Introduction
Colorectal cancer (CRC) is one of the most common
types of malignancy worldwide (1).
Although surgery is the most effective treatment option for CRC,
chemotherapy is also used to control tumor growth and reduce
recurrence (2). The application of
novel antitumor drugs has improved the prognosis of CRC; however,
intrinsic or acquired chemoresistance is frequently encountered
during chemotherapy (3). Therefore,
there it is necessary to understand the molecular mechanisms
underlying drug resistance.
Paclitaxel, a member of the taxane class of agents,
has been widely used as an antineoplastic agent for >20 years
and is effective in the treatment of a number of types of cancer
and other malignancies (4–6). Paclitaxel binds to tubulin and
stabilizes microtubule filaments to induce mitotic arrest during
the G2/M phase and promote apoptosis (7). However, as a single agent, paclitaxel
has low cytotoxicity in adenocarcinoma of the colon or rectum
(8). There are multiple known
mechanisms of paclitaxel resistance, such as microtubule mutations
(9), upregulation of survivin
expression (10) and protein kinase
B/extracellular signal-regulated kinase activation (11), and additional factors continue to be
evaluated.
Previous studies have demonstrated that connexins, a
group of tumor suppressor genes, are potential anti-oncogenic
targets for chemotherapy, and the upregulation of connexin
expression can increase sensitivity to antitumor drugs in many
cancer types (12,13). Connexins form gap junctions, which
are important intercellular channels. The downregulation of
connexin expression and loss of gap junctional communication (GJC)
are important events in carcinogenesis (14). Connexin 43 (Cx43) is a member of the
gap junction protein family of connexins and is widely expressed in
different tissues to provide GJC (15). Expression of Cx43 is reduced in many
types of cancer; however, some cancer cell lines exhibit a
substantial level of Cx43 expression, such as human mammary
carcinoma (16) and CRC (17). Thus, it was speculated that Cx43
expression level may be associated with paclitaxel cytotoxicity in
CRC.
In the present study, the influence of Cx43
expression on paclitaxel cytotoxicity was evaluated in three CRC
cell lines. The results of this study may be relevant in the
development of a new paclitaxel-based chemotherapy strategy for
patients with CRC and a high level of Cx43 expression.
Materials and methods
Reagents and antibodies
All cell culture media, trypsin and antibiotics were
purchased from Gibco (Thermo Fisher Scientific, Inc., Waltham, MA,
USA), and fetal bovine serum (FBS) was purchased from HyClone (GE
Healthcare Life Sciences, Logan, UT, USA). Rabbit anti-Cx43
polyclonal antibody (C6219), rabbit anti-caspase-3 polyclonal
antibody (C9598), rabbit anti-survivin polyclonal antibody
(SAB3500269), rabbit anti-α-tubulin polyclonal antibody
(SAB4500087), rabbit anti-cyclin B1 polyclonal antibody (C8831),
rabbit anti-β-actin polyclonal antibody (SAB2100037), anti-rabbit
IgG-peroxidase antibody (SAB3700870), MTT, neomycin (G418) and
paclitaxel were purchased from Sigma-Aldrich (Merck KGaA,
Darmstadt, Germany). Rabbit anti-ATPase β3
(Na+/K+) polyclonal antibody (GTX114272) was
purchased from GeneTex, Inc. (Irvine, CA, USA). ProteoExtract
Native Membrane Protein Extraction kit and Immobilon membranes were
purchased from EMD Millipore (Billerica, MA, USA). pTARGET
Mammalian Expression Vector system was purchased from Promega
Corporation (Madison, WI, USA). Lipofectamine reagent was purchased
from Invitrogen (Thermo Fisher Scientific, Inc.). Electrochemical
Luminescence (ECL) Plus substrate, bicinchoninic acid (BCA)
reagents and radioimmunoprecipitation (RIPA) lysis buffer were
purchased from CWBio (Beijing, China).
Cell lines
Human colorectal carcinoma cell lines HCT106,
HCT116, LoVo were donated by Dr Shiwu Zhang, Department of
Pathology, Tianjin Union Medical Center (Tianjin, China). All cell
lines were cultured at 37°C in an atmosphere containing 5%
CO2 in RPMI-1640 medium supplemented with 10% FBS, 100
U/ml penicillin and 100 µg/ml streptomycin.
Cx43 transfection
Total RNA was extracted from LoVo cells at
confluence by TRIzol (Invitrogen; Thermo Fisher Scientific, Inc.).
A total of 5 µg of total RNA was used for cDNA synthesis using
BeyoRT cDNA synthesis kit (D7166; Beyotime Institute of
Biotechnology, Haimen, China). The reverse transcription reaction
mixture contained 5 µg total RNA, 1 µl random hexamer primer and
diethyl pyrocarbonate -treated water to produce a final volume of
12 µl. After incubation in 70°C for 5 min, the mixture was cool
down on ice, the following agents were added: 4 µl reaction buffer,
1 µl RNase inhibitor, 2 µl dNTP mix and 1 µl reverse transcriptase.
