organism from culture, 19 CSF samples tested
positive through the use of conventional Z-N staining and 22 CSF
samples tested positive by GeneXpert. In addition, there were 22
probable TBM cases with 39 smears and 50 possible TBM cases with 76
smears. Among the 99 patients with definite, probable or possible
TBM, 68 patients were classified as stage 1, and the remaining 31
patients were classified as stage 2. In the 56 non-tuberculous
control cases, there were 17 cases of meningeal carcinomatosis, 10
cases of purulent meningitis, 6 cases of cryptococcal meningitis, 8
cases of leukemia with central nervous system involvement, 4 cases
of neurocysticercosis cases and 11 cases of viral encephalitis.
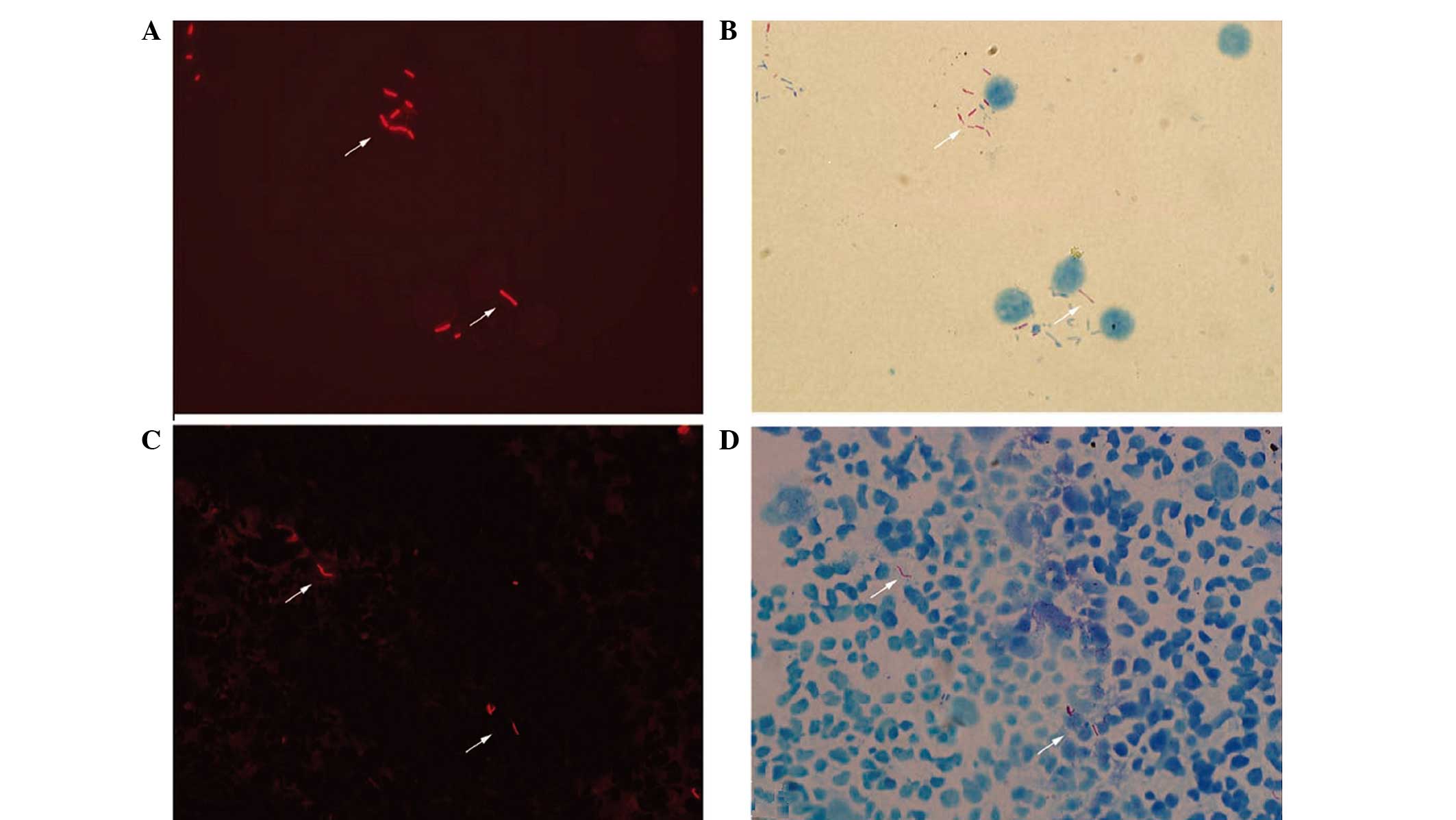
Micrographs of AFB obtained with two
observational methods
The fuchsin-stained AFB revealed bright orange-red
fluorescing rods under fluorescence or red, lightly curved rods
under transmitted light (Fig. 1).
