Introduction
‘Kissing’ aneurysms were initially described and
defined by Jefferson (1). They are
special types of multiple aneurysms defined as two adjacent
aneurysms arising from identical or different arteries with
separate origins and partially adherent walls (1). Cases of ‘Kissing’ aneurysms make up
<1% of all intracranial aneurysms (2). Due to ‘kissing’ aneurysms occurring in
arteries sharing adherent walls, they may be misdiagnosed as a
single aneurysm, resulting in patients undergoing the wrong
treatment, which may lead to the subsequent rupture of the
aneurysms (2). Fortunately, 96.8% of
reported cases had a favourable prognosis with only one case having
an unknown prognosis (Table I).
‘Kissing’ aneurysms are commonly located in the proximal of the
internal carotid artery following fenestration deformity (3). Notably, ‘kissing’ aneurysms of
bilateral distal anterior cerebral arteries (DACAs) are rare and,
to date, only 3 cases of DACA ‘kissing’ aneurysms have been
reported prior to the current case (2,4,5).
 | Table I.Characteristics of ‘kissing’ aneurysms
reported before May 2015. |
Table I.
Characteristics of ‘kissing’ aneurysms
reported before May 2015.
| Author, year | Cases | Sex/age (years) | Location | Hunt-Hess grade | Treatment method | Prognosis | (Refs.) |
|---|
| Jefferson, 1978 | 5 | F/46 | Upper segment of the
carotid artery bed | II | Clipping | Good | (1) |
| Yaşargil and Carter,
1974 | 2 | F/36 | Bilateral corpus
arteries | III | Clipping | Good | (4) |
| Sakakibara et
al, 2006 | 1 | F/47 | Upper segment of the
carotid artery bed | Unknown | Clipping | Good | (27) |
| Takahashi et
al, 2011 | 1 | F/62 | Upper segment of the
carotid artery bed | II | Embolization | Good | (24) |
| Guo et al,
2012 | 1 | F/50 | Upper segment of the
carotid artery bed | II | Clipping | Good | (9) |
| Matsumoto et
al, 2005 | 1 | M/48 | Bilateral A1-A2
junction | IV | Embolization | Good | (16) |
| Ide et al,
2002 | 1 | F/31 | Bilateral carotid
artery segment | II | Clipping | Good | (28) |
| Komiyama et
al, 1994 | 1 | F/66 | Upper segment of the
carotid artery bed | II | Clipping | Good | (8) |
| Czapiga et al,
2013 | 1 | F/45 | Middle cerebral
artery segment | II | Clipping | Good | (14) |
| Wanifuchi et
al, 2001 | 1 | M/45 | Bilateral brain
before A1-A2 junction | II | Clipping | Good | (19) |
| Baldawa et al,
2011 | 1 | M/63 | Bilateral front
traffic | II | Clipping | Good | (17) |
| Choi et al,
2011 | 1 | M/59 | Bilateral brains
distal | II | Clipping | Unknown | (2) |
| Mori et al,
1995 | 1 | F/43 | Bilateral brains
distal | II | Clipping | Good | (5) |
| Sorimachi et
al, 2006 | 1 | F/45 | Upper segment of
the carotid artery bed | II | Clipping | Good | (20) |
| Jagetia et
al, 2013 | 1 | M/55 | Basilar artery
(window deformity fenestration) | II | Embolization | Good | (11) |
| Saatci et
al, 2002 | 1 | M/20 | Basilar artery
(window deformity) | IV | Embolization | Good | (3) |
| Suh et al,
2008 | 1 | M/56 | Bilateral
intracervical-anterior communicating | II | Embolization | Good | (18) |
| Lv et al,
2008 | 1 | M/32 | Upper segment of
the carotid artery bed | II | Embolization | Good | (25) |
| Mitsuhara et
al, 2011 | 1 | F/71 | Right A1 segment
(window deformity) | I | Embolization | Good | (29) |
| Im et al,
2006 | 1 | F/51 | Basilar artery
(window deformity) | I | Embolization | Good | (30) |
| Matsumoto et
al, 2005 | 1 | M/48 | Bilateral front
traffic | III | Embolization | Good | (16) |
| Present study | 1 | F/54 | Bilateral brain
before the A3 segment | II | Clipping | Good | – |
The present study reported a rare instance of DACA
‘kissing’ aneurysms, which were clipped. To the best of our
knowledge, this is the first report regarding the successful
treatment of a patient with DACA ‘kissing’ aneurysms characterized
by bilateral frontal lobes completely adhering to each other. The
management of such aneurysms is challenging, as the space available
for dissection is limited (6).
