Introduction
Coronary atherosclerotic heart disease is a type of
severe disease which, due to the organic lumen stenosis or even
blockages of coronary arteries, often leads to a decrease in the
blood supply of coronary arteries, which can barely satisfy the
need of oxygen supply of the myocardium, further resulting in
ischemic injury of myocardium (1).
The occurrence rate of coronary heart disease is increasing with
the social and economic development in China, as well as an
improvement in people living conditions. Currently, percutaneous
coronary intervention is the most effective method for the
treatment of acute coronary syndromes. Previous research has
confirmed the insufficient effect of coronary arteriography in
identifying whether the coronary artery stenosis patients are
concomitant with the myocardial ischemia, especially for patients
with moderate coronary artery stenosis (2). Severe myocardial ischemia is believed
to be a key factor leading to the death of patients and poor
prognosis (3).
Fractional flow reserve (FFR) is the ratio of
maximum blood volume that can be achieved in the lesion vessels to
the normal reference value in the presence of coronary artery
stenosis (4). In the presence of
significant coronary artery stenosis, some of the kinetic energy of
the blood flow through the stenosis parts becomes converted into
thermal energy with a decrease in the pressure of blood flow, thus
leading to a great loss of energy. Therefore, we can indirectly
estimate the influence of stenosis on the myocardial perfusion by
measuring the changes in pressure (5). Since the FFR is free from the influence
of systemic hemodynamics and its clinical normal reference value is
already established, the FFR can be applied to better guide the
percutaneous coronary intervention to achieve better clinical
efficacy (6). In the present study,
the aim was to investigate the predictive value of FFR for the
prognosis of patients who received the percutaneous coronary
intervention due to acute coronary syndromes. Specific procedures
are reported below.
Materials and methods
Sample selection
We enrolled 120 patients who were admitted to the
hospital to receive coronary stenting for acute coronary syndromes
between May 2014 and June 2015. Before enrollment, 120 patients
were asked about their conditions in detail, including the past
medical history, age, height, weight, the history of smoking and
drinking, combined hypertension, diabetes, or chronic obstructive
pulmonary diseases, cardiac functions, previous physical condition.
The measurement of vital signs such as blood pressure, heart rate,
breathing rates were performed, the combination examination of
electrocardiogram and biochemical test for determining the indexes
of myocardial enzyme, troponin, B-type natriuretic peptide, blood
routine examination and blood clotting function was also conducted.
Fasting elbow venous blood was drawn for assaying blood glucose,
blood fat and hepatic as well as renal functions. All the patients
could afford the cost for the treatment of cardiac intervention by
implanting the stent and the cost for assaying the FFR, which was
performed before and after intervention therapy. Before enrollment,
all patients had signed the written informed consent of
intervention therapy and the written informed consent of
enrollment, and the present study was approved by the Ethics
Committee of the Tangshan Hospital.
The exclusion criteria were: i) patients who had
history of open coronary artery bypass surgery, ii) patients who
were in cardiac shock, iii) patients who were diagnosed with
myocardial diseases, iv) patients with ventricular hypertrophy, v)
patients with severe renal and hepatic dysfunction and vi) patients
who were allergic to the drugs used in the present study. The
enrolled patients were divided into two groups, the observation
group and the control group, according to the post-surgery levels
of FFR. Each group contained 60 patients and general
characteristics of both groups are shown in Table I, in which there was no statistically
significant difference in the comparison of sex, age, ratio of
hyperlipidemia, ratio of patients with a history of smoking and
drinking, height, weight, mean arterial pressure, heart rate,
stenosis degree of coronary artery, pre-surgery left ventricular
ejection fraction (LVEF) and pre-surgery FFR between the two groups
(P>0.05). Additionally, these patients were divided into two
groups, the occurrence group (n=45) and the non-occurrence group
(n=75), according to the occurrence of major adverse cardiovascular
events (MACE).
 | Table I.Comparison between the observation
group and the control group. |
Table I.
