Introduction
The frequency of diagnosing small nodules in the
lungs by biopsy is increasing due to a high incidence of lung
cancer and the requirement for early diagnosis. Computed tomography
(CT)-guided percutaneous fine needle biopsy is a common method for
harvesting the lesion with adjacent lung tissue (1–3), thereby
facilitating histological analysis of the pathology of the nodule
(4,5). Solitary pulmonary nodules >30 mm in
diameter are predominantly malignant (6,7).
Malignant diagnoses of solitary pulmonary lesions <20 mm in
diameter range from 60 (8) to 67%
(9) and have a lower detection rate
due to the absence of typical features, such as Spicule sign or
Pleural indentation, in imaging examinations and limitations in
bronchoscopy and sputum cell screening. Factors that markedly
improve the accuracy of diagnosis are larger lesions (>10 mm)
and a shorter needle path (≤40 mm) (10). In addition, dynamic observation of
small nodules may result in a psychological burden on patients, and
clinical resection of these small nodules may be radical. Resection
of these nodules may not only cause physical injury to the
patients, but also increase medical costs; therefore, qualitative
diagnosis is important for nodules ≤30 mm in diameter.
CT-guided percutaneous fine needle biopsy is an
economic method that rarely causes metastasis (11,12). The
most common complications of CT-guided percutaneous fine needle
biopsy include pneumothorax and hemorrhage. The rate of
pneumothorax ranges from 4 to 17% (7) in patients who receive CT-guided biopsy
for large pulmonary lesions (mean diameter, 36 mm; range, 5–136 mm)
(4,13). The rate of pneumothorax following
CT-guided percutaneous core needle biopsy of small lesions (<20
mm in diameter) varies widely, ranging from 10 to 35% (8–10,14,15).
A high rate of pneumothorax (52.7%) has been reported following
CT-guided fine needle aspirate biopsies of lesions ≤10 mm in
diameter (16). Secondly, the rate
of hemorrhage or hemoptysis ranges from 4 (17) to 27% (13,15) and
can be influenced by the proximity of the nodule to the pulmonary
hilum. Air embolisms and/or infarctions are rare complications in
patients with CT-guided biopsies.
The wide range of accuracy and complication rates
suggests that different instruments, operators and patient
populations may contribute to the heterogeneity. Therefore,
comparison of the effects of lesion sizes on the accuracy of
CT-guided biopsy capture in patients without emphysema, pulmonary
bullae, pulmonary fibrosis or interstitial lung diseases by an
experienced team from a single facility may minimize confounding
factors. It was hypothesized that the lesion size, proximity to
pleura and the length of the needle path may affect the accuracy of
CT-guided biopsy and/or the frequency of various complications.
Therefore, the present retrospective study was undertaken to
analyze the clinical outcomes of 155 patients who received
CT-guided percutaneous lung biopsies of intrapulmonary solitary
nodules of ≤30 mm in diameter between June 2013 and March 2014 at
the Department of Radiology, Shengjing Hospital of China Medical
University (Shenyang, China). Patients were grouped by lesion size
to explore the factors affecting the accuracy of biopsy of
intrapulmonary solitary nodules of ≤30 mm in diameter and the
safety of the procedure. The findings may provide insights for the
clinical use of CT-guided percutaneous fine needle biopsy for
nodules ≤30 mm in diameter.
Materials and methods
Ethics statement
The Ethics Committee Institutional Review Board of
Shenyang Hospital of China Medical University approved the present
retrospective study (IRB2016PS192K). The informed consent
requirement was waived.
Patients
Prospectively collected data on the medical records
of 450 patients admitted to the hospital between June 2013 and
March 2014 for lung biopsy were retrospectively reviewed. Inclusion
criteria were preoperatively evaluated by enhanced CT. In order for
the patients to be included, CT results had to show that
bronchoscopy was not possible; nodules were free of major vessels;
CT-guided biopsy of a single, intra-pulmonary, solid tumor of ≤30
mm in diameter had been conducted; and absence of prior therapy of
intra-pulmonary nodules. Additionally, patients were required to be
>18 years of age, with normal clotting and platelet function
pre-biopsy and have sufficient tissue for pathological examination.
Exclusion criteria included: Patients without pre-operative
enhanced CT records; blood-rich nodules; two or more nodules;
ground-glass opacity in the intrapulmonary solitary nodule
(18); and major vessel involvement
in the nodule. Patients were separated into three age subgroups
(≤41, 41–67 and ≥67 years) three puncture depth subgroups (≤25.6,
25.6–34.6 and ≥34.6 mm).
In order to ensure the final results were reliable
and convincing, two radiologists evaluated the image findings and
confirmed that the solitary nodules were ≤30 mm in diameter.
Following biopsy, imaging re-examination was performed. In total,
155 patients were included in the final analysis. Patients with
extensive lung disease (including emphysema, pulmonary bullae,
pulmonary fibrosis and interstitial lung diseases), and patients
with coagulation abnormalities and bleeding-associated diseases
were not included in the present study.
A routine chest X-ray was performed 10 min after
biopsy to confirm the absence of complications, such as
pneumothorax or bleeding. Patients were monitored for 24 h after
surgery and delayed complications were determined according to the
vital signs.