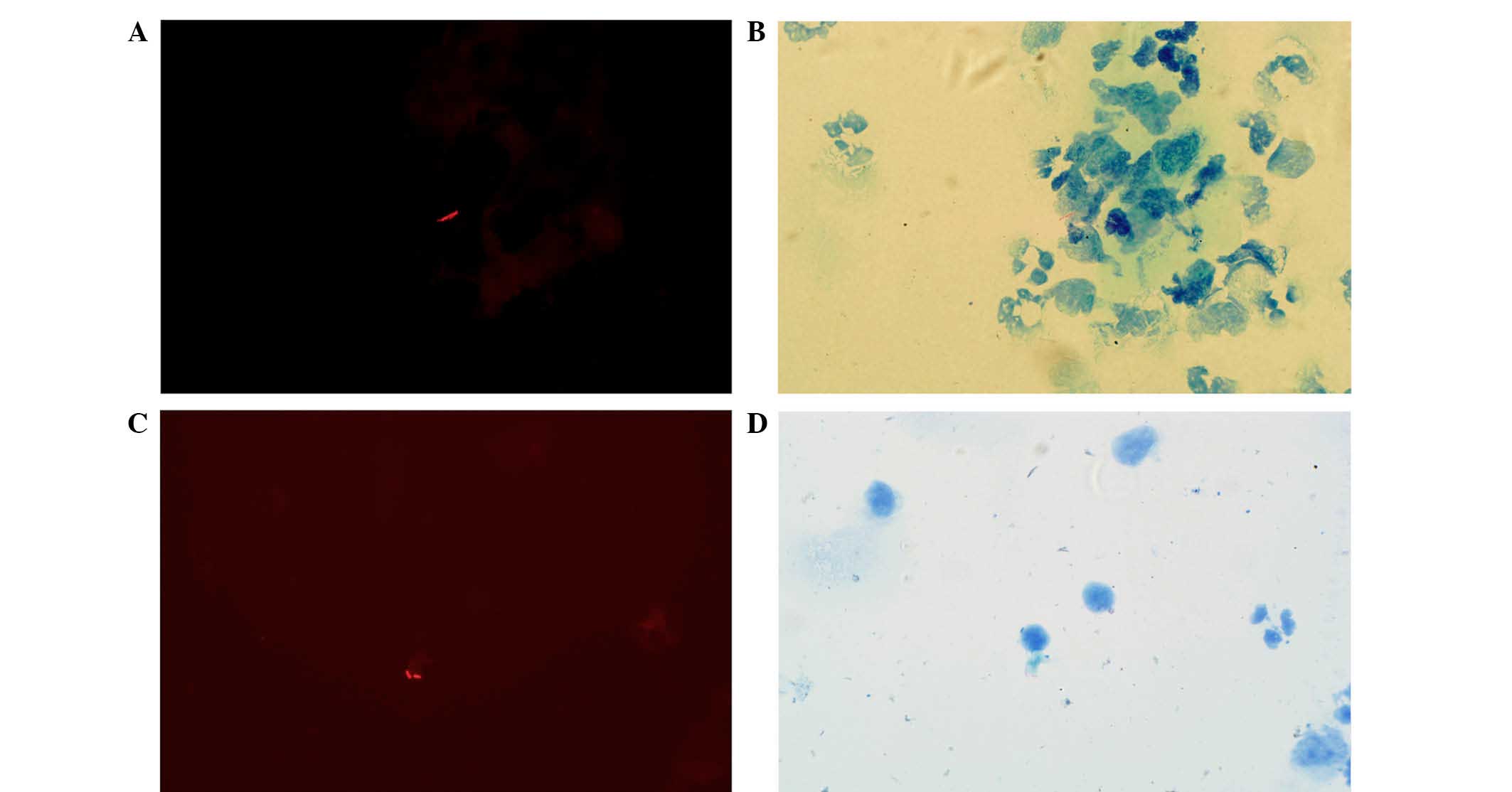
The shapes of the AFB were diverse and appeared thin and slightly
curved prior to treatment (Fig. 2A and
B), however, they became shorter and thicker following
treatment (Fig. 2C and D). AFB were
clearly observed within the immune cells, including neutrophils,