Comparison between the observation
group and the control group.
| Items | Observation
group | Control group | t-test or
χ2 | P-value |
|---|
| Sex
(male/female) | 36/24 | 35/25 | 0.034 | 0.853 |
| Age (years) | 62.1±1.8 | 62.3±1.8 | 0.609 | 0.544 |
| Ratio of
hyperlipidemia (%) | 40 (66.7%) | 41 (68.3%) | 0.038 | 0.845 |
| Ratio of patients
with a history of smoking and drinking (%) | 26 (43.3%) | 27 (45.0%) | 0.034 | 0.854 |
| Height (cm) | 163.2±2.1 | 163.3±2.1 | 0.261 | 0.795 |
| Weight (kg) | 68.5±1.4 | 68.6±1.5 | 0.378 | 0.706 |
| Mean arterial
pressure (mmHg) | 125.6±2.5 | 126.1±2.6 | 1.074 | 0.285 |
| Heart rate
(beats/min) | 98.5±2.3 | 98.6±2.4 | 0.233 | 0.816 |
| Stenosis degree of
coronary artery (%) | 65.3±2.9 | 65.4±3.0 | 0.186 | 0.853 |
| Pre-surgery LVEF
(%) | 43.2±1.8 | 43.3±1.8 | 0.304 | 0.761 |
| Pre-surgery FFR
(%) | 0.72±0.05 | 0.73±0.06 | 0.992 | 0.323 |
Treatments
For all enrolled patients, we performed intensive
care, which closely monitored their conditions by a 24-h ECG,
ensured bed rest, discharges of urinary and fecal matter in bed and
a light diet. In addition, we administered sedation to dull the
pain and nitroglycerine to dilate their vessels, aspirin for
anti-platelet therapy, low-molecular-weight heparins by
subcutaneous injection for anti-coagulation therapy and a
combination of angiotensin and β-receptor blocker for regulating
the pressure. These patients were divided into two groups according
to the pre-surgery levels of FFR, i.e., the control group (FFR
>0.80) and the observation group (FFR ≤0.80). For the control
group, conservative treatment by a single administration of drugs
was applied, while for the observation group, stenting for
revascularization was performed in addition to the relevant
conservative treatment.
Observation indexes
All patients were followed up for 2 years either by
telephone or through outpatient service. During the follow-up
period, we compared the occurrence rates of MACE in 30 days after
surgery and the Kaplan-Meier survival analysis curves between the
observation group and the control group, as well as the general
materials and FFR before and after surgery between the occurrence
group and the non-occurrence group. We also performed multi-factor
logistic regression analysis for the occurrence of MACE 30 days
after surgery, and analyzed the predictive value of post-surgery
FFR for the occurrence of MACE in 1 year.
Assessment methods
i) Two dimensional ultrasonography was applied in
the ECG to assay the relevant data of the enrolled patients heart,
including the left arterial diameter and LEVF, and used the pulsed
wave Doppler to investigate the blood flow and its orientation in
the bicuspid valve, the tricuspid valve, aortic valve and the
pulmonary valve; ii) coronary angiography, coronary angiography was
performed using the standard Judkins method for all the enrolled
patients, i.e., patients that had signed the written informed
consent before surgery, and the physicians selected the radial
artery in order to perform the puncture when patients were under
local anesthesia. Thereafter, according to the results of coronary
angiography, patients whose one-vessel stenosis degree was over 50%
would be diagnosed as coronary heart disease; while the coronary
artery TIMI blood flow refers to the condition of blood flow in the
infarction-related sites during the onset of acute myocardial
infarction, which was divided into five degrees (0 to IV), and a
lower degree represented more severe infarction and iii) measuring
the FFR: this process was performed using the pressure sensor, in
which the FFR value was set to 1.00 when the changes of aortic
pressure were paralleled with the pressure curve of the pressure
guidewire. Based on the settings, we investigated the variation of
FFRs before and after treatment and the minimum and mean of the
FFRs, in whom the reference value of FFR was set as 0.80. For
patients with the FFR higher than 0.80, a conservative therapy by
administration of drugs could be simply applied. The FFR assay and
the coronary angiography were performed strictly under the
instructions of qualified clinical physicians at this hospital with
the work experience longer than 10 years.
Statistical analysis
SPSS 13.0 software (SPSS, Inc., Chicago, IL, USA)
was applied to the statistical process. Nonparametric test was
performed for the non-normally distributed data. For normally
distributed data, a t-test was performed for intergroup comparison
of the mean. Measurement data were presented as mean ± standard
variation, and the ROC curve was drawn for assessing the predictive
value of FFR after surgery for the occurrence of MACE in 1 year.
The χ2 test was applied to the intergroup comparison of
rates, and the log-rank test was performed for statistics of
intergroup data and the survival curve was accordingly established.
A multi-factor logistic regression analysis was carried out for
analyzing the relevant influential factors. P<0.05 suggested
that the difference was statistically significant.
