Introduction
Nasal septum deviation (NSD) involves displacement
of the nasal septum and typically occurs following
otorhinolaryngologic surgery (1).
Severe cases of NSD may be treated with a surgical procedure known
as septoplasty. Based on the biomechanical characteristics of NSD,
a novel surgical procedure termed nasal endoscopic three minus
septoplasty has been developed by Wang et al (2). This modified version of septoplasty has
so far been shown to be safe and effective at treating NSD, however
it lacks the ability to measure preoperative biomechanical
parameters required to evaluate the severity of NSD.
The deformation rate (DR) is defined as a change in
tissue structure induced by an external force (3). During development and growth of the
nasal septum, or in the process of ossification, imbalanced growth
between the nasal bones or between the bones and cartilage may lead
to nasal septum malformation and/or deviation, leading to formation
of an apophysis at the nasal crest and/or junction (4). This process represents the elastic
strain model of NSD. Due to the technical limitations of detection
methods, few previous studies have successfully measured
preoperative biomechanical parameters of NSD (2). However, due to the development of
clinical three dimensional computer tomography (3D-CT)
reconstruction techniques (5), it is
now possible to measure and consult biomechanical parameters prior
to nasal endoscopic septoplasty. DR, which is a key biomechanical
parameter of the elastic strain model (2), may be calculated using 3D-CT
reconstruction techniques. Therefore, using 3D-CT reconstruction
techniques to measure the DR of the nasal septum at maximum
deviation sites, the present study aimed to determine whether DR is
associated with visual analogue scale (VAS) and nasal airway
resistance (NAR) (2,6), and to evaluate the application of DR
measurements in nasal septoplasty endoscopic surgery.
Materials and methods
Clinical materials
The current study was conducted in 30 patients
presenting with symptoms of NSD, who received nasal septoplasty
endoscopic surgery in Longgang ENT Hospital (Shenzhen, China)
between May 2014 and May 2015. The patient cohort included 21 males
and 9 females and mean age was 35.2±12.3 years. Patients exhibited
mild to moderate clinical symptoms of nasal obstruction, including
nasal hemorrhage, headache, nasal discharge, sneezing, snore and
breathing through the mouth. VAS score was recorded by measuring
the degree/strength of the symptoms to provide a measurable
continuum as previously described (2,7). NAR was
measured using an NR6 nasal airway resistance dynamometer (GM
Instruments Ltd., Kilwinning, UK) according to the manufacturer
instructions. The mean VAS and NAR scores were 6.97±1.69 and
1.36±0.30 kPa.s.L−1, respectively. Patients suffering
from nasal sinusitis or nasal polyp, granulomatous diseases of the
nose or nasal masses, or with a past history of nasal surgery were
excluded from the current study. The current study was approved by