Additionally, by reviewing the relevant literature, the etiology,
imaging characteristics, misdiagnosis reasons, treatment modalities
and prognosis of DACA were investigated in order to improve the
diagnosis and treatment of this disease.
Case report
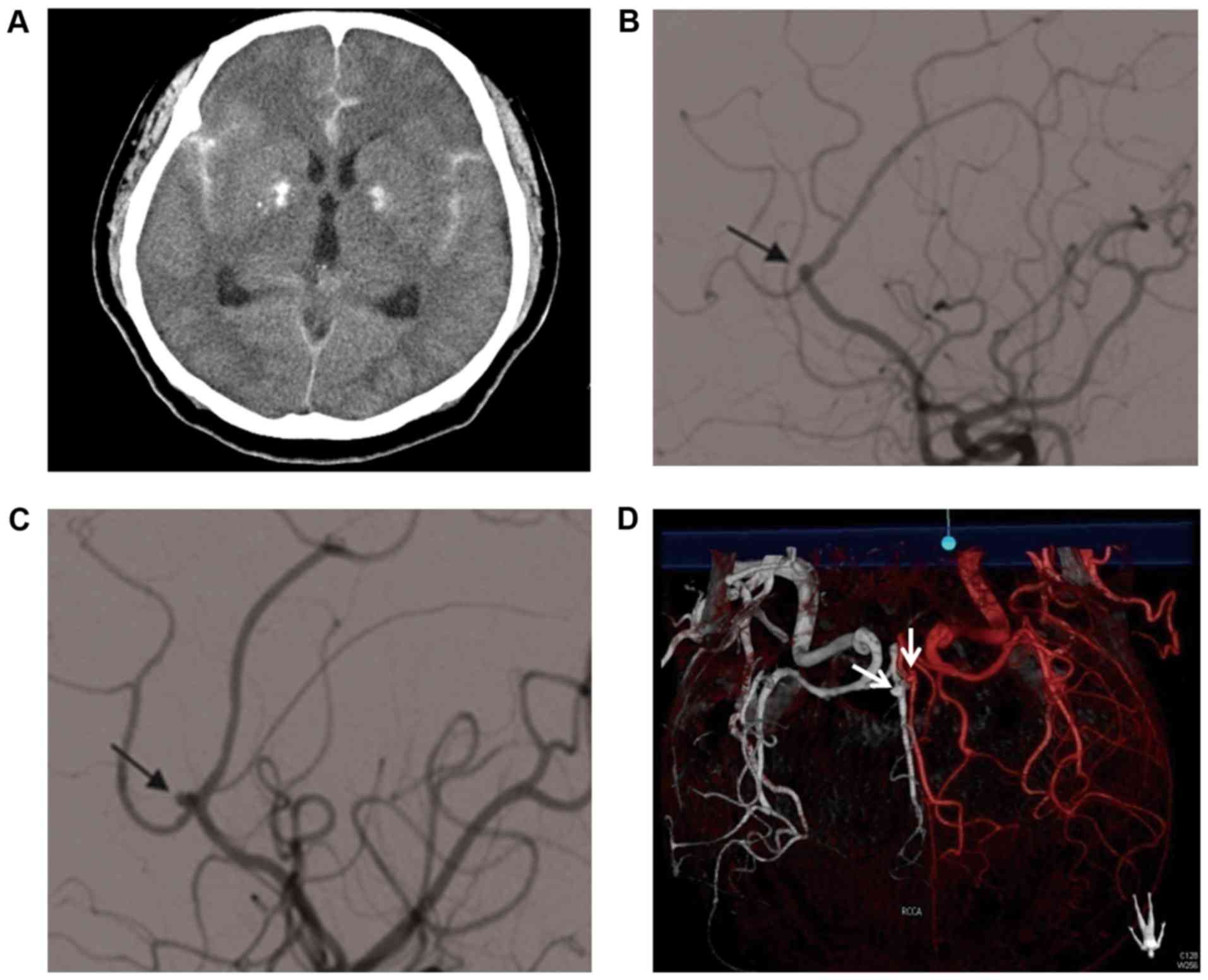
A 54-year-old female patient was admitted to the
People's Hospital of Hainan Province on January 2015 due to
dizziness and headache accompanied by limb fatigue for 8 h, without
any evident disturbance of consciousness during the course of the
disease. The patient had a previous history of hypertension for 2
years and had intermittently taken antihypertensive drugs on her
own (details were not clear). In the outpatient department, a head
computed tomography (CT) scan revealed an increased density in the
interhemispheric fissure, bilateral Sylvian and basal cisterns
(Fig. 1A). The present study was
approved by the Ethics Committee of Hainan General Hospital
(Hainan, China) and informed consent was received from the patient
prior to the study.