Results
Comparison of MACE occurrence in 30
days post-surgery between the observation group and the control
group
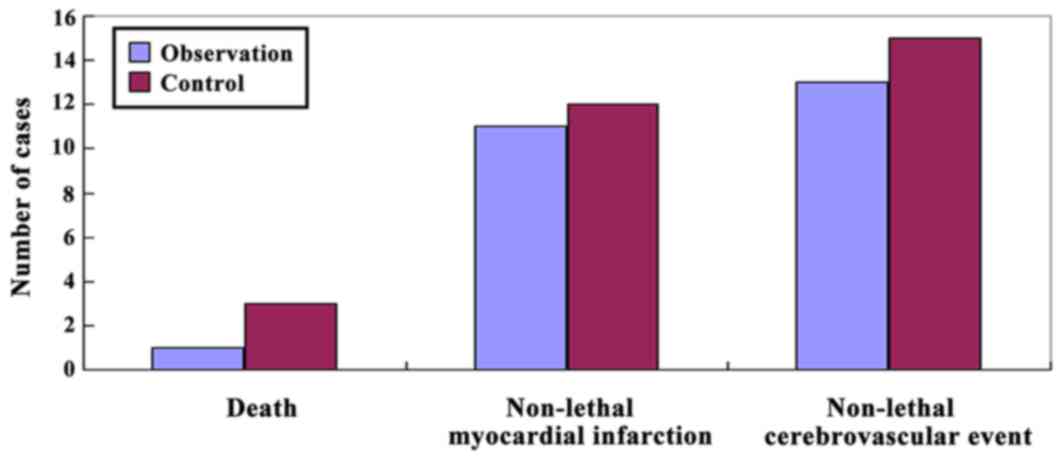
For the MACE occurrence in 30 days post-surgery of
the observation group, there was 1 death (1.7%), 11 cases with
non-lethal myocardial infarction (18.3%) and 13 cases with
non-lethal cerebrovascular event (21.7%). While for that of the
control group, there were 3 deaths (5.0%), 12 cases with non-lethal
myocardial infarction (20.0%) and 15 cases with non-lethal
cerebrovascular event (25.0%) (Fig.
1). There were no statistically significant differences in the
comparison of the MACE occurrence between the groups.
Analysis of the Kaplan-Meier survival
curves of the observation group and the control group
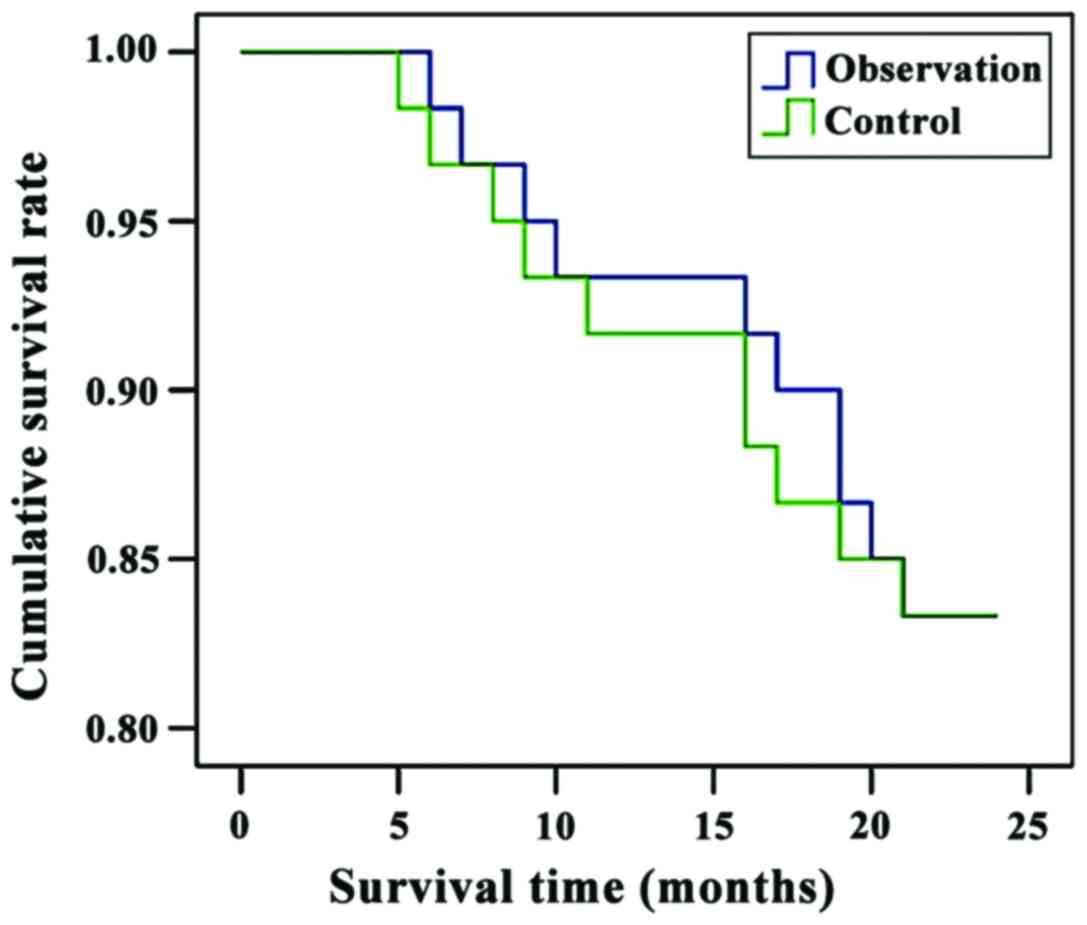
For the observation group, the 1-year survival cases
were 56 with a survival rate of 93.3%, and 2-year survival cases
were 50 with a survival rate of 83.3%. For the control group, the
1-year and 2-year survival cases were, respectively, 55 and 49 (the
survival rates were 91.7 and 81.7%) (Fig. 2).