The mixture was gently mixed and centrifuged transiently at 6,000 ×
g at 4°C. The supernatant was incubated at 25°C for 10 min and 42°C
for 60 min. The reaction was terminated by incubation at 70°C for
10 min and the product was used for the following polymerase chain
reaction (PCR). cDNA of the human Cx43 coding region was amplified
by PCR using PCR kit with Taq (D7232; Beyotime Institute of
Biotechnology) according to the manufacturer's instructions. The
Cx43 primers used were as follows: forward,
5′-cacaattgagtggaatcttgatg-3′; reverse, 5′-caa cat ggg tga ctg gag
c-3′. β-actin was used as the control. The β-actin primers used
were as follows: forward, 5′-gtg ggg cgc ccc agg cac ca-3′;
reverse, 5′-cttccttaatgtcacgcacgatttc-3′. The PCR reaction mixture
contained 5 µl 10xPCR buffer, 4 µl 2.5 mM dNTP, 0.1 µg template, 2
µl primers, 0.25 µl Taq DNA polymerase, and was added to 50 µl of
total volume by double distilled water. The PCR profile was 94°C
for 30 sec, 55°C for 30 sec, and 72°C for 60 sec for 30 cycles,
followed by 72°C for 10 min. The results were analyzed and
quantified by Quantity One software (v4.62; Bio-Rad Laboratories,
Inc., Hercules, CA, USA). A total of 45 ng purified PCR product was
inserted into 140 ng pTARGET vector (A1410; Promega Corporation,
Madison, WI, USA). Constructed expression vector (0.8
µg/106 cells) was transfected into the aforementioned
three cell lines by lipofection using Lipofectamine reagent,
according to the manufacturer's protocol. After transfection,
cultures were selected with 400 µg/ml G418. Cells of subclones were
diluted and seeded to obtain further clones.
Parachute dye-coupling assay
Functional GJC of transfected and paclitaxel-treated
cells was evaluated as described by Wang et al (18). Briefly, cells for analysis were grown
to confluence in 6-well plates. Two fluorescent dyes, CM-Dil and
Calcein-AM, were used to analyze GJC function. CM-Dil is a membrane
dye that is not able to spread to coupled cells. Calcein-AM can be
converted intracellularly into the GJC-permeable dye calcein
(18). Donor cells in one well were
stained with fresh culture medium containing 10 µg/ml calcein-AM
and 5 µg/ml CM-Dil for 30 min at 37°C. After this incubation, donor
cells were washed with culture medium three times to remove
unincorporated dye. Donor cells were then trypsinized and seeded
onto a monolayer of receiver cells grown in another well. Receiver
cells were cultured in a 6-wells plate at 37°C in an atmosphere
containing 5% CO2 to confluence (106
cells/well) when donor cells were seeded. The ratio of donor to
receiver was 1:150. Cells were cultured for 4 h at 37°C in order to
allow GJC between donor and receiver cells. GJC function was then
measured using a fluorescence microscope (Olympus CKX41; Olympus
Corporation, Tokyo, Japan). Red fluorescence of CM-Dil was used to
locate donor cells, and green fluorescence of calcein-AM was used
to calculate the average number of fluorescent receiver cells
around each donor cell. This number was used to represent the
degree of GJC function. Five fields of each group were used to
calculate.
Paclitaxel treatment and cell survival
assay
Stock solutions of 1 µM paclitaxel in dimethyl
sulfoxide were freshly prepared and added to wild type (WT) or
transfected cell lines at a series of concentrations (0, 1, 5, 20
and 80 nM). Cells with two culture densities (3×104 or
1×102 cells/cm2) were treated with paclitaxel
in a 37°C incubator for 48 h and then their viability was tested.
Briefly, cells were seeded into 6-well dishes. For high density
cultures, cells were seeded at 3×104
cells/cm2 density and exposed to paclitaxel when the
cells achieved 80–100% confluency, where GJC formation was
possible. For low density cultures, cells were seeded at
1×102 cells/cm2 density in 6-well dishes.
Following substrate attachment (at 10 h), the cultures were treated
with paclitaxel.
The inhibitory effects of paclitaxel on cell
viability were evaluated using a cell survival assay. Briefly, 20
µl 5 mg/ml MTT solution was added to each well after exposure to
paclitaxel for 24 h, and the cells were incubated for 4 h at 37°C.
The cell medium was removed, and 100 µl DMSO was added to dissolve
the purple formazan crystals. After 10 min of slow vibration,
fluorescence was monitored at a wavelength of 490 nm. Cell
viability was calculated as a percentage, where the absorption of
cells not treated with paclitaxel (control group) was considered to
be 100%. The experiment was repeated three times for each cell
line.
Western blot analysis
Cx43 expression in the membrane of WT and
transfected cells was analyzed by western blotting. The WT and
transfected clones of the three cell lines were identified.
Briefly, the membrane proteins of cells were extracted using a
ProteoExtract Native Membrane Protein Extraction kit, according to
the manufacturer's instructions, and subjected to western blot
analysis of Cx43. Protein content was quantified using BCA reagent.
Protein samples were suspended in SDS loading buffer (Beyotime
Institute of Biotechnology). After boiling, 50 µg proteins were run
on 12% SDS-PAGE gels, then transferred to Immobilon membranes by
the semi-dry blot method. ATPase β3 was used as a loading control.
The membranes were blocked by blocking reagent (P0023B; Beyotime
Institute of Biotechnology) at room temperature for 1 h. The
membranes were probed with anti-Cx43 antibody (1:4,000) and
anti-ATPase β3 (1:4,000) antibody at room temperature for 1 h, then
with anti-rabbit IgG-peroxidase (1:10,000) at room temperature for
1 h using standard techniques. The signals were visualized using
ECL Plus and exposed film. Expression levels were quantified using
Quantity One software (v4.62; Bio-Rad Laboratories, Inc., Hercules,
CA, USA) and normalized against ATPase β3.
For further analysis of other proteins, high density
cultured cells were treated with 80 nM paclitaxel at 37°C in an
atmosphere containing 5% CO2, and harvested after 12 h
of treatment. For the survivin and cyclin B1 expression assays and
detection of caspase-3 cleavage, harvested cells were lysed with
RIPA lysis buffer supplemented with protease inhibitor mixture
(Roche Applied Science, Penzberg, Germany). Cell lysate was used
for the western blot assay method described below.
