Introduction
Pulmonary aspergillosis is an infectious disease
caused by Aspergillus and one of its special types is
pulmonary aspergilloma, most of which is secondary to pulmonary
tuberculosis. Its main clinical symptoms are repeated hemoptysis
and features are repetition, deferment and different amounts of
hemoptysis, in most cases. General symptoms are slight but some
patients have unmanageable massive hemoptysis (hemoptysis amount
>500 ml/day or hemoptysis amount at one time >300 ml)
(1), indicating rare clinical acute
lung disease, for which medical hemostatic drugs are not
effective.
Currently, most Chinese scholars insist on surgery,
which has achieved good results (2,3), but
some patients are not willing to receive surgery or cannot
withstand surgery. To explore the intervention embolotherapy
effects, a retrospective analysis was performed on the intervention
treatment of 25 massive hemoptysis of pulmonary aspergilloma cases.
The study is presented in detail in the following sections.
Materials and methods
General materials
Twenty-five massive hemoptysis of pulmonary
aspergilloma cases diagnosed in the Second People's Hospital of
Weifang (Shandong, China) from 2008 to 2016 were chosen as study
subjects. Of these 25 cases, 11 were males and 4 females, aged
20–78 years and an average of 56.5±5.2 years. Location of
aspergilloma: 12 cases on superior lobe of the right lung, 3 cases
on inferior lobe of the right lung, 8 cases on superior lobe of the
left lung, and 2 cases on inferior lobe of the left lung. The
diameter of focus was 2–8 cm. Sputum smear, or sputum culture was
performed before surgery, and 3 cases were positive lung
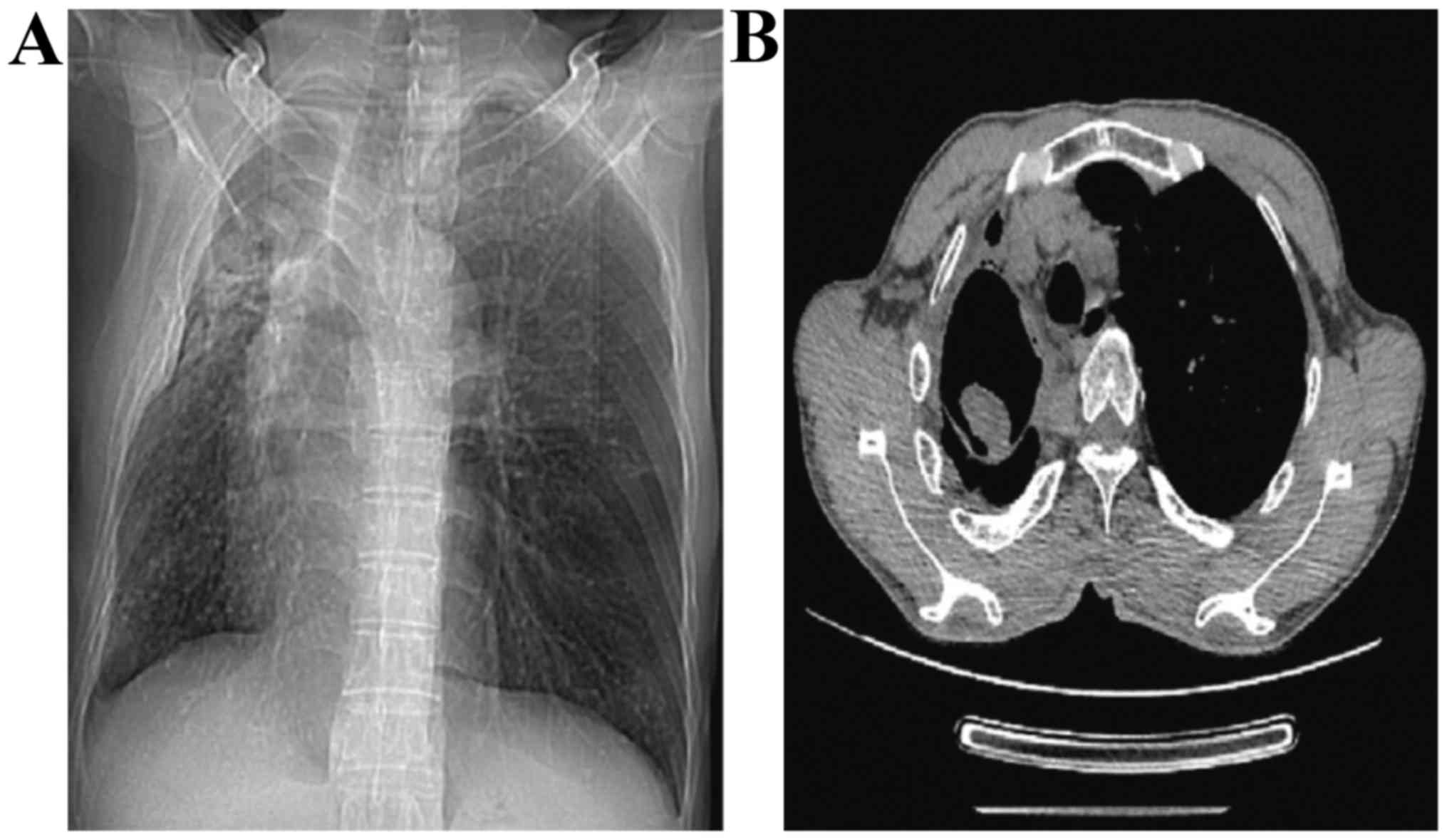
aspergillosis. Chest computed tomography (CT) showed 10 cases with
representative massive shadow with ‘meniscus sign’ (Fig. 1), 5 cases received skin puncture lung
biopsy, and 7 cases received bronchoscopic biopsy. This study was
approved by the Ethics Committee of the Second People's Hospital of
Weifang. Signed written informed consents were obtained from all