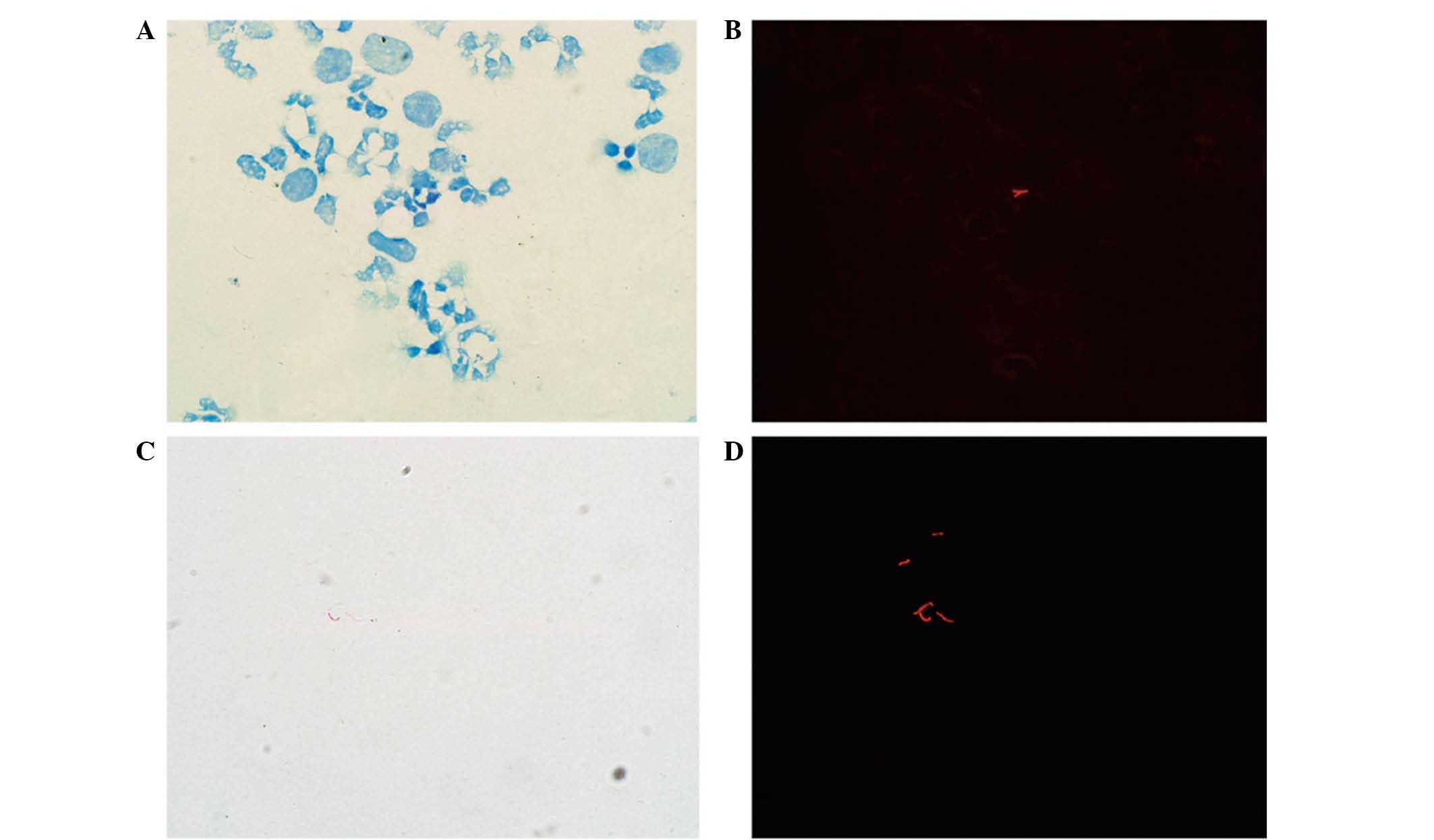
monocytes and lymphocytes. Within the same microscopic field, a
greater number of AFB were observed using fluorescence compared
with transmitted light, and AFB that were not visible under
transmitted light were detectable using fluorescence (Fig. 3).
