Introduction
Chemotherapy-induced peripheral neuropathy (CIPN) is
a common, dose-limiting adverse drug reaction in cancer treatment
(1), which primarily presents as
varying degrees of motor and sensory deficits, as well as autonomic
dysfunction. Currently, paclitaxel, cisplatin, and vinblastine are
the most commonly prescribed anti-cancer chemotherapy drugs
(2). Unfortunately, these drugs all
produce treatment-limiting peripheral neuropathy, for which there
is no reliable clinical intervention. The primary treatment of CIPN
is to reduce the chemotherapy dose and to extend the interval
between treatments, or cease treatment completely (3). However, this is not an optimal choice
for the long-term prognosis of the patient.
Acetyl-L-carnitine (ALC) is a nutrient supplement
with the ability to stimulate the expression of nerve growth factor
receptor, strengthen the tubulin of nerve cells and prevent
cytoskeletal damage and cystic nerve fibrosis, as well as improve
sensory nerve conduction (4,5). In addition, numerous basic and clinical
studies have demonstrated that ALC alleviates CIPN without reducing
the antitumor drug activity (6–8).
Sigma Tau Pharmaceuticals, Inc. developed
levocarnitine acetate hydrochloride gastro-resistant tablets
(Nicetile®), which is an oral drug that first appeared
on the Italian market in July 1984, with peripheral nerve or nerve
root mechanisms of action and inflammatory injury as the registered
indication. However, the effects of Nicetile® in Chinese
individuals with CIPN remains to be elucidated. The aim of the
present study was to investigate the efficacy and safety of
levocarnitine acetate hydrochloride gastro-resistant tablets on
CIPN in a large Chinese population.
Materials and methods
Study design and approval
This study was a multicenter, randomized,
double-blind, and placebo-controlled phase II clinical trial. It
was approved by the Chinese State Food and Drug Administration
(approval no. 2007L03540). The clinical trial registration number
is NCT01526564. The clinical study was carried out in accordance
with The Code of Ethics of the World Medical Association
(Declaration of Helsinki) for experiments involving humans. In
addition, informed consent was obtained from all participants
involved in this study.
Eligible patients were aged 18–75 years without
gender limitation. Eligibility criteria included: Grade ≥3
neuropathy, as determined by NCI-CTC criteria version 3.0 (9), while receiving paclitaxel, cisplatin or
vinblastine treatment, and/or grade ≥2 neuropathy persisting for at
least one month after the discontinuation of either drug, and
neurotoxicity for <6 months; at least one abnormality on
electrophysiological examination; Karnofsky physical score (KPS) of
≥60; absolute neutrophil count of ≥1.5×109/l, hemoglobin
count of ≥80 g/l, platelet count of ≥75×109/l, total
bilirubin counts of 1.5-fold less than normal value,
glutamic-pyruvic transaminase (GPT/ALT) and glutamic-oxalacetic
transaminease (GOT/AST) no more than 2.5-fold greater than the
normal value; normal blood urea nitrogen, serum creatinine and
electrocardiogram (ECG) findings. During the study, the use of
steroids, analgesic or neuroprotectant drugs was not permitted.
Patients were enrolled after providing written informed
consent.
Exclusion criteria included: Neuropathy caused by
other antineoplastic treatment except paclitaxel, cisplatin or
vinblastine; pre-existing diabetes mellitus and/or neuropathy
caused by vitamin deficiency, infection, trauma, poisoning,
oppression, ischemia, metabolic disorders; genetic neuropathy
and/or peripheral sensory nerve dysfunction due to central nervous
system lesions; use of other drug therapy for neuropathy in the
last 30 days (such as nerve growth factor, amifostine reduced
glutathione, vitamin E or B, glucocorticoids, ethosuximide,
carbamazepine, gabapentin, sodium thiosulfate, glutamic acid,
lamotrigine, α-fatty acid, lithium salt, lithium salt or magnesium
salt); participation in other clinical trials in the past 30 days;
out of control clinical problems (such as serious mental, nerve,
cardiovascular and/or respiratory system disease); pregnant or
lactating women; and poor compliance.
During the trial, patients were withdrawn if serious
adverse events occurred, and/or the patient became pregnant.
Patients
A total of 240 patients met the criteria and were
recruited for the present study at Shanghai Changzheng Hospital
(Shanghai, China) between September 4, 2010 and November 7, 2013.
All patients were treated with at least one type of taxoid, either
satraplatin (80 mg/m2; GPC Biotech, Munich, Germany) or
vincristine (0.05 mg/kg2; Pharmachemic Hisun, Zhejiang,
China). Their peripheral sensory neuropathy grading following
chemotherapy was ≥ grade 3 or 2, lasted for ≥ 1 month, and the
course of neuropathy was ≤6 months. The patient either no longer
required chemotherapy or did not choose to undergo chemotherapy.