Instruments and methods
A Philips MX8000 IDT 16-row multislice spiral CT
scanner (Philips Medical Systems, Inc., Bothell, WA, USA) and a
MAX-CORE biopsy instrument (20 G/16 cm) (C.R. Bard, Inc., Murray
Hill, NJ, USA) were utilized for transverse scanning by spiral CT
and biopsy, respectively. The depth and angle of the needle were
recorded prospectively and were measured retrospectively from
images exhibiting the needle. The preoperative enhanced CT scan
recorded the position of the major blood vessels. The site of
needle puncture, puncture route, puncture depth and direction were
calculated according to the findings in the preoperative chest
enhanced CT scan, and followed the principle of the shortest
distance and an angle between the pleura and needle as close as
possible to 90° (19,20). CT scan images were used to identify
the presence of pneumothorax prior to marking the site of needle
insertion. For patients with pleural adhesion caused by
tuberculosis (TB), a real-time CT scan was utilized to ensure the
chosen needle path avoided the TB-induced adhesion region. The site
of puncture was marked with lead. Patients breathed freely in the
optimized prone, supine or lateral position and a 19-G locating
needle was inserted into the proximal end of the nodule. Subsequent
to the confirmation of needle location, the needle was withdrawn
and a BARD 20-G needle was used for biopsy 2–3 times until
sufficient tissue for further experiments was obtained. Biopsy
tissue was subjected to immediate cytological evaluation by a
technician with 15 years of experience to ensure there was
sufficient tissue for adequate analysis. Tissues were subsequently
fixed in formaldehyde and processed for pathological
examination.
Pathological examination and
diagnostic accuracy of CT-guided biopsy capture
Two pathologists, each with 25 years of experience,
examined every whole biopsy specimen obtained from the first
puncture for pathological characteristics, such as atypical
adenomatous hyperplasia, squamous cell carcinoma, adenosquamous
carcinoma and infectious nodules. Both pathologists agreed with the
findings. A biopsy specimen with a pathological characteristic was
scored as a successful biopsy. When a first puncture biopsy showed
findings of only necrotic tissues or normal lung tissues, it was
scored as a biopsy failure.
Diagnostic criteria of pulmonary
complications
For the present study, two clinicians were invited
to review and evaluate the postoperative images to assure the
reliability of complication identification. Immediately following
surgery, CT imaging was performed by two physicians to examine the
puncture site for complications. A third physician was consulted in
the case of disagreement. Symptomatic pneumothorax (referred to as
pneumothorax in the present study) was defined as: The presence of
free gas in the pleural cavity with no intrapulmonary hemorrhage
and no intrapleural hemorrhage; the presence of clinical symptoms
(chest tightness, shortness of breath within 24 h and unilateral
auscultation breath sounds); and X-ray confirmation after 24 h.
Hemorrhage was defined as the presence of intrapulmonary bloody
exudate or intrapleural bloody fluid, with no free gas in the
pleural cavity. Hemorrhage concomitant with pneumothorax was
defined as free gas within the pleural cavity and intrapulmonary
hemorrhage and/or intrapleural bloody fluid. Hemoptysis was defined
as the presence of >10 ml of blood in the sputum and/or
spit.
Statistical analysis
The cut-off points that defined the three age
subgroups (≤41, 41–67 and ≥67 years) and three puncture depth
subgroups (≤25.6, 25.6–34.6 and ≥34.6 mm) were calculated as the
mean ± one standard deviation. Puncture depth was an indicator of
the nodule's proximity to the pulmonary hilum. Patients with a
pathological characteristic in their biopsy tissue were presented
as counts and percentages within associated factors. Chi-square or
Fisher's exact tests were performed to investigate the correlation
between the success (and non-success) of puncture and the
associated factors, such as gender, age and tumor diameter. The
pleural-lesion angle was presented as the mean ± one standard
deviation and a two-tailed, independent t-test was performed to
compare the differences between the successful and non-successful
punctures. Univariate logistic regression analyses were performed
to identify the factors associated with the success of puncture.
P<0.05 was considered to indicate a statistically significant
difference. SPSS 22.0 statistical software (IBM SPSS, Armonk, NY,
USA) for Windows was used for statistical analysis.
Results
Patients
Medical records of 155 patients (128 smokers and 27
non-smokers) diagnosed with an intrapulmonary solitary nodule were
retrospectively reviewed and the images and biopsy slides were
re-examined. The 105 males and 50 females had a mean age of 54±13
years (range, 21–91 years). The mean diameter of the solitary
nodules examined was 19.8±6 mm (range, 6–30 mm). The mean biopsy
depth, which was determined as the distance between visceral pleura
and outside border of nodules, was 25.6±9 mm (range, 6–78 mm). The
mean number of biopsies per person was 2±1 (range, 1–6). A single
puncture event (n=25) yielded an 86.2% [95% confidence interval
(CI): 67.43–95.49%] accuracy of diagnostic CT-guided biopsy
capture, and two to three punctures (n=111) demonstrated a 91.7%
(95% CI: 84.96–95.75%) diagnostic accuracy of the CT-guided capture
(P=0.331). Insertion of a chest tube was not required for any of
the patients and no patients experienced an air embolism.
