Introduction
Atlantoaxial vertebra is the joint part of skull and
spine, characterized as a unique and complex anatomical structure.
There is an extension of cervical cord and medulla oblongata in
spinal canal. There are important structures, such as vertebral
artery, nerve root and venous plexus, outside the spinal canal
(1). The stability is mainly
maintained by the ligaments between ring pillow and ring axis.
Trauma, inflammation, congenital malformations and tumors are among
the main causes of instability (2).
Stability may be recovered only by internal fixation with bone
graft fusion because of its large mobility and lack of
self-repairing capacity.
With the constant progress in building new internal
fixation devices in recent years, a variety of methods have been
developed for atlantoaxial internal fixation with bone graft
fusion. Atlantal pedicle screw internal fixation surgery is
characterized by small injury and wide indications, and a large
number of anatomical and imaging measurements have been completed
(3). The entry points are selected
outward, the entry angle on cross section is generally inward or
vertical, and the exposure area of posterior arch of atlas is large
with high risk of injury and single entry point. Chen et al
(4) suggested the safe placement
area, but only selected the placement direction in the leaning
angle of 0 and 10°. The present study aimed to identify the safe
placement area and possibility of outward fixation for atlantal
pedicle screw placement via computed tomography (CT) measurement,
and to establish the individual measurement method for
intraoperative positioning. This may facilitate the preoperative
plan, reduce the incidence of surgical complications, be applied
clinically and produce excellent results. The entry point and
pedicle of pedicle screw were easily exposed, and the screw may be
directly implanted visually, as long as the extension of vertebral
artery and pedicle deformity were excluded before operation.
Resnick and Benzel method may be used as long as mastering the
entry point and direction, which was not the case in the present
study (5).
Materials and methods
Materials
Atlantal spiral CT (scan slice thickness of 1 mm) of
38 patients was used in the present study. There were 31 males and
7 females aged 24–80 years (average age, 48.7 years). Axial spiral
CT films with entry channel in the middle of left and right
pedicles were used. A vernier caliper (Nanjing New and High
Technology Industry Development Zone, Jiangsu, China) accurate to
0.02 mm and protractor (accurate to 0.1°).
Measurement contents and methods
Screw placement space. Screw accreta space (SAS) was
defined as the distance between the tangent lines of entry channel
on the atlantal cross section and inner edge of transverse foramen
and outer edge of spinal canal.
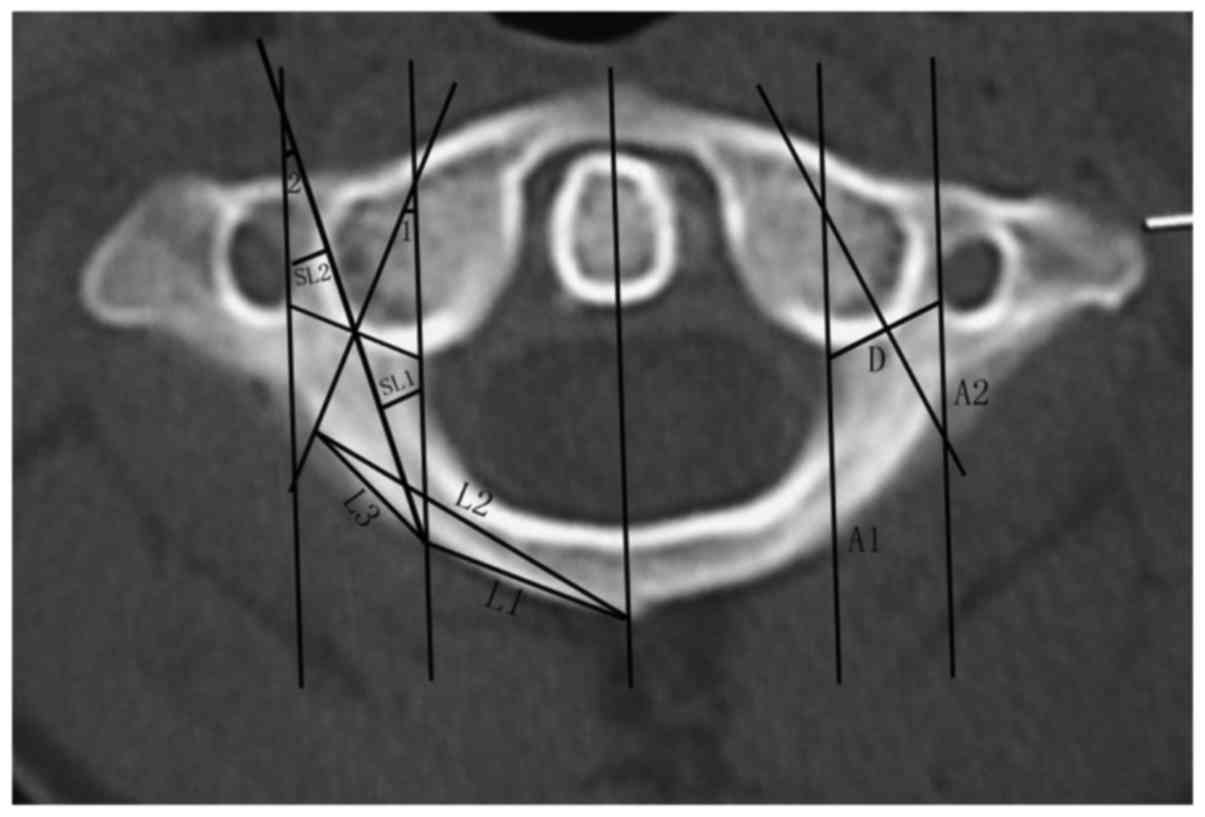
Determination of safety placement area
(SPA)
The line of anterior and posterior tubercles of
atlas was taken as the middle line of atlas, the parallel to middle
line was made across the outer edge of spinal canal and inner edge
of transverse foramen, and the intersections with posterior arch
were A1 and A2. SPA should not exceed the range of A1-A2. Pedicle
width was defined as the minimum distance from the outer edge of
the spinal canal to the inner edge of transverse foramen, and the
outer boundary was defined as the intersection of the perpendicular
bisector of the above line and posterior arch of atlas. If this
intersection was on the outside of the intersection of the parallel
line to the atlas middle line crossing the inner edge of transverse
foramen and posterior arch (A2), the latter was defined as the
external boundary. The inner boundary was defined as the
intersection of central axis of screw channel and posterior arch of
atlas when the placement space was 5 mm. If this intersection was
on the inside of the intersection of the parallel line to atlas
middle line crossing the outer edge of spinal canal and posterior
arch (A1), the latter was defined as the internal boundary
(Fig. 1).