participants before the study.
Clinical manifestation
With hemoptysis as the main clinical symptom which
repeatedly occurs and lasts for a long time and cannot be treated
through conventional medical treatment, the course of disease is
long for most patients and their nutrition condition is poor, with
pale appearance, low immunity and general symptoms such as fever,
yellow sputum, and weakness if complicated with bacterial
infection.
Surgical method
Under local anesthesia, Seldinger technology was
used to puncture femoral artery at one side. Subsequently, we
placed 4F arterial sheath, selected the proper catheter (Cobra,
Simmon) to perform bronchial arteriesa imaging and then observed
for signs of increasing or expanding of bronchial arteries and
concentration or leakage of contrast medium (Yangze Pharma,
Taizhou, China). After defining the offending artery, 2.7F
microcatheter was chosen to perform super-selective catheterization
and to perform embolotherapy over ostium of intercostal artery.
Polyvinyl alcohol (PVA) particle (Yangze Pharma) was chosen as a
common embolic agent (diameter, 500–700 µm) and injected using
low-pressure flow control method to avoid embolus backflow. If
combined with obvious pulmonary artery fistula, the larger diameter
gelatin sponge sections were used and PVA particulate embolization
was performed. For obviously expanded bronchial arteries, if PVA
particulate embolization was not ideal, then spring coil or
N-butyl cyanoacrylate (NBCA) glue was used to continue
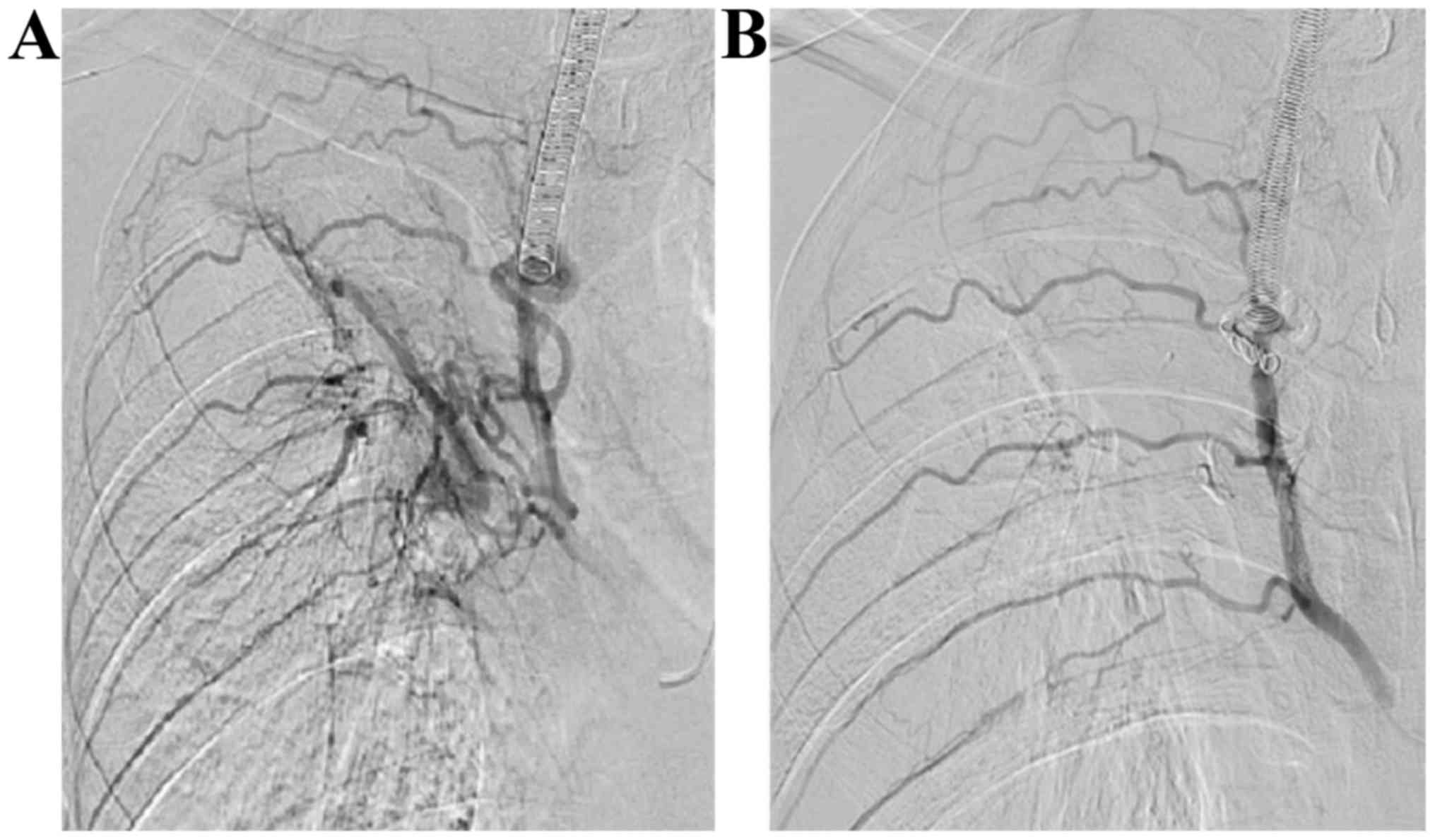
embolism (Fig. 2) until the blood
flow of the offending artery was retarded or embolism was arrested
after contrast media flow back. Following digital subtraction
angiography (DSA) radiography, the embolism was considered
successful when abnormal staining at distant end disappeared. Since
there are a large amount of bronchial arteries, all of them were
observed carefully one by one. Besides observing bronchial
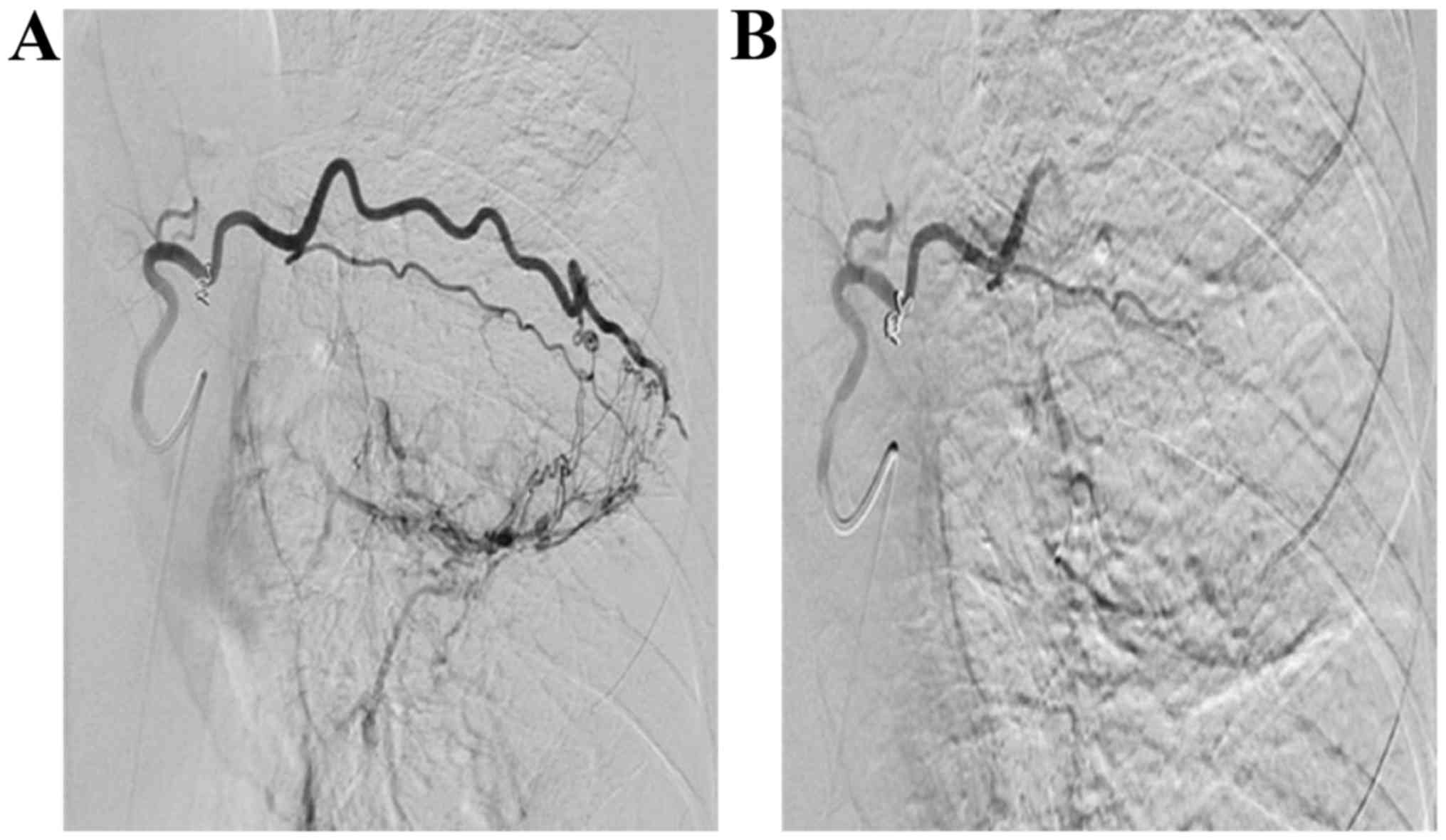
arteries, the intercostal artery (Fig.