Physical examination at admission revealed a blood
pressure of 170/95 mmHg, Hunt-Hess scale II, normal consciousness,
extremities muscle force grade 5, normal muscular tension, reduced
superficial sensibility, equal and round pupils of ~3 mm in
diameter and reactive to light, and neck rigidity. Admission
diagnosis was spontaneous subarachnoid hemorrhage with high
probability of intracranial aneurysm rupture. Emergency cerebral
digital subtraction angiography (DSA) indicated small aneurysms at
segment A3 of bilateral anterior cereal arteries, ~2×2
mm2 with wide necks (Fig.
1B-D). Synthetic analysis of CT and DSA results did not
determine the offending aneurysm; therefore, bilateral aneurysms
should be treated together as otherwise there would be a great risk
for another hemorrhage. Bilateral aneurysms were located at segment
A3, the junction of pericallosal and callosomarginal arteries, with
a small body size and wide neck. Furthermore, the aneurysm-bearing
artery formed a right angle. Finally, microsurgical treatment was
preferentially adopted using an interhemispheric fissure approach
for aneurysm clipping.
The patient was immediately transferred to the
operating room for emergency tracheal intubation following DSA
examination. During treatment of the patient, as the longitudinal
fissure was narrow, the surgical space was limited; therefore, it
was likely to lead to aneurysm rupture during parent artery
isolation. Conventional application of mannitol (20% mannitol, 125
ml, 0.5 mg/kg, i.v., Hunan Kelun Pharmaceutical Co., Ltd., Yueyang,
China) was performed as soon as the dura was cut, with
anesthesiologists providing hyperventilation. Following
satisfactory general anesthesia, an incision was made at the right
forehead flap, and the forehead and bone flaps were successively
freed. The dural tension was high and following detachment of the
dura mater, the intracranial tension was also increased.
Next, the lateral cisterns were cut open to drain
the cerebrospinal fluid (CSF) as much as possible, and the
intracranial pressure was evidently decreased. Through longitudinal
fissure, it was revealed that the bilateral frontal lobes
completely adhered to each other from below the falx cerebri. As
the bilateral frontal lobes grew together from the falx below the
brain, the anterior communicating artery was detected making full
use of the normal anatomical space. An incision was made into the
anterior cranial base to expose the anterior communicating artery.
Exploration was performed along the parent artery to the distal
dissection of bilateral frontal lobes initiated from the segment of
A2, and when hematoma was detected, which was likely to be the
aneurysm area, separation of aneurysms was undertaken following
temporary occlusion of bilateral aneurysms. Subsequently, an
incision was made to dissect bilateral frontal lobes and to explore
the bilateral anterior cerebral arteries to segment A3. The
bilateral aneurysms were located at the bifurcation of segment A3,
both ~2×2 mm2, and their bodies adhered to each other.
Following dissection to thoroughly expose the aneurysm necks, one
Yasagier 720 aneurysm clip and one Yasagier 740 aneurysm clip
(Rebstock Instruments GmbH Dürbheim, Germany) were used to clip
aneurysm necks. The aneurysms did not rupture and no hemorrhage
occurred during clipping.