Performance of fluorescence microscopy
and light microscopy
A total of 52 CSF samples were identified by the
gold standard method, smear microscopy. The number of CSF samples
that tested positive under transmitted light was 44, while 50
tested positive under fluorescence. Hence, the sensitivity of
fluorescence microscopy was 96.2%, whilst that of light microscopy
was 84.6% (P<0.05). In the negative control group, 6 samples
tested positive by fluorescence and light microscopy, so the
positive predictive value of fluorescence microscopy was 89.3% and
of light microscopy was 88.0%, and the specificities of
fluorescence microscopy and light microscopy were 89.3%. The
negative predictive value of fluorescence microscopy was 96.2% and
of light microscopy was 86.2%. A comparison of fluorescence
microscopy observations and light microscopy observations for the
different groups are summarized in Table
I. When the results for either patients or samples were
analyzed, a statistically significant difference (P<0.05) was
identified in the positive rate of Z-N staining between
fluorescence microscopy and light microscopy. When a sample
analysis was conducted, the positive rate was 57.5% with light
microscopy observation and 73.1% with fluorescence microscopy
observation (P<0.05). When a patient analysis was conducted,
light microscopy observations indicated a positivity of 82.8%,
whilst fluorescence microscopy observations revealed a positivity
of 90.9% (P<0.05).
 | Table I.Evaluation of the two observational
methods in each diagnostic group. |
Table I.
Evaluation of the two observational
methods in each diagnostic group.
|
|
|
| Positive results, n
(%) |
|---|
|
|
|
|
|
|---|
| Analysis type | Group | N | Fluorescence
microscopy | Light microscopy |
|---|
| Patients | Definite | 27 | 27 (100) | 27 (100) |
|
| Probable | 22 | 17 (77.3) | 11 (50.0) |
|
| Possible | 50 | 46 (92.0) | 44 (88.0) |
|
| Control | 56 | 6 (10.7) | 6 (10.7) |
| Sample | Definite | 52 | 41 (78.8) | 35 (67.3) |
|
| Probable | 39 | 28 (71.8) | 16 (41.0) |
|
| Possible | 76 | 53 (69.7) | 45 (59.2) |
|
| Control | 56 | 6 (10.7) | 6 (10.7) |
Comparison of disease duration prior
to hospitalization and positive rate between the two observational
methods
The positive rate of samples at stage 1 was 86.8%
(59/68) by fluorescence microscopy observation, and 95.6% (65/68)
by fluorescence microscopy observation. At stage 2, the positive
rate of fluorescence microscopy and light microscopy observation
was 77.4% (24/31) and 77.4% (24/31), respectively (Table II). The positive rate between
fluorescence microscopy and light microscopy was significantly
different at stage 1 (P<0.05). There was no statistically
significant difference between the two methods for the diagnosis of
TBM at stage 2 (P>0.05). The positive rate of fluorescence
microscopy observation between stages 1 and 2 was also
significantly different (P<0.05).
 | Table II.Comparison of positive rates of
tuberculous meningitis diagnosis for the two observational methods
according to disease duration prior to hospitalization. |
Table II.
Comparison of positive rates of
tuberculous meningitis diagnosis for the two observational methods
according to disease duration prior to hospitalization.
|
| No. of samples |
|---|
|
|
|
|---|
| Disease duration and
diagnosis | Light microscopy | Fluorescence
microscopy |
|---|
| <1 month |
|
|
|
Positive | 59 | 65 |
|
Negative | 9 | 3 |
| ≥1 month |
|
|
|
Positive | 24 | 24 |
|
Negative | 7 | 7 |
Comparison of positive rates of
fluorescence microscopy prior to and after treatment
Initial lumbar puncture CSF was defined as the CSF
prior to treatment, and the CSF of the patients who received
antituberculosis drugs and had <10 white blood cells/µl were
defined as CSF after treatment. Of the 77 CSF specimens classified
into the ‘prior to’ treatment group, 61 tested positive. Of the 47
post-treatment CSF specimens, 29 tested positive. The positive rate
prior to treatment was higher compared with that after treatment
(P<0.05).