General comparison between the
occurrence group and the non-occurrence group
There was no statistically significant difference in
comparison of sex, age, height and weight between the occurrence
group and the non-occurrence group (P>0.05). Both of the
occurrence rate of hyperlipidemia and ratio of patients with a
history of smoking and drinking in the occurrence group were
significantly higher than those in the non-occurrence group
(P<0.05); the mean arterial pressure in the occurrence group was
significantly higher than that in the non-occurrence group
(P<0.05); the heart rate in the occurrence group is
significantly faster than that in the non-occurrence group
(P<0.05); the stenosis degree in the occurrence group was
significantly higher than that in the non-occurrence group
(P<0.05); the LVEF before surgery in the occurrence group was
significantly lower than that in the non-occurrence group
(P<0.05) (Table II).
 | Table II.Results between the occurrence group
and the non-occurrence group. |
Table II.
Results between the occurrence group
and the non-occurrence group.
| Items | Occurrence group | Non-occurrence
group | t-test or
χ2 | P-value |
|---|
| Sex
(male/female) | 25/20 | 40/35 | 0.056 | 0.813 |
| Age (years) | 62.6±1.9 | 62.5±1.9 | 0.279 | 0.781 |
| Ratio of
hyperlipidemia (%) | 41 (91.1%) | 51 (68.0%) | 7.155 | 0.007 |
| Ratio of patients
with a history of smoking and drinking (%) | 40 (88.9%) | 50 (66.7%) | 7.407 | 0.006 |
| Height (cm) | 163.6±2.1 | 163.6±2.0 | 0.000 | 1.000 |
| Weight (kg) | 68.6±1.4 | 68.5±1.5 | 0.362 | 0.718 |
| Mean arterial
pressure (mmHg) | 141.6±5.1 | 126.3±2.5 | 21.988 | <0.001 |
| Heart rate
(beats/min) | 108.7±3.3 | 93.5±2.3 | 29.678 | <0.001 |
| Stenosis degree of
coronary artery (%) | 75.8±2.8 | 63.2±3.1 | 22.336 | <0.001 |
| Pre-surgery LVEF
(%) | 41.3±1.7 | 46.8±1.9 | 15.956 | <0.001 |
Comparison of FFRs before and after
treatment between the occurrence group and the non-occurrence
group
There were no statistically significant differences
in the comparison of FFRs before the treatment between the
occurrence group and the non-occurrence group (P>0.05). After
treatment, the FFR of the the occurrence group was significantly
lower than that of the non-occurrence group (P<0.05) (Table III).
 | Table III.Comparison of FFRs before and after
treatment between the occurrence group and the non-occurrence group
(mean ± standard variation). |
Table III.
Comparison of FFRs before and after
treatment between the occurrence group and the non-occurrence group
(mean ± standard variation).
| Items | Before treatment | After treatment |
|---|
| Occurrence group | 0.75±0.11 | 0.83±0.02 |
| Non-occurrence
group | 0.75±0.10 | 0.93±0.05 |
| t-test | 0.000 | 12.799 |
| P-value | 1.000 | <0.001 |
Multi-factor logistic regression
analysis for the occurrence of MACEs in 30 days after surgery
The multi-factor logistic regression analysis was
performed with the MACE in 30 days post-surgery as the dependent
variable, which indicates that the increased blood fat, a history
of smoking and drinking, augmented mean arterial pressure,
accelerated heart rate, severe coronary artery stenosis and the
remarkably decreased LVEF were all identified as independent risk
factors leading to MACE (Table
IV).
 | Table IV.Multi-factor logistic regression
analysis for the occurrence of MACE 30 days after surgery. |
Table IV.
