Introduction
Osteoporosis (OP) is a clinically common disease in
systemic skeletal system, characterized by the microstructural
damage of bone tissues and low bone mass, and patients are prone to
fracture (1). Maintenance
hemodialysis (MHD) of chronic renal failure (CRF) will lead to a
variety of complications, such as infection, cardiovascular
diseases and OP. The OP incidence rate in MHD patients is up to
40–60%, seriously affecting their life quality (2). MHD patients often have oxidative stress
(OS) and microinflammatory status; advanced oxidized protein
product (AOPP) is one of the markers reflecting the OS status in
the body, and malondialdehyde (MDA) is the end metabolite of OS and
can be used as a marker reflecting the OS level in the body; the
microinflammation in MHD patients is often characterized by the
increased tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) and
IL-1 (3,4). Melatonin (MT) is a kind of hormone
secreted by the pineal gland, which not only has the effects of
anti-inflammation, anti-oxidation and wakening regulation, but also
can promote the proliferation and differentiation of osteoblasts
and inhibit the proliferation and differentiation of osteoclasts
through a variety of ways, and it has a close relationship with OP
(5). In this study, the levels of
MT, AOPP, MDA, TNF-α, IL-6 and IL-1 in CRF patients receiving MHD
were detected to analyze whether they were involved in the
occurrence of OP and their relationships with osteoporosis.
Materials and methods
General materials
Ninety-four CRF patients treated in Dezhou People's
Hospital (Dezhoo, China) from May 2016 to April 2017 were selected.
Inclusion criteria: 1) patients meeting the diagnostic criteria of
chronic renal failure; 2) patients receiving MHD for more than 3
months; 3) patients who signed the informed consent. Exclusion
criteria: 1) patients with severe heart, brain or liver diseases,
or accompanied with mental illness; 2) patients with malignant
tumors, pregnant or lactating women. According to whether
osteoporosis was involved, patients enrolled were divided into the
osteoporosis group (observation group, n=49) and the
non-osteoporosis group (control group, n=45). There were no
statistically significant differences in the baseline data between
the two groups (P>0.05) (Table
I).
 | Table I.Baseline data of patients in the two
groups. |
Table I.
Baseline data of patients in the two
groups.
| Item | Control group
(n=45) | Observation group
(n=49) | t/χ2
test | P-value |
|---|
| Sex
(male/female) | 25/20 | 29/20 | 0.022 | 0.883 |
| Age (years) | 35–70 | 35–65 |
|
|
| Average age
(years) | 46.56±8.43 | 46.85±8.52 | 0.166 | 0.869 |
| Course of disease
(month) | 13.62±3.46 | 13.25±3.37 | 0.525 | 0.601 |
| BMI
(kg/m2) | 22.43±3.27 | 21.87±3.58 | 0.790 | 0.432 |
| Blood glucose
(mmol/l) |
5.78±1.15 |
5.63±1.24 | 0.607 | 0.545 |
| Total cholesterol
(mmol/l) |
6.12±0.73 |
6.09±0.68 | 0.206 | 0.837 |
| Triglyceride
(mmol/l) |
2.38±1.27 |
2.52±1.34 | 0.519 | 0.605 |
Hemodialysis method
Using the hemodialysis machine (Fresenius,
Oberursel, German), the double-lumen catheter was placed in the
right side of the neck or right femoral vein to establish
cardiopulmonary bypass; the diluted displacement liquid (Shanghai
Changzheng Pharmaceutical Co., Shanghai, China) was injected using
the negative-pressure ultra-filter pump, and the
low-molecular-weight heparin (Tianjin Chase Sun Pharmaceutical Co.,
Ltd., Tianjin, China, approval no. NMPN H20020469) was used for
anticoagulation (first dose 3,000 U, addition 500 U/h, replacement
rate 4.0 l/h), and the blood flow was maintained at approximately
200 ml/min. Patients were treated for 4 h each time and received
dialysis 3 times per week.
Bone mineral density (BMD)
detection
BMD was measured using dual-energy X-ray bone
densitometer (Shenzhen XRAY Electric Co., Ltd., Shenzhen, China),
including the lateral lumber spine. The graphical analysis area was
divided into total lateral lumber spine and lateral medial area
(approximately 1/2 of the whole vertebral body in the length and
width); the T-value (the ratio of patients' BMD to age) was
calculated.