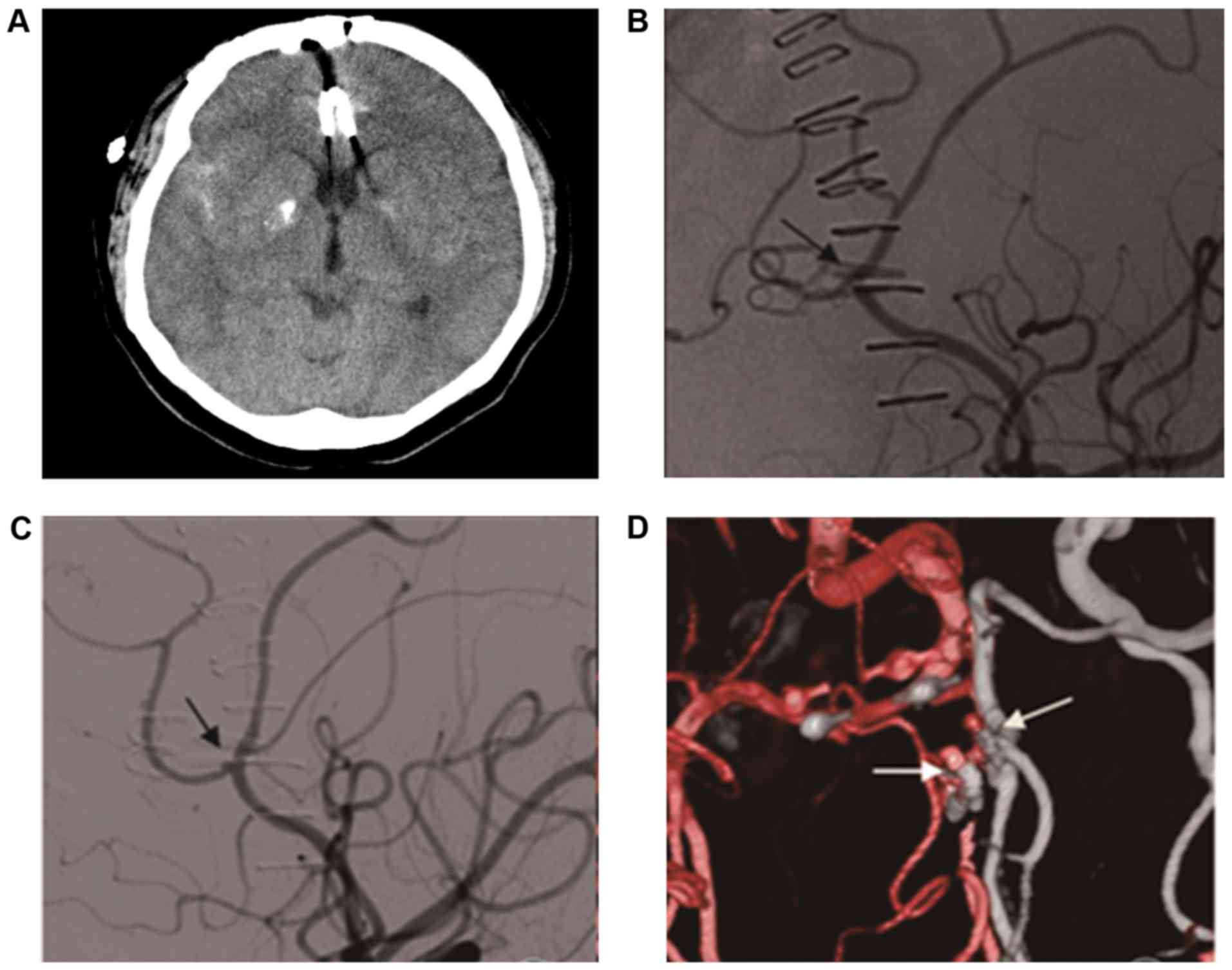
Following examinations performed to ensure that the
aneurysms were completely clipped and the aneurysm-bearing arteries
were open, the skull was closed. Due to the poor brain distal
compensatory circulation, it was recommended that the blocking time
should be <10 min in order to avoid new nerve dysfunction
following postoperative cerebral infarction, and the surgery was
successful. After the patient woke up from the anesthesia, head CT
was performed to exclude hemorrhage at the surgery areas (Fig. 2A). Furthermore, lumbar puncture was
performed intermittently to drain CSF following the surgery. In
total, 10 days later, re-examination demonstrated completely
clipped aneurysms and fluent blood flow in aneurysm-bearing
arteries (Fig. 2B-D). The patient
recovered well and was discharged 12 days postoperatively with a
Modified Rankin Scale=0 (7). A
follow-up at 6 months after discharge was used to determine that
the patient had recovered successfully.