Ethics Committee of Longgang ENT Hospital and all patients provided
written informed consent prior to participation in the study.
Preoperative 3D-CT reconstruction of
the nasal septum
Preoperative 3D-CT scanning of nasal sinuses was
performed in all patients using a Philips Brilliance 16-slice
spiral CT (Philips Medical Systems B.V, Eindhoven, The
Netherlands), to reconstruct coronal and/or axial nasal septum
structures as original scanning image data. The 3D-CT scan ranged
from the top of the frontal sinus to the bottom of hard palate. The
scanning conditions were as follows: Voltage, 120 kV; current, 0.25
amp slice thickness, 1 mm and layer spacing, −1 mm. The bone window
settings were as follows: Window width, 2000 Hu and window level,
200 Hu. The soft-tissue window settings were as follows: Window
width, 350 Hu; and window level, 40 Hu. Scanning data were
transferred to a Philips Extended Brilliance Workspace 3.5
workstation (Philips Medical Systems B.V.) and processed using a CT
Viewer (Philips Medical Systems B.V.) for multiplanar
reconstruction. Original soft tissue images were used to create 3D
reconstruction models using a Sinus Trachea protocol (provided with
workstation) and following reconstruction tissues adjacent to the
nasal septum on the images were processed to expose the nasal
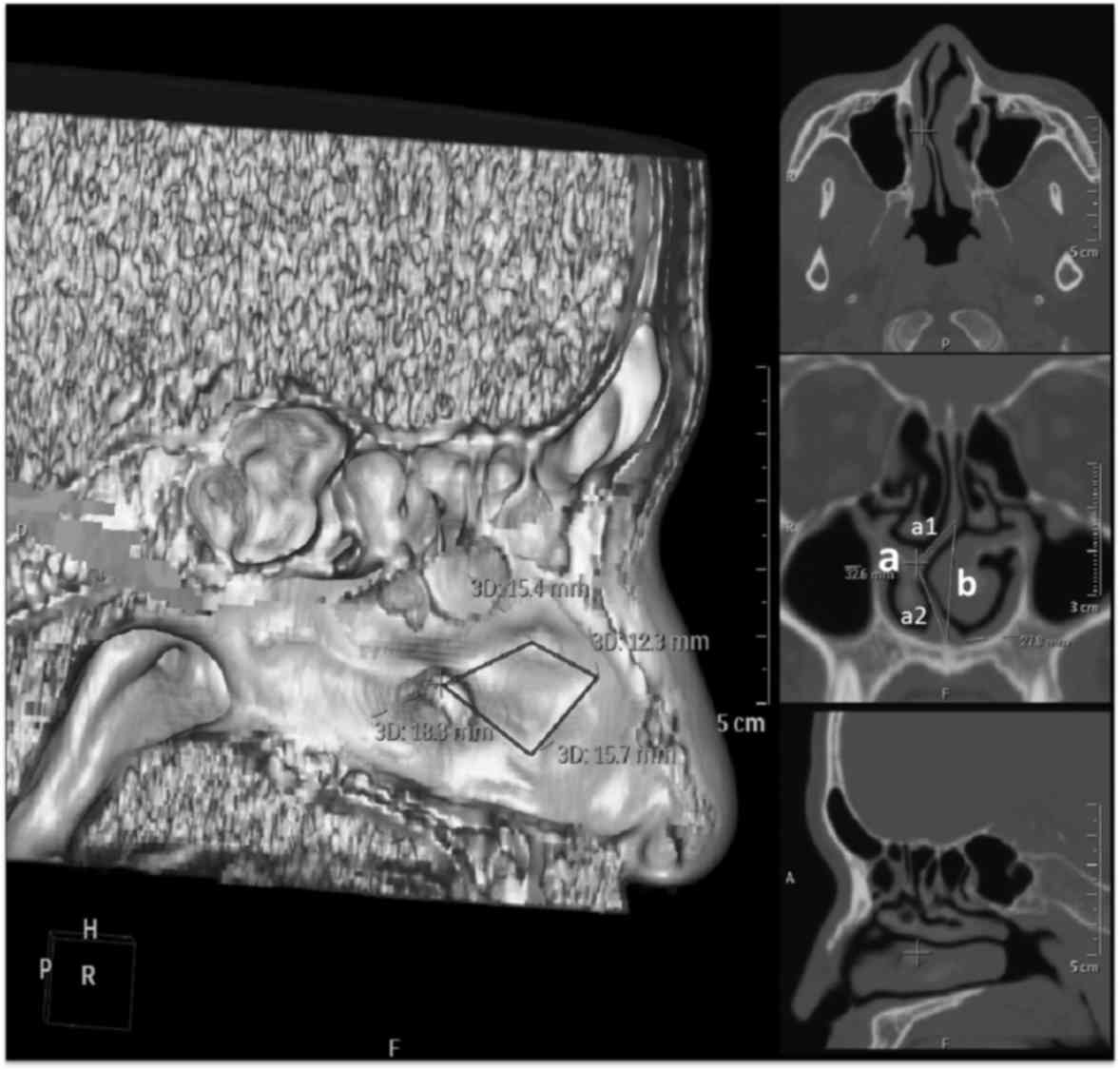
septum. The position and lengths of four stress lines [as described
by Wang et al (2)], the
maximal deformation side of flexure and the original vertical
length of the nasal septum were measured based on 3D and coronal
images. The 3D reconstruction images were marked with the
positioning and lengths of four stress lines: First line, between
the quadrangular cartilage and the medial crus of the greater alar
cartilage; second line, between the cartilage and vomer bone; third
line, between the cartilage and the perpendicular plate of the
ethmoid; fourth line, between the quadrangular cartilage and the
nasal bone (Fig. 1).
Biomechanical analysis of the DR at
the NSD site
The stress within deviated nasal septum bone is
generally formed by flexural deformation. According to mechanical
principles, the extent of stress is in direct proportion with the
distance from the upper and lower boundaries to the central axis,
with increased distance to the central axis resulting in greater
stress (2,8). The value of DR is equal to the maximal
flexural deformation (a) minus the original length (b) divided by
the original length (b), i.e., DR=(a-b)/b. In the current study,
the deformed length of the nasal septum was defined as the maximal
side of flexure (Fig. 1, indicated
by the letter a). The strained side of the deformed septum
cartilage was potentially caused by the nasal bone (upper side,
a1), vomer and nasal crest of maxilla (lower side, a2). The
original length was defined as the original vertical length of the
maximal flexural side (Fig. 1,
indicated by the letter b). The following formula was used to
calculate the DR value: DR=(a-b)/b.