Multi-factor logistic regression
analysis for the occurrence of MACE 30 days after surgery.
| Items | B | s | OR | P-value |
|---|
| Sex
(male/female) | 0.358 | 0.628 | 2.336 | 0.219 |
| Age (years) | −421 | 0.602 | 0.658 | 0.459 |
| Ratio of
hyperlipidemia (%) | 1.653 | 0.853 | 0.206 | 0.031 |
| Ratio of patients
with a history of smoking and drinking (%) | 1.596 | 0.758 | 0.196 | 0.030 |
| Height (cm) | 0.325 | 0.599 | 2.321 | 0.218 |
| Weight (kg) | 0.336 | 0.621 | 2.336 | 0.231 |
| Mean arterial
pressure (mmHg) | 1.360 | 0.862 | 0.235 | 0.042 |
| Heart rate
(beats/min) | 1.625 | 0.758 | 0.125 | 0.006 |
| Stenosis degree of
coronary artery (%) | 1.456 | 0.869 | 0.214 | 0.011 |
| Pre-surgery LVEF
(%) | 1.038 | 0.678 | 0.209 | 0.036 |
Analysis of predict value of the
post-surgery FFR for the MACE occurrence in 1 year
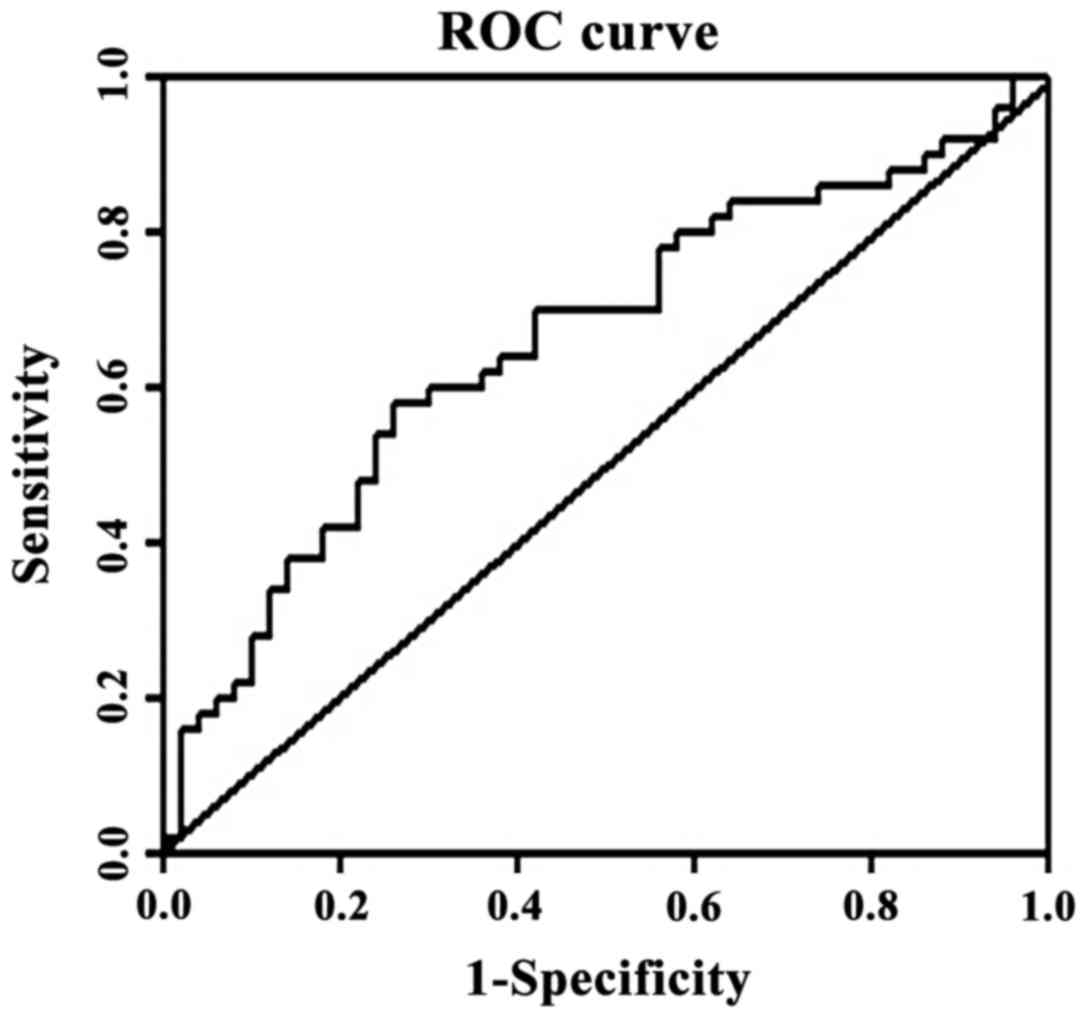
In the present study, we established the ROC curve
with the post-surgery FFR as the measurement vector, the occurrence
of MACE as the state variable and the reference for grouping and 1
as the defined value. The AUC of ROC was 0.716, in which P-value
was 0.005, indicating that the sum of specificity and sensitivity
of treatment reached its peak when the post-surgery FFR was 0.875,
the calculated sensitivity was 82.4%, and the specificity was 50.8%
(Fig. 3).