Discussion
The World Health Organization estimated that, in
2010, there were 8.8 million new cases of tuberculosis of all forms
globally, and 1.45 million mortalities from the infection (14). Although TBM represents ~1% of all
cases of tuberculosis, ~50% of those affected will become severely
disabled or succumb to mortality as a result of the disease
(15). A diagnosis of TBM can be
made by various techniques, including clinical, immunological and
radiological methods, and the identification of Mycobacterium
tuberculosis in samples is the most accurate and reliable
method of diagnosis of tuberculosis (16). However, the number of effective
diagnostic techniques was limited prior to the investigation of
modified Z-N staining from China. Shapiro and Hänscheid reported
that M. tuberculosis stained too faintly by fuchsin to be
detectable under transmitted light could successfully be detected
by green-excited orange-red fluorescence (17). Cryptosporidium parvum and
Isospora belli oocysts stained with fuchsin also fluoresce
bright red under green light (546 nm) (18). However, this study was not a
case-control study, and requires repetition using a larger sample
size. Based on this, the present group performed a comparative
study to examine the reliability of combined modified Z-N staining
and fluorescence microscopy observation for AFB. A good positive
rate was achieved with fluorescence microscopy detection of
Z-N-stained AFB. The sensitivity of fluorescence microscopy
observation was 96.2% and the specificity was 89.3%. The
sensitivity of fluorescence microscopy observation was 10% higher
than that of light microscopy observation. The results are
consistent with the literature (19). We hypothesize that the combination of
modified Z-N staining and fluorescence microscopy without auramine
O is superior to using light microscopy alone.
It is generally accepted that fluorescence
microscopy has the advantages of increased sensitivity and reduced
workload (12,20–26).
However, conventional fluorescence microscopic observation of AFB
requires the use of dyes such as auramine-rhodamine or acridine,
which are relatively expensive and whose fluorescence is rapidly
quenched. Furthermore, they are toxic substances and carcinogenic.
The modified method presented in the current study involves the use
of fuchsin instead of auramine O and observed the auto-fluorescence
of fuchsin-stained AFB through a green excitation filter (546–590
nm) under a fluorescence microscope. The fluorescent contrast
caused by fuchsin-stained AFB was observed more readily compared
with the red of AFB against a blue background in light microscopy.
Furthermore, the background of stained slides under fluorescence is
brighter than under transmitted light, facilitating the focus on
and examination of smears with fewer bacilli for the laboratory
technician. The well-stained smears may be stored for an extended
duration prior to review. The examination time of fluorescence
microscopy observation was ~50% more rapid compared with light
microscopy examination, consolidating upon the results reported by
Xia et al (27). The
fuchsin-stained AFB exhibited a bright orange-red fluorescence,
clustered or diffused distribution and thin and slightly curved
bacilli. It was also observed that the AFB were markedly shorter
and thicker subsequent to antituberculosis treatment. It is
reported that bacteria are able to enter into a cell-less state
known as L-form conversion under certain conditions (28). L-forms display a variety of
morphological shapes, including bulbiform, rod-shaped bacteria and
filamentous structures. The use of isoniazide is a cause of AFB
entering into L-form (29).
In the current study, the positive rate of AFB was
higher with fluorescence microscopy compared with light microscopy,
irrespective of whether the results were analyzed according to the
number of samples or patients in each group. The positive rate in
the definite group was the highest. There was no statistically
significant difference between the probable and possible groups.
This suggested that the international TBM diagnostic criteria may
assist the optimization of the diagnostic process of TBM. Once
analysis of all patients was complete, fluorescence microscopy
observation indicated 90.9% positivity, whereas light microscopy
observation indicated 82.8% positivity. Furthermore, with the same
microscopic field, a greater number of AFB were detectable using
fluorescence compared with transmitted light, and more AFB that
were undetectable under transmitted light could be clearly seen
under fluorescence. Equivocal smears encountered with fluorescence
microscopy may then be observed under transmitted light directly.
Therefore, fluorescence microscopy may help to focus bacilli and
light microscopy may then assist in distinguishing bacilli. This is
likely to largely avoid false positive results. The combination of
the modified Z-N staining and fluorescence microscopy should
greatly improve the diagnostic value of CSF smears, particularly
those with a low density of bacilli that are likely to be missed by
light microscopy observation, and reduce the inconvenience to
microscopists. In countries with a high tuberculosis burden,
fluorescence microscopy was not previously widely used due to the
expense involved in purchasing and maintaining fluorescence
microscopy materials, which is far greater compared with that of
light microscopy. However, an evaluation in Thailand found that the
total cost of fluorescence microscopy operated in the National
Tuberculosis Reference Laboratory (NTRL) in Bangkok, Thailand, was
similar to that of light microscopy performed in the NTRL and in
four regional Thai laboratories (30). Thus, fluorescence microscopy and
light microscopy should be used in combination to improve the
detection rate. The positive rate of AFB was higher when the
analysis was conducted on the basis of patient numbers than when
analyzed according to sample numbers in the same group, suggesting
that the sensitivity will increase if the number of specimens for
each patient is increased.