For the detection of α-tubulin polymerization
levels, soluble and polymerized tubulins in cell lysate were
separated according to a previously published method (19). In brief, the harvested cells
(1×106 cells) were lysed at 37°C with 100 µl hypotonic
buffer [1 mM MgCl2, 20 mM Tris-HCl (pH 6.8), 2 mM EGTA,
0.5% NP-40, protease inhibitor mixture] for 5 min in the dark. The
cell lysate was treated with an additional 100 µl hypotonic buffer
and vortexed briefly, then sonicated on ice. The cell lysate was
centrifuged at 10,000 × g for 10 min at room temperature. The
supernatant contained the soluble tubulin and the pellet fraction
included polymerized tubulin. The pellets were resuspended in 200
ml of hypotonic buffer. Expression levels of soluble and
polymerized α-tubulin were determined by analysis of the
supernatant and resuspended pellets, respectively. The percentage
of polymerized tubulin was determined by dividing the densitometric
value for polymerized tubulin by the total tubulin (polymerized +
soluble) densitometric value.
After quantification of protein concentration using
BCA reagents, equal amounts of proteins (20 µg/lane) were loaded
onto gel and separated by 12% SDS-PAGE. The gel was transferred to
Immobilon membranes by the semi-dry blot method. The membranes were
blocked using blocking reagent (P0023B; Beyotime Institute of
Biotechnology) at room temperature for 1 h. The membranes were
probed with anti-survivin (1:4,000), anti-cyclin B1 (1:4,000),
anti-α-tubulin (1:4,000), anti-caspase-3 (1:4,000), anti-β-actin
(1:3,000) primary antibodies at room temperature for 1 h and
anti-rabbit IgG-peroxidase secondary antibody (1:10,000) at room
temperature for 1 h. The signals were visualized by ECL. β-actin
was used as a loading control. Expression levels were quantified
using Quantity One software and normalized against β-actin. The
percentage of cleaved caspase-3 was determined by dividing the
densitometric value of cleaved caspase-3 by the total caspase-3
(cleaved + procaspase-3) densitometric value.
Statistical analysis
All data in figures represent the mean ± standard
deviation. Statistical analysis was performed by Student's t-test
using SPSS software (ver 17.0; SPSS, Inc., Chicago, IL, USA).
P<0.05 was considered to indicate a statistically significant
result.
Results
Confirmation of transfection and GJC
function
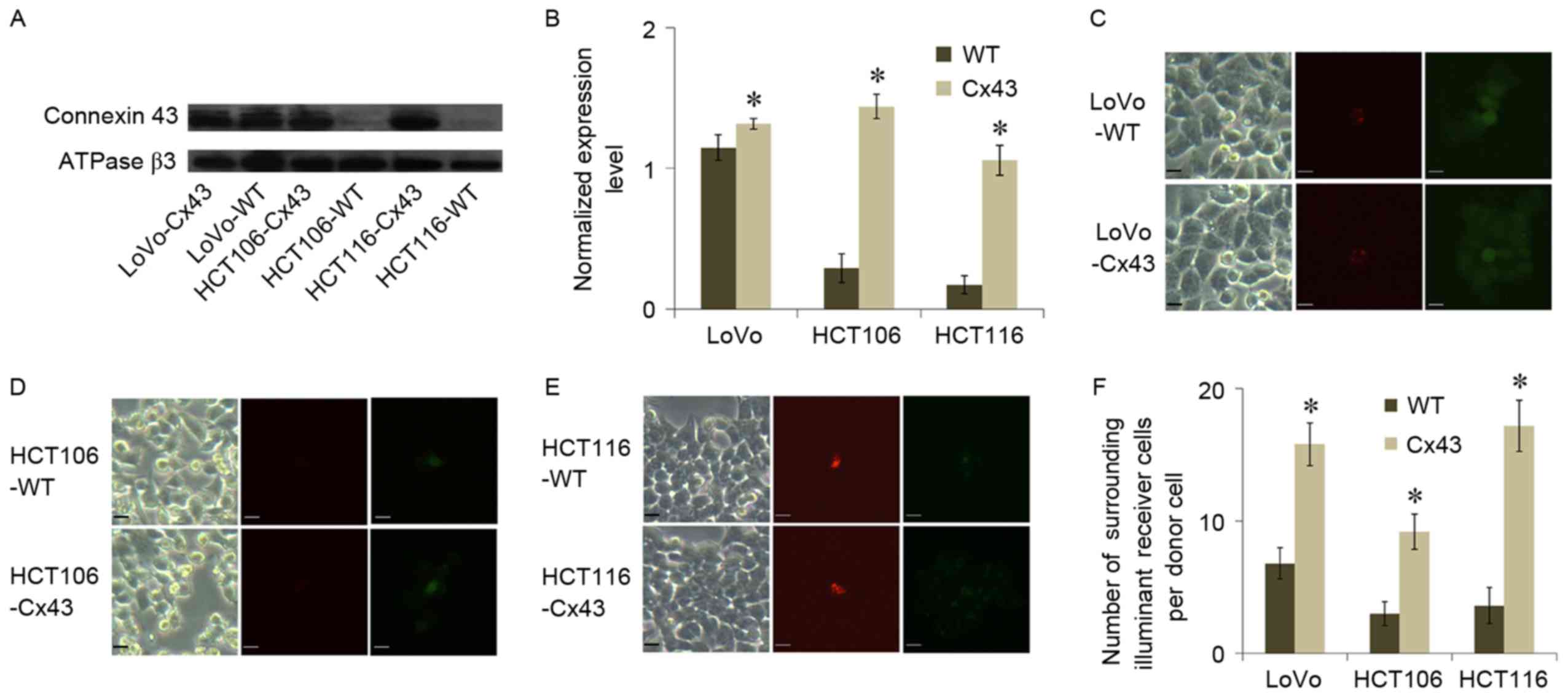
Membrane expression of Cx43 in WT and
Cx43-transfected cells of the three cell lines was analyzed using
western blot assays (Fig. 1A and B).
