Introduction
Lung cancer is a malignant tumor that severely
threatens human health (1), and is
characterized by high morbidity and mortality rates. Furthermore,
lung cancer accounts for the highest incidence of male cancer and
mortality rate of all malignant tumors in males, and the second
highest in females worldwide. The high morbidity and mortality of
lung cancer is closely associated with the alterations observed in
the biological behavior of lung cancer cells. Non-small cell lung
cancer (NSCLC) comprises approximately 80–85% of all the lung
cancer cases (2); however, the
treatment of NSCLC remains challenging, with a low overall 5-year
survival rate (3,4). As a result of poor early diagnosis and
the high rates of recurrence and metastasis, the curative effect of
surgical treatment for NSCLC is poor (5). In addition, the incidence rate of NSCLC
has been reported to be rising in recent decades (6). Therefore, it is urgent to explore novel
therapeutic means for NSCLC treatment.
Mucin 1 (MUC1), a large trans-membrane protein, is
mainly expressed on the apical border of normal secretory
epithelial cells (7). It is
synthesized as a single polypeptide, while N-terminal (MUC1-N) and
C-terminal (MUC1-C) are its two subunits. MUC1 is frequently
overexpressed in epithelial cancer (8), and previous evidence has verified that
the abnormal upregulation of MUC1 in tumors is involved in the
regulation of cancer transformation, occurrence, metastasis and
invasion. Studies have also indicated that MUC1 interacts with
various signals that participate in cell adhesion, growth and
survival, including protein kinase C, c-Src, Grb2/SOS and various
member of the human epidermal growth factor receptor family
(9,10). Furthermore, MUC1 serves critical
roles in the regulation of the phosphoinositide 3-kinase/protein
kinase B (AKT) and B-cell lymphoma-xL pathway activation.
A previous study (11) suggested that MUC1 may be a novel
target for lung cancer treatment, and may be involved in the
regulation of lung cancer cell growth. However, the exact role of
MUC1 in NSCLC progression and the underlying molecular mechanisms
involved remain poorly understood. Thus, in the present study, the
aim was to investigate the role of MUC1 in the development of NSCLC
and further explore the underlying molecular mechanisms.
Materials and methods
Cell culture
The human NSCLC cell line NCI-H1650 (CRL-5883) and
normal human lung epithelial cell line BEAS-2B (TCP-2030) were
obtained from the American Type Culture Collection (Manassas, VA,
USA). BEAS-2B cells were grown in bronchial epithelial cell growth
medium (Lonza, Basel, Switzerland). NCI-H1650 cells were cultured
in RPMI-1640 medium containing 10% fetal bovine serum (Corning
Incorporated, Corning, NY, USA), 1% penicillin-streptomycin
solution (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA)
in a 5% CO2 incubator at 37°C. Cell were passaged every
2–3 days.
Cell transfection
At 24 h before the transfection, 1×105
NCI-H1650 cells/well were seeded in a 6-well plate. To investigate
the role of MUC1 in the development of NSCLC, MUC1-siRNA or a
control-siRNA (synthesized by Shanghai GenePharma Co., Ltd.,
Shanghai, China) were transfected into NCI-H1650 cells with 30 µl
Lipofectamine 2000 transfection reagent (Invitrogen; Thermo Fisher
Scientific, Inc.) following the manufacturer's instructions.
Following incubation for 48 h, the transfected NCI-H1650 cells were
used for subsequent analysis.
Cell proliferation assay
NCI-H1650 cell proliferation was determined by Cell
Counting Kit-8 (CCK-8; Dojindo Molecular Technologies, Inc.,
Kumamoto, Japan) assay, in line with the manufacturer's
instructions. Briefly, at 48 h post-transfection with MUC1-siRNA or
the control-siRNA, NCI-H1650 cells were collected, reseeded into
96-well plates at a density of 3×103 cells/well and then
incubated for 24 h at 37°C under 5% CO2. Subsequently,
CCK-8 solution (10 µg/ml) was added to the cell culture medium in
each well and incubated at 37°C for 2 h. The optical density value
at 450 nm was assayed using a spectrophotometer. All experiments
were performed in triplicate.
Cell apoptosis assay
For the analysis of cell apoptosis, at 48 h after
transfection, the NCI-H1650 cells were collected, washed three
times with phosphate-buffered saline (PBS) solution and fixed with
70% ethanol for 30 min. Subsequently, the cells were again washed
three times with PBS and then labeled with Annexin V-FITC and
propidium iodide (Cell Signaling Technology, Inc., Boston, MA, USA)
following the manufacturer's instructions. Cells were subsequently
analyzed by flow cytometry (FACSCalibur) and CellQuest Pro software
(both from BD Biosciences, Franklin Lakes, NJ, USA) according to
the manufacturer's protocols. Experiments were repeated three
times.