Each patient was administered one ALC hydrochloride enteric-coated
tablet (oral administration; 500 mg/tablet, 2 tablets/time) three
times a day for eight consecutive weeks. The patients of the
control group received a placebo (lactose, 500 mg/tablet, 2
tablets/time) in the same manner. Patients were instructed that the
interval between doses should be at ≥4 h and were monitored at week
4, 8 and 12. Since drug treatment ceased after week 8, the results
obtained after week 12 represented the long-term effects of ALC
intervention.
Safety analysis set (SS) was an analysis in those
who received at least one dose of the investigational drug and
safety valuation. Full analysis set (FAS) was analysis in which
patients are included in the group to which they were randomized
irrespective of compliance, administrative errors (such as error in
eligibility), or other protocol deviations. Per protocol set (PPS)
was an analysis in which patients are included in the group
corresponding to the treatment they actually received. Patient
compliance and “switchovers” were considered in the analysis.
Primary endpoint
The primary endpoint of the study was to demonstrate
an improvement of ≥1 grade in neurotoxicity, as determined by
NCI-CTC criteria (version 3.0) at week 8 of ALC administration
(9).
Secondary endpoints
Prior to ALC administration at 4, 8 and 12 weeks,
electrophysiological examinations were carried out at each time
point, which included examination of the nerves (handedness, median
nerve, ulnar nerve, common peroneal nerve, tibial nerve,
superficial peroneal nerve and sural nerve). Three neural
electricity experts compared the electrophysiology examination
results at the 8th week (including nerve conductive velocity,
latency period and amplitude) to the results obtained prior to ALC
administration. The unified curative effect standard to centralized
assess was followed and the evaluation results were recorded and
signed by the experts. The results were categorized into improved,
effective improved and no change, based on the efficient rate which
was calculated by the following formula: Efficient rate = (Number
of patients that improved + Number of effective improved patients)
/ (All patients - Number of patients that could not be evaluated) ×
100%.
Evaluation of safety and efficacy
The case histories of the patients, previous
chemotherapy information, and disease and treatment histories were
recorded during screening. Prior to 4, 8, and 12 weeks of testing,
all patients underwent baseline assessment, which included
comprehensive physical examinations, laboratory examinations, and
electrophysiological and 12-lead ECG examination. The physical
examinations included the measurement of vital signs (temperature,
pulse, respiration and blood pressure), the grading of
neurotoxicity (9), cancer-associated
fatigue classification (10) and KPS
assessment (11). Laboratory
examination included a routine blood panel, liver and kidney
function (12) and fasting glucose
measurement (13). Electrophysiology
examination was performed as described and the results were
categorized into improved, effective improved and no change. During
the study, all disease factors, drug combinations and adverse
events were recorded in the case report form (CRF).
Nerve conductive velocity (NCV)
NCV was examined to evaluate the changes prior to
ALC administration and after 8 weeks of ALC administration.
Treatment was defined as effective if the NCV was improved after
ALC administration, whereas, it was defined as ineffective if the
NCV was reduced or unchanged. Effective analysis was conducted
according to the results using the following formula: Efficient
rate = number of patients effectively treated/(number of patients
that could not be evaluated) ×100%.
Statistical analysis
Statistical analysis was performed using SAS
software version 9.2 (SAS Institute, Cary, North Carolina, USA).
Independent sample t-tests or Wilcoxon tests were used to compare
continuous variables between groups, and paired t-test or Wilcoxon
tests were used for comparison within groups. For the categorical
variable analysis, a χ2 test or exact test were used for
comparisons between groups. The
Cochran-Mantel-Haenszel-χ2 test was used to analyze
ordinal categorical data. Data were presented as the mean±standard
deviation. P<0.05 was considered to indicate a significantly
significant result.
Results
Subjects
A total of 240 patients were originally eligible for
this study, although the final full study group included 239 CRF
subjects. The safety analysis set (SS) contained 236 patients, 118
in the experimental group and 118 in the control group. The full
analysis set (FAS) contained 225 patients, 109 in the experimental
group and 116 in the control group. The per-protocol set (PPS)
contained 203 patients, 95 in the experimental group and 108 in the
control group.
Primary endpoint-neurotoxicity
As shown in Table I,
in the FAS, at the 8th week of the study, ALC treatment reduced
neurotoxicity in 50.5% of the experimental patients, compared with
a 24.1% reduction in the control group. The difference between the
ALC and placebo groups was statistically significant [95%
confidence interval (CI), 14.1–38.5%; P<0.001]. The 8-week
efficacy in the PPS was 51.6% (ALC) and 23.1% (control), which was
significantly different (95% CI, 15.6–41.2%; P<0.001). The
statistical significance of these findings was maintained following
correction for the effect of different hospital centers
(P<0.001; data not shown). The reduction of neurotoxicity was
time-dependent for the patients in both treatment groups. A
comparison of the effect of ALC between the 4th, 8th, and 12th week
revealed that the improvement in neurotoxicity was significantly
different between the experimental and control group (P<0.05;
Table I). As shown in Table II, there was a observable
improvement on the 4th week, with a decrease in the number of
patients displaying grade ≥3 neuropathy, and an increase in the
number of patients displaying grade 2, although the differences
between the two groups did not reach statistical significance
(P>0.05). By the 8th week of treatment, the difference between
the experimental and control group was statistical significant
(P<0.05).
 | Table I.Peripheral sensory neurotoxicity
evaluation at each visit at weeks 4, 8 and 12. |
Table I.