Pathological findings were detected in 140 (90.3%)
of 155 biopsies, and these were defined as successful biopsy
punctures. Regardless of their gender of age, 90.3% of patients
exhibited pathology in their biopsies (Table I). The diameter of the tumor and
pleural adhesiveness were significantly correlated with the success
or non-success of the puncture. The percentage of successful
punctures was significantly higher in patients with a tumor
diameter of 21–30 mm [97.01% (95% CI: 88.68–99.48%)] compared with
those with a tumor diameter of ≤10 [85.71% (95% CI: 42.00–99.25%)]
and 11–20 mm [85.19% (95% CI: 75.16–91.79%)] (P=0.049). The
percentage of successful punctures was significantly higher in
patients with negative pathological findings in pleural
adhesiveness [100% (95% CI: 86.27–100%)] compared with those
subjects with positive pathological results [87.9% (95% CI:
80.53–92.84%); P=0.042]. The puncture success rate of the puncture
depth of 25.6–34.6 mm was higher [96.6% (95% CI: 87.05–99.4%)] than
the shallower or deeper punctures; however, the differences
observed between the depths did not reach statistical significance.
The puncture success rate was 91.74% (95% CI: 84.96–95.75%) with
puncture repetition of 2–3 times, which was greater than those with
punctures performed once or >3 times. The mean pleural lesion
angle was 61.29° in subjects with successful puncture (Table I).
 | Table I.Baseline distribution of successful
biopsies. |
Table I.
Baseline distribution of successful
biopsies.
| Variable | Unsuccessful | Successful | P-value |
|---|
| Total | 15 | 140 |
|
| Gender |
|
| 0.285 |
| Male | 12 (11.43) | 93 (88.57) |
|
|
Female | 3 (6.00) | 47 (94.00) |
|
| Age (years) |
|
| 0.055 |
| ≤41 | 4 (17.39) | 19 (82.61) |
|
|
41–67 | 11 (10.78) | 91 (89.22) |
|
| ≥67 | 0 (0.00) | 30 (100.00) |
|
| Diameter of tumor
(mm) |
|
| 0.049a |
| ≤10 | 1 (14.29) | 6 (85.71) |
|
|
11–20 | 12 (14.81) | 69 (85.19) |
|
|
21–30 | 2 (2.99) | 65 (97.01) |
|
| Pleural
adhesiveness |
|
| 0.042a |
| + | 15 (12.1) | 109 (87.9) |
|
| − | 0 (0.00) | 31 (100.00) |
|
| Puncture depth
(mm) |
|
| 0.088 |