Western blot analysis
In order to detect the protein expression levels of
MUC1, vascular endothelial growth factor (VEGF), VEGF-C, p-AKT and
p-extracellular signal-regulated kinase (p-ERK), western blot
analysis was performed according to standard procedures. Briefly,
cellular total protein was extracted from each sample using
radioimmunoprecipitation assay buffer (BioVision, Inc., Milpitas,
CA, USA). Protein concentration was determined by the BCA method,
then proteins (40 µg) were electrophoresed by 12% SDS-PAGE,
transferred onto a polyvinylidene fluoride membrane (EMD Millipore,
Billerica, MA, USA) and blocked in PBS solution supplemented with
5% fat-free milk for 1 h at 25°C. Subsequently, membranes were
blotted at 4°C overnight with the following primary antibodies:
MUC1 (14161; 1:1,000; Cell Signaling Technology, Inc., Danvers, MA,
USA), VEGF (SAB1402390; 1:1,000; Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany), VEGF-C (2445; 1:1,000), p-AKT (13038; 1:1,000)
and p-ERK (5683; 1:1,000) (all from Cell Signaling Technology,
Inc.), with GAPDH (166574; 1:2,000; Santa Cruz Biotechnology, Inc.,
Santa Cruz, CA, USA) serving as the internal control. Blots were
then incubated with horseradish peroxidase (HRP)-conjugated
secondary antibodies: Anti-rabbit (7074) and anti-mouse (14709)
(1:5,000; both from Cell Signaling Technology, Inc.) at 25°C for 2
h. Protein bands were visualized using a chemiluminescence
phototope-HRP kit (Pierce; Thermo Fisher Scientific, Inc.),
according to the manufacturer's protocol. The mean density of the
bands was quantified using an ImageJ v2.1.4.7 (National Institutes
of Health, Bethesda, MD, USA) after the film was scanned.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA from cultured cells was extracted using
TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.)
following the manufacturer's instructions. The first-strand cDNA
was generated from total RNA using the PrimeScript RT reagent kit
(Takara Bio, Inc., Otsu, Japan). Subsequently, qPCR was conducted
with the SYBR Premix Ex Taq II reagent (Takara Bio, Inc.). GAPDH
served as an internal control for detection of the mRNA expression
of MUC1. The sequences of the primers used were as follows: GAPDH
forward, 5′-GACTCATGACCACAGTCCATGC-3′ and reverse,
5′-AGAGGCAGGGATGATGTTCTG−3′ with a product size of 208 bp; MUC1
forward, 5′-CGCCGAAAGAACTACGGGCAGCTG-3′ and reverse,
5′-CAAGTTGGCAGAAGTGGCTGCCAC-3′ with a product size of 100 bp. The
thermal cycling conditions were: 60 sesc at 95°C, followed by 40
cycles of 95°C for 15 sec, 60°C for 15 sec and 72°C for 45 sec.
Relative quantification was performed using the 2−ΔΔCq
method (12). All qPCR reactions
were repeated three times.
Statistical analysis
Data are expressed as the mean ± standard deviation.
All statistical analyses were performed using SPSS version 16.0
statistical software (SPSS, Inc., Chicago, IL, USA). Student's
t-test was used to evaluate the differences between groups. A value
of P<0.05 was considered as an indicator of a statistically
significant difference.
Results
MUC1 expression in human NSCLC
cells
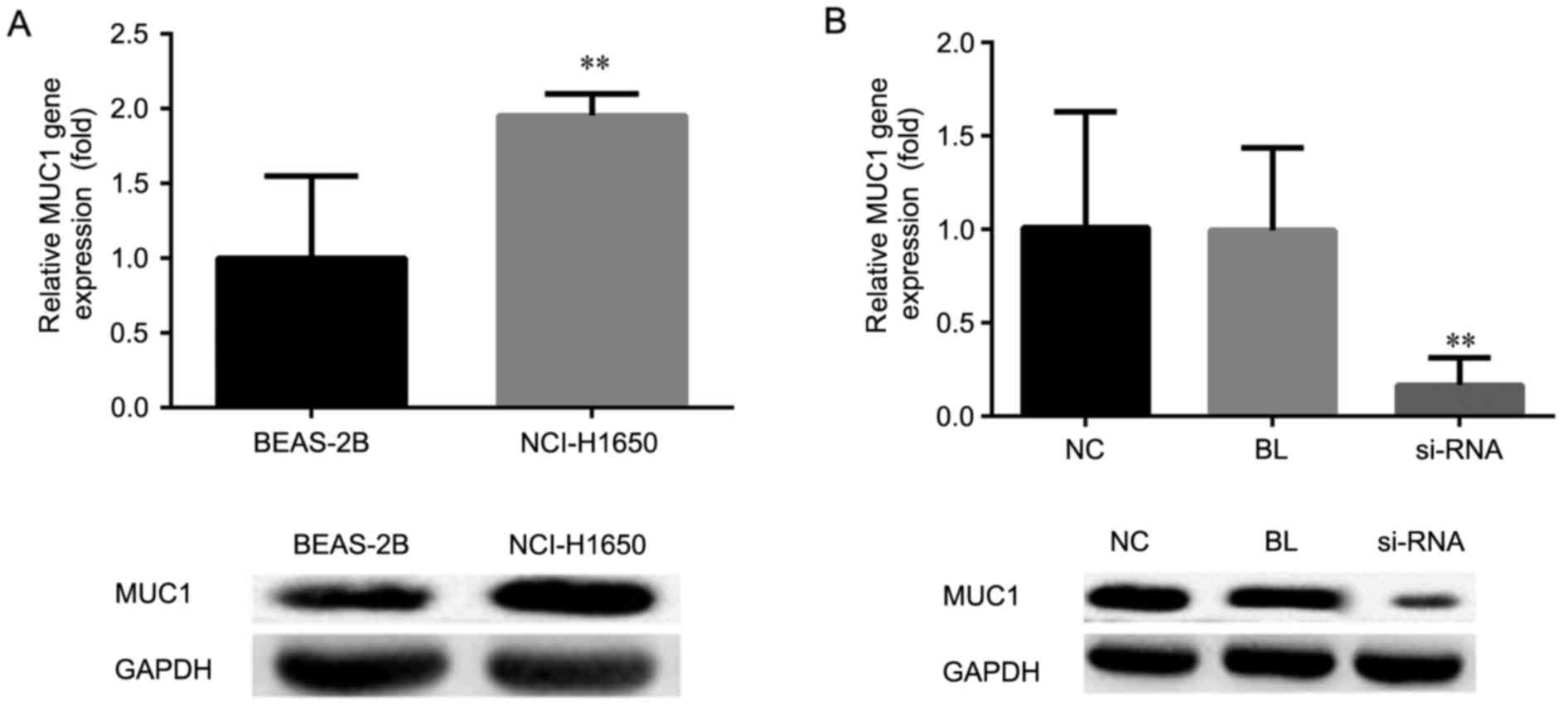
To investigate the expression of MUC1 in human NSCLC
cells, RT-qPCR and western blot analysis were performed,
respectively. As shown in Fig. 1A,
compared with the normal human lung epithelial cell line BEAS-2B,
the mRNA and protein expression levels of MUC1 in the human NSCLC
cell line NCI-H1650 were significantly increased (P<0.01).