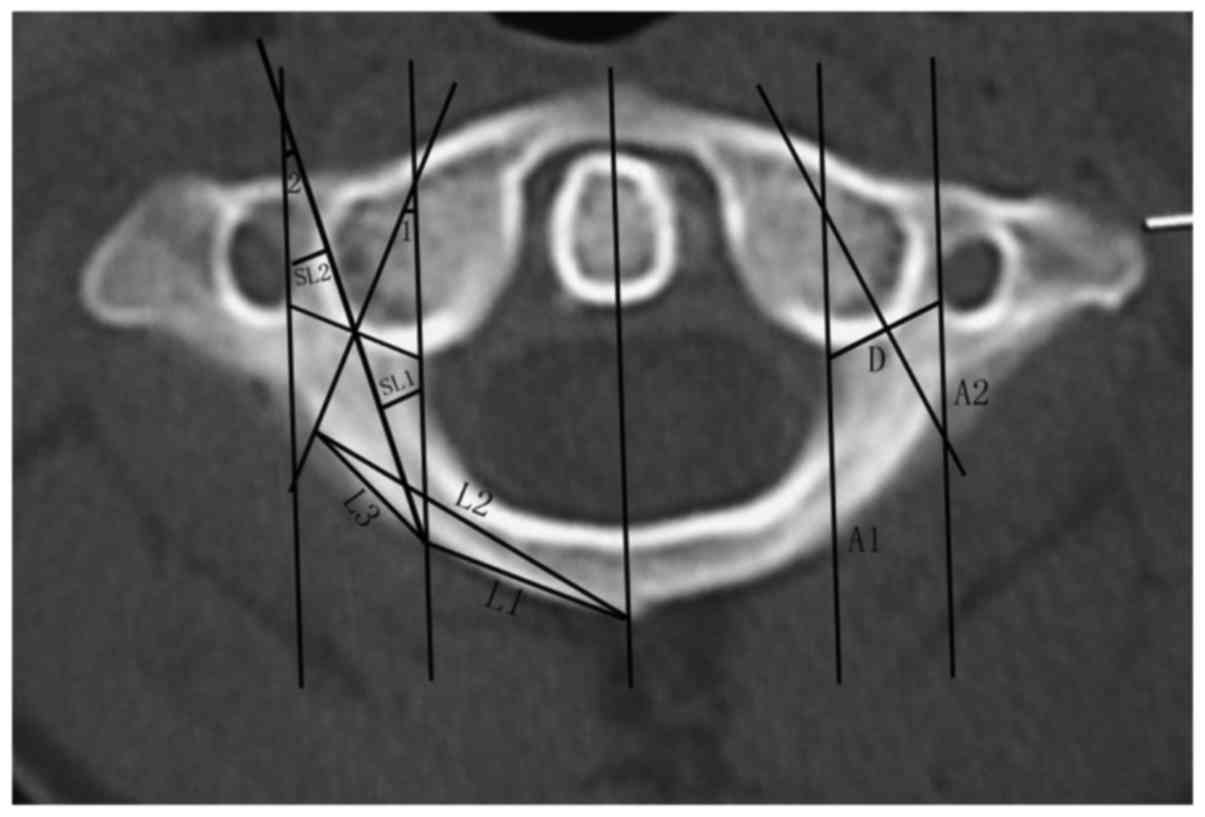 | Figure 1.Determination of SPA. D, pedicle
width; L1, distance between posterior tubercle and internal
boundary point of SPA; L2, distance between posterior tubercle and
external boundary point of SPA; L3, distance between SPA and
internal and external boundary points; SL1, minimum distance
between entry channel axis and outer edge of spinal canal; SL2,
minimum distance between entry channel axis and inner edge of
transverse foramen; SL1 + SL2, SAS distance; maximum inclined
angle, <1; maximum camber angle, <2. SPA, safety placement
area. |
SPA measurement
The distance between the inner and outer boundaries
of SPA and the posterior tubercle of atlas, the distance between
the inner and outer boundaries, the entry angle and the length of
entry channel, the width of atlantal pedicle and the minimum SAS
within SPA were measured.
Clinical application
General information
From March 2010 to June 2012, 7 patients received
the atlantal pedicle screw internal fixation (14 pieces). There
were 6 males and 1 female aged 26–55 years (average age, 40.57
years). There were 3 cases of Anderson II-type fracture of the
odontoid process (comminuted) (including 1 case of failed anterior
hollow screw operation), 1 case of old odontoid fracture, 1 case of
transverse atlantal ligament disruption, 1 case of os odontoideum
and 1 case of atlantoaxial intraspinal tumor.
Preoperative preparation
Before operation, all the patients routinely
received the atlantoaxial mouth-open and cervical lateral X-ray
examination, as well as left and right oblique and
flexion-extension X-ray examination for non-fresh fractures. The
results obtained through examination, revealed a poor atlantoaxial
stability in all the patients. Standard lateral film was used to
measure the bone thickness of basilar part of vertebral artery
groove. Upper cervical spinal CT scan and three-dimensional
reconstruction were performed to observe other malformations,
measure the height of posterior arch of atlas and related data
regarding SPA of atlantal pedicle. Magnetic resonance imaging (MRI)
examination was used to determine the situation of intraspinal
spinal cord. No pedicle dysplasia was detected in any of the
patients, and the height of posterior arch as well as the bone
thickness of basilar part of vertebral artery groove were >4
mm.