Discussion
Previously, coronary angiography was frequently
applied to investigate the stenosis of coronary artery lesion and
the efficiency in perioperative assessment of the efficacy for
patients with acute coronary syndromes, failing to effectively
evaluate the condition of blood flow in the distal parts of the
stenosis vessels, causing less accurate understanding of the
patients conditions before surgery (7), or even unnecessary stenting procedures
for patients with no severe myocardial ischemic coronary diseases
(8). These actions results in a
great loss of medical resources, and may even affect the prognosis
of patients. FFR, which is mainly applicable to those with stenosis
lesion of coronary artery (9),
refers to a ratio of the maximum blood volume that can be achieved
in the lesion vessels to the maximum value in the same site under
the normal physiological conditions (10). FFR is free from the variations of
heart rate, blood pressure, and myocardial contractility. In
clinical practice, the normal reference value of FFR is set to 1.0
(11). Moreover, FFR is apt to
operate and can be repeatedly measured. Thus, it can serve as the
functional index for assessing the coronary artery stenosis, which
has been widely used by physicians of the cardiology department for
decision of intervention therapy (12).
Previous studies have confirmed that FFR of 0.8, can
serve as a clinical reference value for the decision to perform the
intervention therapy of stenting. In the present study, we divided
the enrolled patients into the observation group (FFR >0.8) and
the control group (FFR ≤0.8) and set 0.8 as the clinical reference
value for the decision to perform the stenting procedures. The
results showed that there was no statistically significant
difference in the comparison of MACE in 30 days after surgery
between the two groups, such as the ratio of deaths, non-lethal
myocardial infarction cases and non-lethal cerebrovascular cases.
The 1-year and 2-year survival rates in both groups were higher
than 90 and 80%, respectively, which was in accordance with the
results of studies conducted by Fröhlich et al and Varho
et al (13,14). Such results indicate that determining
the implementation of coronary artery stenting by the FFR value can
achieve better efficacy in guiding clinical practice, which can
effectively reduce the ratio of less considered stenting
procedures, facilitate the functional revascularization, and
minimize the surgical risk and the adverse reaction due to the
application of a contrast agent (15). Despite the confirmed positive
reference value of FFR in the selection of therapeutic strategies
of coronary artery stenting, some patients that received the
treatment strictly under the guidance of FFR still suffered the
MACE after surgery, such as death, non-lethal myocardial infarction
and non-lethal cerebrovascular events. In the present study, we
mainly investigated MACE in 30 days after surgery, and found that
there were 45 cases with MACE in varying degrees, especially the
non-lethal myocardial infarction cases and cases with non-lethal
cerebrovascular events (16). Both
the occurrence rate of hyperlipidemia and ratio of patients with a
history of smoking and drinking in the occurrence group were
significantly higher than those in the non-occurrence group. The
mean arterial pressure in the occurrence group was significantly
higher than that in the non-occurrence group. The heart rate in the
occurrence group is significantly faster than that in the
non-occurrence group and the stenosis degree in the occurrence
group was significantly higher than that in the non-occurrence
group. The LVEF before surgery in the occurrence group was
significantly lower than that in the non-occurrence group. These
results indicate that patients with increased blood fat, a history
of smoking and drinking, augmented mean arterial pressure,
accelerated heart rate, severe coronary artery stenosis and the
remarkably decreased LVEF were more susceptible to MACE in 30 days
after surgery, which is coincident with the results of Park et
al (17). Through multi-factor
logistic regression analysis for the occurrence of MACE in 30 days
after surgery, we found that increased blood fat, a history of
smoking and drinking, augmented mean arterial pressure, accelerated
heart rate, severe coronary artery stenosis and remarkably
decreased LVEF were all independent risk factors leading to the
MACE in 30 days after surgery (18).