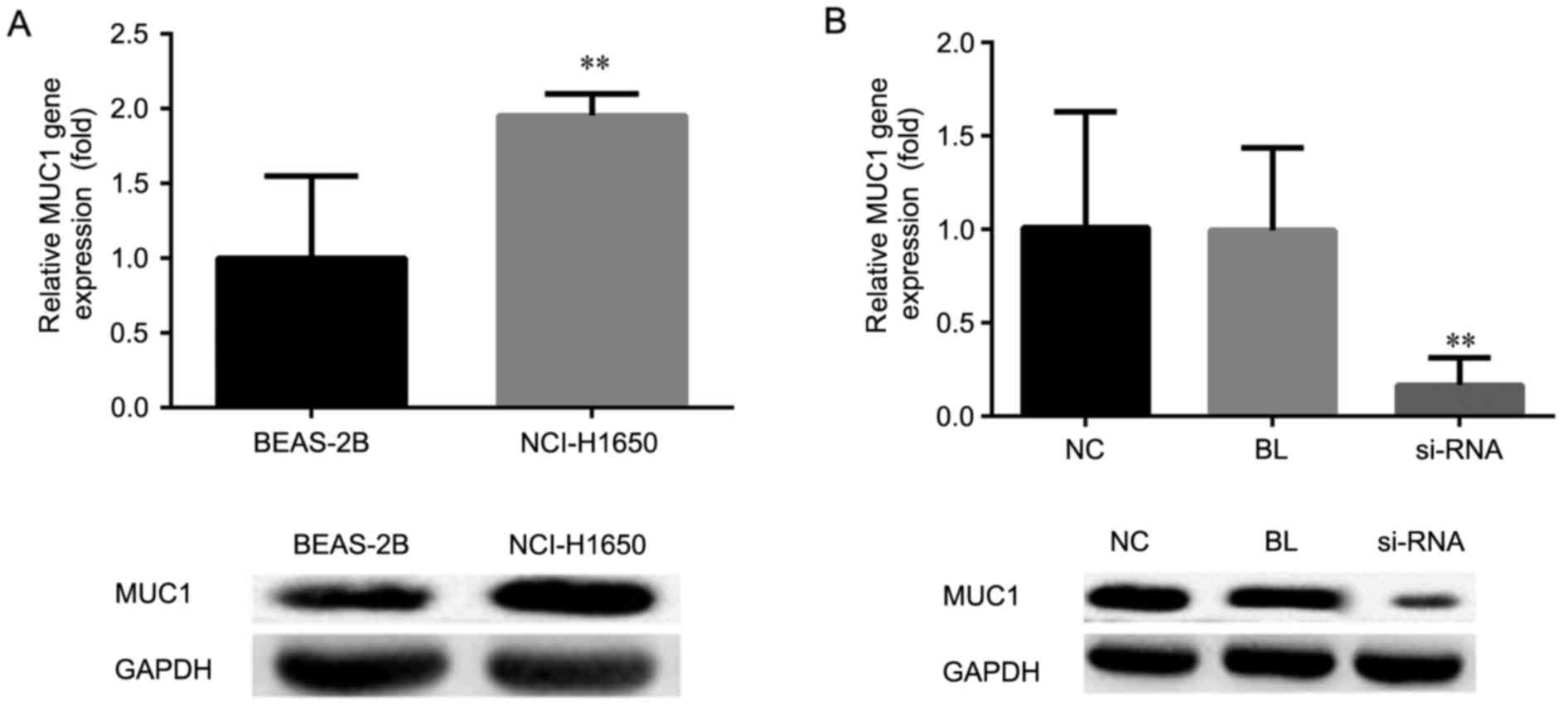 | Figure 1.mRNA and protein expression levels of
MUC1 were determined by reverse transcription-quantitative
polymerase chain reaction and western blot analysis, respectively,
in (A) NCI-H1650 and BEAS-2B cells, and (B) NCI-H1650 cells
transfected with MUC1-siRNA or control-siRNA, at 48 h after
transfection. All data are presented as the mean ± standard
deviation of three independent experiments. **P<0.01, vs. NC and
BL groups. MUC1, mucin 1; siRNA, small interfering RNA; NC,
negative control group (transfected with control-siRNA); BL, blank
control group (non-transfected); siRNA, MUC1-siRNA group
(transfected with MUC1-siRNA). |
In order to investigate the role of MUC1 in human
NSCLC, MUCI was silenced by using MUC1-siRNA. At 48 h after cell
transfection, the effective downregulation of the mRNA and protein
expression levels of MUC1 was confirmed by RT-qPCR and western blot
analysis, respectively, as compared with the non-transfected and
control-transfected cells (P<0.01; Fig. 1B).
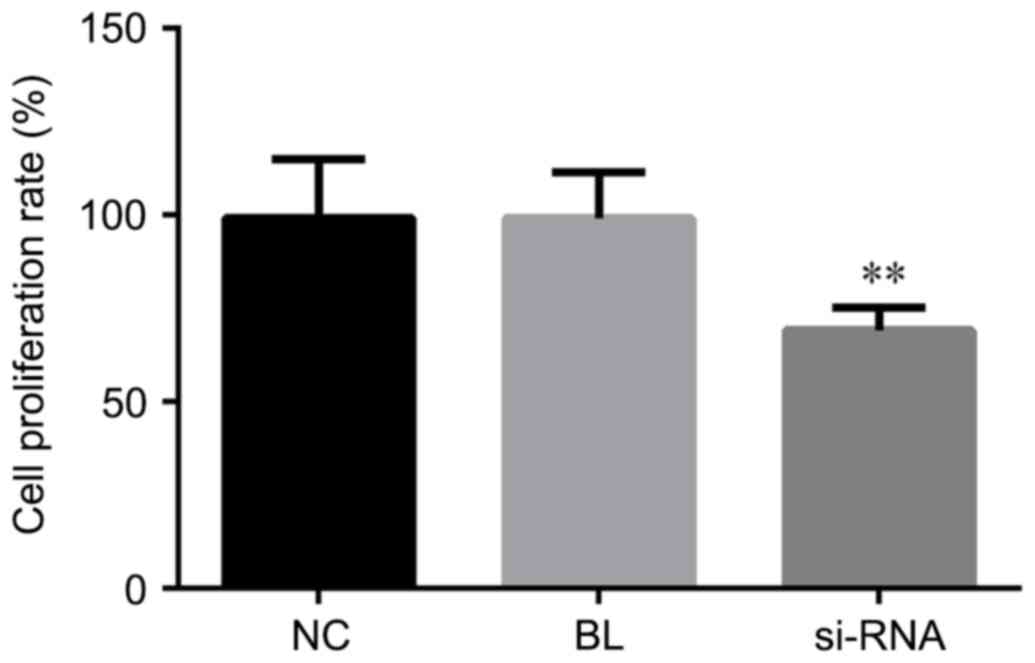
MUC1 downregulation inhibits cell
proliferation
CCK-8 assay was performed for cell proliferation
determination. To investigate the role of MUC1 in NSCLC cell
proliferation, MUC1-siRNA or control-siRNA were transfected into
NCI-H1650 cells. At 48 h after the cell transfection, the cell
proliferation ability was detected in the different groups. The
data suggested that, compared with the non-transfected and
control-transfected groups, the cell proliferation ability of cells
with MUC1 downregulation by siRNA transfection was significantly
declined (P<0.01; Fig. 2). Thus,
these results indicated that downregulation of MUC1 in NCI-H1650
cells inhibited cell proliferation.