Detection of MT, AOPP, MDA, TNF-α,
IL-6 and IL-1 levels
Venous blood (5 ml) was collected from patients (at
7:00 in the morning after fasting for 8 h), and the serum was
immediately separated and placed at −80°C for standby application.
The levels of serum AOPP, MT, TNF-α, IL-6 and IL-1 were measured
via enzyme-linked immunosorbent assay (ELISA). The relevant kits
were provided by Shanghai Hengyuan Biotechnology Co., Ltd.
(Shanghai, China) and the operation was strictly according to the
instructions of the kit. Samples (1-fold dilution) and 100 µl
enzyme-labeled solution were added into the micro-holes of reaction
plate for incubation at 37°C for 90 min. After the plate was washed
3 times (15 sec interval at every two times), the color developing
agents A and B (50 µl for each) were added for incubation at room
temperature at 20°C in the dark for 15 min. The OD value was read
at a wavelength of 450 nm using the microplate reader (Shenzhen
SinoThinker Technology Co., Ltd., Shenzhen, China) within 15 min.
Then the levels of AOPP, MT, TNF-α, IL-6 and IL-1 were
calculated.
The serum MDA was detected via thiobarbituric acid
(TBA) assay. Preparations: the reagent A in the MDA kit (Nanjing
Jiancheng Bioengineering Institute, Nanjing, China) was heated to
transparency through water bath, and 340 ml double distilled water
was added and mixed evenly into the reagent B and stored at 4°C.
After the reagent C was fully dissolved by 60 ml double distilled
water (95°C), 60 ml glacial acetic acid was added, mixed evenly and
stored in the dark at 4°C. The standard product (10 nmol/ml
tetraethoxypropane) was stored at 4°C. Operating steps: 1) The
standard product (1 ml) was added into the standard tube, the serum
(0.1 ml) was added into the testing tube, and the anhydrous ethanol
was added into the standard blank tube; 2) the reagent A (0.1 ml)
was added and mixed evenly into the standard tube, testing tube,
standard blank tube and testing blank tube, and then the reagent B
(0.1 ml) was added; 3) the reagent C (0.1 ml) was added into the
standard tube, testing tube and standard blank tube, and 50%
glacial acetic acid (0.1 ml) was added into the testing blank tube;
4) the solution was mixed evenly using the swirling mixer; the tube
mouth was tightened using the fresh-keeping membrane and one riser
vent was punctured; then the tube was soaked in hot water (95°C)
for 40 min and cooled under the running water; 5) after the
centrifugation for 10 min at 2,000 × g, the supernatant was taken,
the OD value at a wavelength of 532 nm was measured using the
microplate reader, and the content of MDA in serum was
calculated.
Evaluation criteria
Fasting venous blood (5 ml) was collected from
patients in the morning. The levels of serum AOPP, inflammatory
factors (TNF-α, IL-6 and IL-1) and MT were analyzed via ELISA, and
the level of MDA was detected via TBA assay.
Judgment criteria of OP: 1) normal bone mass:
T-value >-1; 2) bone mass loss: T-value =−1 to −2; 3) OP:
T-value <-2.
Statistical analysis
Data were processed using SPSS 19.0 software (SPSS
Inc., Chicago, IL, USA). Measurement data are presented as mean ±
standard deviation, and t-test was used; enumeration data are
presented as ratio, and Chi-square test was used. Pearson's
correlation coefficient analysis was used for the correlation.
P<0.05 was considered to indicate a statistically significant
difference. The study was approved by the Ethics Committee of
Dezhou People's Hospital and written informed consents were signed
by the patients and/or guardians.
Results
Comparison of oxidative stress and MT
level in patients in the two groups
The levels of AOPP and MDA in observation group were
significantly higher than those in the control group, but MT level
was significantly lower than that in the control group (P<0.05)
(Table II).
 | Table II.Comparisons of oxidative stress and MT
level in patients between the two groups. |
Table II.