3), internal thoracic artery, inferior phrenic artery and
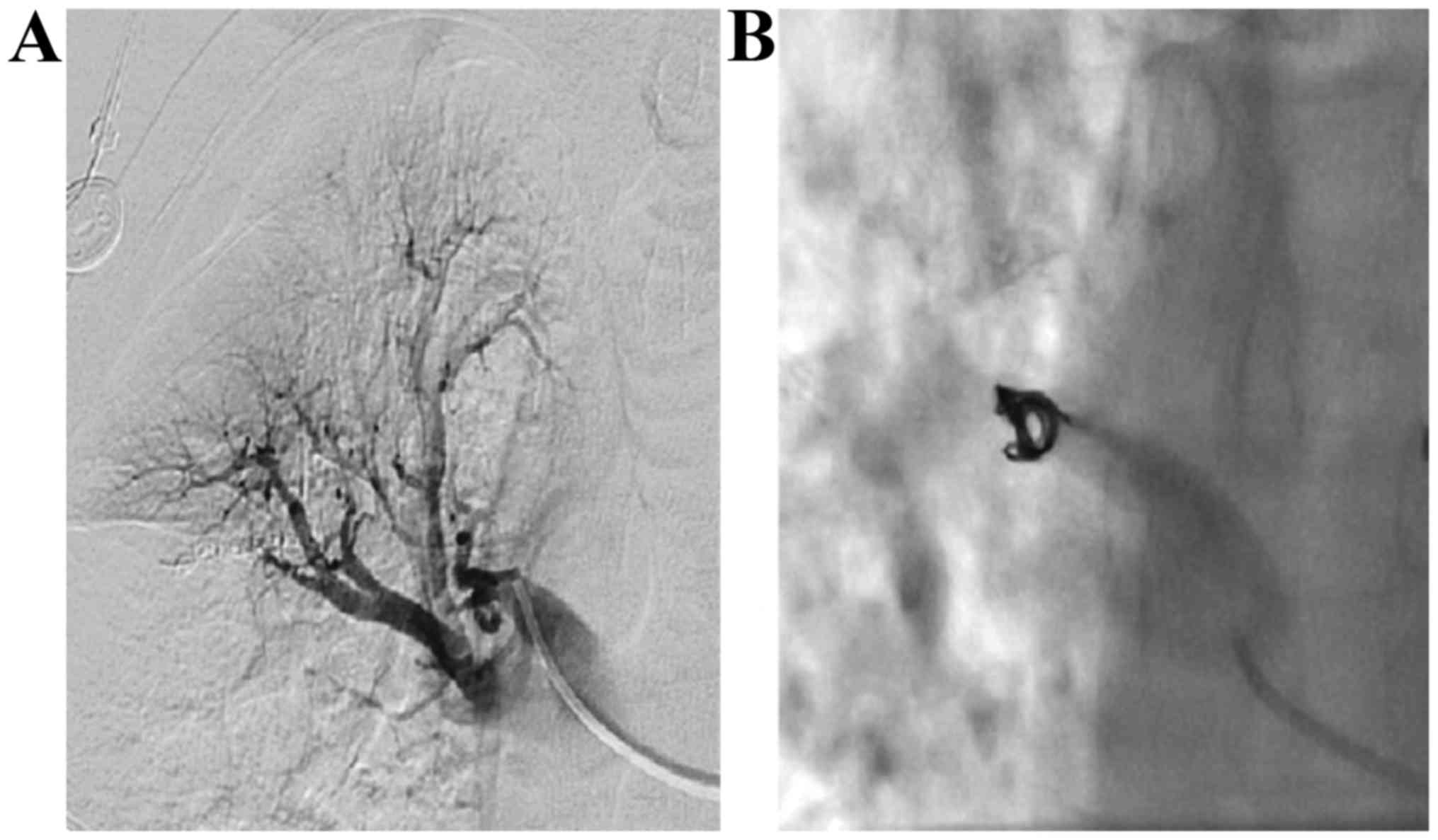
pulmonary artery need to be checked for (Fig. 4) sources of bleeding. In addition,
spinal arteries or its communicating branches need to be avoided
during embolism. When removing the sheath after surgery, the
puncture point is pressed for 15–20 min to stop bleeding with
compression bandage, and then patient conditions were observed
carefully for 2 weeks on anti-fungal therapy to avoid relapse.
Results
Through radiography, 68 embolism offending arteries
were found, among 36 bronchial arteries (52.94%), 15 intercostal
arteries (22.06%), 9 internal thoracic arteries (16.17%), 5
inferior phrenic arteries (7.35%), and 3 pulmonary arterial
branches (4.41%). Vital signs of 25 patients after surgery were
stable with no death during perioperative period or complications
such as spinal cord injury, intercostal cutaneous necrosis,
substernal burning sensation or bronchoesophageal fistula.