Surgical methods
All surgeries were performed using a Storz nasal
endoscope (KARL STORZ GmbH & Co., KG, Tuttlingen, Germany) and
surgical monitoring system (Medtronic, Minneapolis, MN, USA).
According to assessments of disease severity, general conditions
and psychological status, 30 patients were administered general
anesthesia by an anesthetist according to standard clinical
practices and placed in a supine position. The nasal skin was
incised to expose the perichondrium by Killian incision. Structures
from the superior and posterior side of the lamina mediana and
Vomer to the inferior and posterior structures at the nasal bottom,
including the nasal septum bottom, Vomer and nasal crest of maxilla
were separated. On the posterior side, within 1–2 mm of the first
skin and mucous incision, two incisions with an interval of 2 mm
were made in parallel through the cartilage of the nasal septum.
Cartilage between the two incisions was removed and contralateral
mucous cartilage membrane was separated using a nasal endoscope, in
order to separate the mucous cartilage membrane from the nasal
septum cartilage, as previously described (9). A double heads nasal septum elevator
(Guangzhou in LaCrosse Medical Devices Co., Ltd., Guangzhou, China)
was used to compress the junction between the nasal septum
cartilage and lamina mediana, as the connection between the nasal
septum cartilage, Vomer ridge at the basal base and nasal crest of
maxilla. Pressure was applied to dislocate the nasal septum
cartilage and separate the nasal septum cartilage at the front,
posterior and inferior sides. Based on preoperative 3D
reconstruction data, selective excision was conducted to remove the
core areas of stress and eliminate the stress between the septum
cartilage and sclerostin (2). Images
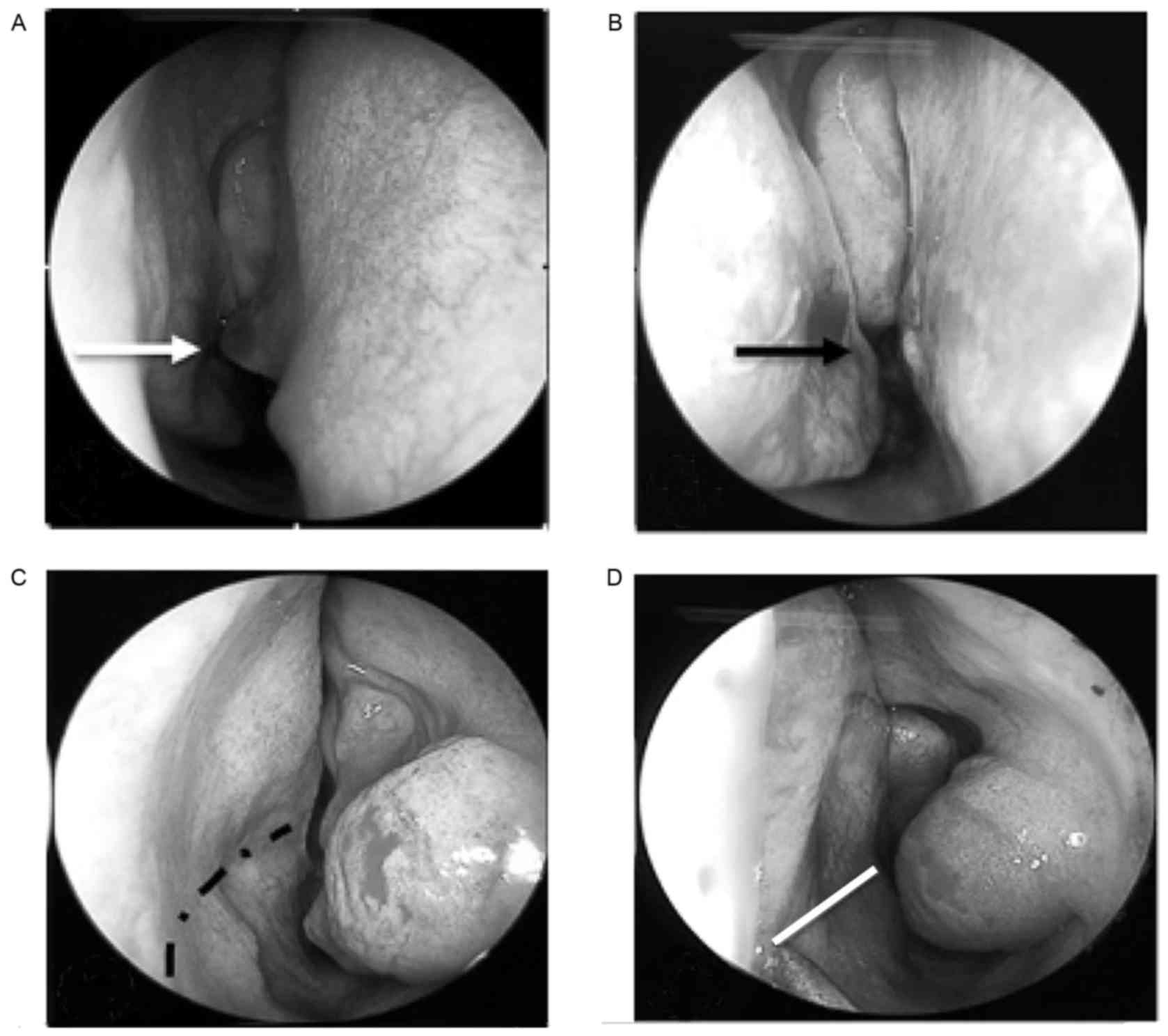
of the bilateral nasal cavities were obtained by endoscopic
examination immediately before and after surgery.