Comparisons of oxidative stress and MT
level in patients between the two groups.
| Group | n | AOPP (µmol/l) | MDA (nmol/l) | MT (pg/ml) |
|---|
| Observation
group | 49 | 108.95±15.13 | 5.97±1.47 | 19.76±3.38 |
| Control group | 45 | 43.69±9.06 | 2.73±0.86 | 24.43±3.27 |
| t-test |
| 25.091 | 12.894 | 6.797 |
| P-value |
| <0.001 | <0.001 | <0.001 |
Comparisons of inflammatory factor
levels in patients in the two groups
The levels of TNF-α, IL-6 and IL-1 in observation
group were obviously higher than those in control group (P<0.05)
(Table III).
 | Table III.Comparisons of inflammatory factor
levels in patients between the two groups (ng/l). |
Table III.
Comparisons of inflammatory factor
levels in patients between the two groups (ng/l).
| Group | n | TNF-α | IL-6 | IL-1 |
|---|
| Observation
group | 49 | 49.98±3.15 | 53.48±3.35 | 47.28±3.19 |
| Control group | 45 | 37.83±3.04 | 41.45±3.23 | 35.39±3.17 |
| t-test |
| 18.996 | 17.693 | 18.106 |
| P-value |
| <0.001 | <0.001 | <0.001 |
Comparisons of mid-lateral lumbar
vertebrae and total lumbar BMD
The mid-lateral lumbar vertebrae and total lumbar