HCT106-WT and HCT116-WT exhibited a lower level of Cx43 expression
compared with LoVo-WT. All of the transfected cell lines exhibited
a significantly higher level of Cx43 expression compared with their
WT counterparts (P<0.05; Fig.
1B). The results of parachute dye-coupling assays also
suggested an association between GJC function and Cx43 expression.
All transfected cell lines exhibited a significantly higher level
of GJC function compared with their WT counterparts (P<0.05;
Fig. 1C-F). This evidence suggested
that GJC in transfected cells was associated with Cx43
expression.
Cx43 enhances paclitaxel-induced
apoptosis
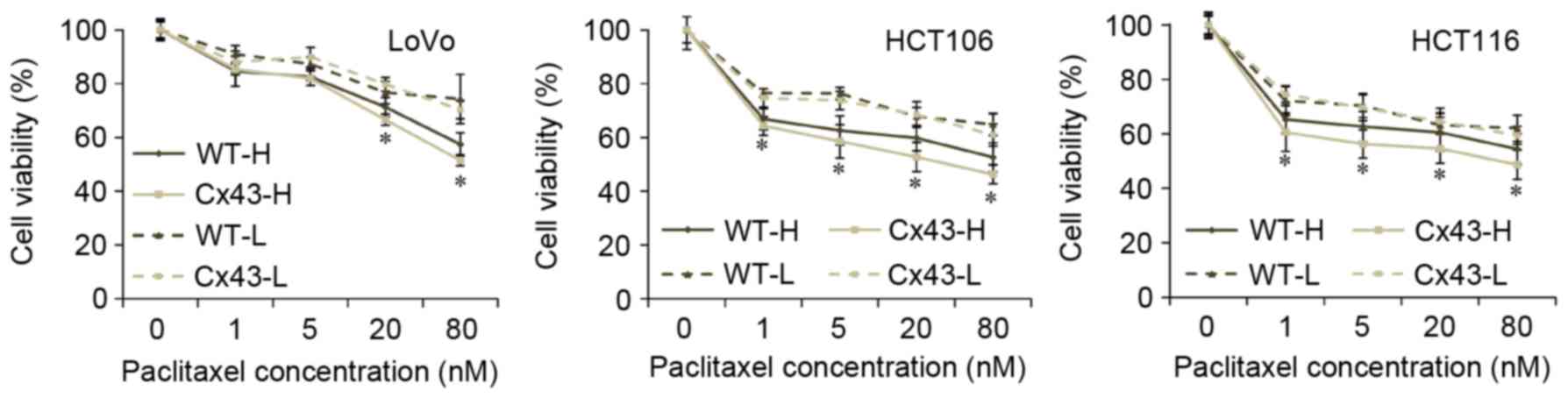
MTT assays indicated that the cytotoxicity of
paclitaxel differed between WT and transfected cells (Fig. 2). High culture density ensures GJC
function (20), and all transfected
cell lines with high culture density were significantly more
sensitive to paclitaxel compared with their WT counterparts when