Massive hemoptysis of 21 cases stopped after
embolotherapy immediately and the effective rate of embolism was
84.00%; for 3 cases, massive hemoptysis occured within 24 h and it
was stopped through second imaging with embolism; 1 patient had a
small amount of hemoptysis after surgery and it was stopped after
corresponding medical treatment; in addition, 10 cases were treated
with PVA particulate embolization solely, 12 cases with PVA with
spring coil and 3 cases with PVA, spring coil, and NBCA glue.
Discussion
Pulmonary aspergillosis is closely related to basic
diseases of lung, most cases are secondary to diseases such as
pulmonary tuberculosis, bronchiectasia, pulmonary cystic fibrosis,
pulmonary cyst, and lung cancer and it is reported that the ratio
of cases secondary to pulmonary tuberculosis is 80.2% (4). Aspergillus parasiticus is easily
formed on the upper respiratory tract and diseases are caused when
organism immunity is low. Aspergillosis can multiply within cavity
and characteristic aspergilloma will be formed with a large amount
of mycelium mixing with bleeding sphacelus, fibrous protein,
mucosa, epithelial cell and inflammatory necrosis cells. Besides
purulent hemorrhagic inflammation of inflammatory granulation
tissue, aspergilloma will also cause necrosis and bleeding of
tissues and vessels due to its erosion of blood vessels by active
enzyme toxins; in addition, rich vasoganglion even arterial
aneurysm will be formed due to inflammatory stimulation around the
lesion, its mechanical motion will invade intercostal and bronchus
arteries to cause angiorrhexis and massive hemoptysis with
life-threathening risks (5). There
are great difficulties for medical treatment of massive hemoptysis,
which has no obvious effects; surgical removal provides a radical
treatment method, which is considered as the first option (6,7), but
most old patients are also suffering from lung diseases such as
pulmonary tuberculosis, pneumoconiosis, and bronchiectasia, the
lung function has decreased severely so the risks of surgery are
greatly increased.
Bronchial artery embolization (BAE) was first
suggested in 1974 and it has become the most effective method of
controlling massive hemoptysis currently through 40 years of
developing and improving, which is featured by being safe,
minimally invasive and highly efficient and its success rate of
hemostasis is more than 90% (8). In
our cases embolism was performed in 25 cases, of these hemoptysis
in 21 cases was stopped immediately and the effective rate was
84.00%, and it basically agrees with other reports. In order to
improve the successful rate of BAE, it is believed by us that the
following items should be paid attention to during surgery: i)
Finding of all offending arteries. The main resource is bronchial
artery and the opening is at the thoracic anterior aortic wall or
side wall of 5th to 6th thoracic vertebrae, in most cases, there
are 1–2 on the right and 2–4 on the left. About 1/3 cases have
bronchial arteries on both sides from one stem and when the
catheter is passing through, there is a hooking sensation. For a
small number of cases, it is from internal thoracic artery,
intercostal artery, subclavian artery, phrenicartery and
thyrocervical trunk. In order to improve the successful rate of
embolism, chest CT scanning is to be performed before surgery to
determine the bleeding location within lung and the surroundings.