Therapeutic evaluation
Patients were followed up 3 months after surgery to
evaluate NSD-related symptoms (10).
As a subjective evaluation standard, VAS was used to identify the
severity of nasal obstruction caused by lesions of the nasal
cavity. NAR was assessed using an NR6 nasal airway resistance
dynamometer (GM Instruments Ltd.) as an objective evaluation
parameter of nasal ventilation function. Data were collected from
patients before and 3 months after the operation.
Statistical analysis
Data are presented as the mean ± standard deviation.
Data from the preoperative assessment of VAS (VAS1), preoperative
NAR (NAR1), postoperative VAS (VAS2) and postoperative NAR (NAR2)
were analyzed using a paired t test and Pearson correlation
analysis. SPSS 19.0 software (IBM SPSS, Armonk, NY, USA) was used
for statistical analysis and P<0.05 was considered to indicate a
statistically significant difference.
Results
Reconstructed 3D images of the nasal
septum
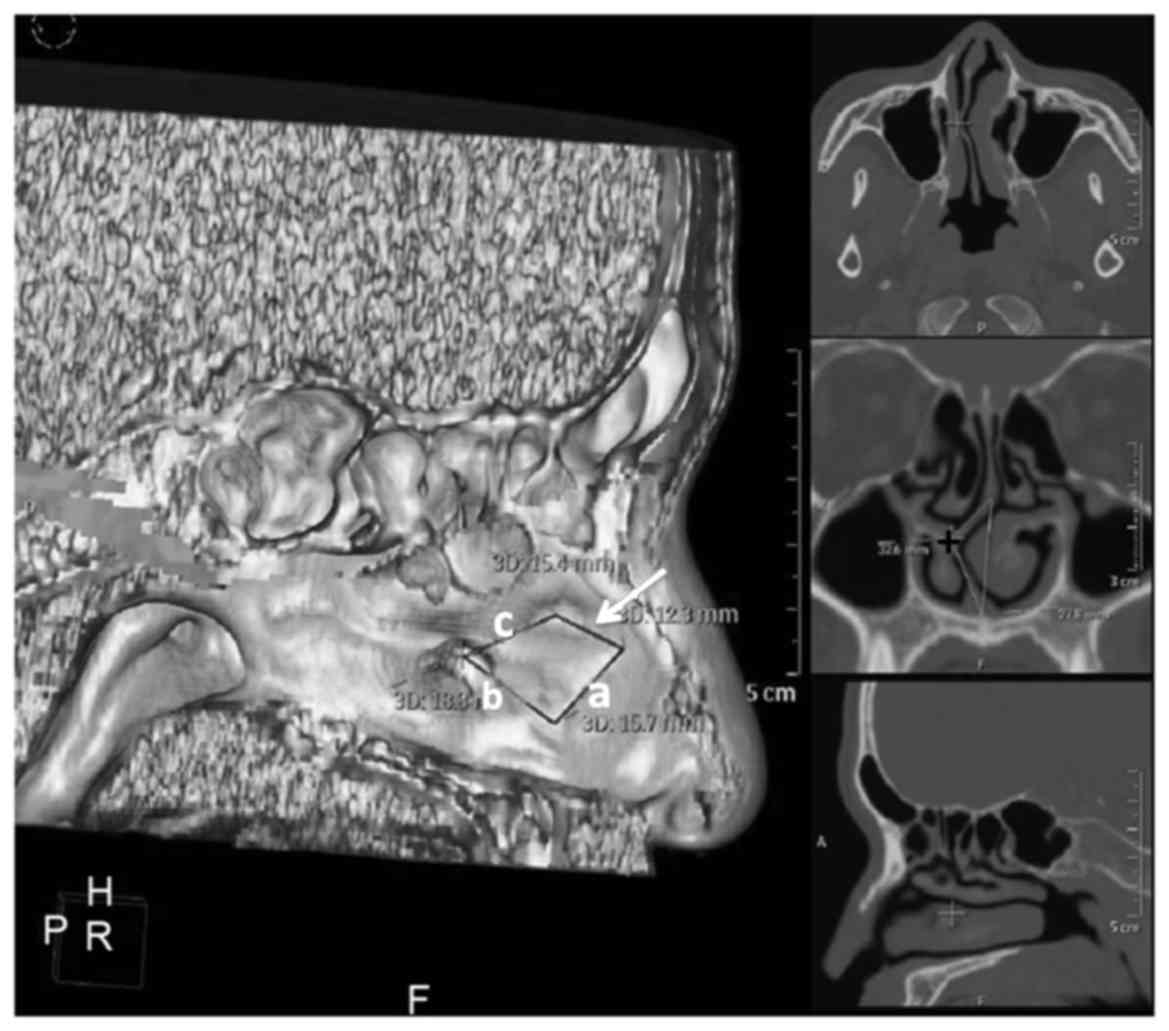
Among the 30 patients of NSD enrolled in the present
study, there were 24 cases of ‘C’ deviation, 6 cases of ‘S’
deviation, 18 cases of crest elevation and 3 cases of nasal process
deviation (7). A total of 19
patients exhibited deviation at the superior position and 7
patients exhibited deviation at the caudal end. Following 3D
reconstruction and excision, distinct 3D images of the nasal septum
indicating the shape and site of deviation were obtained. For