Surgical methods
Under general anesthesia, neck was kept in a
slightly flexed position. The median incision was made to expose
the posterior arch of atlas, and the posterior arch was separated
along the posterior periosteum until the measurement range. The
upper and lower posterior arch of atlas was probed using a nerve
detacher, followed by subperiosteal dissection, in order to fully
expose the entrance of atlantal pedicle. The approximate locations
of inner edge and lateral mass of posterior arch of atlas were
detected via a nerve detacher. Using the SPA data measured before
operation, the entry point in posterior arch was selected and
cortical bone was rubbed off using abrasive drilling to expose the
entrance of pedicle. According to the preoperative measurement, the
entry direction was selected, and the cancellous bone was scraped
away using curette (diameter, 2 mm). Walls of pedicle screw channel
were detected at any time, and if any issue occurred, the direction
was adjusted. The screw channel was detected using probe along the
pedicle screw channel until approximately 15 mm length was drilled,
and the surrounding bone suggested that the screw position was
good. The hole was drilled using pointed cone (diameter, 2.5 mm)
until the measurement length without breaking the anterior bone
cortex, and the hole was expanded slowly using the screw tap
(diameter, 3.0 mm). The probe was used again to detect the walls of
pedicle screw channel to confirm its integrity, and a screw
(diameter, 3.5 mm) was screwed into the channel. Using the
preoperative measurements, the pedicle screw was screwed into the
channel, and titanium rod was pre-bended and used to lift and fix
the dislocation according to the size of atlantoaxial dislocation.
We also determined whether foramen magnum decompression and
posterior arch of atlas was needed. The rough surfaces of posterior
arch of atlas, vertebral plate and spinous process cortex were
grounded, followed by bone graft fusion as well as routine
placement and drainage.
Statistical analysis
We used SPSS 19.0 statistical software for our
statistical analyses. Data were presented as mean ± standard
deviation (mean ± SD) and t-test was used for the comparison of
data on the left and right sides. P<0.05 was considered to
indicate a statistically significant difference.
Results
CT image measurement results
The camber angle was negative and the width of
pedicle was ~9.15±2.57 mm, which was able to safely accommodate 3.5
mm diameter screws (Table I). SPA
was located in posterior arch of atlas. It was 18.35±2.86 to
25.26±1.76 mm away from the posterior tubercle, the entry angle was
ranged from −9.09±7.45° outward to 18.72±17.42° inward, and the
length of screw channel ranged from 26.20±2.69 to 27.04±2.51 mm.
The width of SPA was up to 6.91±7.66 mm on posterior arch, and the
entry angle on cross section was up to 27.81±10.32°. There were
some individual differences. There were two cases (5.26%) with the
pedicle width of ~5 mm on four sides and in three cases (5.26%) we
observed the pedicle width of ~5 mm on four sides but SAS width
within SPA of <5 mm. Over 10% of the cases were not suitable for
pedicle fixation. There was one case with the smallest left
vertebral artery foramen and pedicle width of 27.43 mm, indicating
the abnormal vertebral artery shape.
 | Table I.CT image measurement. |
Table I.
CT image measurement.
| Parameters | Left side | Right side | Two sides |
|---|
| Pedicle width
(mm) | 9.41±3.37
(5.04–27.43) | 8.89±1.36
(5.47–12.30) | 9.15±2.57 |
| Maximum entry angle
inward on cross section (°) | 18.3±5.7
(5.1–29.3) | 19.1±5.7
(2.4–31.4) | 18.72±17.42 |
| Screw channel length
under the maximum leaning angle (mm) | 25.85±2.87
(18.97–31.87) | 26.55±2.48
(19.32–30.39) | 26.20±2.69 |
| Distance from
external boundary of SPA to posterior tubercle (mm) | 25.47±1.94
(19.50–29.10) | 25.06±1.56
(22.08–28.99) | 25.26±1.76 |
| Minimum entry angle
on cross section (°) | −9.1±7.6