It was further confirmed in the present study that patients with
the above risk factors, though being treated strictly under the
guidance of FFR, would have the significantly increased ratio of
MACE in 30 days after surgery.
In addition, the FFR can serve to assess the
efficacy immediately after the stenting procedures in clinical
practice, especially the target-vessel revascularization after
surgery. Previous studies have confirmed that the FFR less than 0.9
(19), which indicates insufficient
dilation of stent or poor target-vessel revascularization, but the
FFR higher than 0.90 suggests the desired clinical efficacy and
better prognosis of patients. In the present study, for
investigating the MACE occurrence in 30 days after surgery, we
compared the FFRs before treatment and found that there was no
statistically significant difference in the comparison of FFR
before treatment between the occurrence group and the
non-occurrence group and that the FFRs were all significantly lower
than the normal range. After treatment, the FFR in the occurrence
group was lower than that in the non-occurrence group (the average
FFR was higher than 0.90), which is coincident with the result of
Corban et al (20). For
further investigation of the predictive value of the post-surgery
FFR for the occurrence of MACE 1 year after surgery, we established
the ROC curve with the post-surgery FFR as the measurement vector,
and the occurrence of MACEs as state variable and the reference for
grouping and 1 as the defined value. The AUC of ROC was 0.716, in
which P-value was 0.005, which indicates that the sum of
specificity and sensitivity of treatment reached its peak when the
post-surgery FFR was 0.875, and the calculated sensitivity was
82.4%, and the specificity was 50.8%. Thus, we believe that the
MACE in 30 days after surgery would be significantly decreased and
increased, respectively, when the post-surgery FFR reached 0.875,
and the prognosis of patients would be significantly improved when
the post-surgery FFR surpassed 0.875.
In conclusion, the measurement of FFR after
percutaneous coronary intervention could not only effectively
evaluate the target vessel revascularization, but also predict the
occurrence of major adverse myocardial events 1 year after surgery,
which could serve as guidance for clinical treatment.
Acknowledgements
The present study was funded by the Hebei Province
Planning Commission (no. 20150944).
References
|
1
|
Park SH, Jeon KH, Lee JM, Nam CW, Doh JH,
Lee BK, Rha SW, Yoo KD, Jung KT, Cho YS, et al: Long-term clinical
outcomes of fractional flow reserve-guided versus routine
drug-eluting stent implantation in patients with intermediate
coronary stenosis: five-year clinical outcomes of DEFER-DES trial.
Circ Cardiovasc Interv. 8:e0024422015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Maehara A, Ben-Yehuda O, Ali Z, Wijns W,
Bezerra HG, Shite J, Généreux P, Nichols M, Jenkins P,
Witzenbichler B, et al: Comparison of stent expansion guided by
optical coherence tomography versus intravascular ultrasound: the
ILUMIEN II study (observational study of optical coherence
tomography [OCT] in patients undergoing fractional flow reserve
[FFR] and percutaneous coronary intervention). JACC Cardiovasc
Interv. 8:1704–1714. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vos NS, van der Schaaf RJ, Amoroso G,
Herrman JP, Patterson MS, Slagboom T and Vink MA: REVascularization
with paclitaxEL-coated balloon angioplasty versus drug-eluting
stenting in acute myocardial infarcTION-a randomized controlled
trial: rationale and design of the REVELATION trial. Catheter
Cardiovasc Interv. 87:1213–1221. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cho S, Kim JS, Ha J, Shin DH, Kim BK, Ko
YG, Choi D, Jang Y and Hong MK: Three-dimensional optical coherence
tomographic analysis of eccentric morphology of the jailed
side-branch ostium in coronary bifurcation lesions. Can J Cardiol.
32:234–239. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Doh JH, Nam CW, Koo BK, Park SH, Lee JH,
Han JK, Yang HM, Lim HS, Yoon MH, Cho YK, et al: Long-term
patient-related and lesion-related outcomes after real-world
fractional flow reserve use. J Invasive Cardiol. 27:410–415.