BMD and T-values in observation group were significantly lower than
those in control group (P<0.05) (Table IV).
 | Table IV.Comparisons of lateral lumbar bone
mineral density (BMD) and T-value. |
Table IV.
Comparisons of lateral lumbar bone
mineral density (BMD) and T-value.
|
|
| BMD
(g/cm2) | T-value |
|---|
|
|
|
|
|
|---|
| Group | n | Total lateral
lumbar | Mid-lateral
lumbar | Total lateral
lumbar | Mid-lateral
lumbar |
|---|
| Observation
group | 49 | 0.73±0.12 | 0.65±0.13 | −3.75±0.93 | −4.15±0.86 |
| Control group | 45 | 0.91±0.13 | 0.86±0.14 | −1.03±0.86 | −1.09±0.76 |
| t-test |
| 6.981 | 7.541 | 14.683 | 18.213 |
| P-value |
| <0.001 | <0.001 | <0.001 | <0.001 |
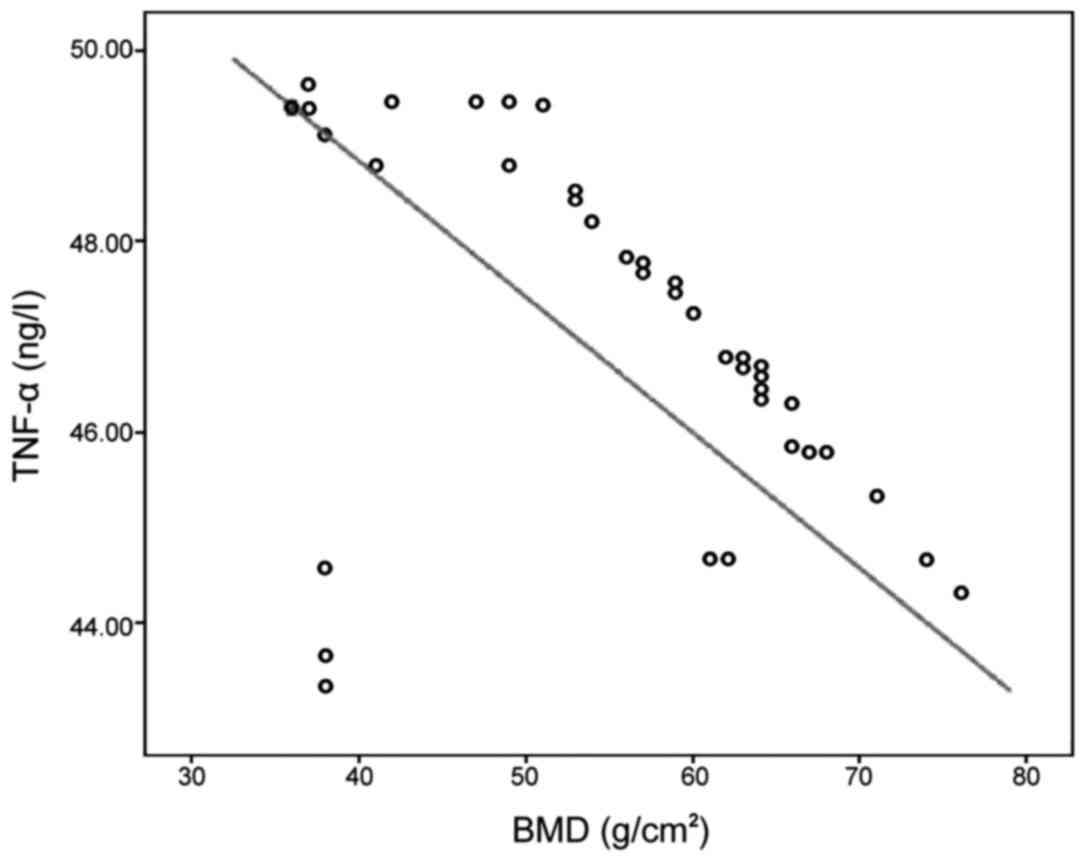
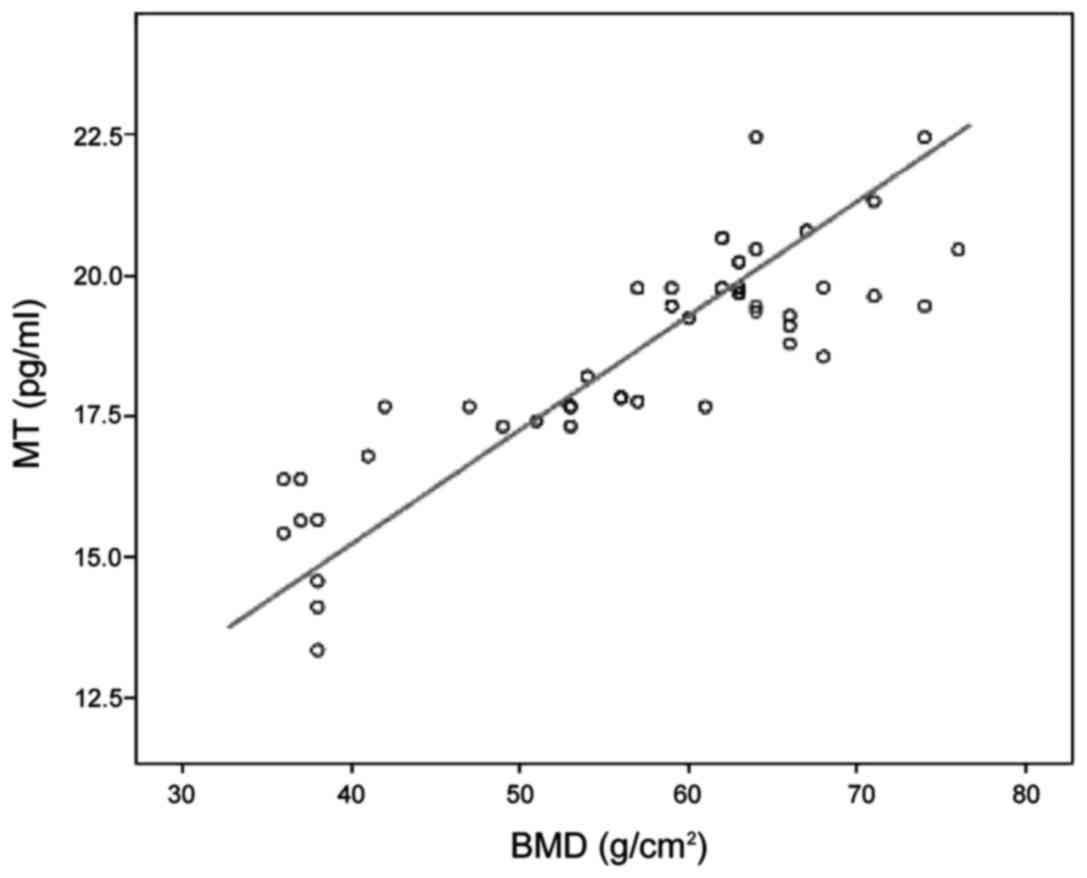
Correlation analysis of oxidative
stress, inflammation and MT level with BMD
Pearson's correlation analysis showed that AOPP,
MDA, TNF-α, IL-6 and IL-1 levels were negatively correlated with
BMD, but MT was positively correlated with BMD (P<0.05)
(Figs. 1–6, Table
V).
 | Table V.Correlation analysis of oxidative
stress, inflammation and MT level with BMD. |
Table V.