they were treated with 20 or 80 nM paclitaxel (P<0.05). At lower
concentrations of paclitaxel treatment (1 or 5 nM), the cell
viability rates of HCT106 and HCT116 were also significantly
decreased by transfection with Cx43 (P<0.05 vs. WT). No
significant differences in viability rates existed between
transfected and WT cells when cells were seeded at low density.
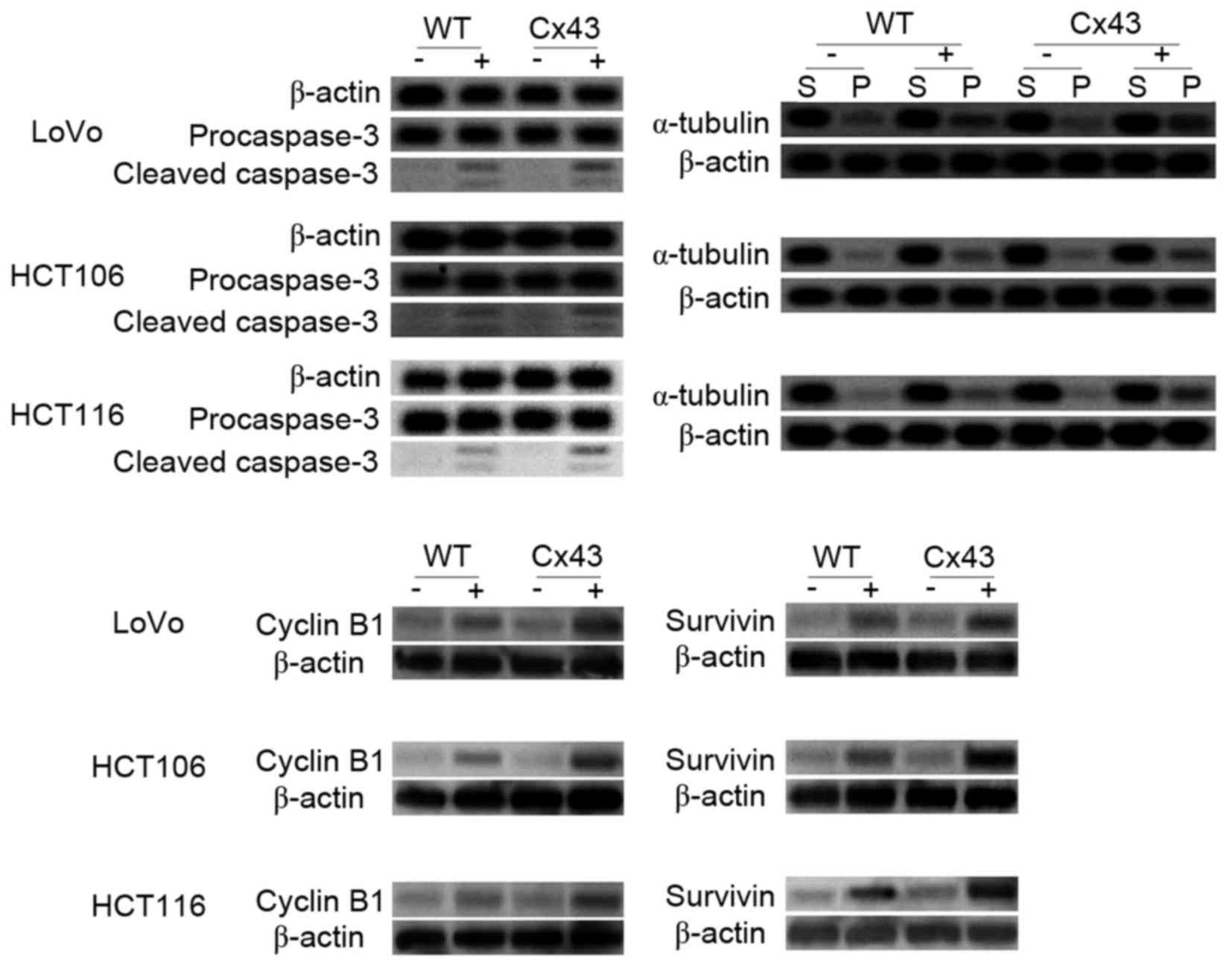
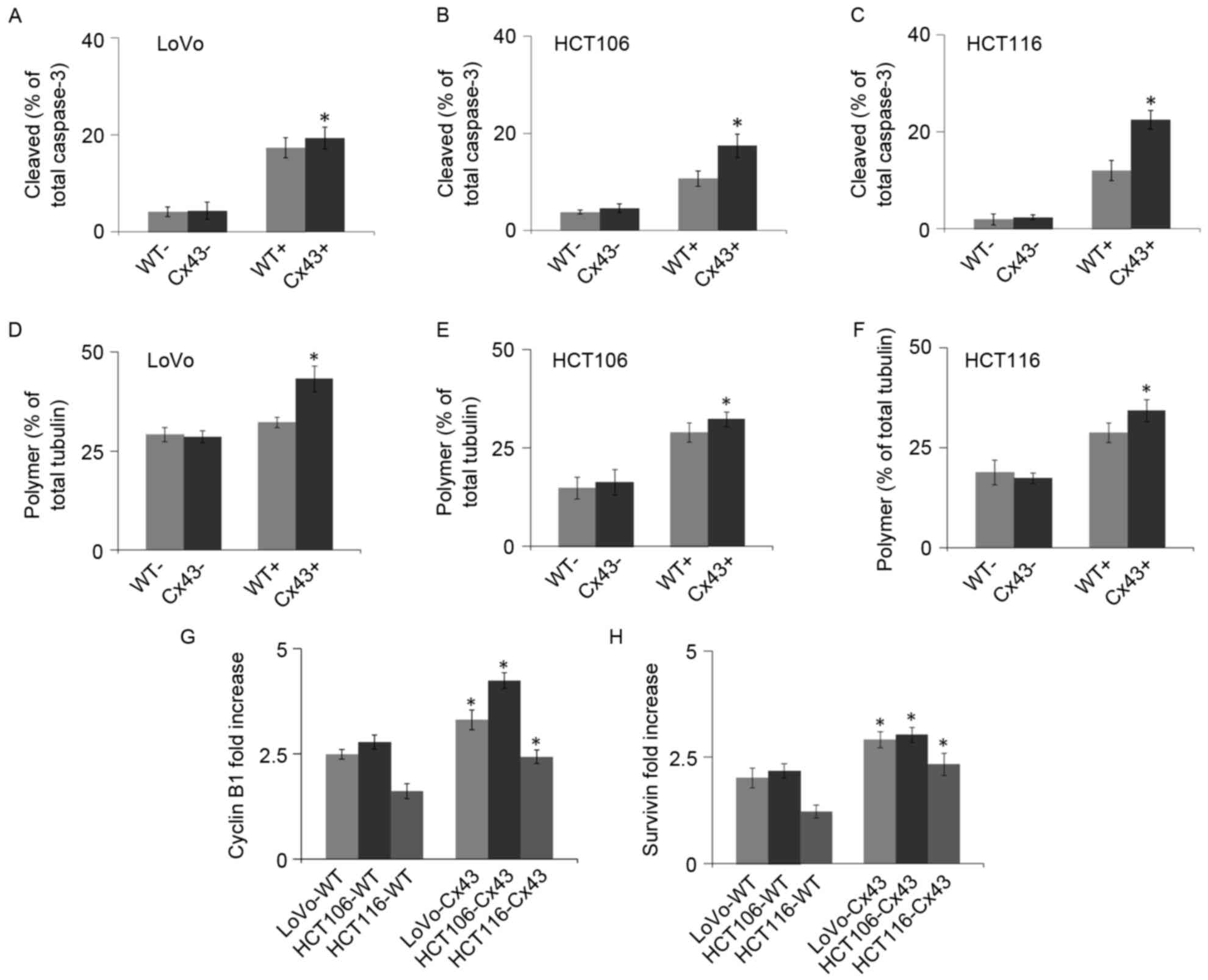
Caspase-3 is a frequently activated death protease. The activation
of caspase-3 occurs at an early stage of apoptosis (21). The analysis of caspase-3 revealed
that the activated (cleaved) form of caspase-3 was significantly
increased in paclitaxel-treated Cx43-transfected cells compared
with paclitaxel-treated WT cells from all three cell lines
(P<0.05; Figs. 3 and 4A-C). No significant differences in
caspase-3 activation were observed between untreated WT and
Cx43-transfected cells (Figs. 3 and
4A-C).