instance, the coronal and sagittal 3D-CT images from one patient
presented with right deviation of the nasal septum, located at the
first [Fig. 2; a], second [Fig. 2; b] and third [Fig. 2; c] stress lines. However, deviation
was not detected at the fourth stress line (Fig. 2; black arrow). The most marked
deviation site was located at the junction between the
quadrilateral cartilage and lamina mediana, at the borderline
between the second and third stress lines (Fig. 2, ‘+’ symbol). Using the coronal plane
of this point, values of deformation and original length were
determined.
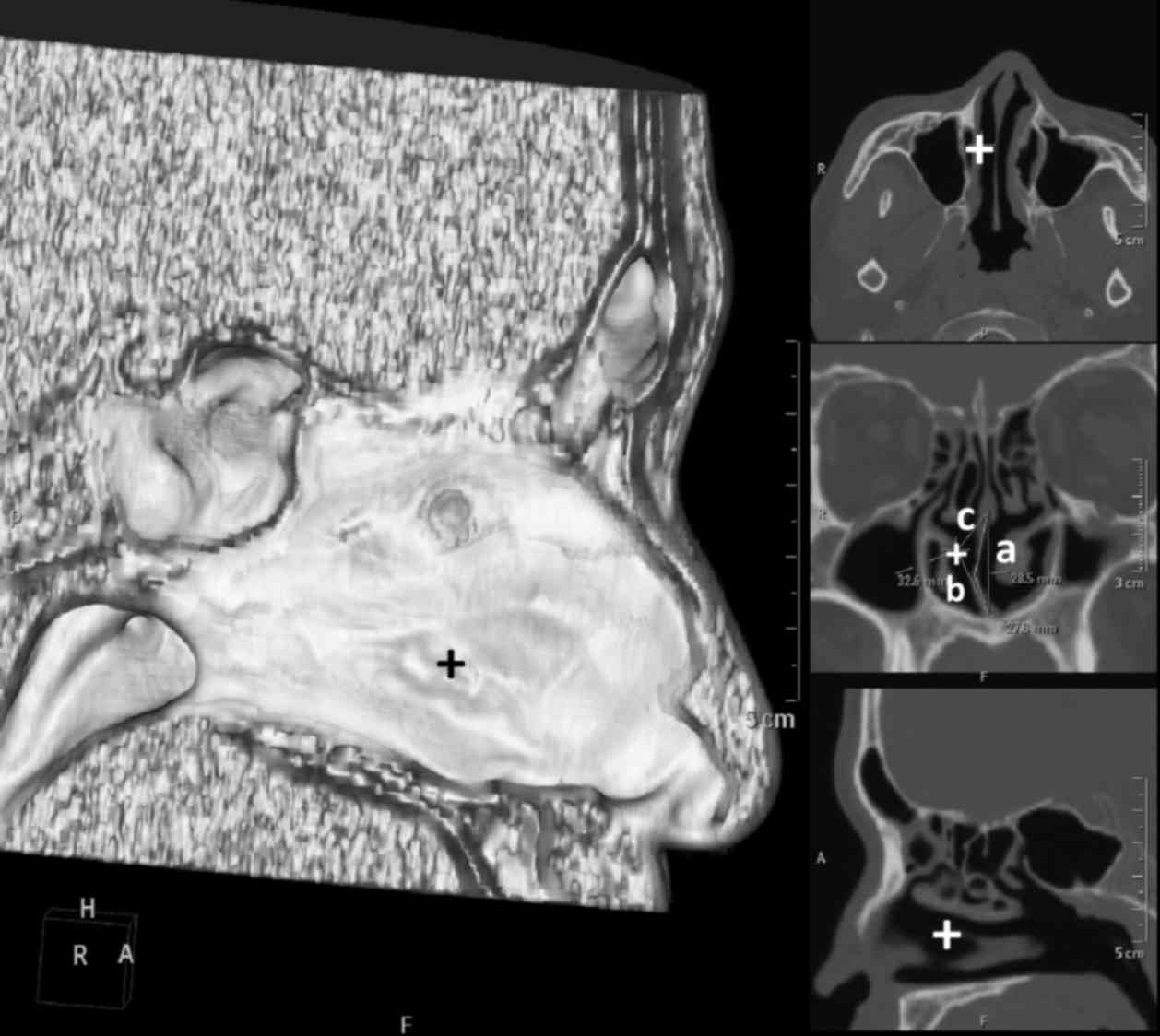
Preoperative 3D reconstruction images successfully
identified the following: The most severe region of the original
deviation (Fig. 3, ‘+’); the
original vertical length (Fig. 3;
a), the primary maximum curved edge of NSD (Fig. 3; b); and the maximum edge of
membranous deviation (Fig. 3; c).
Based on these observations, regions of stress were determined.
According to preoperative 3D reconstruction images and the
calculated DR (0.148±0.105), pointed intraoperative relief of nasal
septum stress was performed. Preoperative 3D-CT reconstruction
images were reviewed 3 months after surgery. Images of the
bilateral nasal cavities obtained by endoscopic examination
immediately before and after surgery (Fig. 4) confirmed that the state of the
nasal septum at the time of operation was consistent with the data