2015.PubMed/NCBI
|
|
6
|
De Maria GL, Cuculi F, Patel N, Dawkins S,
Fahrni G, Kassimis G, Choudhury RP, Forfar JC, Prendergast BD,
Channon KM, et al: How does coronary stent implantation impact on
the status of the microcirculation during primary percutaneous
coronary intervention in patients with ST-elevation myocardial
infarction? Eur Heart J. 36:1–3177. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wijns W, Shite J, Jones MR, Lee SW, Price
MJ, Fabbiocchi F, Barbato E, Akasaka T, Bezerra H and Holmes D:
Optical coherence tomography imaging during percutaneous coronary
intervention impacts physician decision-making: ILUMIEN I study.
Eur Heart J. 36:3346–3355. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kimura Y, Tanaka N, Okura H, Yoshida K,
Akabane M, Takayama T, Hirayama A, Tada T, Kimura T, Takano H, et
al: Characterization of real-world patients with low fractional
flow reserve immediately after drug-eluting stents implantation.
Cardiovasc Interv Ther. 31:29–37. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Reith S, Battermann S, Hellmich M, Marx N
and Burgmaier M: Correlation between OCT-derived intrastent
dimensions and fractional flow reserve measurements after coronary
stent implantation and impact on clinical outcome. J Invasive
Cardiol. 27:222–228. 2015.PubMed/NCBI
|
|
10
|
Courand PY, Dementhon J, Rioufol G and
Finet G: Very late neoatherosclerotic plaque rupture in
drug-eluting stent restenosis. J Cardiovasc Med (Hagerstown). 16
Suppl 1:27–28. 2015. View Article : Google Scholar
|
|
11
|
Ito T, Tani T, Fujita H and Ohte N:
Relationship between fractional flow reserve and residual plaque
volume and clinical outcomes after optimal drug-eluting stent
implantation: insight from intravascular ultrasound volumetric
analysis. Int J Cardiol. 176:399–404. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McNeice AH, McAleavey NM and Menown IB:
Advances in clinical cardiology. Adv Ther. 31:837–860. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fröhlich GM, Redwood S, Rakhit R,
MacCarthy PA, Lim P, Crake T, White SK, Knight CJ, Kustosz C, Knapp
G, et al: Long-term survival in patients undergoing percutaneous
interventions with or without intracoronary pressure wire guidance
or intracoronary ultrasonographic imaging: a large cohort study.
JAMA Intern Med. 174:1360–1366. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Varho V, Karjalainen PP, Ylitalo A,
Airaksinen JK, Mikkelsson J, Sia J, Pietilä M and Kiviniemi TO:
Transthoracic echocardiography for non-invasive assessment of
coronary vasodilator function after DES implantation. Eur Heart J
Cardiovasc Imaging. 15:1029–1034. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dörr R, Stumpf J, Dalibor J, Simonis G and
Spitzer SG: Percutaneous coronary intervention versus bypass
surgery in patients with diabetes and multivessel coronary disease.
Coronary revascularization after FREEDOM. Herz. 39:331–342.
2014.(In German).
|
|
16
|
Onuma Y, Dudek D, Thuesen L, Webster M,
Nieman K, Garcia-Garcia HM, Ormiston JA and Serruys PW: Five-year
clinical and functional multislice computed tomography angiographic
results after coronary implantation of the fully resorbable
polymeric everolimus-eluting scaffold in patients with de novo
coronary artery disease: the ABSORB cohort a trial. JACC Cardiovasc
Interv. 6:999–1009. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park SJ, Ahn JM, Park GM, Cho YR, Lee JY,
Kim WJ, Han S, Kang SJ, Park DW, Lee SW, et al: Trends in the
outcomes of percutaneous coronary intervention with the routine
incorporation of fractional flow reserve in real practice. Eur
Heart J. 34:3353–3361. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rao VU, Pavlov A, Klearman M, Musselman D,
Giles JT, Bathon JM, Sattar N and Lee JS: An evaluation of risk
factors for major adverse cardiovascular events during tocilizumab
therapy. Arthritis Rheumatol. 67:372–380. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsuo A, Fujita H, Tanigaki T, Shimonaga
T, Ueoka A, Tsubakimoto Y, Sakatani T, Kimura S, Inoue K and
Kitamura M: Clinical implications of coronary pressure measurement
after stent implantation. Cardiovasc Interv Ther. 28:170–177. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Corban MT, Eshtehardi P and Samady H:
Fractional flow reserve for the assessment of complex multivessel
disease in a patient after hybrid coronary revascularization.
Catheter Cardiovasc Interv. 81:1169–1173. 2013. View Article : Google Scholar : PubMed/NCBI
|