Cx43 enhances the effect of tubulin
polymerization caused by paclitaxel
Paclitaxel can bind to assembled tubulin and inhibit
microtubule disassembly to lock microtubules in a polymerized state
(22). As shown in Figs. 3 and 4D-F, western blotting results indicated
that paclitaxel increased microtubule assembly. This increase was
significantly higher in Cx43-transfected cells compared with their
WT counterparts (P<0.05). In the cells that were not treated
with paclitaxel, no significant differences in tubulin
polymerization were observed between WT and Cx43-transfected cells
(Figs. 3 and 4D-F).
Cx43 increases cyclin B1 and survivin
expression
Arrest of the cell cycle at mitotic phase is a
molecular mechanism of paclitaxel-induced cytotoxicity. Cyclin B1
is a regulatory protein involved in mitosis. It has a critical role
in regulating cyclin-dependent kinase 1, which initiates
progression from the G2 phase to mitosis (23). The quantity and activity of cyclin B1
increase through the cell cycle (24). As shown in Figs. 3 and 4G, the cyclin B1 expression levels in all
cells increased markedly after paclitaxel treatment. The increase
was significantly higher in transfected cells compared with their
WT counterparts (P<0.04). These results suggest that Cx43
promotes the mitotic arrest caused by paclitaxel.
Survivin is an anti-apoptotic protein that is highly
expressed in cancer. Paclitaxel-mediated mitotic arrest of cancer
cells is associated with survivin induction, and survivin
expression increases in the G2/M phase of cell cycle
(25). As shown in Figs. 3 and 4H, survivin expression levels increased
after paclitaxel treatment. This increase was significantly higher
in transfected cells compared with their WT counterparts
(P<0.05).
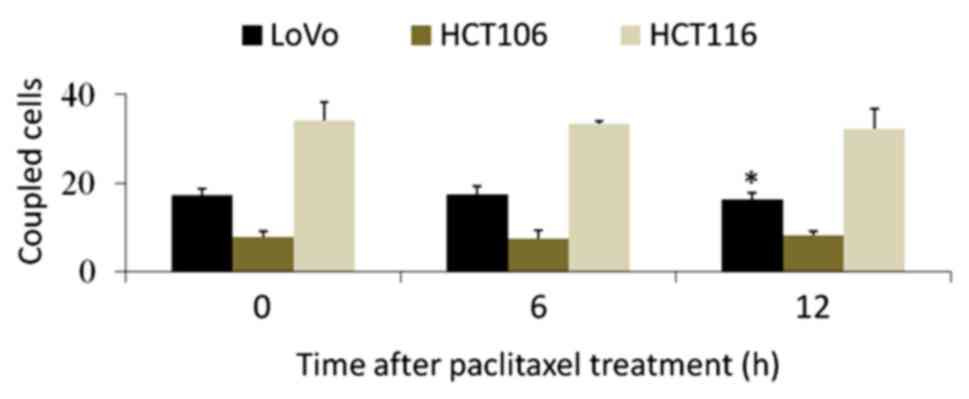
Effect of paclitaxel treatment on GJC
function
The parachute dye-coupling assay was used to
evaluate whether GJC function was inhibited by paclitaxel
treatment. GJC function was represented by the mean number of
coupled cells, and the results are shown in Fig. 5. No inhibitory effect on GJC function
in HCT106 or HCT116 cells was observed within 12 h of paclitaxel
treatment. LoVo exhibited a significant inhibition at 12 h but not
earlier. Cells with longer treatment times were not suitable for
the analysis of GJC function because they were reduced in size and
lost intercellular contact.
Discussion
Cx43 is a structural component of gap junctions,
which permits the transfer of small water-soluble molecules
(molecular weight <1 kDa) directly between cells without passing
through the cell membrane (14).
Paclitaxel and other small molecules involved in apoptosis can be
transferred through GJC and the cytotoxic effect is enhanced in
Cx43-transfected cells (26). The
effect of Cx43 on cytotoxicity varies in different cell types and
with different antitumor drugs. For example, Cx43 expression is
upregulated in glioblastoma multiforme cells, which are resistant
to a frontline antitumor drug, temozolomide (27). However, Cx43 enhances paclitaxel
cytotoxicity in HeLa cells (28) and
cisplatin cytotoxicity in mesothelioma cells (29). The mechanism of the effect of Cx43 on
antitumor drugs is complex; a previous study reported that Cx43
sensitized tumor testicular cells in response to cisplatin but
caused normal testicular cells to become resistant to cisplatin
(20). Therefore, three CRC cell
lines, LoVo, HCT106 and HCT116, were used in the present study in
order to perform a comprehensive analysis of the role of Cx43 in
CRC, and it was demonstrated that Cx43 enhanced paclitaxel
cytotoxicity in all three of these cell lines.
The expression levels of connexins differ in various
types of CRC. Immunohistochemical studies have reported that Cx26,
Cx32 and Cx43 are downregulated or relocalized in CRC (30,31).
These findings suggest that dysregulation of connexins and loss of
GJC may be early events in CRC development. However, other studies
have reported increased connexin expression in CRC. For example,
upregulated Cx43 expression was exhibited in advanced stages of CRC
(32), and high levels of Cx26 were
also identified in some colorectal patients with lung metastases
(33). Therefore, connexins may be
prognostic markers in CRC and are considered to be potential
targets for cancer chemoprevention and chemotherapy.
Previous studies have indicated that Cx43 is able to
sensitize cells to apoptosis in response to chemotherapeutic drugs
through GJC (18,28); however, another study reported that
the role of Cx43 in chemotherapy-induced apoptosis is independent
of GJC function (12). The results
of the MTT assay in the current study indicated a role for Cx43 in
mediating the apoptosis of CRC cell lines. Cx43-transfected cells
exhibited a lower viability rate when treated with paclitaxel (20
or 80 nM) than did their WT counterparts when they were cultured at
high density. When cells were sparsely seeded, they were not in
contact and not able to form GJC, and there was no significant
difference in apoptotic rate between Cx43-transfected cells and
their WT counterparts. This evidence indicates that upregulating
Cx43 expression level alone does not sensitize CRC cells to
paclitaxel, but GJC function increased by Cx43 can increase
sensitivity to paclitaxel when the cells are in contact with each
other.