|
≤25.6 | 9 (12.00) | 66 (88.00) |
|
|
25.6–34.6 | 2 (3.45) | 56 (96.55) |
|
|
≥34.6 | 4 (18.18) | 18 (81.82) |
|
| Puncture times |
|
| 0.331 |
| 1 | 4 (13.79) | 25 (86.21) |
|
|
2–3 | 10 (8.26) | 111 (91.74) |
|
|
>3 | 1 (20.00) | 4 (80.00) |
|
| Pleural-lesion
angleb | 59.67±9.32 | 61.29±12.19 | 0.617 |
Factors associated with successful
biopsy
The factors associated with successful biopsy that
were examined in the present study did not reach statistical
significance in the univariate and multivariate logistic analysis
(P>0.05; Table II).
 | Table II.Factors associated with successful
puncture. |
Table II.
Factors associated with successful
puncture.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Variable | OR (95% CI) | P-value | OR (95% CI) | P-value |
|---|
| Gender |
|
|
|
|
|
Male | 0.49
(0.13–1.13) | 0.293 | 0.51
(0.13–2.13) | 0.352 |
|
Female | Ref |
| Ref |
|
| Age | 1.04
(1.00–1.00) | 0.076 | 1.04
(0.99–1.99) | 0.093 |
|
Diameter of tumor | 1.09
(0.99–1.99) | 0.071 | 1.08
(0.97–1.97) | 0.157 |
|
Pleural-lesion angle | 1.01
(0.97–1.97) | 0.615 | 1.02
(0.97–1.97) | 0.419 |
| Pleural
adhesiveness |
|
|
|
|
| + | NA |
| NA |
|
| − | Ref |
| Ref |
|
| Puncture depth
(mm) | 1.01
(0.95–1.95) | 0.760 | 1.01
(0.95–1.95) | 0.733 |
| Puncture times |
|
|
|
|
| 1 | Ref |
| Ref |
|
|
2–3 | 1.78
(0.51–6.51) | 0.363 | 1.44
(0.36–5.36) | 0.609 |
|
>3 | 0.64
(0.06–7.06) | 0.719 | 0.73
(0.05–10.05) | 0.813 |
Diagnoses and complication rates
The predominant diagnosis of the successful biopsies
was cancer [94.3% (95% CI: 88.69–97.32%)], particularly
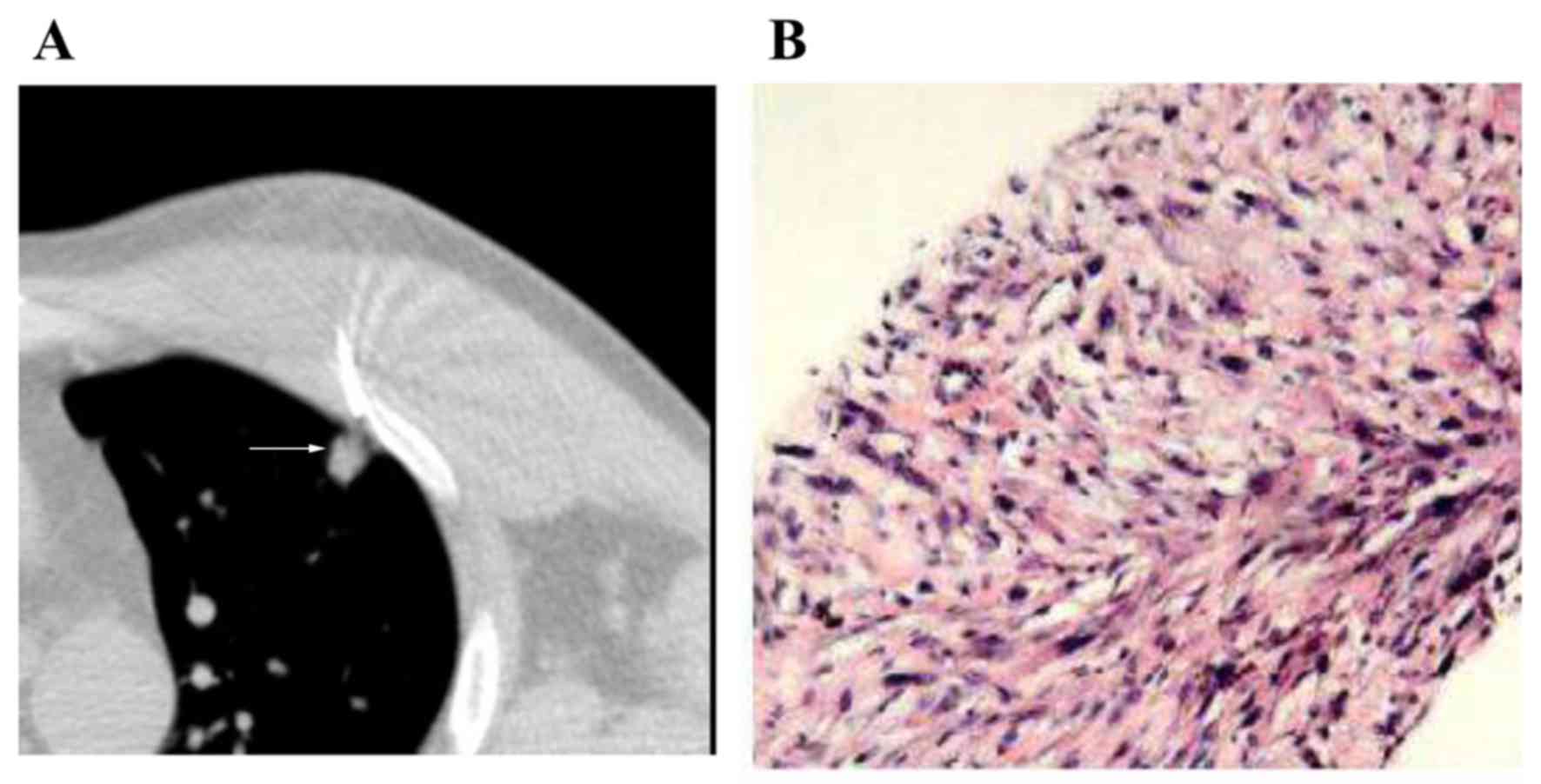
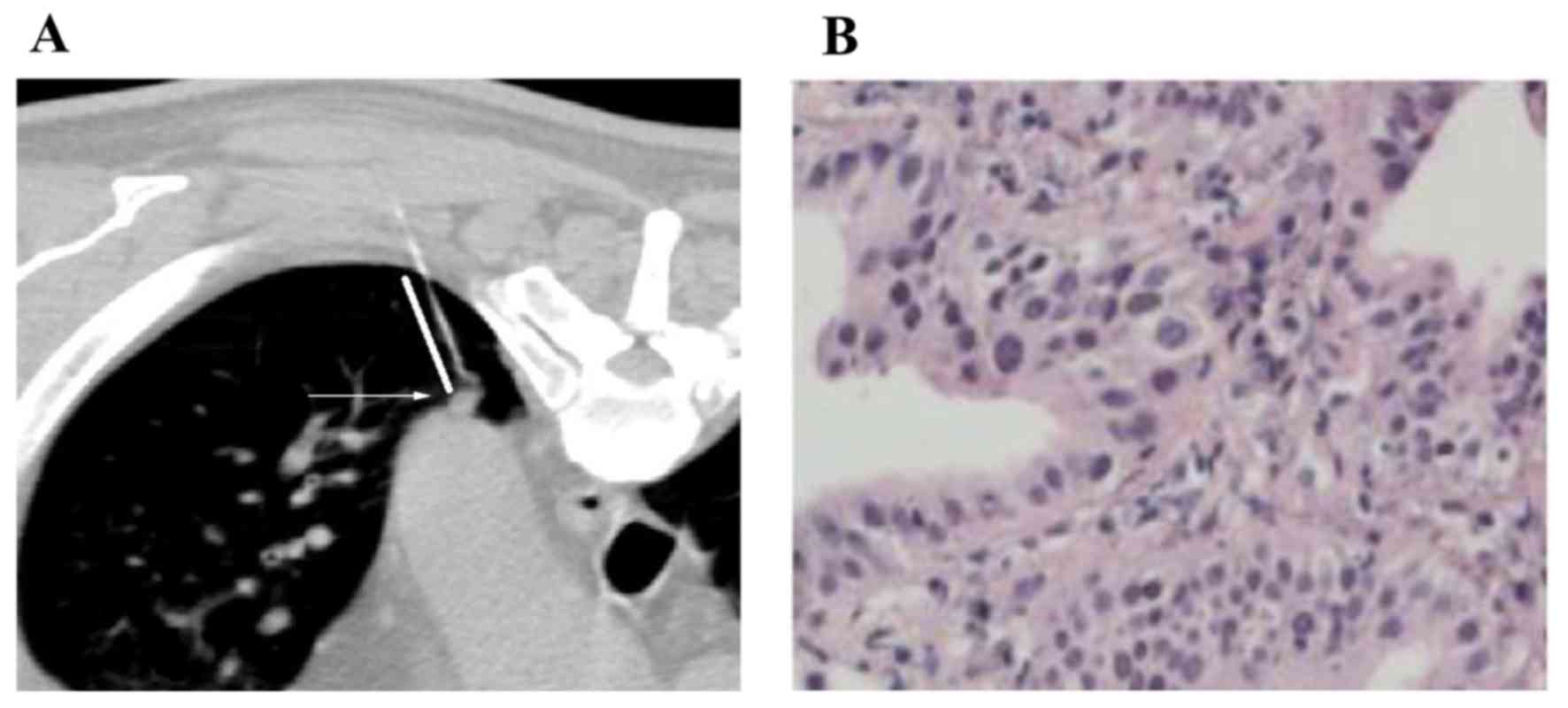
adenocarcinoma of the lung [81.4% (95% CI: 73.79–87.9%)] (Table III). Four successful CT-guided
percutaneous lung biopsies of solitary pulmonary lesions with
diameters of 6, and 6 mm are shown in Figs. 1 and 2, respectively.
 | Table III.Pathological findings in subjects
with a successful biopsy. |
Table III.
Pathological findings in subjects
with a successful biopsy.
| Variable | N | Incidence rate
(%) |
|---|
| Pathology |
|
|
|
Adenocarcinoma | 114 | 81.4 |