provided by preoperative 3D reconstruction images.
Correlation analysis of preoperative
DR1, NAR1 and VAS1
Potential correlations between DR1, NAR1 and VAS1
were evaluated by Pearson correlation analysis (Table I). DR1 was significantly correlated
with VAS1 (P=0.002) with a Pearson correlation coefficient of
0.534. The Pearson correlation coefficient between DR1 and NAR1 was
0.397, indicating a significant association between DR1 and NAR1
(P=0.03). NAR1 was not significantly correlated with VAS1.
 | Table I.Correlation analysis of DR1, NAR1 and
VAS1. |
Table I.
Correlation analysis of DR1, NAR1 and
VAS1.
| Item | DR1 | NAR1 | VAS1 |
|---|
| DR1 |
| R | 1 | 0.397a | 0.534b |
| P |
| 0.030 | 0.002 |
| NAR1 |
| R |
| 1 | 0.359 |
| P |
|
| 0.051 |
| VAS1 |
| R |
|
| 1 |
| P |
|
|
|
Postoperative follow-up and clinical
efficacy
Based on preoperative 3D reconstruction images and
DR analysis, a general nasal septoplasty endoscopic operation was
performed, whereby relaxing surgery was conducted on the nasal
septum. During a 3 month follow-up period, 23 cases (73.1%) were
cured and 7 cases (23.3.%) had improved. The postoperative DR2,
NAR2 and VAS2 values 3 months after surgery were all significantly
decreased compared with the preoperative DR1, NAR1 and VAS1 values,
respectively (P<0.01; Table II).
During this time, no complications occurred.
 | Table II.Comparison of pre and postoperative
DR, NAR and VAS values. |
Table II.