(−23.9–9.4) | −9.1±7.4
(−20.6–15.8) | −9.09±7.45 |
| Screw channel length
under the minimum entry angle (mm) | 27.31±2.62
(21.48–31.60) | 26.76±2.39
(21.27–31.74) | 27.04±2.51 |
| Distance from
internal boundary of SPA to posterior tubercle (mm) | 18.52±2.89
(13.26–27.95) | 18.18±2.85
(13.54–27.69) | 18.35±2.86 |
| Screw channel width
under the minimum entry angle (mm) | 5.37±0.94
(3.08–9.78) | 5.43±0.74
(3.96–7.05) | 5.40±0.84 |
| Distance from
internal boundary to external boundary of SPA (mm) | 6.95±2.82
(0–14.53) | 6.87±2.59
(0–10.35) | 6.91±7.66 |
| Entry angle range in
SPA (°) | 27.37±10.69
(0–44.2) | 28.25±10.06
(0–43.6) | 27.81±10.32 |
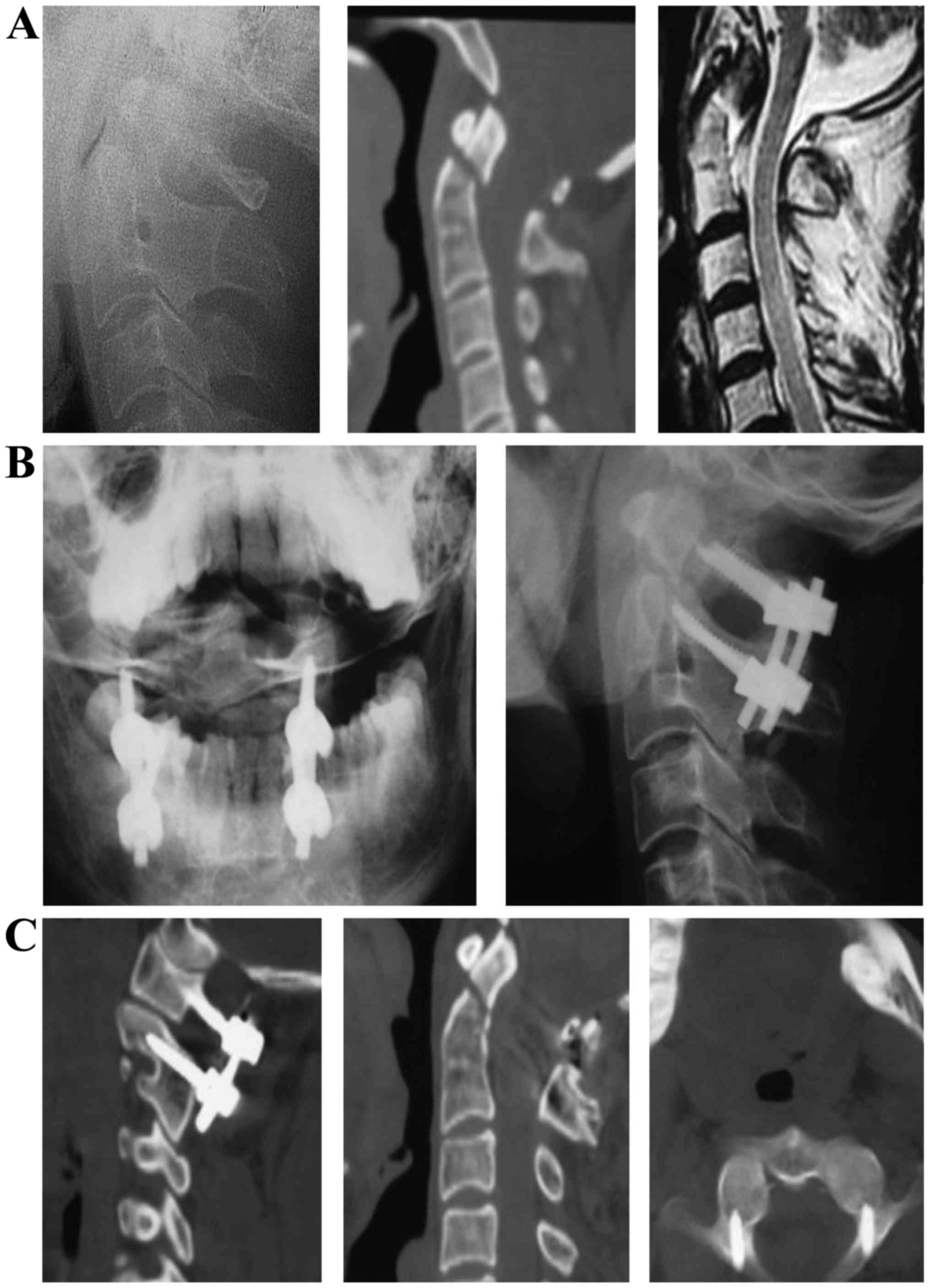
Clinical application results
The total amount of bleeding in all patients, during
the operation, ranged from 60 to 300 ml for 90–120 min. Patients
did not suffer any injury to their vertebral artery, nerve root and
spinal cord. Postoperative lateral side X-ray photograph and spiral
CT examination for cervical spine showed that 14 pedicle screws had
the ideal position within SPA measured before operation, and there
was no perforation of the pedicle bone cortex. During the
postoperative follow-up for 6 to 12 months, there was no internal
fixation loosening and fracture. After the bone grafting, all 7
patients had the bone fusion. Figs.
2 and 3 showed pre- and
post-operation images for two typical cased with odontoid
fractures.
Discussion
Anatomical basis of atlantal pedicle
internal fixation
Atlas has a special anatomical structure, where the
bone ring is composed of the anterior arch, posterior arch and two
lateral masses and transverse process without vertebral body and
spinous process but with huge lateral masses on both sides. The
connection part of posterior arch of atlas and lateral mass is
similar to the pedicle of other vertebrae in structure and
mechanics. The posterior arch of atlas is fixed by the pedicle
screw, which is referred to as the atlantal pedicle screw by
Resnick and Benzel (5). Ma et
al (6) suggested that the
vertebral artery groove was the weakest in the structural mechanics
and anatomy of atlas, which is termed as the ‘isthmus’ of atlas.
Tan et al (7) observed 50
cases of vertebral artery grooves, including 2 sides of non-groove
type, 83 sides of shallow groove type, 7 sides of deep groove type
and 8 sides of ring groove type (2 sides of full-ring type and 6
sides of half-ring type), and the deep groove type and ring groove
type accounted for 15%. The vertebral artery of ring-type vertebral
artery groove is actually embedded in the bone tube, and the upper
edge of bone tube may be mistaken as the upper edge of posterior
arch, causing the injury to vertebral artery. The bone thickness at
the bottom part of deep-type vertebral artery groove is small, and
vertebral artery may also be damaged during the entry via posterior
arch. There are two commonly accepted theories to explain the
possible causes of atlantal artery groove ring, congenital
malformations and acquired atlanto-occipital ligament ossification
(8).
Feasibility of atlantal pedicle screw
fixation
Atlas connects the skull and spine, and atlantoaxial
dislocation or atlanto-occipital instability may directly oppress
the medulla oblongata and endanger the lives of patients.
Therefore, the stability reconstruction of atlas is essential.
Prior studies have suggested that the cervical spine screw fixation
technique is the three-column fixation (9). A large number of studies have shown
that its biomechanical stability is significantly superior to the
conventional cervical anterior plate fixation, posterior lateral
mass fixation and anterior-posterior combined fixation (10). Atlantoaxial screw fixation technique
introduced by Magerl and Seemann reported a better biomechanical
stability (especially the rotary stability) (11). The bone graft fusion rate has been
reported to be close to 100% via the clinical combination of
posterior wire fixation (12).