|
Squamous cell carcinoma | 10 |
7.1 |
|
Alveolar cell carcinoma in
situ | 1 |
0.7 |
|
Malignant mesothelioma | 1 |
0.7 |
| Small
cell lung cancer | 1 |
0.7 |
| Lung
metastasis | 4 |
2.9 |
|
Adenosquamous carcinoma | 1 |
0.7 |
| Chronic
inflammation | 4 |
2.9 |
|
Pulmonary tuberculosis | 3 |
2.1 |
|
Coccidioidomycosis | 1 |
0.7 |
The incidences of pneumothorax, bleeding and
pneumothorax plus bleeding in the successful puncture subjects were
20 (95% CI: 13.91–27.78%), 10 (95% CI: 5.78–16.51%) and 7.14% (95%
CI: 3.67–13.08%), respectively. The incidences of pneumothorax,
bleeding and pneumothorax plus bleeding in the patients with the
non-successful biopsies were 20 (95% CI: 5.31–48.63%), 13.3 (95%
CI: 2.34–41.61%) and 0% (95% CI: 0.00–25.35%), respectively
(Table IV). No patients experienced
hemoptysis and no patients received a chest tube (i.e. chest tube
rate is 0). The following factors were examined for their potential
effect on the development of pneumothorax, bleeding and
pneumothorax plus bleeding: Lesion size; pleural adhesion; puncture
depth; and number of punctures (Table
IV). The lesion size was significantly associated with the
development of pneumothorax, bleeding, and pneumothorax plus
bleeding (P=0.013). The highest incidence of pneumothorax occurred
in the 11–20 mm lesion size group [23.19% (95% CI: 14.22–35.18%)].
The highest incidence of bleeding occurred in the ≤21–30 mm lesion
size group [16.92% (95% CI: 9.14–28.68%)]. The highest incidence of
pneumothorax plus bleeding was observed in patients with lesions
<10 mm in diameter [33.33% (95% CI: 6.00–75.89%); P=0.013;
Table IV). The incidences of
pneumothorax, bleeding and pneumothorax plus bleeding were not
significantly associated with pleural adherence, puncture depth or
number of punctures (P>0.05; Table
IV).
 | Table IV.Effect of lesion size on the
incidence of pneumothorax, bleeding, and pneumothorax plus bleeding
in patients with successful biopsies. |
Table IV.
Effect of lesion size on the
incidence of pneumothorax, bleeding, and pneumothorax plus bleeding
in patients with successful biopsies.
