Introduction
Fungal keratitis (FK) was first described by Leber
(1) in 1879 as a suppurative,
ulcerative and sight-threatening infection of the cornea caused by
fungi. Significant damage to the eye, such as blindness, may occur
if FK is not diagnosed early or left untreated for long periods of
time. Compared with bacterial keratitis, FK has a poor prognosis,
and the condition accounts for almost 50% of all cases of
infectious keratitis in developing countries (2,3).
Currently available topical antifungal drugs have limitations, such
as limited spectra of activity and surface toxicity (4–6). The
clinical efficacy of antifungal drugs depends on the concentration
achieved in ocular tissue, which, in turn, depends on the molecular
mass, route of administration, duration of contact, and ability of
the compound to penetrate the eye (7). Some antifungal agents have a high
molecular mass exceeding 500 Da (such as amphotericin B, natamycin
and ketoconazole), leading to their poor penetration, even if they
are lipophilic in nature (6). FK
responds poorly to antifungal agents, and thus surgical
intervention in the form of therapeutic keratoplasty is required
more frequently in cases of FK compared with bacterial keratitis
(3–6,8).
However, the shortage of corneal donors for keratoplasty in
countries such as China has made conjunctival flap (CF) surgery a
promising alternative for the treatment of refractory FK. This
method is an alternative to the Gunderson's flaps technique that
involves covering the whole cornea (9), which has the disadvantage of making it
difficult to observe the anterior chamber or monitor disease
progression.
In the present study, the efficacy of a
tongue-shaped partial flap was evaluated in study subjects.
Specifically, the study assessed the use of selective, partial,
pedunculated (tongue-shaped) CF for the treatment of refractory FK
with or without perforation, and investigated the effectiveness of
this method in managing FK.
Materials and methods
Ethical approval
The present study was approved by the Ethics
Committee of the First Hospital of Jilin University (Changchun,
China), and all study patients provided written informed consent
prior to their participation in the study.
Study design and patients
The present study was a non-comparative
retrospective study. Study subjects were recruited from the
Department of Ophthalmology at the First Hospital of Jilin
University. A total of 31 patients who had undergone CF surgery for
treatment of corneal diseases between April 2014 and October 2015
at the hospital were assessed. Of these, 16 patients who were
diagnosed with FK were selected for further investigation,
according to the criteria below. Study participants were divided
into four age groups: <40, 40–60, 61–80, and >80 years old.
Patient clinical characteristics are listed in Table I.
 | Table I.Patient clinical characteristics and
outcomes. |
Table I.
Patient clinical characteristics and
outcomes.
| Patient number | Age (years) | Sex | Diagnosis | Surgical duration
(min) | Pre-operative VA | Post-operative
VA | Further surgery | Post-operative
hospitalization (days) | Occupation | Complications |
|---|
| 1 | 81 | M | FK | 30 | 0.4 | 0.4 | CAD | 3 | Farmer | N |
| 2 | 68 | F | FK | 30 | CF/30 cm | HM | CAD | 3 | Farmer | Ya |
| 3 | 86 | F | FK | 60 | NPL | NPL | CAD+ACL | 3 | Other | N |
| 4 | 65 | M | FK+ P | 30 | LP | LP | CAD | 6 | Farmer | N |
| 5 | 77 | M | FK + P | 40 | HM | HM | CAD | 5 | Farmer | N |
| 6 | 78 | F | FK | 60 | LP | LP | CAD+ACL+ER | 18 | Farmer | Yb |
| 7 | 58 | M | FK | 60 | 0.1 | 0.1 | CAD | 7 | Farmer | Yb |
| 8 | 62 | M | FK | 60 | 0.12 | 0.12 | CAD | 9 | Farmer | N |
| 9 | 47 | M | FK | 85 | 0.01 | CF/20 cm | CAD | 4 | Farmer | N |
| 10 | 52 | M | FK | 60 | CF/20 cm | CF/20 cm | CAD | 17 | Other | N |
| 11 | 63 | M | FK | 30 | HM/50 cm | HM/50 cm | CAD | 7 | Farmer | N |
| 12 | 60 | M | FK + P | 40 | HM/30 cm | HM/30 cm | CAD | 3 | Farmer | N |
| 13 | 39 | M | FK | 30 | CF/30 cm | HM/20 cm | CAD | 4 | Farmer | N |
| 14 | 74 | M | FK | 30 | HM/30 cm | HM | CAD | 9 | Farmer | N |
| 15 | 70 | F | FK | 80 | 0.3 | 0.3 | CAD | 3 | Farmer | N |
| 16 | 58 | F | FK + P | 30 | HM/10 cm | LP | CAD | 4 | Farmer | N |
Inclusion and exclusion criteria of
the patients
The inclusion criteria were as follows: i) Patients
from the Department of Ophthalmology; ii) Patients of all ages;
iii) admitted patients; and iv) patients with FK. Participants were
excluded based on the following criteria: i) Patients from
ophthalmologic hospitals; ii) outpatients; and iii) patients with
other types of keratitis.