Literature review
For the literature review, all articles referring to
‘kissing aneurysms’ in PubMed (https://www.ncbi.nlm.nih.gov/pubmed) were retrieved,
and a total of 21 articles were a hit, of which one was an original
report and remaining 20 were case reports. Altogether there were 30
cases of ‘kissing’ aneurysms reported in these articles (Table I). There were 12 male patients and 18
female patients, with a mean age of 46.4 years. In 4 cases,
aneurysms were located at DACAs.
Discussion
Aneurysms of the DACA make up 3–7% of intracranial
aneurysms (6). As particular types
of multiple aneurysms, ‘kissing’ aneurysms account for <1% of
intracranial aneurysms (8), and are
most commonly observed at the supraclinoid internal carotid artery
(this occurred in 15 cases in total from the literature reviewed in
the present study, accounting for ~50% of all cases). Furthermore,
‘kissing’ aneurysms at the DACA are rare, and there are a total of
5 known cases, including the present one. Analyses of previous case
reports demonstrated that the morbidity of ‘kissing’ aneurysms is
higher in females than in males (9),
with no difference in the age of onset compared to other types of
aneurysms. A study by Harada et al (10) classified ‘kissing’ aneurysms into two
types according to whether their necks originated from the same
aneurysm-bearing artery: Type I from the same artery and type II
from different arteries. A study by Jagetia et al (11) reported a special type of ‘kissing’
aneurysms, which were located at a variant and fenestrated artery
and could be classified as a sub-type of type I. Although a
fenestrated artery has a normal morphology, the endothelium is
thin, the elastic layer is discontinuous and the incidence of
‘kissing’ aneurysms is high (1).
This indicates that the occurrence of ‘kissing’ aneurysms may be
associated with congenital abnormality of the embryo (1,12). Among
5 cases of ‘kissing’ aneurysms reported by Jefferson (1), the first-grade relatives of 2 young
patients had a history of aneurysms, supporting the viewpoint that
this type of aneurysm may be affected by hereditary factors.
Furthermore, ‘kissing’ aneurysms are also associated
with vascular structural changes, such as the anterior
communicating artery complex (4,13).
Vascular structural changes may induce the formation of aneurysms
via influencing the hemodynamics, although certain researchers
doubt the reason of hemodynamics (2). In the present study, there were no
evident abnormalities in the morphology and running of cerebral
arteries. However, bilateral frontal lobes were adhered to each
other, indicating the abnormal development of brain tissues, which
may have interfered with the development of the aneurysm-bearing
artery wall. In the present case, bilateral anterior cerebral
arteries almost formed a right angle from segment A3 to A4, and
were subjected to a strong impact force from the blood flow. The
above two factors contributed to the formation of aneurysms.
The clinical manifestations of ‘kissing’ aneurysms
are similar to other types of aneurysms, they mainly manifest with
a subarachnoid hemorrhage and space occupying effect (14). There is only 1 case of ventricle
hematocele not accompanied by intracranial hematoma (15). The specific structure of partial
fusion of aneurysm walls makes diagnosis difficult, and they are
often misdiagnosed as a single irregular or lobulated aneurysm
(16). Statistical analysis by
Harada et al (10)
demonstrated that 57% of ‘kissing’ aneurysms had been misdiagnosed
prior to surgery. Precise preoperative diagnosis of ‘kissing’
aneurysms is paramount, and it may be improved in the following
aspects. First, ‘kissing’ aneurysms are common in the internal
carotid, bilateral posterior communicating, anterior communicating
and anterior cerebral arteries, with different neck locations.
Dynamic observation during DSA may find that ‘kissing’ aneurysms of
the same aneurysm-bearing artery have a prolonged filling phase.
For suspected pulmonary aneurysms, adding multi-angle oblique
scanning and capturing compression images may make a differential
diagnosis. Second, three-dimensional (3D)-DSA and angiography at a
specific angle (17) or 3D-CT
angiography is helpful for diagnosis. It is quite intriguing to
determine the offending aneurysm for ‘kissing’ aneurysm hemorrhage
due to a lack of reported cases (2,16) and
limited literature available for reference. Generally, a diagnosis
could be made in accordance with the determination of the offending
aneurysm of multiple aneurysms: Irregular aneurysm wall with small
vesicle-like bulges and the transparent blue aneurysm wall
occasionally attached with blood clot identified during surgery
(9). In the present case, the right
aneurysm was more irregular than the left and was diagnosed as the
offending aneurysm prior to the surgery, which was confirmed during
the surgery.