However, this operation had no advantage in the anti-axial
displacement, and the complete restoration was needed before screw
placement, thus the risk of vertebral artery and sublingual nerve
injury was large. In addition, this method was not appropriate for
obese patients and those with thoracic kyphosis, barrel chest and
other diseases in which the cervical spine could not bend
excessively. In 1994, Goel and Laheri (13) reported the atlantal lateral mass
screw technique for the first time, and Harms and Melcher (14) reported the application of
atlantoaxial lateral mass screw fixation technique in 2001. When
applying this technique, C2 nerve root and peripheral venous plexus
should be retracted, and C2 nerve root was cut off, which may lead
to nerve damage or bleeding. Resnick and Benzel (5) reported that the atlantal lateral mass
could accommodate the lateral mass screw with the diameter of up to
7 mm. Resnick et al (15)
first reported one atlantoaxial pedicle screw technique, and
treated one female patient for whom the Magerl technique was not
suitable. Through a large number of anatomical and imaging
measurements and biomechanical studies, Chinese scholars have
argued that atlantal pedicle has the conditions of screw placement.
When using pedicle screw technique, the lateral mass and anatomical
structure of posterior arch do not need to be peeled off, and it is
easier to push away the C2 nerve root and venous plexus, thus the
risk of injury is reduced with less bleeding, longer screw channel
than lateral mass screw and firmer fixation (16).
Anatomical measurement of atlantal
lateral mass and pedicle screw channel
Tan et al (17) measured the dry atlas bones in 50
adults, and reported that the middle height of lateral mass was
13.02±1.18 mm/13.11±1.23 mm (left/right, the same below), the
transverse diameter of lateral mass was 11.52±2.97 mm/11.76±2.97
mm, the posterior arch height at the bottom of vertebral artery
groove was 4.58±0.65 mm/4.72±0.68 mm, and the posterior arch height
at the entry point was 5.39±1.58 mm/11.76±2.97 mm. The gap between
entry point in channel direction and front edge of vertebral artery
groove was 10.60±2.87 mm/10.79±1.51 mm. Xia et al (18) measured the dry atlas bones in 30
adults, and reported that the middle width of lateral mass was
11.6±1.4 mm and the thickness of the central point of lateral mass
was 12.7±1.0 mm, and the posterior arch thickness of vertebral
artery was 4.7±1.0 mm, meeting the requirement of inserting screw
with the diameter of 3.5 mm. A large number of anatomical data
showed that atlantal lateral mass and atlantal pedicle met the
requirement of internal fixation of screw with the diameter of 3.5
mm (19–24). Nevertheless, there were also risks of
pedicle screw fixation in some cases of smaller posterior arch
height. The posterior arch height in the thinnest bone at the
bottom of vertebral artery groove was significantly smaller
compared with that of the posterior arch width, and smaller than
the posterior arch height at the entry point. The posterior arch
height at this point is the key to the diameter of screw and
successful operation. The pedicle width and isthmus height are the
main factors limiting the placement of pedicle screw. When the
pedicle screw with the diameter of 3.5 mm is placed, the pedicle
width and isthmus height cannot be smaller than 5 mm. The pedicle
width was measured by the author; the pedicle width was 9.15±2.57
mm, including two cases (5.26%) with the pedicle width of >5 mm
on 4 sides (5.26%). Although the pedicle width was >5 mm, the
width of SAS within SPA was <5 mm.
Biomechanics of internal fixation of
atlantal pedicle screw
Xia et al (25) reported that the pullout force of
atlantal lateral mass posterior screw was significantly smaller
than that of occipital screw, but had no significant difference
with the pullout force of axis pedicle screw. Ma et al
(26) suggested that the pullout
force of bicortical atlantal pedicle screw fixation was the
largest, and there was no significant difference in the pullout
force between the monocortical atlantal pedicle screw fixation and
the bicortical atlantal lateral mass fixation and monocortical
pedicle screw fixation suggesting that the bicortical screw
fixation should be selected in the atlantal lateral mass screw
fixation, and the monocortical screw fixation should be selected in
the atlantal pedicle screw fixation. Zhang et al (27) showed that the atlantal pedicle screw
fixation method could provide a higher stability than atlantal
lateral mass internal fixation.
Imaging measurement of atlantal
pedicle screw channel
Lin et al (28) measured the atlantal CT results in 120
Chinese patients, and reported that the lateral mass thickness was
approximately 12.8 mm, the anteroposterior diameter of lateral mass
was approximately 21.5 mm, and the transverse diameter of lateral
mass was 11.8–13.3 mm, fully meeting the requirement of placing the
screw with the diameter of 3.5 mm. Tan et al (29) performed multi-section CT scan and
measurement for atlantal pedicle screw fixation channel using 50
samples of atlantal bone, and the results showed that the middle
height of lateral mass was 16.98±1.81 mm/16.55±1.07 mm, the
posterior arch height at the bottom of vertebral artery groove was
4.83±0.76 mm/4.94±0.95 mm, the gap between the entry point in the
entry direction and the anterior vertebral artery groove was
10.42±2.02 mm/10.88±1.48 mm, the leaning angle was approximately 0°
and the camber angle was approximately 5°, which was consistent
with the caliper measurement result of dry bone. A large number of
anatomical and imaging measurements of atlas showed that both of
them were consistent, which could make the atlantal pedicle screw
internal fixation feasible, and the entry point, direction and
depth could be selected through measurement. Nevertheless, the
detailed X-ray and three-dimensional spiral CT measurements
provided the individualized data to guide the safe placement of
atlantal pedicle screw during the operation.