Diagnosis and surgery type
The diagnosis of FK was confirmed based on in
vivo confocal microscopy findings. In all study patients,
surgery was performed using a selective, partial, pedunculated
(tongue-shaped) flap to cover only the ulcerated part of the
cornea, as opposed to covering the whole cornea.
Surgical procedure
Surgery was performed in a sterile surgical room
with the patient lying in supine position under an operating
microscope. Retrobulbar anesthesia was administered with 3 ml 2%
lidocaine (Shanghai Fuxing Chaohui Pharmaceutical Co., Ltd.,
Shanghai, China) to the diseased eye and 5% povidone iodine (Jilin
Ytai Mingxing Medicine Co., Ltd.) was applied with a cotton ball to
sterilize the skin around it. The diseased eye was draped and an
eye spectrum was inserted. The surgeon used surgical blades to
remove the corneal epithelium and any necrotic tissue from the
ulcerated cornea or within 0.5–1 mm of the ulcer margin. The
surgeon selected a conjunctival segment close to the ulcer that
exhibited the best blood supply to the corneal ulcer. A 1 ml
subconjunctival injection of balanced 2% lidocaine (Shanghai Fuxing
Chaohui Pharmaceutical Co., Ltd.) with 1:100,000 epinephrine
(Suicheng Pharmaceutical Co., Ltd., Xinzheng, China) was
administered to help separate the conjunctiva from the underlying
Tenon's capsule. The injected solution was spread over the inflated
conjunctiva using a cotton-tipped applicator to stop the
conjunctiva from stretching. Blunt-tipped scissors and blunt
forceps were used to hold the conjunctiva while the surgical blade
was used to make a tongue-shaped incision in the quadrant of the
conjunctiva near the ulcerated region. Only a partial segment of
the conjunctiva was mobilized on the ulcerated part of the cornea
After setting the conjunctival segment in place, a 10-0
monofilament nylon suture was used to secure the flap in the cornea
using interrupted sutures. Finally, one drop of 0.5% Tropicamide
Phenylephrine Eye Drops (Santen Pharmaceutical Co., Ltd., Osaka,
Japan) and ~0.3 g of antibiotic Ofloxacin eye ointment (3.5 g:10.5
mg; Santen Pharmaceutical Co., Ltd.) were introduced into the eye,
and the eye was dressed. The dressing was changed every 24 h and,
depending on the condition of the patient, sutures were removed
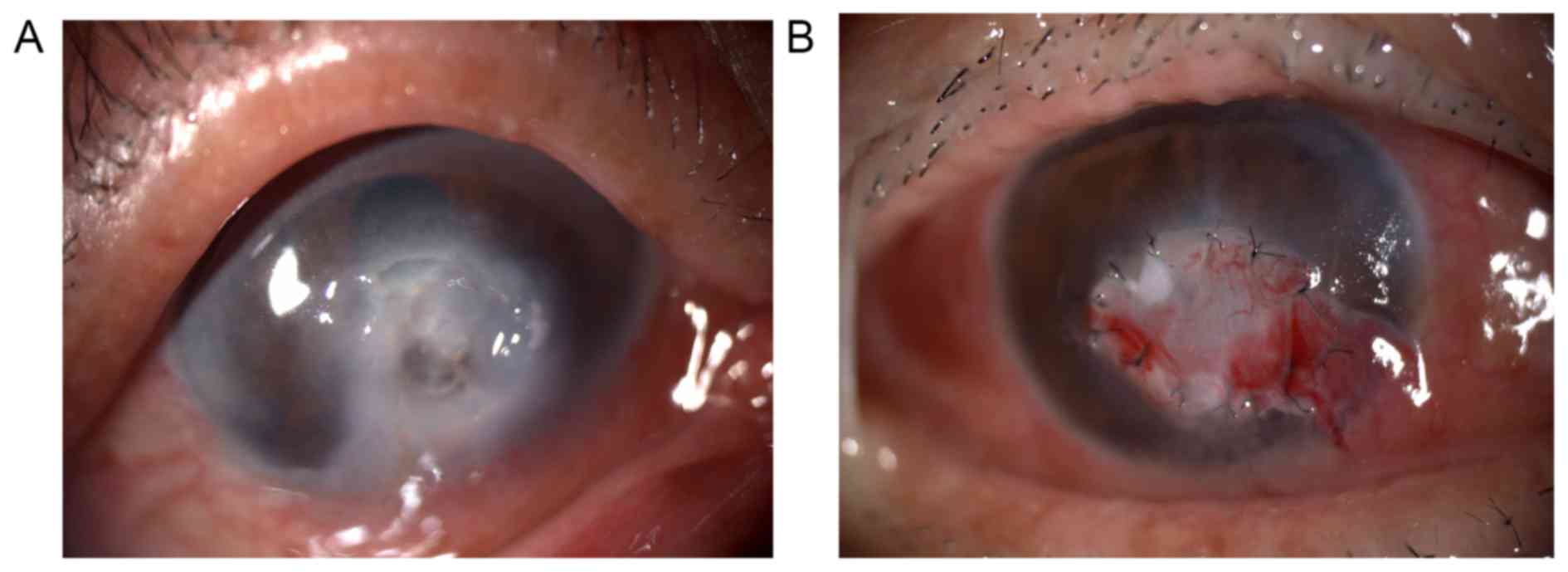
from 2 weeks after surgery. Fig. 1
depicts an ulcerated cornea in one patient before and after CF
surgery.
Statistical analysis
Both descriptive and inferential statistical
analyses were performed. For categorical variables, the descriptive
analyses included both numbers and percentages. χ2 and