In the present study, the ‘kissing’ aneurysms were
thought to be adjacent, therefore, the two aneurysms could be
clipped through one surgery route, and it would be easy to
determine the offending aneurysm in order to explore the
aneurysm-bearing artery and to emergently and temporarily occlude
it during the surgery. If interventional embolization was feasible,
two sets of micro catheters could be used to embolize bilateral
aneurysms simultaneously or to prevent aneurysm rupture during the
surgery. Therefore, compared with intracranial multiple aneurysms
located far from each other, it is not imminent to determine the
offending aneurysm of ‘kissing’ aneurysms.
A literature review revealed that the previous 3
cases of ‘kissing’ aneurysms at the anterior cerebral arteries were
all treated with microsurgery of aneurysm clipping (2,4,5). In the present case, it was difficult to
control the catheter in the distal portion of the artery and
bilateral aneurysms were small with wide necks, making complete
embolism impossible. Additionally, a spring coil (a detachable
spiral metallic material used for embolization of an aneurysm by an
arterial approach) may have migrated and caused occlusion of the
DACA, leading to a large area of cerebral infarction in the
functional areas of the frontal lobe. Aneurysms were located at
segment A3 at the bifurcation of pericallosal and callosomarginal
arteries, where a right angle was formed and artery lumen was
narrow, making it difficult to transport and place the stent. With
reference to literature and by weighing the pros and cons,
bilateral aneurysm clipping was performed through the
interhemispheric fissure approach subsequent to opening the skull
in the right forehead (2,5).
The aneurysms at the segment A3 of the anterior
cerebral arteries were located deep in the longitudinal fissure.
The narrow interhemispheric space and cerebral edema following
subarachnoid hemorrhage left little room for surgery. Additionally,
arachnoid adhesion and occlusion of a number of cisterns made it
difficult to open the cistern for CSF drainage. In order to expose
aneurysm necks, it may be necessary to sacrifice the bridging
veins, which could exacerbate postoperative cerebral edema
(17). In the present study, the
aneurysms were partly attached to the frontal lobes, thus they may
have ruptured again during brain tissue stretching or aneurysm
isolation during the surgery. A study by Suh et al (18) reported an intra-operative rupture
rate of 50% during surgery on DACA aneurysms, which was much higher
than that of aneurysms from other sites. Intra-operative CSF
drainage to reduce intracranial pressure and prevent aneurysm
rupture is pivotal for successful therapy (17). One peculiar aspect of the present
case is that the patient's bilateral frontal lobes were completely
adhered to each other from below the falx cerebri during surgery,
which markedly increased the difficulty in exposing aneurysms and
the risk of aneurysm rupture. Thorough preparations were prepared
for this situation, such as the administered of mannitol for
dehydration to reduce intracranial pressure along with skull
opening. Arachnoid membrane was carefully and sharply dissected to
drain CSF from the interhemispheric fissure cistern during surgery.
After achieving satisfactory intracranial pressure, bilateral
segment A1 of the anterior cerebral arteries and anterior
communicating arteries were dissected and exposed through the
anterior cranial fossa. Subsequently, frontal basal tissues were
cut open longitudinally along the anterior cerebral arteries, and
an upward exploration to the bilateral aneurysms at segment A3 was
performed, during which time we took the advantage of the temporary
occlusion technique (9), and clipped
the bilateral aneurysms parallel to the anterior cerebral arteries
following careful isolation of the aneurysm necks. Subsequently,
puncture examination was performed to check whether aneurysms were
completely clipped. An attempt was made not to dissect the adhesion
walls between aneurysms prior to clipping to prevent rupture and
hemorrhage (19,20). The advantage of this method is that
once aneurysm rupture and hemorrhage occur in the course of
exploration for aneurysms, they may be instantly and temporarily
blocked. The limitation is that a relatively large area of injured
brain tissues may exacerbate postoperative cerebral edema and cause
postoperative hemorrhage in the surgery area. Previously, a number
of researchers have used the navigation system (21) and intraoperative ultrasound (22) to pinpoint intraoperative brain tissue
injury during anterior cerebral artery aneurysm surgery. These
techniques may also be applied in the surgery on ‘kissing’
aneurysms of DACA.