Peripheral sensory neurotoxicity
evaluation at each visit at weeks 4, 8 and 12.
|
| Full analysis
set | Per-protocol set |
|---|
|
|
|
|
|---|
| Time | ALC (%) | Placebo (%) | χ2 | Pa | ALC (%) | Placebo (%) | χ2 | Pa |
|---|
| Week 4 |
|
|
Valid | 29 (26.6) | 16 (13.8) | 5.766 | 0.016 | 26 (27.4) | 14 (13.0) | 6.629 | 0.010 |
|
Invalid | 80 (73.4) | 100 (86.2) |
|
| 69 (72.6) | 94 (87.0) |
|
|
| Week 8 |
|
|
Valid | 55 (50.5) | 28 (24.1) | 16.722 | <0.001 | 49 (51.6) | 25 (23.1) | 17.636 | <0.001 |
|
Invalid | 54 (49.1) | 88 (75.9) |
|
| 46 (48.4) | 83 (76.9) |
|
|
| Week 12 |
|
|
Valid | 63 (57.8) | 46 (39.7) | 7.406 | 0.007 | 57 (60.0) | 41 (38.0) | 9.830 | 0.002 |
|
Invalid | 46 (42.2) | 70 (60.3) |
|
| 38 (40.0) | 67 (62.0) |
|
|
 | Table II.Peripheral sensory neurotoxicity
grading. |
Table II.
Peripheral sensory neurotoxicity
grading.
| CTC grade | ALC (%) | Placebo (%) | χ2 | Pa |
|---|
| FAS |
|
|
Baseline |
|
|
I | 0 (0.0) | 0 (0.0) | 1.175 | 0.278 |
|
II | 42 (38.5) | 53 (45.7) |
|
|
|
III | 67 (61.5) | 63 (54.3) |
|
|
| 4th
week |
|
|
I | 6 (5.6) | 8 (7.3) | 0.873 | 0.646 |
|
II | 61 (57.0) | 56 (50.9) |
|
|
|
III | 40 (37.4) | 46 (41.8) |
|
|
| 8th
week |
|
|
I | 27 (25.2) | 20 (18.2) | 6.242 | 0.0441 |
|
II | 54 (50.5) | 46 (41.8) |
|
|
|
III | 26 (24.3) | 44 (40.0) |
|
|
| 12th
week |
|
|
I | 37 (34.6) | 28 (25.5) | 3.7594 | 0.153 |
|
II | 48 (44.9) | 48 (43.6) |
|
|
|
III | 22 (20.6) | 34 (30.9) |
|
|
| PPS |
|
|
Baseline |
|
|
I | 0 (0.0) | 0 (0.0) | 1.910b | 0.167 |
|
II | 34 (35.8) | 49 (45.4) |
|
|
|
III | 61 (64.2) | 59 (54.6) |
|
|
| 4th
week |
|
|
I | 5 (5.3) | 8 (7.8) | 1.007b | 0.605 |
|
II | 52 (55.3) | 50 (49.0) |
|
|
|
III | 37 (39.4) | 44 (43.1) |
|
|
| 8th
week |
|
|
I | 22 (23.4) | 18 (17.6) | 5.364b | 0.068 |
|
II | 48 (51.1) | 42 (41.2) |
|
|
|
III | 24 (25.5) | 42 (41.2) |
|
|
| 12th
week |
|
|
I | 32 (34.0) | 25 (24.5) | 4.299b | 0.117 |