In the present study, the association between
disease duration prior to hospitalization and the positive rate of
the two observational methods was observed. With the use of
fluorescence microscopy observation, a difference was observed
between stages 1 and 2, indicating the earlier the inspection, the
higher the positive rate. The positive rate was ~20% higher at
stage 1 compared with stage 2. At stage 1, 65 patients tested
positive with fluorescence microscopy observation while 59 patients
were positive with light microscopy observation. Thus, missed
diagnosis as a result of numerous false negatives was largely
avoided by fluorescence microscopy observation. Furthermore, we
hypothesize that a higher proportion of patients will be detected
earlier using the modified observational method, compared with
previous methods.
The positive rate of fluorescence microscopy was
72.2% prior to treatment compared with a 61.7% post-treatment
positive rate (P<0.05). This suggests that Z-N staining results
may be useful for predicting clinical effects. However, the present
study also observed that the post-treatment positive rate of Z-N
staining remained high. Thus, it may be speculated that the
bacteria may be dead but continue to exist in the CSF for a long
period of time. Furthermore, in a number of immunocompromised
patients, the immune function cannot be activated effectively, so
removal of the bacteria is not possible. The result of Z-N staining
may remain positive even when there are <10 white blood cells/µl
in the CSF; for such patients, an improvement of clinical
manifestations was not evident.
Overall, there are a number of advantages of this
modified technique. Firstly, the combination of the modified Z-N
staining and fluorescence microscopy is convenient and sufficiently
sensitive to examine samples for the presence of AFB rapidly,
especially for the detection of AFB in CSF. On this basis, a
greater number of AFB may be observed in a field using fluorescence
rather than transmitted light. The work efficiency of the
microscopist should be improved and the workload reduced. Secondly,
the microscopist may compare the fluorescence and transmitted light
images on the same smears simultaneously, to clarify the AFB
status. Finally, Z-N dyeing followed by fluorescence microscopy
observation is utilized instead of auramine O or rhodamine, which
will reduce the waste in the laboratory and reduce the harm to
microscopists. Thus, this method may be easily carried out in the
general laboratory.
In the present study, 6 patients in the negative
control group tested positive, including 4 patients with meningeal
carcinomatosis, 1 patient with neurocysticercosis and 1 patient
with viral encephalitis. Each of the 6 patients had a diagnostic
score of >6 according to the international TBM diagnostic
criteria, and one of the patients with meningeal carcinomatosis was
classified into the probable group. It remains uncertain as to
whether these were true- or false-positives. However, there are
reports concerning the coexistence of tuberculosis and cancer
(31,32) and the coexistence of tuberculosis and
viral encephalitis (33). Initially,
for a patient with tuberculosis, a decline in cellular immune
function creates favorable conditions for tumorigenesis. Similarly,
tumor cells are able to produce immunosuppressive factors that may
reduce the body's immune function and increase the chances of
tuberculosis (34). Secondly,
inflammation associated with infection may contribute to
carcinogenesis, and inflammation has powerful effects on tumor
development (32). Neutrophils are
the initial recruited effectors of the acute inflammatory response.
Reactive nitrogen and oxygen species released from inflammatory
cells are able to bind to DNA, inducing tumorigenesis and
metastasis (32). Thirdly, during
tissue repair in patients with pulmonary tuberculosis, there is
increased cell proliferation and angiogenesis, and the epithelium
is increasingly prone to metaplasia. Furthermore, there may be an
association between tuberculosis and cancer or tuberculosis and
viral encephalitis. However, whether the 6 patients in the control
group who tested positive actually had tuberculosis was not
determined. The clinicians did not further examine the patients
subsequent to the detection of malignant cells or etiological
diagnosis from the CSF.
In conclusion, the combination of modified Z-N
staining and fluorescence microscopy without auramine O is a
reliable alternative method for the diagnosis of tuberculous
meningitis and has many favorable attributes, and thus may be
widely used in countries with a high tuberculosis burden.