Comparison of pre and postoperative
DR, NAR and VAS values.
| Item | DR | NAR, kPa.s.L-1 | VAS score |
|---|
| Preoperative |
0.148±0.105a |
1.36±0.30a |
6.97±1.69a |
| 3 months after
surgery | 0.017±0.015 | 0.27±0.14 | 1.37±0.89 |
| t | 6.98 | 21.96 | 16.75 |
| P-values | <0.01 | <0.01 | <0.01 |
Discussion
NSD is a prevalent clinical condition, with severe
cases typically leading to breathing difficulties, nasal
obstruction, nasal hemorrhage and headache. Fischer and Gubisch
(11) documented that NSD was the
primary cause of obstructive disorders of the nasal valve area and
may interfere with the elimination of inflammatory mediators. NSD
correlates with the pathogenesis of allergic rhinitis and is a
major risk factor of obstructive sleep apnea syndrome (12). Severe NSD generally requires the
surgical treatment, usually septoplasty, as it is considered to be
the most effective method of treating NSD (13). The fundamental purpose of septoplasty
is to relieve the clinical symptoms induced by NSD and the surgery
may also be used to treat concurrent disorders such as nasal
sinusitis (14). In nasal septum
reconstruction, the traditional procedure of submucous septectomy
has been developed into the more novel techniques of nasal
submucous septorhinoplasty, used in cases requiring septal
cartilage alteration, and nasal endoscopic three minus
septorhinoplasty (15). These novel
procedures preserve the nasal supporting structures and reduce
complications; however, they are more complicated than the
traditional technique, and require higher operating skills and
sufficient awareness of the deviation site, stress area and
biomechanical parameters to evaluate the levels of NSD prior to
operation. Furthermore, Akoglu et al (16) suggested that any substantial bony and
mucosal enlargements in the anterior and middle segments of the
inferior turbinate should be unaltered, due to their supporting
roles in turbinate reduction during septoplasty. Few studies of
operative techniques have involved the assessment of the NSD
elastic stress area and preoperative biomechanical parameters.
Biomechanical principles are extensively applied in orthopedics and
other fields (17,18). Despite a lack of muscle tissue and
the influence of other mechanical factors, the anatomical structure
of the nasal septum can be generally viewed as an elastic
mechanical model that conforms to biomechanical rules (19). During the embryonic phase of
development, the nasal septum is composed of different cartilages
(20). As development of the skull
occurs prior to maturation of the nasal septum, the upper and
bottom boundaries of nasal septum are fixed, and any imbalanced
growth between the bone and cartilage and/or bone and bone during
development and ossification produces strain and stress variation
(21). This variation is
predominantly concentrated in the junctions between the thin nasal
septum cartilage and peripheral bones, eventually leading to the
development of nasal deformity or deviation and apophysis at the
crest of the nasal septum (22,23). In
biomechanical terms, the strain and stress that occurs in NSD is
consistent with flexural load, and the DR represents the ratio
between the septum deformation and original septum size, reflecting
the magnitude of strain and stress in the nasal septum. Therefore,
analysis of the DR is an important factor to consider for nasal
submucous septorhinoplasty, as the results of the present study
indicated that according to the evaluation of DR, relieving strain
and stress in NSD is key for successful correction of NSD.
In the present study, the general morphology,
deviation site, maximum point of deviation and stress lines of the
nasal septum were accurately identified by 3D-CT reconstruction
images prior to surgery. In addition, assessment of the DR enabled
accurate selection of the correct procedure and the operating site
for stress relief, resulting in successful septorhinoplasty based
on three line stress relaxation. In classical nasal septum
reconstruction, the left Killian incision aims to penetrate at the
borderline between the skin and mucus; however in practice, this
incision is complicated and should be selected and modified based
on preoperative evaluation of 3D-CT images and DR. Preoperative
analysis in the current study also identified a fourth stress line,
as a potential region to excise a fraction of cartilage and bone
during surgery. The actual sites of excision were ultimately
determined by specific measurements and observations during
surgery, in order to maximally preserve the supporting structures.
However, the results of the current study are limited due to the
relatively small sample size. Therefore, future large sample
studies are warranted to validate the use of DR assessment in
determining the strain area in NSD.
In conclusion, 3D-CT reconstruction techniques and
subsequent mechanical analysis were used in the present study to
calculate the DR of NSD prior to surgery. The distribution of
stress lines at the site of NSD were also evaluated prior to
surgery. It was determined that the DR of NSD was significantly
associated with preoperative NAR and VAS score. Therefore,
preoperative measurement of the septum DR by 3D-CT reconstruction
techniques may be important in determining the specific surgical
approach required for nasal septoplasty.
Acknowledgements
The present study was supported by the Natural
Science Foundation of China (grant nos. 31400856, 81571790 and
81501573), the Longgang District Science and Technology Plan (grant
no. YLWS20140609120004346), the Key Laboratory Project of Shenzhen
(grant no. ZDSYS201506050935272) and the Innovation of Science and
Technology Commission of Shenzhen Municipality (grant no.
JCYJ20140411150916749, JCYJ20160429091935720).
References
|
1
|
Schuman TA and Labadie RF: Concurrent
nasal surgery and tympanoplasty in adults. Ear Nose Throat J.