Mann-Whitney tests were used to investigate differences in the
distribution of study patients based on age and sex. Using surgical
complications as dependent variables and age, sex, combined surgery
and surgical duration as independent variables, simple and multiple
logistic regression analyses (inferential statistics) were used to
investigate factors associated with the occurrence of complications
after CF surgery. SPSS 18.0 software (SPSS, Inc., Chicago, IL, USA)
was used for all statistical analyses, and P<0.05 was considered
to indicate a statistically significant difference.
Results
Patient characteristics
A total of 16 patients were diagnosed with FK and
underwent CF surgery. Among these 16 patients, 11 (68.8%) were male
and 5 (31.2%) were female; however, there was no statistical
difference in the gender ratio of patients (Table I). Male farmers comprised the
majority of the patient cohort (n=11, 68.8%), and plant trauma was
the primary cause of disease. The <40, 40–60, 61–80 and >80
years age groups had 1, 5, 8 and 2 cases, respectively. The 61–80
years old group had the largest number of patients (50.0%). The
results of the present study demonstrated that the sex, age group
and age-sex distributions of study patients did not differ
significantly (Table II).
 | Table II.Sex, age, and age-sex distributions
of patients. |
Table II.
Sex, age, and age-sex distributions
of patients.
| Variable | Value |
t-test/χ2-value | P-value |
|---|
| Mean age |
| 14.50 | 0.141 |
| Male
(n=11) | 61.64 |
|
|
| Female
(n=5) | 72.00 |
|
|
| Sex |
| 2.25 | 0.134 |
|
Male | 11 |
|
|
|
Female | 5 |
|
|
| Age groups
(years) |
|
7.50e | 0.058 |
|
<40 | 1 |
|
|
|
40–60 | 5 |
|
|
|
61–80 | 8 |
|
|
|
>80 | 2 |
|
|
Patient outcomes
Among the study patients, 4 presented with
perforation associated with FK prior to surgery. Corneal scraping
was performed on all patients prior to CF surgery. Among the 16
patients enrolled, 14 patients underwent CF combined with corneal
ulcer debridement (without anterior chamber lavage), while 2
patients underwent anterior chamber lavage in addition to CF
surgery and corneal ulcer debridement. A total of 3 patients
experienced post-operative complications; 1 patient exhibited
corneal perforation, 1 patient ultimately had his eyeball
surgically removed 10 days after CF due to the uncontrolled
spreading of purulent exudates (hypopion) beyond the anterior
chamber; and another patient with hypopion in the anterior chamber
underwent an anterior chamber lavage plus further CF surgery and
healed well. The remaining 13 patients recovered well.