Correlation analysis of oxidative
stress, inflammation and MT level with BMD.
|
| Correlation with
BMD |
|---|
|
|
|
|---|
| Item | r-value | P-value | Item | r-value | P-value |
|---|
| TNF-α | −0.487 | −0.401 | AOPP | −0.406 | −0.424 |
| IL-6 | −0.401 | −0.417 | MDA | −0.424 | 0.439 |
| IL-1 | −0.417 | −0.406 | MT | 0.439 | 0.015 |
Discussion
OP is caused by the bone metabolic disorders (bone
resorption is greater than bone formation), characterized by the
decreased bone mass per unit volume and increased bone fragility,
and it will continuously develop and easily leads to fractures
(6). In the past, it was thought
that the mechanism of OP accompanied in CRF patients was that the
calcium-phosphorus metabolic disturbance in patients reduced the
level of vitamin D in the body, thus leading to metabolic acidosis
and secondary hyperparathyroidism. In recent years, with the
deepening of research, it has been recognized that the bone
metabolism in CRF patients receiving long-term MHD will be jointly
regulated by a variety of hormones and cytokines, thus causing the
abnormal expression levels and functions of OPG/RANKL/RANK system
in the body, ultimately affecting the differentiation and function
of osteoclasts and inducing OP (7).
MT is a kind of indole neuroendocrine hormone
secreted by pineal body, as well as the strongest free radical
scavenger currently known (8).
Studies have shown that MT secretion in CRF patients is
significantly lower than that in normal population, especially in
MHD patients whose MT peak at night disappears (9). The antioxidant mechanism in normal
state of human body is perfect, which can eliminate oxygen free
radicals through the enzyme catalysis and enzyme-free catalysis,
thus playing an antioxidant effect (10). When the defense system function in
the body is low, the redox reaction will be out of balance,
resulting in the accumulation of reactive oxygen species (ROS),
imbalance between oxidation and anti-oxidation, among which
oxidation dominates, causing OS (11). AOPP is a kind of double-arginine
protein cross-linking agent produced by albumin in OS state. MDA is
a toxic substance produced by the peroxidation of unsaturated fatty
acids in the cell membrane due to superoxide anion in the body
(12,13). The results of this study showed that
the level of MT in observation group was significantly lower than
that in control group, but the levels of AOPP and MDA were
significantly higher than those in the control group (P<0.05),
indicating that CRF patients with OP are in an obvious
oxidative-antioxidant system imbalance, because AOPP results not
only from ROS, but also is the result of OS. Besides, MDA has a
strong cytotoxicity and will cause the cross-linking polymerization
of macromolecules (proteins, lipids and nucleic acids), whose
content directly reflects the rate and intensity of lipid
peroxidation, and it can be used as an index for the severity of
free radical damage, indirectly reflecting the process of oxygen
free radical damage. The decreased MT level may be related to OS,
and interacts in CRF patients with OP.
Clinically, BMD is often used for the OP diagnosis.
Cancellous bone (60–75%) in the total skeletal system is
concentrated in the human lumbar spine, so the measurement of
lumbar BMD in MHD patients can reflect the early changes in bone
mineral content. In addition, the bone turnover rate of cancellous
bone is higher than that of cortical bone, and it is more sensitive
to all kinds of metabolic stimuli. Moreover, its accumulation of
bone mass will reach the peak earlier than cortical bone, so the
measurement of lateral lumbar BMD has a higher sensitivity
(14).