Selection of entry point of atlantal
pedicle screw fixation and placement technique
For the atlantal pedicle screw, the entry point
should be clear and easy to determine. During the entry process,
the vertebral artery in the vertebral artery groove above should be
protected, the vertebral artery in transverse foramen outside
should also be protected, the venous plexus between C1 and C2 and
C2 nerve root below should be avoided as far as possible, and the
spinal dura mater and spinal cord inside should be protected. The
key to the atlantal pedicle screw fixation is the selection of
entry point and entry angle. The entry angle on the sagittal plane
can be measured through the standard cervical lateral film, 5–10°
upward. Different scholars offered diverse views on the selection
of entry angle and inclined angle on cross section. Tan et
al (17) suggested that the
entry point was defined as the intersection of 18–20 mm on both
sides of the middle point of posterior tubercle of atlas and 2 mm
above the lower edge of the posterior arch, and the entry direction
was defined as 5° vertical to the coronal plane. Wang et al
(30) reviewed 159 cases of atlantal
pedicle screw fixation or lateral mass fixation with complete image
data, detected the inner edge of atlantal lateral mass below using
nerve dissector along the vertebral pedicle, and speculated the
entry point of atlantal pedicle or lateral mass internal fixation.
Chen et al (4) measured 30
atlanto-axis with normal shape for CT thin-slice scan and
three-dimensional reconstruction, and measured that SAS under the
leaning angle of 0 and 10° on cross section was 7.81±1.28 mm and
9.69±1.23 mm (>3.5 mm). The entry point under the leaning angle
of 10° was 2 mm outward compared with that under the leaning angle
of 0°. The results of that study showed that the entry point of
atlantal lateral mass screw should also have the corresponding SPA
on cross section of posterior arch, rather than a single-entry
point, and the entry point and direction should be determined based
on the preoperative X-ray and CT measurements. He et al
(31) measured 48 dry atlas bones.
According to the bone thickness at the bottom of vertebral artery
groove, with the adults' atlantal pedicle screw with the diameter
of 3.5 mm as the standard, the posterior arch can be divided into
three types based on the posterior arch at the bottom of vertebral
artery: i) Ordinary type, posterior arch height >3.5 mm
accounting for 83%; ii) mild variation, posterior arch height
1.75–3.5 mm accounting for 13%; and iii) severe variation,
posterior arch height <1.75 mm accounting for 4%. During the
operation, the entry method is determined according to the bone
thickness at the bottom of the vertebral artery groove measured by
three-dimensional spiral CT. Pedicle screw fixation can be used for
the ordinary type and mild variation, but the screw is likely to
break through the bone below pedicle for mild variation. The
fixation of severe variant is similar to that of lateral mass screw
without going through the pedicle, however, the entry point is in
the intersection of lower edge of posterior arch and lateral mass,
and the typical entry point of lateral mass screw is in a high
position; therefore, the risk of damaging C2 nerve root and venous
plexus is small. Tan et al (32) suggested the ‘pedicle-exposed
placement method’. According to preoperative imaging measurements,
the entry point and direction were determined, the bone cortex was
removed on the surface of entry point on posterior arch of atlas to
expose the entrance of pedicle, and the hole was drilled by hand.
For the height of posterior arch of atlas <4 mm, the vertebral
artery and venous plexus above the posterior arch of atlas could be
peeled off to protect the vertebral artery, expose the initial
segment of lateral mass and posterior arch, and the atlantal
pedicle screw with the diameter of 3.5 mm was placed safely using
the pedicle-exposed placement method. Screw was exposed below the
vertebral artery, the fascia tissue was taken above the screw, and
the vertebral artery was isolated and protected.
Methods and significance of the
present study
One of the keys to the success of atlantal pedicle
screw is the selection of entry point and direction. Most of the
above scholars chose the single-entry point, but the positioning
method was different, and the entry angle was mostly 0–10°.
Although Chen et al (4)
recommended the concept of SPA, practically the inward entry was
employed. Hao et al (33)
suggested the anatomical measurement of outward entry, and used the
corresponding posterior arch to lateral edge of spinal canal as the
entry point. In this study, the possible SPA of entry point and the
possible entry angle were detected through atlantal CT
cross-sectional measurement, in order to guide the screw placement,
achieving satisfactory results. In the measurement, posterior
tubercle of atlas was taken as the reference, and the straight-line
distance from posterior tubercle to entry point was measured
directly to facilitate the intraoperative measurement. In the past,
the vertical distance between simulated middle lines of entry point
and posterior and anterior tubercle of atlas. Consequently, the
intraoperative measurement was difficult with numerous errors. The
entry angle on the sagittal plane of the atlantal pedicle screw was
measured through the standard atlantoaxial lateral film, which is
relatively simple.
To determine SPA of the atlantal pedicle screw,
screw placement space was defined as the distance between the
tangent lines of entry channel on atlantal cross section and inner
edge of transverse foramen and outer edge of spinal canal. A large
number of studies argued that to insert the screw with the diameter
of 3.5 mm securely, the placement space of atlantal pedicle screw
should be at least 5 mm, therefore the placement space should also
be >5 mm (34). This could ensure
the safety of screw placement and prevent the screw from breaking
through the bone cortex into the spinal canal or transverse
foramen. The width of atlantal pedicle is not accurately defined;
thus, the author defined the pedicle width as the minimum distance
from the outer edge of spinal canal to the inner edge of transverse
foramen. The author also defined the outer boundary as the
intersection of perpendicular bisector of the above line and
posterior arch of atlas. The line of posterior and anterior
tubercles of atlas was taken as the middle line of atlas, and the
parallel line to middle line was made crossing the outer edge of
spinal canal and inner edge of transverse foramen. If this
intersection was outside the intersection of the parallel line to
atlas middle line crossing the inner edge of transverse foramen and
posterior arch, the latter was defined as the external boundary.
The inner boundary was defined as the intersection of central axis
of screw channel and posterior arch of atlas when the placement
space was 5 mm. If this intersection was inside the intersection of
parallel line to atlas middle line crossing the outer edge of
spinal canal and posterior arch, the latter was defined as the
internal boundary.