| Variable | N | PTx | Bleeding | PTx + Bleeding | P-value |
|---|
| Total successful
punctures | 140 | 28 | 14 | 10 |
|
| Size of lesion
(mm) |
|
|
|
| 0.013 |
|
≤10 | 6 | 0 (0.0) | 1
(16.7) | 2 (33.3) |
|
|
11–20 | 69 | 16 (23.2) | 2 (2.9) | 3 (4.4) |
|
|
21–30 | 65 | 11 (16.9) | 11 (16.9) | 5 (7.7) |
|
| Pleural
adhesion |
|
|
|
| 0.400 |
|
Yes | 31 | 9 (29.0) | 2
(6.45) | 1 (3.2) |
|
| No | 109 | 18 (16.5) | 12 (11.0) | 9 (8.3) |
|
| Puncture depth
(mm) |
|
|
|
| 0.062 |
|
<25.6 | 66 | 15 (22.7) | 5 (7.6) | 4 (6.1) |
|
|
25.6–34.6 | 56 | 9 (16.1) | 5 (8.9) | 2 (3.6) |
|
|
>34.6 | 18 | 3 (16.7) | 4
(22.2) | 4 (22.2) |
|
| Number of
punctures |
|
|
|
| 0.704 |
| 1 | 25 | 6 (24.0) | 2 (8.0) | 1 (4.0) |
|
| 2 | 111 | 20 (18.0) | 12 (10.8) | 8 (7.2) |
|
| ≥3 | 4 | 1 (25.0) | 0 (0.0) | 1 (25.0) |
|
Discussion
The present retrospective study of 155 patients
demonstrated that CT-guided percutaneous lung biopsy of
intrapulmonary solitary nodules of ≤30 mm in diameter had a high
accuracy rate (90.3%), which is consistent with the findings
reported by Lee et al (4),
Hwang et al (9), Choi et
al (15), Li et al
(21) and Capalbo et al
(22). Preoperative evaluation of
puncture routes, preoperative guidance to properly control
respiratory amplitude and frequency, avoidance of injury to major
vessels and precise recognition of the tip position of the needle
may help to maintain an acceptable risk/benefit ratio of the
CT-guided biopsy, particularly for the examination of nodules close
to major vessels. Additionally, CT-guided biopsy can be used to
determine the nature of small nodules without the requirement of
additional surgery, which is beneficial for both patients and
clinicians (7,23).
In the present study, it was demonstrated that
nodule size and adhesion of the nodule to the pleura significantly
affected the accuracy of biopsy. The accuracy of the biopsy was
significantly higher for nodules of 21–30 mm in diameter compared
with the accuracy for smaller nodules, particularly for those that
were <10 mm in diameter. It is possible to speculate that the
small nodules are more likely to move during respiration, which may
result in the CT failing to accurately indicate the needle path
throughout the respiration cycle. A slight change in needle angle
or respiration phase during insertion may cause the needle to miss
the nodule, resulting in failure of the biopsy. In addition, the
small nodules may not possess sufficient tissue to render a
conclusive pathological diagnosis, reducing the likelihood of a
successful diagnosis. Secondly, adhesion of a nodule to the pleura
may fix the position of the nodule, resulting in less movement
during respiration. This may explain why increased biopsy accuracy
is obtained with pleural-adhered nodules during CT-guided
biopsy.
Ohno et al (10) found that biopsy depth affected the
accuracy of biopsy; for example, biopsies with needle path lengths
of ≤40 mm exhibited an accuracy rate of ≥88%, while those with
lengths of 41–80 mm decreased to an accuracy rate of 50–62% and
those with needle path lengths of >81 mm exhibited a 12.5%
accuracy rate. In comparison, the majority of biopsies in the
present study utilized shorter needle path lengths; 87.1% of
successful biopsies utilized needle paths <34.5 mm and the
needle path lengths of the 15 unsuccessful biopsies exhibited a
median length of 24 mm (range, 12–37 mm). In addition, Choi et
al (15) found no correlation
between accuracy and needle path lengths (biopsy depth) up to 120
mm, suggesting that increased accuracy rates may decrease the
ability to detect potential factors that are important at other
facilities. An additional contributing factor to biopsy accuracy
may be the use of larger needles (20- or 18-G), which may obtain
larger and more complete samples compared with smaller needles.
Hemorrhage and pneumothorax are the two most common
complications of CT-guided percutaneous needle biopsy (24). Rates of hemorrhage or hemoptysis have
varied in previous studies; with values reported to be 4 (17), 9 (22), 14.5 (15), 20–22 (2) and 27% (13,23).
Similar to Capalbo et al (22) and Choi et al (15), bleeding occurred in 10% of patients
in the present study; patients with nodules of 21–30 mm had a
significantly higher risk of hemorrhage compared with those with
smaller nodules. Elevated bleeding risk may be associated with a
rich blood supply in larger nodules. Both needle path length and a
needle path that traversed a pulmonary vessel were observed as risk
factors for hemorrhage in a study by Nour-Eldin et al
(2). Additionally, lesions measuring
<20 mm have been identified as a significant risk factor for
hemorrhage (2), but there are
conflicting reports (22). However,
the present study demonstrates that smaller nodules are associated
with a higher risk for postoperative pneumothorax and hemorrhage. A
smaller nodule size may increase the risk of the needle damaging
the surrounding small vessels or lung tissue. The results of the
present study indicated that a shallower biopsy depth was
associated with a higher risk for pneumothorax and hemorrhage. It
may be speculated that the needle was not effectively fixed in the
lung when the biopsy depth was shallow, meaning the needle was more
likely to move with respiration, resulting in injury to the pleura
and an increased risk of hemorrhage and pneumothorax.
Successful CT-guided biopsy of a solitary pulmonary
nodule involves: Fixing the positions of the needle and the nodule
by preoperative training of the respiration of each patient;
intraoperative precise localization of both the nodule and the
needle; a larger needle bore size to reduce the number of biopsies;
and a longer depth of the intramuscular part of the needle, which
allows the position of the needle to be fixed, thus reducing
displacement and increasing the accuracy rate. One biopsy of a
nodule may result in the nodule becoming covered by surrounding
lung tissue or gas cavity, resulting in the movement of this nodule
and a decrease in the accuracy of subsequent biopsies of the same
nodule. Decreasing the number of biopsies is also a key factor in
reducing postoperative complications, such as hemorrhage and
pneumothorax. Biopsy depth should be accurately controlled to
prevent needle-induced injury to the local lung tissues and
subsequent hemorrhage. A thorough discussion with patients before
the procedure reduces intraoperative stress. In addition,
administration of local anesthesia close to the parietal pleura may
reduce any potential pleural twitching or reflex (25) and may improve the patient cooperation
during surgery.