Acknowledgements
The present study was supported by the Medical
Science Research of Hebei Province, Shijiazhuang, China (grant no.
20120319).
References
|
1
|
Yu HY, Hu FS, Xiang DR and Sheng JF:
Clinical management of tuberculous meningitis: Experiences of 42
cases and literature review. Neurol Sci. 35:303–305. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Elkington PT: Tuberculosis: Time for a new
perspective? J Infect. 66:299–302. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zou Y, He J, Guo L, Bu H and Liu Y:
Prediction of cerebrospinal fluid parameters for tuberculous
meningitis. Diagn Cytopathol. 43:701–704. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Marais S, Thwaites G, Schoeman JF, Török
ME, Misra UK, Prasad K, Donald PR, Wilkinson RJ and Marais BJ:
Tuberculous meningitis: A uniform case definition for use in
clinical research. Lancet Infect Dis. 10:803–812. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Thwaites GE: Advances in the diagnosis and
treatment of tuberculous meningitis. Curr Opin Neurol. 26:295–300.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen P, Shi M, Feng GD, Liu JY, Wang BJ,
Shi XD, Ma L, Liu XD, Yang YN, Dai W, et al: A highly efficient
Ziehl-Neelsen stain: Identifying de novo intracellular
Mycobacterium tuberculosis and improving detection of extracellular
M. tuberculosis in cerebrospinal fluid. J Clin Microbiol.
50:1166–1170. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Feng GD, Shi M, Ma L, Chen P, Wang BJ,
Zhang M, Chang XL, Su XC, Yang YN, Fan XH, et al: Diagnostic
accuracy of intracellular Mycobacterium tuberculosis detection for
tuberculous meningitis. Am J Respir Crit Care Med. 189:475–481.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ulrichs T, Lefmann M, Reich M, Morawietz
L, Roth A, Brinkmann V, Kosmiadi GA, Seiler P, Aichele P, Hahn H,
et al: Modified immunohistological staining allows detection of
Ziehl-Neelsen-negative Mycobacterium tuberculosis organisms and
their precise localization in human tissue. J Pathol. 205:633–640.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yeager H Jr, Lacy J, Smith LR and
LeMaistre CA: Quantitative studies of mycobacterial populations in
sputum and saliva. Am Rev Respir Dis. 95:998–1004. 1967.PubMed/NCBI
|
|
10
|
Thwaites GE, Chau TT and Farrar JJ:
Improving the bacteriological diagnosis of tuberculous meningitis.
J Clin Microbiol. 42:378–379. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Radhakrishnan VV and Mathai A: Correlation
between the isolation of Mycobacterium tuberculosis and estimation
of mycobacterial antigen in cisternal, ventricular and lumbar
cerebrospinal fluids of patients with tuberculous meningitis.
Indian J Pathol Microbiol. 36:341–347. 1993.PubMed/NCBI
|
|
12
|
Marais BJ, Brittle W, Painczyk K,
Hesseling AC, Beyers N, Wasserman E, van Soolingen D and Warren RM:
Use of light-emitting diode fluorescence microscopy to detect
acid-fast bacilli in sputum. Clin Infect Dis. 47:203–207. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nhu NT, Heemskerk D, Thu do DA, Chau TT,
Mai NT, Nghia HD, Loc PP, Ha DT, Merson L, Thinh TT, et al:
Evaluation of GeneXpert MTB/RIF for diagnosis of tuberculous
meningitis. J Clin Microbiol. 52:226–233. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
World Health Organization, . Global
Tuberculosis Control: WHO Report 2010. World Health Organization;
Geneva: 2010
|
|
15
|
Thwaites GE, van Toorn R and Schoeman J:
Tuberculous meningitis: More questions, still too few answers.