Compared with microsurgery, interventional
embolization causes less injury to the nerve tissues and reduces
the incidence of complications. Furthermore, it should be a
preferential therapy (6),
particularly for patients with poor general conditions (23). Researchers have treated aneurysms
with interventional embolization at the vertebrobasilar, middle
cerebral, bilateral ophthalmic and anterior communicating arteries
with favorable therapeutic effects (11,18,24,25).
Although interventional embolization for the treatment of distal
anterior cerebral aneurysms has been reported to be beneficial
(13,26), thus far reports of this therapy on
‘kissing’ aneurysms of DACA are rare. The possible reasons are as
follows: A number of cases of ‘kissing’ aneurysms at DACA were
treated with interventional embolization and could not be diagnosed
by imaging and their diagnosis was missed (10,16).
Furthermore, the long distance and narrow lumen of DACA make it
difficult for micro-catheter manipulation (18).
‘Kissing’ aneurysms at DACA are mostly small, thus
the walls are easily punctured during micro-catheter and
guided-wire manipulation, causing hemorrhage, which is hard to
repair (2). Furthermore, a wide neck
is commonly observed and the aneurysm-bearing artery is evidently
curved, making it difficult to implant the stent (9). The structure of ‘kissing’ aneurysms are
complex, and it is hard for surgeons to grasp their complete
morphology, resulting in an increase in unpredictable factors
during the surgery. Furthermore, familiarity of surgeons with the
two therapies may also influence their choice of surgery
strategies. By accumulating the experience of endovascular
treatment and improvement in interventional materials, ‘kissing’
aneurysms of DACA may be well treated with embolization.
The patient of the present study recovered well and
was discharged without defects in neurological functions. In
previous reports, the majority of patients with ‘kissing’ aneurysms
had a good prognosis, with only one case of unknown prognosis,
reaching a good prognosis rate of 96.8%. This may predominantly be
attributed to the following factors: i) The majority of the
patients had a good pre-operative condition, and only 4 of them had
high Hunt-Hess scales; ii) some ‘kissing’ aneurysms patients
underwent interventional embolization, which made it impossible to
identify whether the aneurysms had partially adherent walls. As a
result, this lead to missed diagnosis and affected the prognosis
analysis; and iii) the sample size was not large enough, and there
were too few cases to thoroughly demonstrate a complete prognosis
of ‘kissing’ aneurysms.
In conclusion, DACA is easily misdiagnosed and the
presence of bi-lobed aneurysms indicated the presence of kissing
aneurysms. Further examination of 3D DSA is helpful for diagnosis
and the application of the longitudinal fissure approach to block
the distal anterior cerebral artery is conducive to DACA.
References
|
1
|
Jefferson A: The significance for
diagnosis and for surgical technique of multiple aneurysms of the
same internal carotid artery. Acta Neurochir (Wien). 41:23–37.
1978. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Choi CY, Han SR, Yee GT and Lee CH:
Kissing aneurysms of the distal anterior cerebral artery. J Clin
Neurosci. 18:260–262. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saatci I, Cekirge HS, Karcaaltincaba M,
Basgun N, Berker M, Timurkaynak E and Ozcan OE: Endovascular
treatment of kissing aneurysms at the fenestrated basilar artery.
Case report with literature review. Surg Neurol. 58:54–58. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yaşargil MG and Carter LP: Saccular
aneurysms of the distal anterior cerebral artery. J Neurosurg.
40:218–223. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mori T, Fujimoto M, Shimada K, Shin H,
Sakakibara T and Yamaki T: Kissing aneurysms of distal anterior
cerebral arteries demonstrated by magnetic resonance angiography.
Surg Neurol. 43:497–499. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Otani N, Takasato Y, Masaoka H, Hayakawa
T, Yoshino Y, Yatsushige H, Sumiyoshi K, Miyawaki H, Aoyagi C,
Takeuchi S and Suzuki G: Clinical features and surgical outcomes of
ruptured distal anterior cerebral artery aneurysms in 20
consecutively managed patients. J Clin Neurosci. 16:802–806. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Banks JL and Marotta CA: Outcomes validity
and reliability of the modified Rankin scale: Implications for
stroke clinical trials: A literature review and synthesis. Stroke.