The distance between the inner boundary of SPA of
atlantal pedicle screw and posterior tubercle was approximately 18
mm, which was greater than the radius of spinal canal measured by
several scholars. The distance between the outer boundary of SPA
and posterior tubercle was approximately 25 mm, which was also
greater than the entry point data reported before, which may be due
to the different measurement methods used. The SPA width of the
atlantal pedicle screw was approximately 7 mm, and the entry angle
within SPA ranged from 9° outward to 18° inward with the span of
nearly 27°, which was safe within this range. Each entry point
within SPA had a corresponding optimal entry angle. When it was
closer to the lateral boundary the SAS was larger and the risk of
injury to the spinal and vertebral artery was smaller. In other
words, it should be exposed to the lateral boundary as far as
possible during the operation, and the outer boundary of SPA should
be selected as the entry point. However, if it was exposed outward,
the risk of venous plexus bleeding was high. Usually bleeding was
successfully controlled using hemostasis by compression, but if it
was difficult to stop bleeding and impossible to expose to the
posterior arch, the pedicle screw was placed according to
preoperative measurement. All 7 patients in the present study,
successfully received the pedicle screw placement using this
method, and the position was proved to be ideal. When the pedicle
screw was placed, the bone cortex at the entry point was ground to
expose the entrance of entry channel. According to the pipeline
dredge method (35), the curette
with the diameter of 2 mm was used to remove the cancellous bone in
a rotation mode along the entry direction of pedicle screw. The end
of curette was the arc-shaped with single-sided blade, thus when
the curette hit the cortical bone of pedicle, it could turn into
the pedicle lumen with soft bone. The walls of pedicle screw
channel should be detected at any time, and if it was difficult to
move forward, the direction could be adjusted. Tan et al
(7) reported that the gap between
entry point in the direction of entry channel and anterior margin
of vertebral artery was approximately 11 mm. Therefore, 15 mm-deep
drilling reached the wide lateral mass across the isthmus, and
bradawl could be used to continue drilling to the appropriate
depth. The measurement results showed that the length of entry
channel was 26–27 mm, which was roughly the same as the measurement
data of other scholars. There were 8 sides (10.53%) without SPA in
the group, which meant that SAS was <5 mm within SPA, so pedicle
screw fixation was not appropriate.
In conclusion, a large number of anatomical
structure observation of atlas, measurements of lateral mass of
atlas and pedicle and biomechanical studies have shown that atlas
has the pedicle structure similar to other cervical vertebra with
the conditions for posterior pedicle screw fixation. The results of
imaging measurement, especially spiral CT and X-ray measurement,
were consistent with the anatomical measurements, thus the
preoperative imaging measurement could be applied to guide the
operation. A large number of clinical application results have
proven that the atlantal pedicle screw has the strong holding
force, good stability and high bone graft fusion rate, and the
operation is characterized by the short time, less bleeding and
relatively simple procedure, which can be widely used in the
treatment of atlantoaxial diseases. This includes Anderson II-type
fractures that anterior fixation could be applied, old odontoid
fractures, transverse atlantal ligament disruption, atlantoaxial
dislocation, odontoid process dysplasia or os odontoideum, basilar
impression, rheumatoid arthritis and atlantoaxial tumor. As long as
the atlantal pedicle and lateral mass was not damaged and the
preoperative measurement showed that the pedicle screw placement
was feasible, atlantal pedicle screw fixation could be performed.
Through the spiral CT measurement of atlantal pedicle screw, it was
found the entry point of atlantal pedicle screw was not definitely
one point. There was a safe placement area, and each entry point
within SPA had its optimal entry angle. The detailed imaging
measurement before operation could determine the individual
placement area and entry angle, and bloodless operation should be
performed as far as possible. Pipeline dredge method may be used in
the screw channel drilling to safely place the atlantal pedicle
screw.
References
|
1
|
Jiang YW, Xia H, Wang ZY, Wu ZH, Ma XY,
Wei GJ, Ma LM, Huang JL, Zheng G and Feng XL: Variation of
craniocervical junction volume as an effective parameter for
basilar invagination treatment. Eur Rev Med Pharmacol Sci.
19:1754–1760. 2015.PubMed/NCBI
|
|
2
|
Duan S, He H, Lv S and Chen L:
Three-dimensional CT study on the anatomy of vertebral artery at
atlantoaxial and intracranial segment. Surg Radiol Anat. 32:39–44.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abumi K, Shono Y, Ito M, Taneichi H,
Kotani Y and Kaneda K: Complications of pedicle screw fixation in
reconstructive surgery of the cervical spine. Spine (Phila Pa
1976). 25:962–969. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen Q, Shen J, Li F and Yang D:
Establishment and application of safe fixation area of lateral mass
of atlas. Chin J Trauma. 22:404–407. 2006.(In Chinese).
|
|
5
|
Resnick DK and Benzel EC: C1-C2 pedicle
screw fixation with rigid cantilever beam construct: Case report
and technical note. Neurosurgery. 50:426–428. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ma X, Zhong S, Liu J, Yin Q, Xu D, Xia H,
Wu Z and Ding Z: The anatomic study on the feasibility of posterior
pedicle screw fixation on atlas. Chin J Clin Anat. 21:554–555.
2003.(In Chinese).
|
|
7
|
Tan M, Zhang G, Li Z, et al: Research on
atlas measurement and lateral screw fixation channel via posterior
Arch. Chin J Spine and Spinal Cord. 12:5–8. 2002.(In Chinese).
|
|
8
|
Ma X, Yin Q, Zhong S, Liu J, Xia H, Wu Z,
Xu D and Ding Z: Anatomic relationship between the posterior
neurovascular plexus of atlantoaxial joint and the placement of
atlas pedicle screw. Chin J Clin Anat. 23:454–457. 2005.(In
Chinese).
|
|
9
|
Abumi K, Kaneda K, Shono Y and Fujiya M:
One-stage posterior decompression and reconstruction of the
cervical spine by using pedicle screw fixation systems. J
Neurosurg. 90:19–26. 1999.PubMed/NCBI
|
|
10
|
Abumi K, Ito M and Sudo H: Reconstruction
of the subaxial cervical spine using pedicle screw instrumentation.