Paclitaxel has long been recognized to induce
mitotic arrest and tubulin polymerization, both of which lead to
cell death (7). The current study
indicates that Cx43 promotes these effects in CRC cells. Despite WT
LoVo cells exhibiting considerable Cx43 expression levels, the GJC
function of these cells was enhanced by Cx43 transfection, and
paclitaxel displayed higher cytotoxicity on the transfected LoVo
cell line compared with its WT counterpart.
The current results suggest that paclitaxel
cytotoxicity is enhanced by Cx43 expression; however, it has
previously been reported that paclitaxel inhibits GJC in certain
cells, such as epithelial and cervical cancer cells (28,34). In
a previous study, researchers analyzed the effect of paclitaxel and
another agent in the taxane family, docetaxel, on GJC function in
HeLa cells. The results revealed that paclitaxel had a stronger
inhibitory effect on GJC compared with docetaxel, which resulted in
paclitaxel having reduced cytotoxicity compared with docetaxel
(28). The ability of paclitaxel to
inhibit GJC in CRC cells was investigated in the present study, and
no marked inhibitory effect occurred within 12 h of paclitaxel
treatment. Western blotting results also suggested that cells
transfected with Cx43 were more sensitive to paclitaxel than were
their WT counterparts at 12 h after treatment. These results
indicate that the cytotoxicity of paclitaxel was not notably
decreased by paclitaxel-induced GJC inhibition in CRC cells.
However, measurements of GJC function for longer times after
paclitaxel treatment may be inaccurate due to cell shrinkage, which
decreases intercellular contact.
In summary, the present study demonstrated the role
of Cx43 in paclitaxel-induced cytotoxicity in CRC cells. GJC
function in Cx43-transfected cells was upregulated compared with
their WT counterparts. The enhancement effect of Cx43 on
paclitaxel-induced cytotoxicity is dependent on GJC function. In
addition, Cx43 promotes other cellular responses to paclitaxel,
such as caspase-3 maturation, mitotic arrest and tubulin
polymerization. The current study offers a possible approach for
further in vitro and in vivo investigations
concerning the effects of Cx43 expression on paclitaxel-treated CRC
cells.
Acknowledgements
This study was supported by the Foundation of
Tianjin Health Bureau (grant nos. 2014KY27, 2014KY28 and 2014KR14),
the Foundation of the Committee on Science and Technology of
Tianjin (grant nos. 15JCQNJC42200 and 13JCYBJC42700), the National
Basic Research Program of China (grant no. 2016YFC0102404) and the
National Natural Science Foundation of China (grant nos. 81503127
and 81472729).
References
|
1
|
Zhang QQ, Wu XJ, Tang T, Zhu SW, Yao Q,
Gao BZ and Yuan XC: Quantitative analysis of rectal cancer by
spectral domain optical coherence tomography. Phys Med Biol.
57:5235–5244. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ades S: Adjuvant chemotherapy for colon
cancer in the elderly: Moving from evidence to practice. Oncology
(Williston Park). 23:162–167. 2009.PubMed/NCBI
|
|
3
|
Jensen NF, Stenvang J, Beck MK, Hanáková
B, Belling KC, Do KN, Viuff B, Nygård SB, Gupta R, Rasmussen MH, et
al: Establishment and characterization of models of chemotherapy
resistance in colorectal cancer: Towards a predictive signature of
chemoresistance. Mol Oncol. 9:1169–1185. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
McGuire WP, Hoskins WJ, Brady MF, Kucera
PR, Partridge EE, Look KY, Clarke-Pearson DL and Davidson M:
Cyclophosphamide and cisplatin compared with paclitaxel and
cisplatin in patients with Stage III and Stage IV Ovarian Cancer. N
Engl J Med. 334:1–6. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Holmes FA, Walters RS, Theriault RL,
Forman AD, Newton LK, Raber MN, Buzdar AU, Frye DK and Hortobagyi
GN: Phase II Trial of taxol, an active drug in the treatment of
metastatic breast cancer. J Natl Cancer Inst. 83:1797–1805. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Murphy WK, Fossella FV, Winn RJ, Shin DM,
Hynes HE, Gross HM, Davilla E, Leimert J, Dhingra H, Raber MN, et
al: Phase II study of taxol in patients with untreated advanced
non-small-cell lung cancer. J Natl Cancer Inst. 85:384–388. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rowinsky EK and Donehower RC: Paclitaxel
(taxol). N Engl J Med. 332:1004–1014. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Einzig AI, Neuberg D, Wiernik PH, Grochow
LB, Ramirez G, O'Dwyer PJ and Petrelli NJ: Phase II trial of
paclitaxel in patients with advanced colon cancer previously
untreated with cytotoxic chemotherapy: An eastern cooperative
oncology group trial (PA286). Am J Ther. 3:750–754. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Orr GA, Verdier-Pinard P, Mcdaid H and
Horwitz SB: Mechanisms of taxol resistance related to microtubules.
Oncogene. 22:7280–7295. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tsai HC, Huang CY, Su HL and Tang CH: CTGF
increases drug resistance to paclitaxel by upregulating survivin
expression in human osteosarcoma cells. Biochim Biophys Acta.
1843:846–854. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu G, Qin XQ, Guo JJ, Li TY and Chen JH:
AKT/ERK activation is associated with gastric cancer cell
resistance to paclitaxel. Int J Clin Exp Pathol. 7:1449–1458.