As medium and large nodules (>20 mm) may have
central necrosis, the selection of an appropriate site for biopsy
is pivotal to increase the accuracy of biopsy (26). It has been demonstrated that a biopsy
of larger nodules with central necrosis may require inclusion of
the border of the nodule for adequate live cells for pathological
analyses (26). Furthermore,
preoperative enhanced CT or positron emission tomography (PET)-CT
is can be used to identify the solid components and display the
internal structure of the nodule, when compared with general CT.
Enhanced CT or PET-CT are able to identify the tissues rich in
blood supply and display the necrotic tissues and nonviable tissues
in the nodule, which increases the accuracy of the biopsy.
The present study has several limitations. Firstly,
it is a retrospective study at a single institution. While the
accuracy and complication rates may be more applicable to this
particular facility, the additional insights gained on these
essential details may encourage additional facilities to test
and/or adopt them and subsequently improve their CT-guided
percutaneous biopsy procedures. The success rate of a biopsy and
the complication rate may vary due to inter-performer variability.
However, the success rate of the biopsies in the present study was
determined by the pathology, and thus the success rate variation
should be limited. The incidence of complications was determined by
two physicians independently, and another physician was consulted
if necessary. The same technique criteria were was used in all
patients and all biopsies were by the same investigator. Secondly,
the number of lesions <10 mm in diameter was low in our patient
population (7/155; 4.5%) in comparison to the studies by Li et
al (32/169; 18.9%) (8), Ohno
et al (21/162; 13%) (10) and
Choi et al (23/173; 13.3%) (15). A possible reason may be that patients
with emphysema, who were excluded from the present study, may be
more likely to be examined and found to possess small nodules
compared with patients without emphysema. However, the accuracy
rate demonstrated in the present study was consistent with rates
reported by Ng et al (16).
Although the number of nodules <10 mm in diameter was low, the
puncture accuracy of these nodules was significant lower (P=0.049)
than observed in the other two subgroups. Nodules sized 10–20 mm in
diameter were analyzed separately to the nodules measuring <10
mm in diameter. The accuracy of the CT-guided biopsy capture
procedure on patients who did not have extensive lung disease (no
emphysema, pulmonary bullae, pulmonary fibrosis or interstitial
lung diseases) was analyzed. Spirometry was not utilized to assess
lung function. In previous studies, emphysema, interstitial lung
disease and pulmonary fibrosis were confounding factors affecting
biopsy accuracy; therefore, such patients were excluded from the
present study (8,10,15).
Thirdly, only biopsies containing sufficient tissue for
pathological examination were included in the analysis, which
created a bias. Furthermore, the patients' smoking history, which
may have influenced the pathology of the nodules, was not included
in the analysis. Finally, unintentionally, the study group was
young (mean age, 54 years). Further studies are required to
determine whether the results of the present study are applicable
to patients with emphysema or other lung diseases.
In conclusion, CT-guided percutaneous lung biopsy is
an accurate and safe method for micro-invasive examinations. It has
an important role in harvesting a portion of an intrapulmonary
lesion (particularly a nodule of ≤30 mm in diameter). Nodule size
and the adhesion of the nodule to the pleura are major factors
affecting the accuracy of biopsy. Mastering the techniques for
biopsy of small nodules and rationally utilizing the natural
advantage of nodule adherence to the pleura may increase biopsy
accuracy. The rate of complications in the present study was only
associated with the lesion size.
References
|
1
|
Wu CC, Maher MM and Shepard JA:
Complications of CT-guided percutaneous needle biopsy of the chest:
Prevention and management. AJR Am J Roentgenol. 196:W678–W682.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nour-Eldin NE, Alsubhi M, Naguib NN,
Lehnert T, Emam A, Beeres M, Bodelle B, Koitka K, Vogl TJ and
Jacobi V: Risk factor analysis of pulmonary hemorrhage complicating
CT-guided lung biopsy in coaxial and non-coaxial core biopsy
techniques in 650 patients. Eur J Radiol. 83:1945–1952. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Khan N, Jadoon H, Zaman M, Subhani A, Khan
AR and Ihsanullah M: Frequency and management outcome of
pneumothorax patients. J Ayub Med Coll Abbottabad. 21:122–124.
2009.
|
|
4
|
Lee IJ, Bae YA, Kim DG, Jung KS, Im HJ,
Lee K, Lee Y and Bae SH: Percutaneous needle aspiration biopsy
(PCNAB) of lung lesions: 5 years results with focusing on repeat
PCNAB. Eur J Radiol. 73:551–554. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sinner WN: Complications of percutaneous
transthoracic needle aspiration biopsy. Acta Radiol Diagn (Stockh).
17:813–828. 1976.PubMed/NCBI
|
|
6
|
Xu C, Hao K, Song Y, Yu L, Hou Z and Zhan
P: Early diagnosis of solitary pulmonary nodules. J Thorac Dis.