Postoperative visual acuity (VA) was decreased in 4 cases (25%) and
remained unchanged in 12 cases (75%). The post-surgical outcome was
good for all patients that underwent surgeries with controlled eye
infections and preserved eyeballs. Simple and multiple logistic
regression analyses indicated that age, sex, surgery duration, and
combined surgeries were not significantly associated with the
development of complications (Table
III).
 | Table III.Logistic regression analyses of
factors influencing conjunctival flap post-surgery
complications. |
Table III.
Logistic regression analyses of
factors influencing conjunctival flap post-surgery
complications.
| Variable | B | OR (95% CI) | P-value |
|---|
| Simple logistic
regression |
|
Age | −0.03 | 0.97
(0.88–1.08) | 0.63 |
|
Sex | −1.90 | 0.15
(0.01–2.29) | 0.17 |
|
Surgical duration | −0.01 | 0.99
(0.93–1.06) | 0.77 |
|
Combined surgery | −1.81 | 0.16
(0.01–2.55) | 0.20 |
| Multiple logistic
regression |
|
Age | 0.24 | 1.27
(0.85–1.91) | 0.24 |
|
Sex | −3.54 | 0.03
(0.00–9.23) | 0.23 |
|
Surgical duration | 0.07 | 1.07
(0.93–1.23) | 0.33 |
|
Combined surgery | −5.54 | 0.00
(0.00–17.68) | 0.20 |
Discussion
Due to different fungal pathogens, complex clinical
manifestations and limited antifungal medications, FK is typically
difficult to treat, which leads to worsening of the condition and
the need for surgical treatment (10). This has resulted in higher rates of
flap surgeries as a non-pharmacological treatment for FK (11). Surgical intervention for patients
with refractory FK is effective, and CF surgery is a simple and
economical option that typically preserves the eye and vision.
The present study included more males (68.8%) than
females (31.2%), though this difference was not statistically
significant. Khater et al (12) performed an epidemiological study of
66,303 patients (264 cases of mycotic keratitis), and in comparing
mycotic keratitis with nonmycotic keratitis, it was demonstrated
that both mycotic and nonmycotic keratitis were markedly more
prevalent in males compared with females. Contrary to results of
the present study, a number of studies have reported a significant
correlation between sex and the distribution of FK patients,
whereby males were more affected by FK than females (13–16).
These studies, including that by Khater et al (12), reported a higher prevalence of FK
among male farmers compared with female farmers, and that plant
trauma was the primary cause of the disease. The results of the
present study were in accordance with this, with FK being most
prevalent in farmers.
Contrary to our results, which suggested that FK was
more prevalent in the 61–80 years age group, previous studies have
reported that FK was more prevalent in young adults (8,15).
However, some studies (15,17) demonstrated a prevalence in males
between 50–60 years of age. Khater et al (12) also observed that mycotic keratitis
was most prevalent in the 40–60 years age group (52.4% of cases)
(12). The results of the present
study differ from those of most of other authors, possibly due to
the relatively small sample used in the present study.
In the majority of patients enrolled in the present
study, the aim of CF surgery was to prevent or stop corneal
perforation and/or inflammation and to preserve the eyeball, rather
than to improve the patient's vision. As such, the decreased or
unchanged post-operative VA observed in the present study does not
indicate that CF surgery was unsuccessful. In a previous study
investigating the different outcomes of Gundersen flap in which
sutures were administered in one group and glue in another, Chung
and Mehta (18) reported unchanged
post operative VA in 5/7 patients, and increased VA in 2/7
patients, with all 7 patients diagnosed with different types of
corneal disorders (18). In the
present study, the tongue-shaped flap was mobilized only on the
ulcerated cornea, as opposed to covering the whole cornea. This
method provides an alternative to Gunderson's flaps, and avoids the
complications associated with the Gunderson's flaps technique
(9). If the conjunctiva covers the
entire cornea, it obstructs any view of the anterior chamber
(19,20), which increases the difficulty of
monitoring disease progression and checking intraocular pressure to
avoid glaucoma development. Furthermore, patients with short
fornices have been subjected to the Gunderson's flaps technique,
where it was observed that the technique may lead to the
development of ptosis (19). These
limitations favored alternative approaches to treatment (21–26).