2014.PubMed/NCBI
|
|
12
|
Du G, Yang Y, Zhang Y, Sun T, Liu W, Wang
Y, Li J and Zhang H: Thrombocytosis and immunohistochemical
expression of connexin 43 at diagnosis predict survival in advanced
non-small-cell lung cancer treated with cisplatin-based
chemotherapy. Cancer Chemother Pharmacol. 71:893–904. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yu BB, Dong SY, Yu ML, Jiang GJ, Ji J and
Tong XH: Total flavonoids of litsea coreana enhance the
cytotoxicity of oxaliplatin by increasing gap junction
intercellular communication. Biol Pharm Bull. 37:1315–1322. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
King TJ and Bertram JS: Connexins as
targets for cancer chemoprevention and chemotherapy. Biochim
Biophys Acta. 1719:146–160. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yamasaki H and Naus CC: Role of connexin
genes in growth control. Carcinogenesis. 17:1199–1213. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Park JM, Munoz JL, Wona BW, Bliss SA,
Greco SJ, Patel SA, Kandouz M and Rameshwar P: Exogenous CXCL12
activates protein kinase C to phosphorylate connexin 43 for gap
junctional intercellular communication among confluent breast
cancer cells. Cancer Lett. 331:84–91. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sirnes S, Bruun J, Kolberg M, Kjenseth A,
Lind GE, Svindland A, Brech A, Nesbakken A, Lothe RA, Leithe E and
Rivedal E: Connexin43 acts as a colorectal cancer tumor suppressor
and predicts disease outcome. Int J Cancer. 131:570–581. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang Y, Zhang S, Zhang C, Zhao Z, Zheng X,
Xue L, Liu J and Yuan XC: Investigation of an SPR biosensor for
determining the influence of connexin 43 expression on the
cytotoxicity of cisplatin. Analyst. 141:3411–3420. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shimomura M, Yaoi T, Itoh K, Kato D,
Terauchi K, Shimada J and Fushiki S: Drug resistance to paclitaxel
is not only associated with ABCB1 mRNA expression but also with
drug accumulation in intracellular compartments in human lung
cancer cell lines. Int J Oncol. 40:995–1004. 2012.PubMed/NCBI
|
|
20
|
Hong X, Wang Q, Yang Y, Zheng S, Tong X,
Zhang S, Tao L and Harris AL: Gap junctions propagate opposite
effects in normal and tumor testicular cells in response to
cisplatin. Cancer Lett. 317:165–171. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Porter AG and Jänicke RU: Emerging roles
of caspase-3 in apoptosis. Cell Death Differ. 6:99–104. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jordan MA and Kamath K: How do
microtubule-targeted drugs work? An overview. Curr Cancer Drug
Targets. 7:730–742. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wolf F, Wandke C, Isenberg N and Geley S:
Dose-dependent effects of stable cyclin B1 on progression through
mitosis in human cells. EMBO J. 25:2802–2813. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ito M: Factors controlling cyclin B
expression. Plant Mol Biol. 43:677–690. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li F and Altieri DC: The cancer
antiapoptosis mouse survivin gene: Characterization of locus and
transcriptional requirements of basal and cell cycle-dependent
expression. Cancer Res. 59:3143–3151. 1999.PubMed/NCBI
|
|
26
|
Mesnil M, Piccoli C, Tiraby G, Willecke K
and Yamasaki H: Bystander killing of cancer cells by herpes simplex
virus thymidine kinase gene is mediated by connexins. Proc Natl
Acad Sci USA. 93:pp. 1831–1835. 1996; View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Munoz JL, Rodriguez-Cruz V, Greco SJ,
Ramkissoon SH, Ligon KL and Rameshwar P: Temozolomide resistance in
glioblastoma cells occurs partly through epidermal growth factor
receptor-mediated induction of connexin 43. Cell Death Dis.
5:e11452014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tang N, Wang Q, Wu D, Zhang S, Zhang Y and
Tao L: Differential effects of paclitaxel and docetaxel on gap
junctions affects their cytotoxicities in transfected HeLa cells.
Mol Med Rep. 8:638–644. 2013.PubMed/NCBI
|
|
29
|
Sato H, Iwata H, Takano Y, Yamada R,
Okuzawa H, Nagashima Y, Yamaura K, Ueno K and Yano T: Enhanced
effect of connexin 43 on cisplatin-induced cytotoxicity in
mesothelioma cells. J Pharmacol Sci. 110:466–475. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hong R and Lim SC: Pathological
significance of connexin 26 expression in colorectal
adenocarcinoma. Oncol Rep. 19:913–919. 2008.PubMed/NCBI
|
|
31
|
Kanczuga-Koda L, Koda M, Sulkowski S,
Wincewicz A, Zalewski B and Sulkowska M: Gradual loss of functional
gap junction within progression of colorectal cancer-a shift from
membranous CX32 and CX43 expression to cytoplasmic pattern during
colorectal carcinogenesis. In Vivo. 24:101–107. 2010.PubMed/NCBI
|
|
32
|
Han Y, Zhang PJ, Chen T, Yum SW, Pasha T
and Furth EE: Connexin43 expression increases in the epithelium and
stroma along the colonic neoplastic progression pathway:
Implications for its oncogenic role. Gastroenterol Res Pract.
2011:5617192011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ezumi K, Yamamoto H, Murata K, Higashiyama
M, Damdinsuren B, Nakamura Y, Kyo N, Okami J, Ngan CY and Takemasa
I: Aberrant expression of connexin 26 is associated with lung
metastasis of colorectal cancer. Clin Cancer Res. 14:677–684. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Giessmann D, Theiss C, Breipohl W and
Meller K: Decreased gap junctional communication in neurobiotin
microinjected lens epithelial cells after taxol treatment. Anat
Embryol (Berl). 209:391–400. 2005. View Article : Google Scholar : PubMed/NCBI
|