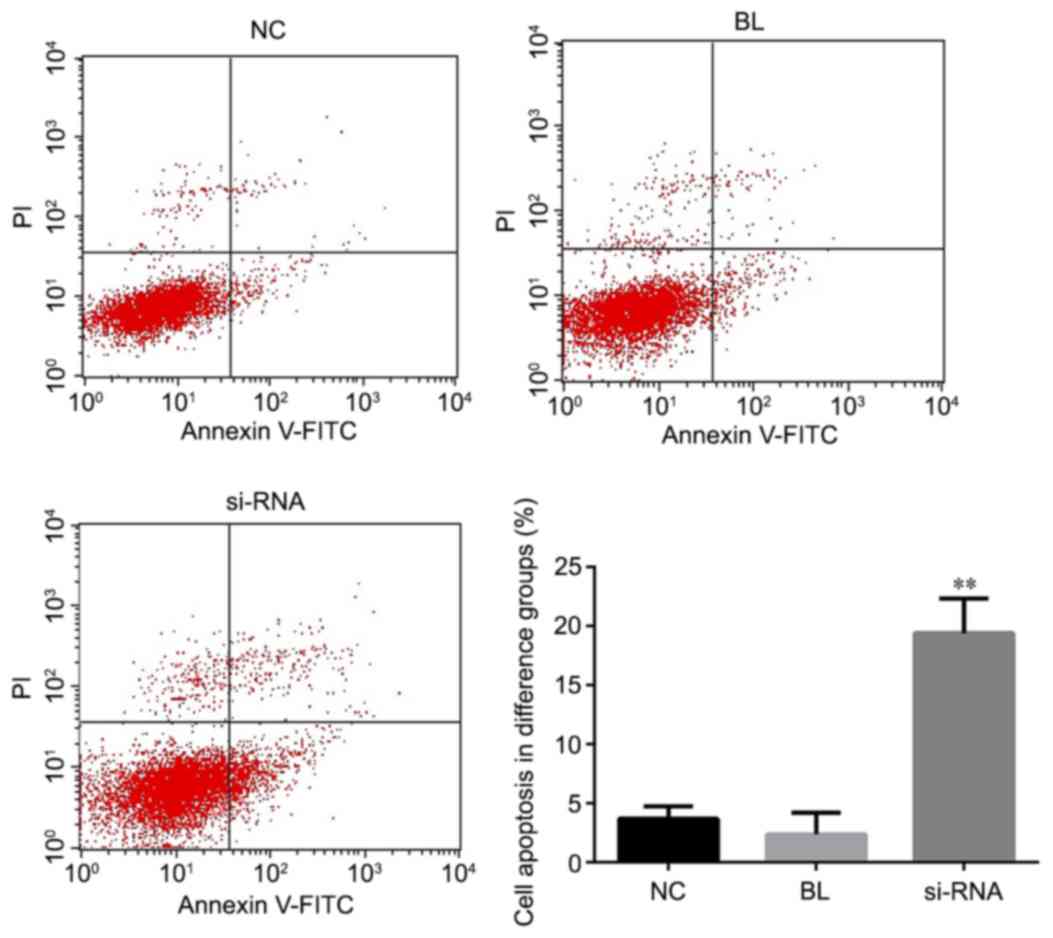
MUC1 downregulation promotes cell
apoptosis
To investigate the effect of MUC1 on cell apoptosis,
the apoptosis rate was measured by flow cytometry assay at 48 h
after NCI-H1650 cell transfected with MUC1-siRNA or control. As
shown in Fig. 3, the apoptosis rate
of the MUC1-siRNA-transfected NCI-H1650 cells was significantly
higher in comparison with that of cells transfected with
control-siRNA or non-transfected cells. These data indicated that
MUC1 downregulation was able to promote NCI-H1650 cell
apoptosis.