38:1091–1096. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Komiyama M, Yasui T, Tamura K, Nagata Y,
Fu Y and Yagura H: ‘Kissing aneurysms’ of the internal carotid
artery. Neurol Med Chir (Tokyo). 34:360–364. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Guo L, Qiu Y, Ge J and Zhang X: Kissing
aneurysms of the internal carotid artery treated with surgical
clipping. Neurol India. 60:353–355. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Harada K, Orita T and Ueda Y: Large
kissing aneurysms of the middle cerebral artery: A case
report-classification of kissing aneurysms. No Shinkei Geka.
32:513–517. 2004.PubMed/NCBI
|
|
11
|
Jagetia A, Bhutte M, Aher R, Sinha S and
Singh D: Kissing aneurysm in a fenestrated mid-basilar arterial
trunk: A case report and review of literature. Neurol India.
61:437–439. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Krings T, Baccin CE, Alvarez H, Ozanne A,
Stracke P and Lasjaunias PL: Segmental unfused basilar artery with
kissing aneurysms: Report of three cases and literature review.
Acta Neurochir (Wien). 149:567–574. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Enesi E, Rroji A, Demneri M, Vreto G and
Petrela M: Mirror image distal anterior cerebral artery aneurysms
treated with coil embolization. a report of two cases and
literature review. Interv Neuroradiol. 19:49–55. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Czapiga B, Kozba-Gosztyla M, Bereza S and
Jarmundowicz W: Unusual angiographic images of unruptured, large,
kissing middle cerebral artery aneurysms. Acta Neurochir (Wien).
155:283–284. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fujimura M, Sugawara T, Higuchi H, Oku T
and Seki H: A ruptured aneurysm at the distal end of the basilar
artery fenestration associated with multiple fenestrations of the
vertebrobasilar system: Case report. Surg Neurol. 47:469–472. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Matsumoto H, Takechi A, Kohno K and Sasaki
U: ‘Kissing aneurysms’ of the anterior communicating artery treated
with coil embolization. J Endovasc Ther. 12:750–754. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Baldawa SS, Menon G and Nair S: Kissing
anterior communicating artery aneurysms: Diagnostic dilemma and
management issues. J Postgrad Med. 57:44–47. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Suh SJ, Kang DG, Ryu KY and Cho JH:
Endovascular treatment of ‘kissing aneurysms’ at the anterior
communicating artery. J Korean Neurosurg Soc. 44:163–165. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wanifuchi H, Shimizu T, Higa T and Nakaya
K: Kissing mirror image anterior communicating artery
aneurysms-case report. Neurol Med Chir (Tokyo). 41:29–32. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sorimachi T, Fujii Y, Nashimoto T and
Morita K: Kissing aneurysms at the junction of the internal carotid
artery and the ipsilateral duplicate anterior choroidal
arteries-case report. Neurol Med Chir (Tokyo). 46:29–31. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang T, Li F and Zheng G: Application of
neuronavigation in the surgery for distal anterior cerebral
aneurysm. J China-Japan Friendship Hospital. 27:79–81. 2013.(In
Chinese).
|
|
22
|
Piao J, Luo Q and Yu J: Surgical treatment
of ruptured anterior cerebral artery aneurysm (22 cases report).
Chin J Nerv Dis. 431–432. 2013.(In Chinese).
|
|
23
|
Park KY, Kim BM, Lim YC, Chung J, Kim DJ,
Joo JY, Huh SK, Kim DI, Lee KC and Lee JW: The role of endovascular
treatment for ruptured distal anterior cerebral artery aneurysms:
Comparison with microsurgical clipping. J Neuroimaging. 25:81–86.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Takahashi C, Kubo M, Okamoto S, Matsumura
N, Horie Y, Hayashi N, Kuwayama N and Endo S: ‘Kissing’ aneurysms
of the internal carotid artery treated by coil embolization. Neurol
Med Chir (Tokyo). 51:653–656. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lv X, Li Y and Wu Z: Endovascular
management for bilateral ophthalmic segment ‘kissing’ aneurysms
presenting with nasal bleeding. A case report. Neuroradiol J.
21:266–269. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Oishi H, Nonaka S, Yamamoto M and Arai H:
Feasibility and efficacy of endovascular therapy for ruptured
distal anterior cerebral artery aneurysms. Neurol Med Chir (Tokyo).
53:304–309. 2013. View Article : Google Scholar : PubMed/NCBI
|