All offending arteries need to be found according to lesion
location. If the lesion is at lobus inferior pulmonis, then
phrenicartery needs to be located, if the lesion is at anterior
upper lung lobe, then subclavian artery, internal thoracic artery,
and axillary artery are targets. Corresponding intercostal arteries
shall be considered if there is local pleural thickening. If the
above-mentioned systemic circulation branches are normal, then it
may be due to pulmonary artery bleeding. In this study, 1 case had
massive hemoptysis within 24 h after surgery, and abnormal
pulmonary artery was found during 2nd imaging and it was stopped
through another embolotherapy of massive hemoptysis. Therefore,
chest CTA before surgery can well define the offending artery,
which will save surgery time and greatly improve the success rate
of surgery. ii) Choosing proper embolic agent. PVA particle and
spring coil are common embolic agents, the first one is cheap and
permanent nonantigenic embolic agent, the common diameter is
500–700 µm, the embolism will be incomplete if the diameter is too
large, and it will cause injuries to vascular bed of arteries if
the diameter is too small. After re-examination of DSA, gelatin
sponge pieces, spring coil or NBCA glue can be added if the blood
flow is too fast for accurate location and permanent hemostasis. It
has been revealed in study that there are different diameters of
embolic agent, compact embolism is able to prevent bleeding
arteries from establishing collateral circulation, and effects of
combined embolism with more than 2 groups are better than one
single embolic agent (9). iii)
Avoiding spinal cord injury and ectopic embolism. The most severe
complication of BAE is spinal cord injury and its incidence rate is
2–3%, and its main manifestations are transverse sensation and
dyskinesia, once it occurs, hormone, vascular dilation and
neuro-nutrition drug treatments should be positively performed.
Most patients will partially or completely recover within weeks or
months, but some patients may have permanent injuries. After
bronchial artery radiography, the results need to be read
carefully, super-selective microcatheter is used when there is
hairpin running anterior spinal artery; PVA particulate with
diameter >500 µm is used in embolization to avoid embolism of
anterior spinal artery. In addition, embolism process needs to be
gentle to avoid ectopic embolism outside the offending arteries
caused by fast injection rate of embolic agent and large pressure.
There are no severe complications for patients in this group, and
it is considered that it may be related to careful angiography,
super-selective catheterization and application of microcatheter
before embolism. No special treatments are needed generally for
other complications such as low-grade fever, intercostal pain,
substernal burning sensation, or dysphagia.
Above all, for patients who suffer from massive
hemoptysis of pulmonary aspergilloma and their medical treatments
are not effective and they have no surgery conditions, bronchial
arteries embolism technique is a simple and effective method as
salvage hemostasis method. Good understanding of the indications
and complete and thorough embolism of bleeding arteries is the key
of successful surgery.
References
|
1
|
Brown HA, Aruny JE, Elefteriades JA and
Sumpio BE: Subclavian aneurysm presenting with massive hemoptysis:
a case report and review of the literature. Int J Angiol. 22:69–74.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Babatasi G, Massetti M, Chapelier A, Fadel
E, Macchiarini P, Khayat A and Dartevelle P: Surgical treatment of
pulmonary aspergilloma: Current outcome. J Thorac Cardiovasc Surg.
119:906–912. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aydoğdu K, İncekara F, Şahin MF, Gülhan
SS, Findik G, Taştepe İ and Kaya S: Surgical management of
pulmonary aspergilloma: clinical experience with 77 cases. Turk J
Med Sci. 45:431–437. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee JG, Lee CY, Park IK, Kim DJ, Chang J,
Kim SK and Chung KY: Pulmonary aspergilloma: analysis of prognosis
in relation to symptoms and treatment. J Thorac Cardiovasc Surg.
138:820–825. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Muniappan A, Tapias LF, Butala P, Wain JC,
Wright CD, Donahue DM, Gaissert HA, Lanuti M and Mathisen DJ:
Surgical therapy of pulmonary aspergillomas: a 30-year North
American experience. Ann Thorac Surg. 97:432–438. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ichinose J, Kohno T and Fujimori S:
Video-assisted thoracic surgery for pulmonary aspergilloma.
Interact Cardiovasc Thorac Surg. 10:927–930. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gezer S, Taştepe I, Sirmali M, Findik G,
Türüt H, Kaya S, Karaoğlanoğlu N and Cetin G: Pulmonary
sequestration: a single-institutional series composed of 27 cases.
J Thorac Cardiovasc Surg. 133:955–959. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alexander GR: A retrospective review
comparing the treatment outcomes of emergency lung resection for
massive haemoptysis with and without preoperative bronchial artery
embolization. Eur J Cardiothorac Surg. 45:251–255. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lorenz J, Sheth D and Patel J: Bronchial
artery embolization. Semin Intervent Radiol. 29:155–160. 2012.
View Article : Google Scholar : PubMed/NCBI
|