5:830–840. 2013.PubMed/NCBI
|
|
7
|
Laspas F, Roussakis A, Efthimiadou R,
Papaioannou D, Papadopoulos S and Andreou J: Percutaneous CT-guided
fine-needle aspiration of pulmonary lesions: Results and
complications in 409 patients. J Med Imaging Radiat Oncol.
52:458–462. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li Y, Du Y, Yang HF, Yu JH and Xu XX:
CT-guided percutaneous core needle biopsy for small (</=20 mm)
pulmonary lesions. Clin Radiol. 68:e43–e48. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hwang HS, Chung MJ, Lee JW, Shin SW and
Lee KS: C-arm cone-beam CT-guided percutaneous transthoracic lung
biopsy: Usefulness in evaluation of small pulmonary nodules. AJR Am
J Roentgenol. 195:W400–W407. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ohno Y, Hatabu H, Takenaka D, Higashino T,
Watanabe H, Ohbayashi C and Sugimura K: CT-guided transthoracic
needle aspiration biopsy of small (< or =20 mm) solitary
pulmonary nodules. AJR Am J Roentgenol. 180:1665–1669. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tsukada H, Satou T, Iwashima A and Souma
T: Diagnostic accuracy of CT-guided automated needle biopsy of lung
nodules. AJR Am J Roentgenol. 175:239–243. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Khouri NF, Stitik FP, Erozan YS, Gupta PK,
Kim WS, Scott WW Jr, Hamper UM, Mann RB, Eggleston JC and Baker RR:
Transthoracic needle aspiration biopsy of benign and malignant lung
lesions. AJR Am J Roentgenol. 144:281–288. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Khan MF, Straub R, Moghaddam SR, Maataoui
A, Gurung J, Wagner TO, Ackermann H, Thalhammer A, Vogl TJ and
Jacobi V: Variables affecting the risk of pneumothorax and
intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur
Radiol. 18:1356–1363. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tomiyama N, Yasuhara Y, Nakajima Y, Adachi
S, Arai Y, Kusumoto M, Eguchi K, Kuriyama K, Sakai F, Noguchi M, et
al: CT-guided needle biopsy of lung lesions: A survey of severe
complication based on 9783 biopsies in Japan. Eur J Radiol.
59:60–64. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Choi JW, Park CM, Goo JM, Park YK, Sung W,
Lee HJ, Lee SM, Ko JY and Shim MS: C-arm cone-beam CT-guided
percutaneous transthoracic needle biopsy of small (</=20 mm)
lung nodules: Diagnostic accuracy and complications in 161
patients. AJR Am J Roentgenol. 199:W322–W330. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ng YL, Patsios D, Roberts H, Walsham A,
Paul NS, Chung T, Herman S and Weisbrod G: CT-guided percutaneous
fine-needle aspiration biopsy of pulmonary nodules measuring 10 mm
or less. Clin Radiol. 63:272–277. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yeow KM, Su IH, Pan KT, Tsay PK, Lui KW,
Cheung YC and Chou AS: Risk factors of pneumothorax and bleeding:
Multivariate analysis of 660 CT-guided coaxial cutting needle lung
biopsies. Chest. 126:748–754. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Winer-Muram HT: The solitary pulmonary
nodule. Radiology. 239:34–49. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Remy-Jardin M, Remy J, Giraud F and
Marquette CH: Pulmonary nodules: Detection with thick-section
spiral CT versus conventional CT. Radiology. 187:513–520. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Berger WG, Erly WK, Krupinski EA, Standen
JR and Stern RG: The solitary pulmonary nodule on chest
radiography: Can we really tell if the nodule is calcified? AJR Am
J Roentgenol. 176:201–204. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li H, Boiselle PM, Shepard JO,
Trotman-Dickenson B and McLoud TC: Diagnostic accuracy and safety
of CT-guided percutaneous needle aspiration biopsy of the lung:
Comparison of small and large pulmonary nodules. AJR Am J
Roentgenol. 167:105–109. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Capalbo E, Peli M, Lovisatti M, Cosentino
M, Mariani P, Berti E and Cariati M: Trans-thoracic biopsy of lung
lesions: FNAB or CNB? Our experience and review of the literature.
Radiol Med. 119:572–594. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yamagami T, Iida S, Kato T, Tanaka O and
Nishimura T: Combining fine-needle aspiration and core biopsy under
CT fluoroscopy guidance: A better way to treat patients with lung
nodules? AJR Am J Roentgenol. 180:811–815. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Boskovic T, Stanic J, Pena-Karan S,
Zarogoulidis P, Drevelegas K, Katsikogiannis N, Machairiotis N,
Mpakas A, Tsakiridis K, Kesisis G, et al: Pneumothorax after
transthoracic needle biopsy of lung lesions under CT guidance. J
Thorac Dis. 6:(Suppl 1). S99–S107. 2014.PubMed/NCBI
|
|
25
|
Yang HH, Liu JJ and Tang XH:
Ultrasound-guided percutaneous biopsy of peripheral pulmonary
lesions: Factors influencing success rate. Chinese Journal of
Medical Imaging. 22:117–120. 2014.
|
|
26
|
Hwang HS, Chung MJ, Lee JW, Shin SW and
Lee KS: C-arm cone-beam ct-guided percutaneous transthoracic lung
biopsy: Usefulness in evaluation of small pulmonary nodules. AJR.
195:W400–W407. 2010. View Article : Google Scholar : PubMed/NCBI
|