|
II | 43 (45.7) | 44 (43.1) |
|
|
|
III | 19 (20.2) | 33 (32.4) |
|
|
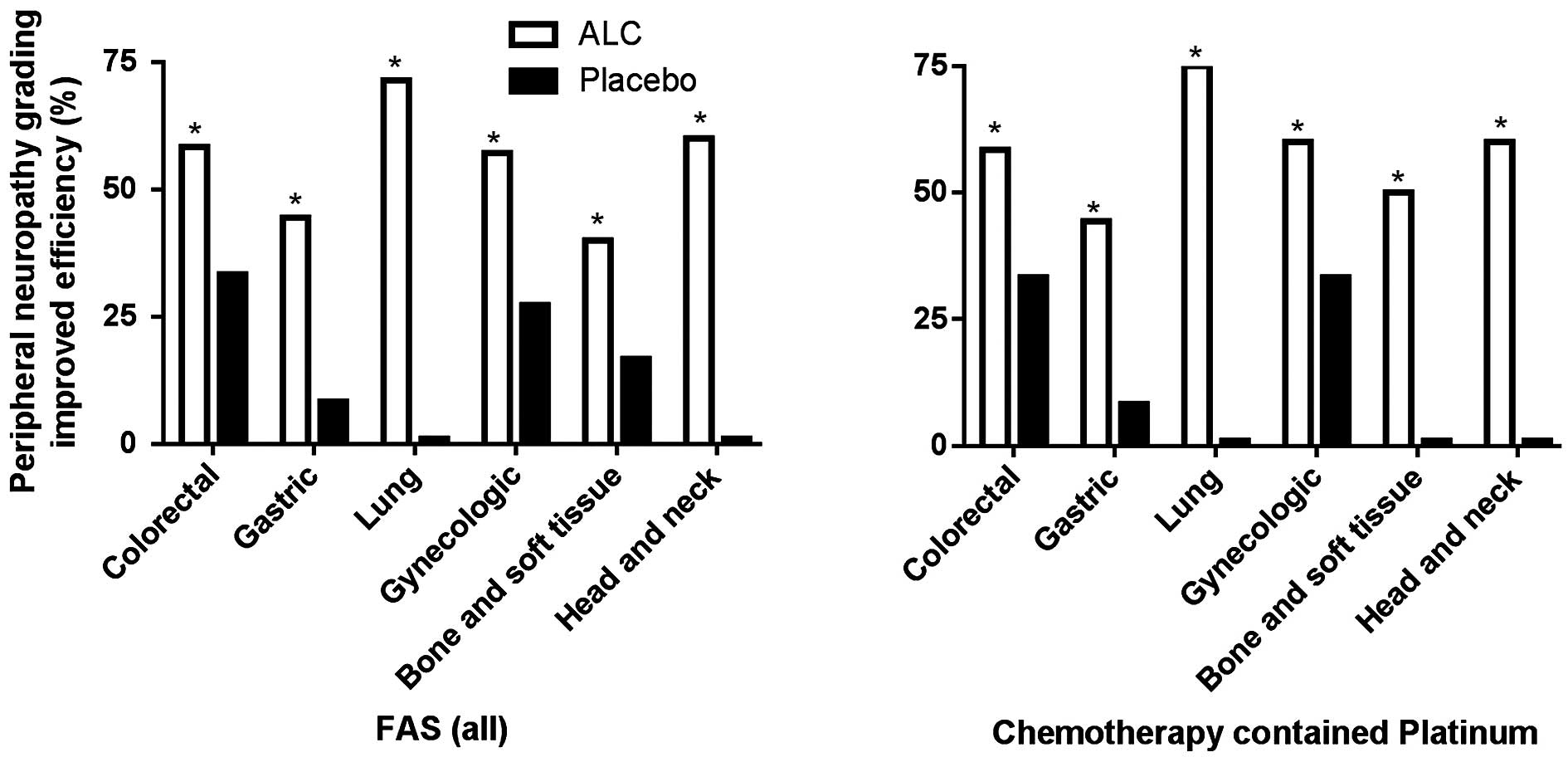
To further examine whether the efficacy of ALC was
affected by chemotherapy treatment and cancer type, the cancer type
in the treatment and placebo groups were classified prior to
comparison of ALC efficacy. In the FAS, ALC was able to
significantly improve the peripheral neuropathy grading in all
cancer types, results which were not observed in the placebo group
(P<0.05; Fig. 1). ALC's effect
was not affected by treatment with platinum-containing chemotherapy
(Fig. 1). In addition, chemotherapy
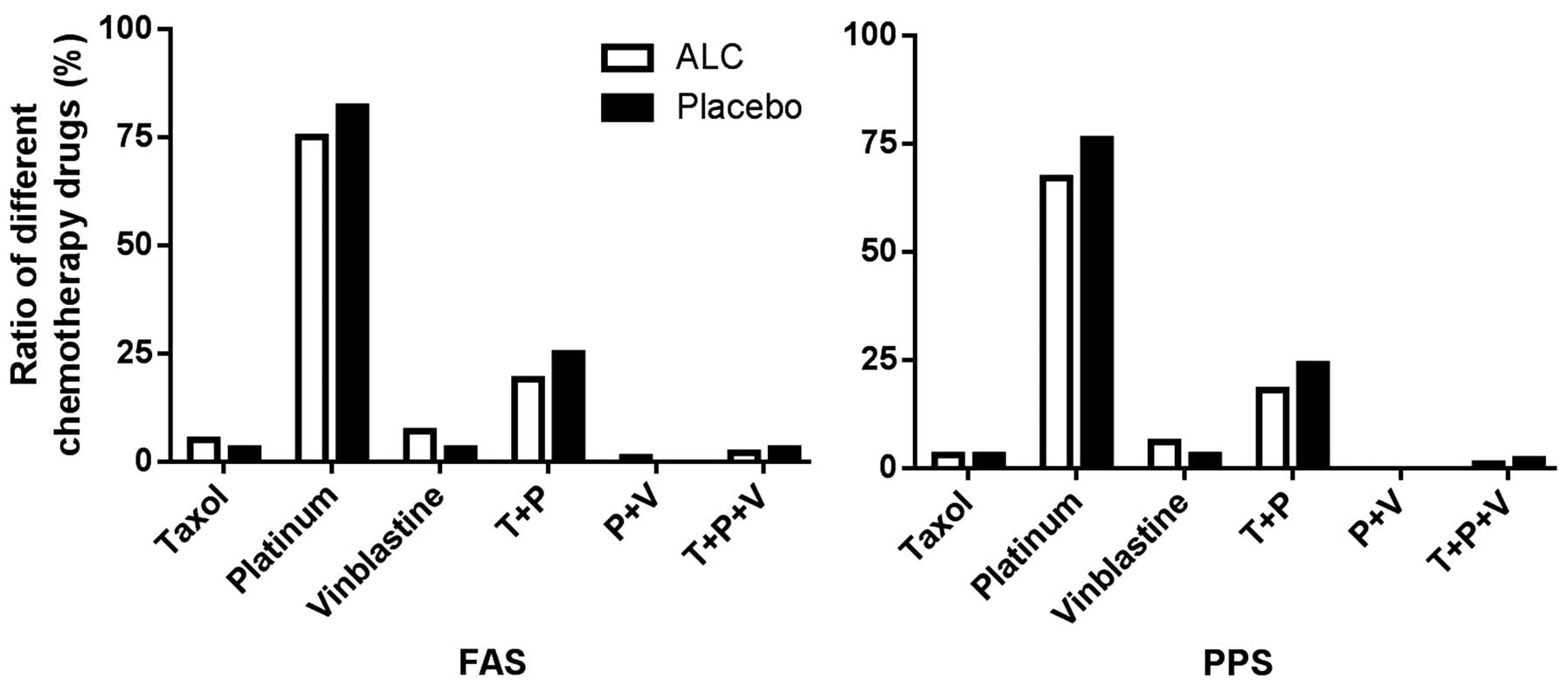
had no difference on the effect of ALC, compared with the (Fig. 2).
Secondary endpoints
Electrophysiological examination
Although the results from week 8 in the NCV test for
the median nerve, ulnar nerve, common peroneal nerve, tibial nerve,
superficial peroneal nerve and sural nerve demonstrate various
degrees of improvement compared with the baseline at week 0, only
the NCV of the sural nerve was significantly different between the
experimental and control groups (P<0.05; data not shown).
Evaluation of electrophysiology
In the FAS, ALC treatment significantly improved NCV
in the experimental group (60.7%), as compared with the control
group (56.9%; P<0.05). Similar results could be observed in the
PPS group, with a 76.8% improvement in the experimental group and a
59.3% in the control group (P<0.05; Table III).
 | Table III.Nerve electrophysiological function
(Week 8). |
Table III.
Nerve electrophysiological function
(Week 8).
|
| Full analysis
set | Per-protocol
set |
|---|
|
|
|
|
|---|
| Effect | ALC (%) | Placebo (%) | χ2 | Pa | ALC (%) | Placebo (%) | χ2 | Pa |
|---|
| Marked effect | 22 (20.2) | 17 (14.7) | 4.133 | 0.126 | 21 (22.1) | 16 (14.8) | 7.330 | 0.026 |