Spine (Phila Pa 1976). 37:E349–E356. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Abumi K and Kaneda K: Pedicle screw
fixation for nontraumatic lesions of the cervical spine. Spine
(Phila Pa 1976). 22:1853–1863. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang C, Yan M, Zhou H, Wang S and Dang G:
Atlantoaxial transarticular screw fixation with morselized
autograft and without additional internal fixation: Technical
description and report of 57 cases. Spine. 32:643–646. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Goel A and Laheri V: Plate and screw
fixation for atlanto-axial subluxation. Acta Neurochir (Wien).
129:47–53. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Harms J and Melcher RP: Posterior C1-C2
fusion with polyaxial screw and rod fixation. Spine. 26:2467–2471.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Resnick DK, Lapsiwala S and Trost GR:
Anatomic suitability of the C1-C2 complex for pedicle screw
fixation. Spine. 27:1494–1498. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kawaguchi Y, Nakano M, Yasuda T, Seki S,
Hori T and Kimura T: Development of a new technique for pedicle
screw and Magerl screw insertion using a 3-dimensional image guide.
Spine (Phila Pa 1976). 37:1983–1988. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tan M, Wang H, Wang Y, Zhang G, Yi P, Li
Z, Wei H and Yang F: Morphometric evaluation of screw fixation in
atlas via posterior arch and lateral mass. Spine. 28:888–895. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xia H, Zhong S, Liu J, et al: Applied
anatomy of lateral atlantoaxial posterior screw fixation. Chin J
Clin Anat. 20:83–85. 2002.(In Chinese).
|
|
19
|
Yin D, Yuan L, Xia H and Li J:
Quantitative measurements and clinical significance of lateral mass
of atlas. Chin J Clin Anat. 21:241–242. 2003.(In Chinese).
|
|
20
|
Yan M, Wang C, Dang G, et al: Anatomical
basis of internal fixation of lateral mass of atlas and isthmus of
axis. Chin J Spine and Spinal Cord. 13:25–27. 2003.(In
Chinese).
|
|
21
|
Ma X, Zhong S, Liu J, Yin Q, Xu D, Xia H
and Wu Z: Anatomical measurement of lateral mass screw fixation of
posterior arch of atlas. Chin J Spine and Spinal Cord. 14:23–25.
2004.(In Chinese).
|
|
22
|
Li G, Zuo B, Feng Z, Chen J and Lin J:
Measurement of atlas and its significance for clinical application.
Sichuan J Anat. 18:18–21. 2010.(In Chinese).
|
|
23
|
Hao D, Fang X, Wu Q, et al: Anatomical
study on stability reconstruction of upper cervical spine via
posterior arch of atlas. Chin J Orthoped. 31:339–342. 2011.(In
Chinese).
|
|
24
|
Chen Q, Jin D and Xiao Z: Anatomical study
on transpedicle screw fixation of atlas and axis. J Guangxi Med
Univ. 26:365–368. 2009.(In Chinese).
|
|
25
|
Xia H, Zhong S, Liu J, et al: Feasibility
research on posterior screw fixation of lateral mass of atlas. Chin
J Orthoped. 10:888–891. 2002.(In Chinese).
|
|
26
|
Ma X, Zhao W, Yin Q, et al: Biomechanical
evaluation of posterior atlantal monocortical or bicortical bone
screw fixation strength. Chin J Spine and Spinal Cord. 15:34–37.
2005.(In Chinese).
|
|
27
|
Zhang H, Bai J, Tan M and Yi P:
Biomechanical analysis of the posterior pedicle screw and the
lateral mass screw on the atlas. J Tsinghua Univ (Sci Technol).
48:419–422. 2008.(In Chinese).
|
|
28
|
Lin F, Chi Y, Xu C, Chen T, Lin X and Lin
Z: Anatomical measurement of atlantoaxial imaging of Chinese and
its clinical significance. J Wenzhou Med Coll. 34:304–305. 2004.(In
Chinese).
|
|
29
|
Tan M, Wang H, Zhang G, Yi P, Liang L, Wei
H, Yang F and Li Z: CT measurement of the path of screw fixation in
atlas via posterior arch and lateral mass. Chin J Spine and Spinal
Cord. 13:28–31. 2003.(In Chinese).
|
|
30
|
Wang S, Wang C, Yan M, Zhou H and Dang G:
Analysis of veracity of the C1 lateral mass screw insertion in the
atlantoaxial fixation. Chin J Surg. 46:115–117. 2008.(In Chinese).
PubMed/NCBI
|
|
31
|
He F, Yin Q and Zhao T: An anatomic study
of the pedicle screw fixation. Chin J Orthopaed Trauma. 10:257–259.
2008.(In Chinese).
|
|
32
|
Tan M, Tang X, Yi P, et al: Clinical
application of atlantal pedicle screw placement technique. J Spine
Surg. 9:148–152. 2011.(In Chinese).
|
|
33
|
Hao D, Xu Z, He B, Guo H, Liu T and Wang
X: Atlantoaxial pedicle screw fixation for old odontoid fracture
combined with atlantoaxial instability. Chin J Trauma. 27:121–124.
2011.(In Chinese).
|
|
34
|
Wang L, Liu C, Zhao Q and Tian J:
Posterior pedicle screw fixation for complex atlantoaxial fractures
with with atlanto-dental interval of ≥5 mm or C2-C3 angulation of
≥11°. J Orthop Surg Res. 9:1042014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tan M, Zhang G, Yi P, Wang H, Wei H, Yang
F and Li Z: Placement of cervical spine pedicle screw with dredging
pipe method. Chin J Spine and Spinal Cord. 12:405–410. 2002.(In
Chinese).
|