The proteinuria and high renin - angiotensin
activity, in CRF patients can stimulate the body's inflammatory
response, and inhibit the T lymphocyte immune function and lead to
immune dysfunction (15). TNF-α is
an important mononuclear inflammatory factor, and IL-6 is a member
of the interleukin family, as well as a lymphocyte factor in the
acute-phase response, playing a variety of roles in the immune
response (16). Moreover, IL-1 is
also one of the important members of the interleukin family,
including IL-1α and IL-1β, in which IL-1β is one of the important
inflammatory cytokines in the inflammatory process (17). The results of this study showed that
the levels of TNF-α, IL-6 and IL-1 in observation group were
obviously higher than those in control group (P<0.05),
suggesting that the microinflammation is more obvious in CRF
patients with OP.
The results in this study showed that AOPP, MDA,
TNF-α, IL-6 and IL-1 levels were negatively correlated with BMD,
but MT was positively correlated with BMD (P<0.05), because
enough MT will decrease the formation and activation of
osteoclasts, thereby inhibiting the bone resorption and increasing
the bone mass (18). In addition, MT
can induce the secretion of growth hormone, and its synergistic
application can promote the formation of new bones. But with the
extension of MHD, the patients are prone to pineal body
calcification; and the greater the area of calcification is, the
less the MT will be secreted and the more easily the patient will
be prone to OP, suggesting that MT is negatively correlated with
OP. Inflammatory factors, such as TNF-α, IL-6 and IL-1, usually
exhibit the effect of promoting bone resorption and inhibiting bone
formation; in particular, TNF-α can induce the stromal cell
expression in osteoblasts and stimulate the osteoclast activation.
IL-1 can promote the osteoclast precursor cell proliferation and
differentiation and enhance the osteoclast activity, making the
bone resorption greater than bone formation and inducing OP
(19). When the oxidant-antioxidant
function is unbalanced in the body, it will inhibit the
differentiation of osteoblast precursor cells into osteoblasts,
inhibit the mineralization of osteoblasts and induce its death.
AOPP inhibits the proliferation and differentiation of
osteoblast-like cells through activating the NF-κB pathway.
Besides, MDA can inhibit the protein and nucleic acid synthesis and
decrease the enzyme activity, resulting in decreased antioxidant
substances in the body and thus gradually reducing the bone mass.
After OS stimulates the osteoclast growth and differentiation,
osteoclasts will in turn produce more ROS, exacerbate the damage to
the antioxidant defense mechanism in the body and form a vicious
circle, ultimately leading to extensive OP (20).
In conclusion, MHD patients are prone to OP, and
there are significant OS and inflammatory status; the MT level, OS
and inflammatory degree in patients are closely related to OP. The
clinical exploration of their relationship is of great significance
in reducing the incidence rate of OP in CRF patients receiving
MHD.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HR and RS detected bone mineral density and MT,
AOPP, MDA, TNF-α, IL-6 and IL-1 levels. JW performed thiobarbituric
acid assay. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Dezhoo People's Hospital (Dezhoo, China). Written informed consents
were signed by the patients and/or guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jeremiah MP, Unwin BK, Greenawald MH and
Casiano VE: Diagnosis and management of osteoporosis. Am Fam
Physician. 92:261–268. 2015.PubMed/NCBI
|
|
2
|
Shigematsu T, Muraoka R, Sugimoto T and
Nishizawa Y: Risedronate therapy in patients with mild-to-moderate
chronic kidney disease with osteoporosis: Post-hoc analysis of data
from the risedronate phase III clinical trials. BMC Nephrol.
18:662017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Del Vecchio L, Locatelli F and Carini M:
What we know about oxidative stress in patients with chronic kidney
disease on dialysis - clinical effects, potential treatment, and
prevention. Semin Dial. 24:56–64. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Oh DJ, Kim HR, Lee MK and Woo YS: Profile
of human β-defensins 1,2 and proinflammatory cytokines (TNF-α,
IL-6) in patients with chronic kidney disease. Kidney Blood Press
Res. 37:602–610. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang WL, Meng HZ, Yang RF, Yang MW, Sun
GH, Liu JH, Shi PX, Liu F and Yang B: Melatonin suppresses
autophagy in type 2 diabetic osteoporosis. Oncotarget.