89:E28–E32. 2010.PubMed/NCBI
|
|
2
|
Wang T, Han D, Zhang L, Zang H, Li Y and
Liu C: A modified septoplasty with three high tension lines
resection. Acta Otolaryngol. 130:593–599. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Atsumi A, Seo Y, Ishizu T, Nakamura A,
Enomoto Y, Harimura Y, Okazaki T, Abe Y and Aonuma K: Right
ventricular deformation analyses using a three-dimensional
speckle-tracking echocardiographic system specialized for the right
ventricle. J Am Soc Echocardiogr. 29:402–411, e2. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hall BK and Precious DS: Cleft lip, nose,
and palate: The nasal septum as the pacemaker for midfacial growth.
Oral Surg Oral Med Oral Pathol Oral Radiol. 115:442–447. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Steinbacher DM: Three-dimensional analysis
and surgical planning in craniomaxillofacial surgery. J Oral
Maxillofac Surg. 73 12 Suppl:S40–S56. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Swoboda S, Thulesius HL and Jessen M:
Paradoxical increase in nasal airway resistance after topical nasal
decongestion-does it really exist? A retro- and prospective study.
Clin Otolaryngol. 41:689–693. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fokkens W, Lund V and Mullol J; European
Position Paper on Rhinosinusitis and Nasal Polyps Group, : EP3O5
2007: European position paper on rhinosinusitis and nasal polyps. A
summary for otorhinolaryngologists. Rhinology. 45:97–101.
2007.PubMed/NCBI
|
|
8
|
Takahashi R: The formation of the nasal
septum and the etiology of septal deformity. The concept of
evolutionary paradox. Acta Otolaryngol Suppl. 443:1–160.
1987.PubMed/NCBI
|
|
9
|
Getz AE and Hwang PH: Endoscopic
septoplasty. Curr Opin Otolaryngol Head Neck Surg. 16:26–31. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Thulesius HL, Cervin A and Jessen M: Can
we always trust rhinomanometry? Rhinology. 49:46–52.
2011.PubMed/NCBI
|
|
11
|
Fischer H and Gubisch W: Nasal
valves-importance and surgical procedures. Facial Plast Surg.
22:266–280. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Georgalas C: The role of the nose in
snoring and obstructive sleep apnoea: An update. Eur Arch
Otorhinolaryngol. 268:1365–1373. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Moore M and Eccles R: Objective evidence
for the efficacy of surgical management of the deviated septum as a
treatment for chronic nasal obstruction: A systematic review. Clin
Otolaryngol. 36:106–113. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Orlandi RR: A systematic analysis of
septal deviation associated with rhinosinusitis. Laryngoscope.
120:1687–1695. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lee JE, Jung HJ, Chang M and Jin HR: A
novel wedge technique to correct the curved deviation of the
cartilaginous nasal septum. Auris Nasus Larynx. 41:190–194. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Akoglu E, Karazincir S, Balci A, Okuyucu
S, Sumbas H and Dağli AS: Evaluation of the turbinate hypertrophy
by computed tomography in patients with deviated nasal septum.
Otolaryngol Head Neck Surg. 136:380–384. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Obert L, Uhring J, Rey PB, Rochet S,
Lepage D, Leclerc G, Serre A and Garbuio P: Anatomy and
biomechanics of distal radius fractures: A literature review. Chir
Main. 31:287–297. 2012.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cardoso L and Weinbaum S: Changing views
of the biomechanics of vulnerable plaque rupture: A review. Ann
Biomed Eng. 42:415–431. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Moshirfar M, Edmonds JN, Behunin NL and
Christiansen SM: Corneal biomechanics in iatrogenic ectasia and
keratoconus: A review of the literature. Oman J Ophthalmol.
6:12–17. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Neskey D, Eloy JA and Casiano RR: Nasal,
septal, and turbinate anatomy and embryology. Otolaryngol Clin
North Am. 42193–205. (vii)2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yilmaz NA, Cicekcibasi AE, Emlik D, Yilmaz
MT, Keles B and Salbacak A: Morphometric analyses of the
development of nasal cavity in human fetuses: An anatomical and
radiological study. Int J Pediatr Otorhinolaryngol. 74:796–802.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cantrell H: Limited septoplasty for
endoscopic sinus surgery. Otolaryngol Head Neck Surg. 116:274–277.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Van Loosen J, Van Zanten GA, Howard CV,
Verwoerd-Verhoef HL, Van Velzen D and Verwoerd CD: Growth
characteristics of the human nasal septum. Rhinology. 34:78–82.
1996.PubMed/NCBI
|