| Improved | 54 (49.5) | 49 (42.2) |
|
| 52 (54.7) | 48 (44.4) |
|
|
| Unchanged | 33 (30.3) | 50 (43.1) |
|
| 22 (23.2) | 44 (40.7) |
|
|
| Valid | 76 (60.7) | 66 (56.90) | 3.972 | 0.046 | 73 (76.8) | 64 (59.3) | 7.121 | 0.008 |
| Invalid |
|
|
|
| 22 (23.2) | 44 (40.7) |
|
|
Cancer-associated fatigue
In the FAS, ALC treatment reduced cancer-associated
fatigue, however, the difference between the control (19.8%) and
treatment (31.2%) groups was not statistically significant after 8
weeks treatment (P=0.0501). Conversely, in the PPS, the effect of
ALC treatment was significantly different between the two groups at
both week 8 (P<0.05) and 12 (P<0.05; Table IV).
 | Table IV.Cancer-associated fatigue. |
Table IV.
Cancer-associated fatigue.
| CTC grade | ALC (%) | Placebo (%) | χ2 | P |
|---|
| FAS |
|
| 4th
week |
|
|
Valid | 17 (15.6) | 16 (13.8) | 0.146 | 0.702 |
|
Invalid | 92 (84.4) | 100 (86.2) |
|
|
| 8th
week |
|
|
Valid | 34 (31.2) | 23 (19.8) | 3.837 | 0.050 |
|
Invalid | 75 (68.8) | 93 (80.2) |
|
|
| 12th
week |
|
|
Valid | 41 (37.6) | 31 (26.7) | 3.063 | 0.080 |
|
Invalid | 68 (62.4) | 85 (73.3) |
|
|
| PPS |
|
| 4th
week |
|
|
Valid | 17 (17.9) | 14 (13.0) | 0.950 | 0.330 |
|
Invalid | 78 (82.1) | 94 (87.0) |
|
|
| 8th
week |
|
|
Valid | 32 (33.7) | 20 (18.5) | 6.100 | 0.014 |
|
Invalid | 63 (66.3) | 88 (81.5) |
|
|
| 12th
week |
|
|
Valid | 39 (41.1) | 27 (25.0) | 5.936 | 0.015 |
|
Invalid | 56 (58.9) | 81 (75.0) |
|
|
KPS
In the FAS, ALC treatment induced a statistically
significant improvement (P<0.05) in KPS (29.3%) compared with
the control group (13.0%). In the PPS, the improvement rate was
31.6% in the experimental group, and 12.0% in the control group, a
difference that was statistically significant (P<0.05). In both
PPS and FAS, the improvement of KPS after 12 weeks of treatment was
also statistically significant compared with the baseline
(P<0.01).