7:52179–52194. 2016.PubMed/NCBI
|
|
6
|
Tanaka T, Latorre MRDO, Jaime PC, Florindo
AA, Pippa MG and Zerbini CA: Risk factors for proximal femur
osteoporosis in men aged 50 years or older. Osteoporos Int.
12:942–949. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cosman F, de Beur SJ, LeBoff MS, Lewiecki
EM, Tanner B, Randall S and Lindsay R: National Osteoporosis
Foundation: Clinician's guide to prevention and treatment of
osteoporosis. Osteoporos Int. 25:2359–2381. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arnao MB and Hernández-Ruiz J: Functions
of melatonin in plants: A review. J Pineal Res. 59:133–150. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pinto AR, da Silva NC and Pinato L:
Analyses of melatonin, cytokines, and sleep in chronic renal
failure. Sleep Breath. 20:339–344. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tocher DR, Mourente G, Van Der Eecken A,
Evjemo JO, Diaz E, Bell JG, Geurden I, Lavens P and Olsen Y:
Effects of dietary vitamin E on antioxidant defence mechanisms of
juvenile turbot (Scophthalmusmaximus L.), halibut
(Hippoglossushippoglossus L.) and sea bream (Sparusaurata
L.). Aquacult Nutr. 8:195–207. 2002. View Article : Google Scholar
|
|
11
|
Maes M, Ruckoanich P, Chang YS, Mahanonda
N and Berk M: Multiple aberrations in shared inflammatory and
oxidative & nitrosative stress (IO&NS) pathways explain the
co-association of depression and cardiovascular disorder (CVD), and
the increased risk for CVD and due mortality in depressed patients.
Prog Neuropsychopharmacol Biol Psychiatry. 35:769–783. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tang X, Rong G, Bu Y, Zhang S, Zhang M,
Zhang J and Liang X: Advanced oxidation protein products induce
hypertrophy and epithelial-to-mesenchymal transition in human
proximal tubular cells through induction of endoplasmic reticulum
stress. Cell Physiol Biochem. 35:816–828. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhao XQ, Liang B, Liu Y and Huang XQ:
Agaricoglycerides protect against hepatic ischemia/reperfusion
injury by attenuating inflammatory response, oxidative stress, and
expression of NF-κB. Evid Based Complement Alternat Med.
2015:1427362015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Izadyar S, Golbarg S, Takavar A and
Zakariaee SS: The effect of the lumbar vertebral malpositioning on
bone mineral density measurements of the lumbar spine by
dual-energy X-ray absorptiometry. J Clin Densitom. 19:277–281.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Norouzi J, Yadollahpour A, Mirbagheri SA,
Mazdeh MM and Hosseini SA: Predicting renal failure progression in
chronic kidney disease using integrated intelligent fuzzy expert
system. Comput Math Methods Med. 2016:60808142016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pedersen BK and Febbraio M: Exercise and
interleukin-6 action. Expert Rev Endocrinol Metab. 1:319–321. 2014.
View Article : Google Scholar
|
|
17
|
Yang L, Zhang J and Wang G: The effect of
sodium hyaluronate treating knee osteoarthritis on synovial fluid
interleukin-1β and clinical treatment mechanism. Pak J Pharm Sci.
28 Suppl 1:407–410. 2015.PubMed/NCBI
|
|
18
|
Yoo YM, Han TY and Kim HS: Melatonin
suppresses autophagy induced by clinostat in preosteoblast MC3T3-E1
cells. Int J Mol Sci. 17:5262016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zong Y, Chen J, Guo J-Z, Zhang X-J, Zhang
T-J and Sun L: Resveratrol inhibits lipopolysaccharide-induced
activation of osteoclast precursor Raw 264.7 cells. Acta Anatomica
Sinica. 46:51–56. 2015.doi:
10.16098/j.issn.0529-1356.2015.01.009.
|
|
20
|
Nurdiana N, Mariati N, Noorhamdani N,
Setiawan B, Budhiparama N and Noor Z: Effects of Labisia
pumila, on oxidative stress in rat model of post-menopausal
osteoporosis. Asian Pac J Reprod. 5:391–394. 2016. View Article : Google Scholar
|