The majority of patients in the present study
underwent CF surgery combined with corneal ulcer debridement (CF +
CAD); however, 2 patients underwent CF surgery with corneal ulcer
debridement and anterior chamber lavage (CF + CAD + ACL). Zeng
et al (27) investigated the
effectiveness of an amniotic membrane covering on the ulcerated
cornea following debridement in a patient with FK, and concluded
that corneal scraping prior to surgical therapy (in this case
amniotic membrane) promotes healing of the cornea. McGrath and Lee
demonstrated in 2015 (28) that
corneal epithelial debridement may be used as an effective therapy
for ocular surface diseases as well as diagnosis. Among 62 eyes
that received corneal epithelial debridement for diagnostic
purposes, 48 were positive for infective keratitis, among which 5
eyes (20.8%) were diagnosed with FK. Corneal scraping is an
effective treatment for pathologies of the corneal surface
(29,30).
In the present study, 3 patients experienced
post-surgical complications; 1 patient exhibited corneal
perforation, another exhibited uncontrolled spreading of purulent
exudates (hypopion) beyond the anterior chamber, and 1 patient
exhibited hypopion in the anterior chamber. The patient with cornea
perforation received a cornea transplant shortly after CF surgery.
The patient with uncontrolled hypopion spreading beyond the
anterior chamber underwent an anterior chamber lavage, though
ultimately had their eyeball surgically removed 10 days after CF.
The patient with hypopion in the anterior chamber underwent an
anterior chamber lavage plus further CF surgery, which ultimately
succeeded in controlling the infection. Based on Table III, age, sex, surgery duration and
combined surgeries were not statistically associated with the
probability of developing post-surgical complications. However, it
was noted that the majority of complications were associated with
higher disease severity, due to its propensity to spread and/or
failure to heal after surgery. Many patients seek medical care at
an advanced stage of the disease when treatment at local clinics
has failed. In the present study, no patients developed any of the
most common post-surgical complications associated with CF surgery,
such as conjunctival buttonholes and flap retractions. This
suggests that subsequent complications did not result from a
failure in the CF surgery itself, but may be associated with the
severity of the disease. However, the relatively small sample used
in the present study may have skewed data; therefore, future
studies with larger sample sizes are now required to verify the
current results.
Although keratoplasty is among the best treatment
strategies for refractory FK with or without perforation, CF
surgery may be a useful alternative treatment in cases where
immediate corneal transplant is not feasible. In the present study,
the outcome was good in all the patients with the exception of 1
patient, who ultimately required surgical removal of the eyeball.
The results of the present study suggest that CF is an effective
treatment for refractory FK when corneal transplantation is not a
possibility.
Acknowledgements
The present study was supported by the Development
and Reform Commission of Jilin Province (grant no. 2015Y031-1) and
the First Hospital of Jilin University (grant no.
JDYY72016055).
References
|
1
|
Leber TH: Keratomycosis spergillina als
ursache von hypopyonkeratites. Graefes Ach Clin Exp Ophthalmol.
25:285–301. 1879. View Article : Google Scholar
|
|
2
|
Ou JI and Acharya NR: Epidemiology and
treatment of fungal corneal ulcers. Int Ophthalmol Clin. 47:7–16.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gopinathan U, Sharma S, Garg P and Rao GN:
Review of epidemiological features, microbiological diagnosis and
treatment outcome of microbial keratitis: Experience of over a
decade. Indian J Ophthalmol. 57:273–279. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Johns KJ and O'Day DM: Pharmacologic
management of keratomycoses. Surv Ophthalmol. 33:178–188. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
O'Day DM, Head WS, Robinson RD and Clanton
JA: Corneal penetration of topical amphotericin B and natamycin.