Safety evaluation: Analysis of adverse reactions
and events
Of the 236 patients, 41 reported a total of 62
incidents of adverse reactions. There was no significant difference
in the number of adverse events between the experimental (19.5%)
and control (15.3%) group (P>0.05; Table V). The adverse reaction rate was 6.8%
(8/118) for the trial group and 5.1% (6/118) for the control group,
a difference that was not statistically significant (P>0.05;
Table V). The primary adverse
reactions were gastrointestinal reactions such as vomiting,
abdominal distension and diarrhea. No statistically significant
differences were observed between the treatment and control group
(P>0.05). The most common adverse event was diarrhea [three
cases in the ALC group (2.5%) and two cases in the control group
(1.7%)]. Secondary events were decreased white blood cell count,
liver dysfunction and insomnia. Notably, the three cases of
decreased white blood cell count were all in the ALC group. There
were three cases of liver dysfunction [one in the ALC group (0.8%)
and two in the control group (1.7%)], and three cases of insomnia
[two in the ALC group (1.7%) and one in the control group (0.8%)].
Four subjects in the ALC group withdrew from the study due to
adverse events, but the adverse events in only one of these
patients were associated with the drug. In total, seven severe
adverse events (SAEs) occurred, two in the experimental group
(1.7%) and five in the control group (4.2%). The incidence of
adverse events was not statistically different between the
treatment and control group (P>0.05), and none of the SAEs were
associated with the drugs.
 | Table V.Comparison of adverse reaction and
adverse event incidence. |
Table V.
Comparison of adverse reaction and
adverse event incidence.
| Incident | ALC (%) | Placebo (%) | χ2 | Pa |
|---|
| Adverse events |
|
|
Yes | 23 (19.5) | 18 (15.3) | 0.738 | 0.3903 |
| No | 95 (80.5) | 100 (84.7) |
|
|
| Adverse
reaction |
|
|
Yes | 8 (6.8) | 6 (5.1) | 0.3037 | 0.5816 |
| No | 110 (93.2) | 112 (94.9) |
|
|
Discussion
Chemotherapy has a crucial role in the comprehensive
treatment of cancer (14). However,
CIPN is one of the most common dose-limiting adverse drug reactions
(15–17). CIPN usually affects the dorsal root
ganglia of primary sensory neurons. However, other sites, such as
nerve terminals (distal terminations of the branches of an axon),
may also be affected (14). Clinical
features of CIPN vary depending on the type of agent involved and
the site of action, and may include pure sensory or sensory-motor
peripheral nerve damage of large myelinated or small unmyelinated
fibers (14). The present study
evaluated the efficacy and safety of ALC in Chinese patients with
CIPN.
In this clinical trial, the therapeutic effect of
ALC on neurotoxicity became evident after 8 weeks of treatment, and
neuropathy was significantly reduced in patients treated with ALC.
However, improvement of CIPN was a slow process, and statistically
significant differences were not observed until week 8 after
treatment. At week 12, there remained a significant difference
between the ALC and the placebo group, demonstrating that the
improvement in neurotoxicity persists without further clinical
intervention (including discontinuation of chemotherapeutics).
Electrophysiological tests of neuronal function
revealed statistical differences between the experimental and
control group, with improvement of electrophysiological function
after 8 weeks of treatment. These findings indicate that ALC is
able to improve neuronal function in patients following
chemotherapy, consistent with previous studies which demonstrated
that prophylactic administration of oral ALC prevents the
development of paclitaxel-induced painful peripheral neuropathy
(18,19). Nerve conduction velocity, one of the
objective indicators of peripheral neuropathy was also improved,
but this improvement was less marked than the improvement in the
subjective symptoms of the patients. Comparison of the neuronal
conduction velocity between the baseline and week 8 of the trial
indicated that only the sural sensory nerve exhibited a significant
improvement in function. The following factors may be responsible:
i) Motor neuron toxicity appears in the early stages of
chemotherapy, thus, following timely treatment, neuronal function
was improved and the difference in conduction speed of the two
groups of motor neurons was not statistically significant; ii) the
median, ulnar, and superficial peroneal nerves are composed of
finer fibers and are located peripherally compared with the nervus
suralis neural fiber of the leg, and the coarser fibers are thus
more resistant to CIPN; iii) the sensory nerve fibers recover more
rapidly, and therefore only the sural sensory nerve demonstrated
significant treatment differences.