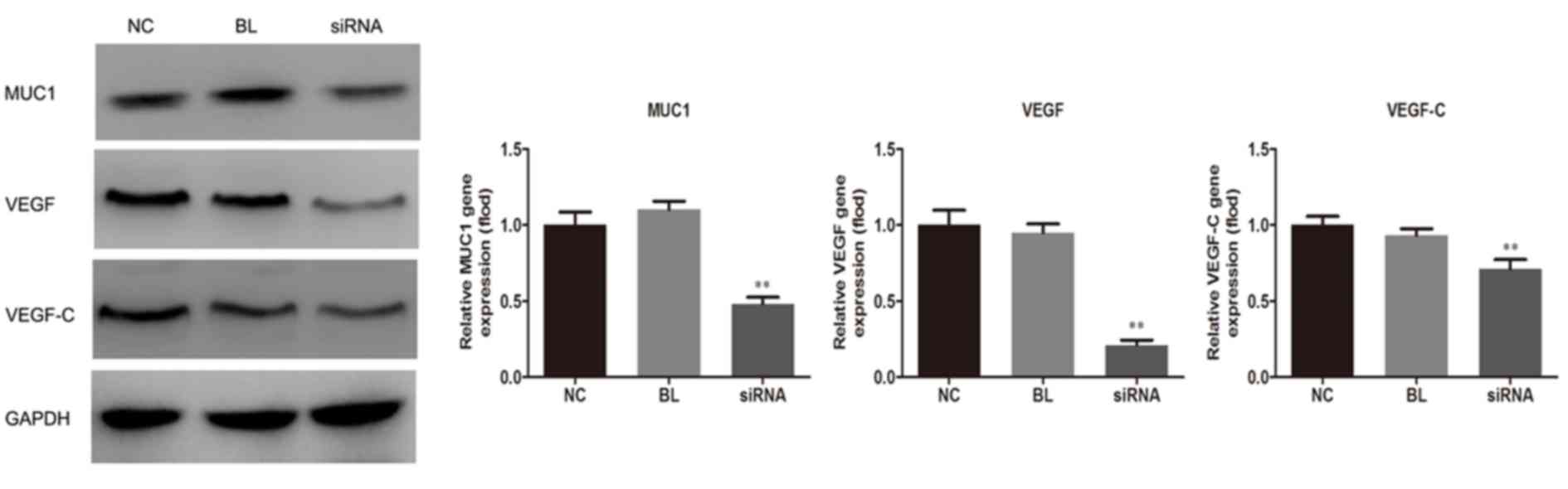
MUC1 downregulation inhibits VEGF and
VEGF-C expression levels
The current study next examined the effect of
suppressed expression of MUC1 on the expression of VEGF. As shown
in Fig. 4, the protein expression
levels of VEGF and VEGF-C were significantly reduced in NCI-H1650
cells in the siRNA group when compared with non-transfected and the
control-transfected groups (P<0.01), indicating the
anti-angiogenic effect of MUC1 downregulation.
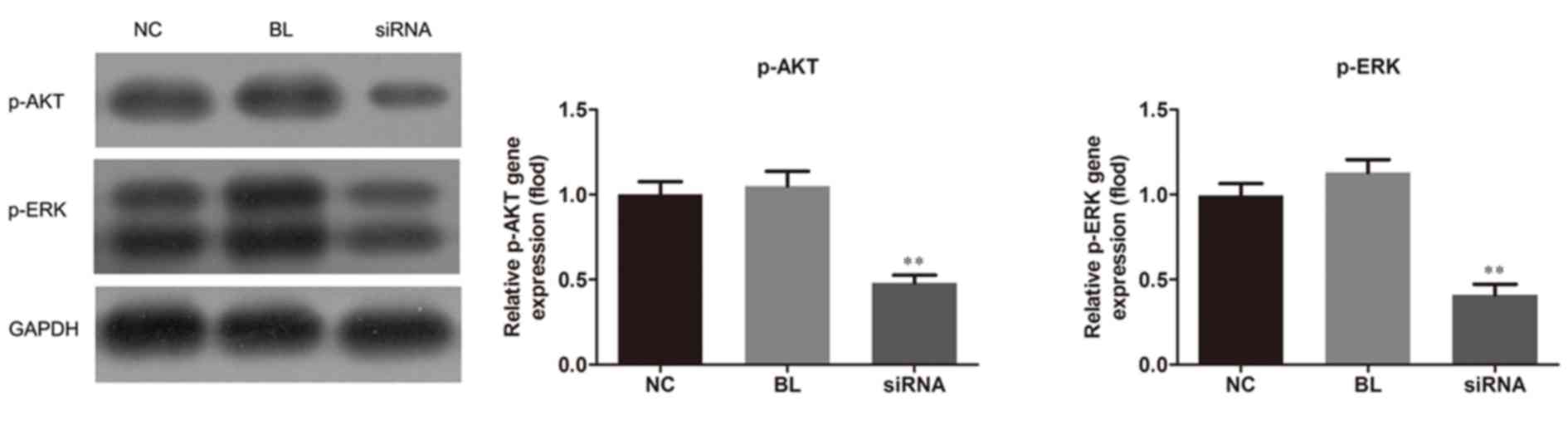
MUC1 downregulation affects AKT and
ERK activation
Since AKT and MAPK signaling pathways have been
strongly involved in tumor angiogenesis (13–15), the
present study also investigated the effect of MUC1 downregulation
on the activation of these two pathways. Western blot analysis
revealed that MUC1 siRNA transfection caused an evident decrease in
the phosphorylation of AKT and ERK, the protein expression levels
of p-AKT and p-ERK were reduced in the siRNA group when compared
with the non-transfected and control-transfected groups
(P<0.01), which is indicative of activation suppression of AKT
and ERK by MUC1 downregulation (Fig.