Curr Eye Res. 5:877–882. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kaur IP, Rana C and Singh H: Development
of effective ocular preparations of antifungal agents. J Ocul
Pharmacol Ther. 24:481–493. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kaur IP and Kakkar S: Topical delivery of
antifungal agents. Expert Opin Drug Deliv. 7:1303–1327. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sony P, Sharma N, Vajpayee RB and Ray M:
Therapeutic keratoplasty for infectious keratitis: A review of the
literature. CLAO J. 28:111–118. 2002.PubMed/NCBI
|
|
9
|
Sandinha T, Zaher SS, Roberts F, Devlin
HC, Dhillon B and Ramaesh K: Superior forniceal conjunctival
advancement pedicles (SFCAP) in the management of acute and
impending corneal perforations. Eye (Lond). 20:84–89. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dursun D, Fernandez V, Miller D and
Alfonso EC: Advanced fusarium keratitis progressing to
endophthalmitis. Cornea. 22:300–303. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sanitato JJ, Kelley CG and Kaufman HE:
Surgical management of peripheral fungal keratitis (keratomycosis).
Arch Ophthalmol. 102:1506–1509. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Khater MM, Shehab NS and El-Badry AS:
Comparison of mycotic keratitis with nonmycotic keratitis: An
epidemiological study. J Ophthalmol. 2014:2543022014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rautaraya B, Sharma S, Kar S, Das S and
Sahu SK: Diagnosis and treatment outcome of mycotic keratitis at a
tertiary eye care center in eastern India. BMC Ophthalmol.
11:392011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bharathi MJ, Ramakrishnan R, Vasu S,
Meenakshi R and Palaniappan R: Epidemiological characteristics and
laboratory diagnosis of fungal keratitis. A three-year study.
Indian J Ophthalmol. 51:315–321. 2003.PubMed/NCBI
|
|
15
|
Chander J and Sharma A: Prevalence of
fungal corneal ulcers in northern India. Infection. 22:207–209.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Deshpande SD and Koppikar GV: A study of
mycotic keratitis in Mumbai. Indian J Pathol Microbiol. 42:81–87.
1999.PubMed/NCBI
|
|
17
|
Saha S, Banerjee D, Khetan A and Sengupta
J: Epidemiological profile of fungal keratitis in urban population
of West Bengal India. Oman J Ophthalmol. 2:114–118. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chung HW and Mehta JS: Fibrin glue for
Gundersen flap surgery. Clin Ophthalmol. 7:479–484. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gundersen T: Conjunctival flaps in the
treatment of corneal disease with reference to a new technique of
application. AMA Arch Ophthalmol. 60:880–888. 1958. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lin DT, Webster RG Jr and Abbott RL:
Repair of corneal lacerations and perforations. Int Ophthalmol
Clin. 28:69–75. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saini JS, Sharma A and Grewal SP: Chronic
corneal perforations. Ophthalmic Surg. 23:399–402. 1992.PubMed/NCBI
|
|
22
|
Hirst LW, Smiddy WE and Stark WJ: Corneal
perforations. Changing methods of treatment, 1960–1980.
Ophthalmology. 89:630–635. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Portnoy SL, Insler MS and Kaufman HE:
Surgical management of corneal ulceration and perforation. Surv
Ophthalmol. 34:47–58. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Weiss JL, Williams P, Lindstrom RL and
Doughman DJ: The use of tissue adhesive in corneal perforations.
Ophthalmology. 90:610–615. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hirst LW and De Juan E Jr: Sodium
hyaluronate and tissue adhesive in treating corneal perforations.
Ophthalmology. 89:1250–1253. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sharma A, Kaur R, Kumar S, Gupta P, Pandav
S, Patnaik B and Gupta A: Fibrin glue versus
N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology.
110:291–298. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zeng B, Wang P, Xu LJ, Li XY, Zhang H and
Li GG: Amniotic membrane covering promotes healing of cornea
epithelium and improves visual acuity after debridement for fungal
keratitis. Int J Ophthalmol. 7:785–789. 2014.PubMed/NCBI
|
|
28
|
McGrath LA and Lee GA: Corneal epithelial
debridement for diagnosis and therapy of ocular surface disease.
Clin Exp Optom. 98:155–159. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kenyon KR: Review of surgical strategies
for ocular surface disease. Ocul Surf. 9:164–168. 2011.
|
|
30
|
Jeng BH, Dupps WJ Jr, Meisler DM and
Schoenfield L: Epithelial debridement for the treatment of
epithelial basement membrane abnormalities coincident with
endothelial disorders. Cornea. 27:1207–1211. 2008. View Article : Google Scholar : PubMed/NCBI
|