At the 4th week of this study, the number of
patients with grade 3 decreased, but there was no statistical
difference between the two groups. By the 8th week, the difference
between the two groups gained statistical significance, suggesting
that the onset and process of CIPN improvement is slow. Therefore,
the treatment of CIPN requires long-term medication. After 4 weeks
of ALC withdrawal (12th week of trial), the two groups returned to
being statistically indistinguishable from one another. The trial
group improved more than the control group with 37 grade 1 patients
(34.6%), compared with 28 (25.5%) in the control group, and 22
cases (20.6%) of grade 3 patients in the trial group, compared with
34 cases (30.9%) in the control group. It was hypothesized that if
this treatment period was extended to 12 weeks, the improvement
would be further increased.
In the current study, the efficacy of ALC on CIPN
improvement was not associated with the subject cancer types or the
chemotherapy. Although chemotherapy may induce CIPN via various
pathways, the main characteristics are inflammation and neuronal
necrosis. Given the potential influence of chemotherapy, all
patients in the study had not previously received chemotherapy
(20–23). Another important point is all the
subjects in the study has stopped and would not receive the
chemotherapy. Therefore, the influence of chemotherapy may be
eliminated.
In the PPS, the ALC group had significantly
diminished cancer-associated fatigue compared with the control
group. In both the FAS and PPS, the ALC group exhibited significant
improvements in KPS compared with the control group. These results
demonstrate that ALC is able to ease cancer-associated fatigue and
improve the physical condition of patients following chemotherapy.
Fatigue, caused by tumors and their associated treatment is a
common problem for patients with cancer, and chronic fatigue
seriously diminishes patient quality of life. Currently, there is a
lack of pharmacological therapies for the treatment of
cancer-associated fatigue. The results of this clinical study
demonstrate that ALC is able to reduce cancer-associated fatigue,
thus improving patient quality of life.
The overall incidence of adverse reactions in this
clinical study was 5.9%, with 6.8% for the ALC group. In total,
3.4% of the patients withdrew from the study due to adverse
reactions. These results demonstrate that ALC is well tolerated in
patients, which is consistent with previous studies (24–27).
Seven cases of SAE [two in the trial group (1.7%) and five in the
control group (4.2%)] were recorded, although none of the SAEs were
determined to be associated with drug administration. These
findings provide evidence of the high safety profile of this type
of treatment intervention.
In conclusion, to the best of our knowledge, the
present study provides the first demonstration of the efficacy and
safety of ALC for reducing chemotherapy-induced peripheral
neuropathy toxicity and its associated symptoms. Based on these
results, ALC may have an important role in the treatment of
chemotherapy-induced peripheral neuropathy in China.
Acknowledgements
The authors of the present study would like to thank
Professor Zhao Naiqing and Professor Luo Jiangfeng for their advice
and help with the statistical analysis involved in the present
study, and are grateful to Dr. Yao Chaoya and Dr. Qian Xuemei for
their participation with the electrophysiology examination. This
study was funded by Lee's Pharmaceutical (Hong Kong) Ltd. and
Sigma-Tau Pharmaceutical, Inc., (Pomezia, Italy).
References
|
1
|
Ocean AJ and Vahdat LT:
Chemotherapy-induced peripheral neuropathy: Pathogenesis and
emerging therapies. Support Care Cancer. 12:619–625.
2004.PubMed/NCBI
|
|
2
|
Urba SG, Orringer MB, Ianettonni M, Hayman
JA and Satoru H: Concurrent cisplatin, paclitaxel and radiotherapy
as preoperative treatment for patients with locoregional esophageal
carcinoma. Cancer. 98:2177–2183. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brewer JR, Morrison G, Dolan ME and
Fleming GF: Chemotherapy-induced peripheral neuropathy: Current
status and progress. Gynecol Oncol. 140:176–183. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Taglialatela G, Angelucci L, Ramacci MT,
Werrbach-Perez K, Jackson GR and Perez-Polo JR: Stimulation of
nerve growth factor receptors in PC12 by acetyl-L-carnitine.
Biochem Pharmacol. 44:577–585. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Westlund KN, Lu Y, Werrbach-Perez K,
Hulsebosch CE, Morgan B, Pizzo DP, Eisenberg HM and Perez-Polo JR:
Effects of nerve growth factor and acetyl-L-carnitine arginyl amide
on the human neuronal line HCN-1A. Int J Dev Neurosci. 10:361–373.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pisano C, Pratesi G, Laccabue D, Zunino F,
Lo Giudice P, Bellucci A, Pacifici L, Camerini B, Vesci L,
Castorina M, et al: Paclitaxel and Cisplatin-induced neurotoxicity:
A protective role of acetyl-L-carnitine. Clin Cancer Res.
9:5756–5767. 2003.PubMed/NCBI
|
|
7
|
Ghirardi O, Lo Giudice P, Pisano C,
Vertechy M, Bellucci A, Vesci L, Cundari S, Miloso M, Rigamonti LM,
Nicolini G, et al: Acetyl-L-Carnitine prevents and reverts
experimental chronic neurotoxicity induced by oxaliplatin, without
altering its antitumor properties. Anticancer Res. 25:2681–2687.