5).
Discussion
In the present study, it was demonstrated that MUC1
protein and mRNA levels were overexpressed in an NSCLC cell line.
The study further investigated the effect of downregulation of MUC1
by siRNA transfection on lung cancer progression using ab in
vitro cell line model. It was demonstrated that MUC1
downregulation in NCI-H1650 cells inhibited cell proliferation,
induced cell apoptosis, inhibited VEGF and VEGF-C production, and
suppressed the activation of AKT and ERK pathways. These results
strongly suggest that MUC1 downregulation inhibited NSCLC
progression.
MUC1 has been verified to be upregulated in a
variety of cancer types (16–18). The
high expression level of MUC1 in lung cancer has been closely
correlated with early recurrence, poor prognosis and high
metastatic potential (19). Ren
et al (20) suggested that
downregulation of MUC1 in lung cancer A549 cells increased their
sensitivity to genotoxic drugs in vitro and in vivo.
In addition, Gao et al (21)
reported that MUC1 knockdown suppresses lung cancer growth and
metastasis via inhibiting cell proliferation and inducing
apoptosis. According to these previous findings, the present study
observed that MUC1 downregulation inhibited the NSCLC NCI-H1650
cell proliferation and promoted cell apoptosis.
Angiogenesis is an important process required for
tumor genesis, growth, invasion and metastasis. VEGF, a member of
the platelet-derived growth factor family, serves critical roles in
inducing angiogenesis and vessel permeability (22). Furthermore, VEGF-C is a ligand of the
VEGF receptor, VEGF-R3, and is the only factor known to cause
lymphangiogenesis (23,24). In a previous study (25), the level of VEGF-C was suggested to
be associated with lymphangiogenesis and metastasis, as well as
with the patient prognosis in various types of cancer. In the
present study, it was observed that MUC1 downregulation inhibited
VEGF and VEGF-C production, indicating that MUC1 served important
roles in the regulation of VEGF and VEGF-C expression levels and in
lung cancer angiogenesis.
Various signaling pathways participate in cancer
development though the regulation of MUC1. For instance, MUC1 is
able to promote various cancer cell growth and survival via
activation of the β-catenin and nuclear factor-kB pathway (26). Additionally, AKT and MAPK pathways
have been reported to be strongly involved in tumor angiogenesis
(12–14), and thus analysis of these two
pathways was conducted in the present study. The data demonstrated
that downregulation of MUC1 inhibited the activation of AKT and ERK
pathways, indicating the participation of these two signaling
pathways in the biological function of MUC1.
In conclusion, the current study provided evidence
that MUC1 downregulation inhibits NSCLC cell proliferation,
facilitates NSCLC cell apoptosis, and suppresses VEGF and VEGF-C
production. The AKT and ERK signaling pathways were observed to
participate in the function of MUC1. These data, combined with
previous findings, indicate that MUC1 is involved in multiple
aspects of tumor progression, thus, representing a novel
therapeutic target for NSCLC treatment.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Graham MV, Purdy JA, Emami B, Harms W,
Bosch W, Lockett MA and Perez CA: Clinical dose-volume histogram
analysis for pneumonitis after 3D treatment for non-small cell lung
cancer (NSCLC). Int J Radiat Oncol Biol Phys. 45:323–329. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhou YY, Hu ZG, Zeng FJ and Han J:
Clinical profile of cyclooxygenase-2 inhibitors in treating
non-small cell lung cancer: A Meta-Analysis of nine randomized
clinical trials. PLoS One. 11:e01519392016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fenchel K, Sellmann L and Dempke WC:
Overall survival in non-small cell lung cancer-what is clinically
meaningful? Transl Lung Cancer Res. 5:115–119. 2016.PubMed/NCBI
|
|
5
|
Quéré G, Descourt R, Robinet G, Autret S,
Raguenes O, Fercot B, Alemany P, Uguen A, Férec C, Quintin-Roué I
and Le Gac G: Mutational status of synchronous and metachronous
tumor samples in patients with metastatic non-small-cell lung
cancer. BMC Cancer. 16:2102016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pope CA III, Burnett RT, Thun MJ, Calle
EE, Krewski D, Ito K and Thurston GD: Lung cancer, cardiopulmonary
mortality, and long-term exposure to fine particulate air
pollution. JAMA. 287:1132–1141. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kufe D, Inghirami G, Abe M, Hayes D,
Justi-Wheeler H and Schlom J: Differential reactivity of a novel
monoclonal antibody (DF3) with human malignant versus benign breast
tumors. Hybridoma. 3:223–232. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim YS, Gum J Jr and Brockhausen I: Mucin
glycoproteins in neoplasia. Glycoconj J. 13:693–707. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Al Masri A and Gendler SJ: Muc1 affects
c-Src signaling in PyV MT-induced mammary tumorigenesis. Oncogene.