Lancet Neurlo. 12:999–1010. 2013. View Article : Google Scholar
|
|
16
|
Zakham F, Akrim M, El Mzibri M, Benjouad
A, El Aouad R and Ennaji MM: Rapid screening and diagnosis of
tuberculosis: A real challenge for the mycobacteriologist. Cell Mol
Biol (Noisy-le-grand). 58:(Suppl). S1632–S1640. 2012.
|
|
17
|
Shapiro HM and Hänscheid T: Fuchsin
fluorescence in Mycobacterium tuberculosis: The Ziehl-Neelsen stain
in a new light. J Microbiol Methods. 74:119–120. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Varea M, Clavel A, Doiz O, Castillo FJ,
Rubio MC and Gómez-Lus R: Fuchsin fluorescence and autofluorescence
in Cryptosporidium, Isospora and Cyclospora oocysts. Int J
Parasitol. 28:1881–1883. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Steingart KR, Henry M, Ng V, Hopewell PC,
Ramsay A, Cunningham J, Urbanczik R, Perkins M, Aziz MA and Pai M:
Fluorescence versus conventional sputum smear microscopy for
tuberculosis: A systematic review. Lancet Infect Dis. 6:570–581.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kivihya-Ndugga LE, van Cleeff MR, Githui
WA, Nganga LW, Kibuga DK, Odhiambo JA and Klatser PR: A
comprehensive comparison of Ziehl-Neelsen and fluorescence
microscopy for the diagnosis of tuberculosis in a resource-poor
urban setting. Int J Tuberc Lung Dis. 7:1163–1171. 2003.PubMed/NCBI
|
|
21
|
Ulukanligil M, Aslan G and Tasçi S: A
comparative study on the different staining methods and number of
specimens for the detection of acid fast bacilli. Mem Inst Oswaldo
Cruz. 95:855–858. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hänscheid T: The future looks bright:
Low-cost fluorescent microscopes for detection of Mycobacterium
tuberculosis and Coccidiae. Trans R Soc Trop Med Hyg. 102:520–521.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lehman LG, Ngapmen Yamadji AL, Ngo Sack F
and Bilong Bilong CF: The CyScope® fluorescence
microscope, a reliable tool for tuberculosis diagnosis in
resource-limited settings. Am J Trop Med Hyg. 83:906–908. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Habtamu M, van den Boogaard J, Ndaro A,
Buretta R, Irongo CF, Lega DA, Nyombi BM and Kibiki GS:
Light-emitting diode with various sputum smear preparation
techniques to diagnose tuberculosis. Int J Tuberc Lung Dis.
16:402–407. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ba F and Rieder HL: A comparison of
fluorescence microscopy with the Ziehl-Neelsen technique in the
examination of sputum for acid-fast bacilli. Int J Tuberc Lung Dis.
3:1101–1105. 1999.PubMed/NCBI
|
|
26
|
Prasanthi K and Kumari AR: Efficacy of
fluorochrome stain in the diagnosis of pulmonary tuberculosis
co-infected with HIV. Indian J Med Microbiol. 23:179–181. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Xia H, Song YY, Zhao B, Kam KM, O'Brien
RJ, Zhang ZY, Sohn H, Wang W and Zhao YL: Multicentre evaluation of
Ziehl-Neelsen and light-emitting diode fluorescence microscopy in
China. Int J Tuberc Lung Dis. 17:107–112. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Willett HP and Thacore H: Formation of
spheroplasts of Mycobacterium tuberculosis by lysozyme in
combination with certain enzymes of rabbit peritoneal monocytes.
Can J Microbiol. 13:481–487. 1967. View
Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ye HP and Xu HP: Research about L-form of
Mycobacterium tuberculosis. Jiang Xi Zhong Yi Xue Yuan Xue Bao.
12:92–93. 2000.(In Chinese).
|
|
30
|
Sohn H, Sinthuwattanawibool C, Rienthong S
and Varma JK: Fluorescence microscopy is less expensive than
Ziehl-Neelsen microscopy in Thailand. Int J Tuberc Lung Dis.
13:266–268. 2009.PubMed/NCBI
|
|
31
|
Silva DR, Valentini DF Jr, Müller AM, de
Almeida CP and Pde T Dalcin: Pulmonary tuberculosis and lung
cancer: Simultaneous and sequential occurrence. J Bras Pneumol.
39:484–489. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Coussens LM and Werb Z: Inflammation and
cancer. Nature. 420:860–867. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Aibar-Arregui MA, de Escalante-Yangüela B,
Tejero-Juste C and Martín-Fortea MP: Mixed meningoencephalitis
caused by Mycobacterium tuberculosis and varicella zoster virus.
Rev Neurol. 48:91–93. 2009.(In Spanish). PubMed/NCBI
|
|
34
|
Cicenas S and Vencevicius V: Lung cancer
in patients with tuberculosis. World J Surg Oncol. 5:222007.
View Article : Google Scholar : PubMed/NCBI
|