2005.PubMed/NCBI
|
|
8
|
Xiao WH and Bennett GJ:
Chemotherapy-evoked neuropathic pain: Abnormal spontaneous
discharge in A-fiber and C-fiber primary afferent neurons and its
suppression by acetyl-L-carnitine. Pain. 135:262–270. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Argyriou AA, Velasco R, Briani C,
Cavaletti G, Bruna J, Alberti P, Cacciavillani M, Lonardi S, Santos
C, Cortinovis D, et al: Peripheral neurotoxicity of oxaliplatin in
combination with 5-fluorouracil (FOLFOX) or capecitabine (XELOX): A
prospective evaluation of 150 colorectal cancer patients. Ann
Oncol. 23:3116–3122. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Portenoy RK and Itri LM: Cancer-related
fatigue: Guidelines for evaluation and management. Oncologist.
4:1–10. 1999.PubMed/NCBI
|
|
11
|
de Kock I, Mirhosseini M, Lau F, Thai V,
Downing M, Quan H, Lesperance M and Yang J: Conversion of Karnofsky
Performance Status (KPS) and Eastern Cooperative Oncology Group
Performance Status (ECOG) to Palliative Performance Scale (PPS),
and the interchangeability of PPS and KPS in prognostic tools. J
Palliat Care. 29:163–169. 2013.PubMed/NCBI
|
|
12
|
Iwasaki N, Ogata M, Tomonaga O, Kuroki H,
Kasahara T, Yano N and Iwamoto Y: Liver and kidney function in
Japanese patients with maturity-onset diabetes of the young.
Diabetes Care. 21:2144–2148. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fisman EZ, Motro M, Tenenbaum A, Boyko V,
Mandelzweig L and Behar S: Impaired fasting glucose concentrations
in nondiabetic patients with ischemic heart disease: A marker for a
worse prognosis. Am Heart J. 141:485–490. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Argyriou AA, Kyritsis AP, Makatsoris T and
Kalofonos HP: Chemotherapy-induced peripheral neuropathy in adults:
A comprehensive update of the literature. Cancer Manag Res.
6:135–147. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brzezinski K: Chemotherapy-induced
polyneuropathy. Part I. Pathophysiology. Contemp Oncol (Pozn).
16:72–78. 2012.PubMed/NCBI
|
|
16
|
Carozzi VA, Canta A and Chiorazzi A:
Chemotherapy-induced peripheral neuropathy: What do we know about
mechanisms? Neurosci Lett. 596:90–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mols F, Beijers T, Vreugdenhil G and van
de Poll-Franse L: Chemotherapy-induced peripheral neuropathy and
its association with quality of life: A systematic review. Support
Care Cancer. 22:2261–2269. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Flatters SJ, Xiao WH and Bennett GJ:
Acetyl-L-carnitine prevents and reduces paclitaxel-induced painful
peripheral neuropathy. Neurosci Lett. 397:219–223. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jin HW, Flatters SJ, Xiao WH, Mulhern HL
and Bennett GJ: Prevention of paclitaxel-evoked painful peripheral
neuropathy by acetyl-L-carnitine: Effects on axonal mitochondria,
sensory nerve fiber terminal arbors, and cutaneous Langerhans
cells. Exp Neurol. 210:229–237. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Scholz J and Woolf CJ: The neuropathic
pain triad: Neurons, immune cells and glia. Nat Neurosci.
10:1361–1368. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Marchand F, Perretti M and McMahon SB:
Role of the immune system in chronic pain. Nat Rev Neurosci.
6:521–532. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Uceyler N, Kafke W, Riediger N, He L,
Necula G, Toyka KV and Sommer C: Elevated proinflammatory cytokine
expression in affected skin in small fiber neuropathy. Neurology.
74:1806–1813. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Areti A, Yerra VG, Naidu V and Kumar A:
Oxidative stress and nerve damage: Role in chemotherapy induced
peripheral neuropathy. Redox Biol. 2:289–295. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Malaguarnera M, Gargante MP, Cristaldi E,
Colonna V, Messano M, Koverech A, Neri S, Vacante M, Cammalleri L
and Motta M: Acetyl L-carnitine (ALC) treatment in elderly patients
with fatigue. Arch Gerontol Geriatr. 46:181–190. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Maestri A, De Pasquale Ceratti A, Cundari
S, Zanna C, Cortesi E and Crinò L: A pilot study on the effect of
acetyl-L-carnitine in paclitaxel- and cisplatin-induced peripheral
neuropathy. Tumori. 91:135–138. 2005.PubMed/NCBI
|
|
26
|
Evans JD, Jacobs TF and Evans EW: Role of
acetyl-L-carnitine in the treatment of diabetic peripheral
neuropathy. Ann Pharmacother. 42:1686–1691. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Bianchi G, Vitali G, Caraceni A, Ravaglia
S, Capri G, Cundari S, Zanna C and Gianni L: Symptomatic and
neurophysiological responses of paclitaxel- or cisplatin-induced
neuropathy to oral acetyl-L-carnitine. Eur J Cancer. 41:1746–1750.
2005. View Article : Google Scholar : PubMed/NCBI
|