24:5799–5808. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li Y, Liu D, Chen D, Kharbanda S and Kufe
D: Human DF3/MUC1 carcinoma-associated protein functions as an
oncogene. Oncogene. 22:6107–6110. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xu M and Wang X: Critical roles of mucin-1
in sensitivity of lung cancer cells to tumor necrosis factor-alpha
and dexamethasone. Cell Biol Toxicol. 33:361–371. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) methods. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cook KM and Figg WD: Angiogenesis
inhibitors: Current strategies and future prospects. CA Cancer J
Clin. 60:222–243. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Arsham AM, Plas DR, Thompson CB and Simon
MC: Akt and hypoxia-inducible factor-1 independently enhance tumor
growth and angiogenesis. Cancer Res. 64:3500–3507. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang Y, Jiang X, Qin X, Ye D, Yi Z, Liu
M, Bai O, Liu W, Xie X, Wang Z, et al: RKTG inhibits angiogenesis
by suppressing MAPK-mediated autocrine VEGF signaling and is
downregulated in clear-cell renal cell carcinoma. Oncogene.
29:5404–5415. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Khodarev N, Ahmad R, Rajabi H, Pitroda S,
Kufe T, McClary C, Joshi MD, MacDermed D, Weichselbaum R and Kufe
D: Cooperativity of the MUC1 oncoprotein and STAT1 pathway in poor
prognosis human breast cancer. Oncogene. 29:920–929. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Retterspitz MF, Monig SP, Schreckenberg S,
Schneider PM, Hölscher AH, Dienes HP and Baldus SE: Expression of
{beta}-catenin, MUC1 and c-met in diffuse-type gastric carcinomas:
Correlations with tumour progression and prognosis. Anticancer Res.
30:4635–4641. 2010.PubMed/NCBI
|
|
18
|
Kaira K, Murakami H, Serizawa M, Koh Y,
Abe M, Ohde Y, Takahashi T, Kondo H, Nakajima T and Yamamoto N:
MUC1 expression in thymic epithelial tumors: MUC1 may be useful
marker as differential diagnosis between type B3 thymoma and thymic
carcinoma. Virchows Arch. 458:615–620. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ohgami A, Tsuda T, Osaki T, Mitsudomi T,
Morimoto Y, Higashi T and Yasumoto K: MUC1 mucin mRNA expression in
stage I lung adenocarcinoma and its association with early
recurrence. Ann Thorac Surg. 67:810–814. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ren J, Agata N, Chen D, Li Y, Yu WH, Huang
L, Raina D, Chen W, Kharbanda S and Kufe D: Human MUC1
carcinoma-associated protein confers resistance to genotoxic
anticancer agents. Cancer Cell. 5:163–175. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gao J, McConnell MJ, Yu B, Li J, Balko JM,
Black EP, Johnson JO, Lloyd MC, Altiok S and Haura EB: MUC1 is a
downstream target of STAT3 and regulates lung cancer cell survival
and invasion. Int J Oncol. 35:337–345. 2009.PubMed/NCBI
|
|
22
|
Ferrara N: Molecular and biological
properties of vascular endothelial growth factor. J Mol Med (Berl).
77:527–543. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kajita T, Ohta Y, Kinura K, Tamura M,
Tanaka Y, Tsunezuka Y, Oda M, Sasaki T and Watanabe G: The
expression of vascular endothelial growth factor C and its
receptors in non-small cell lung cancer. Br J Cancer. 85:255–260.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Karkkainen MJ and Petrova TV: Vascular
endothelial growth factor receptors in the regulation of
angiogenesis and lymphangiogenesis. Oncogene. 19:5598–5605. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Roberts N, Kloos B, Cassella M,
Podgrabinska S, Persaud K, Wu Y, Pytowski B and Skobe M: Inhibition
of VEGFR-3 activation with the antagonistic antibody more potently
suppresses lymph node and distant metastases than inactivation of
VEGFR-2. Cancer. 66:2650–2657. 2006.
|
|
26
|
Kawano T, Ahmad R, Nogi H, Agata N,
Anderson K and Kufe D: MUC1 oncoprotein promotes growth and
survival of human multiple myeloma cells. Int J Oncol. 33:153–159.
2008.PubMed/NCBI
|