Introduction
Palmar and foot hyperhidrosis is a common disease
caused by excessive activation of the sympathetic nervous system
leading to autonomic excessive secretion of head and facial sweat
glands thus resulting in the increased sweating (1). The incidence rate of palmar and foot
hyperhidrosis is approximately 1.0% in the Western countries. The
epidemiological investigation in China displays that the incidence
rate is approximately 4.6% in college and secondary school students
in Fuzhou.
The corresponding symptoms generally can be found
during the elementary school period among patients with palmar and
foot hyperhidrosis. Although the disease cannot affect the health
and longevity of patients, it causes inconvenience to their work,
study and social life, and have a greater impact on their quality
of life (2,3). The therapies of palmar and foot
hyperhidrosis include internal medicine and surgery. The effect of
drug therapy is poor, with greater side effects, and the long-term
use is easy to produce immune tolerance, and relapse easily occurs
once the drug is discontinued (4).
In the 1980s, the clinical application of thoracoscope contributed
to the rapid development of the minimally invasive surgery of
palmar and foot hyperhidrosis. It has the advantages of small
trauma, quick recovery and remarkable curative effect (5).
Minimally invasive surgery was conducted in patients
with palmar and foot hyperhidrosis in this study and obtained
satisfactory curative effect.
Materials and methods
General information
Seventy-six patients with palmar and foot
hyperhidrosis admitted to Yunnan University Hospital from August
2014 to July 2016 were selected and randomly divided into control
group (n=38) and observation group (n=38) using the random number
table. Inclusion criteria: i) Patients met the diagnostic criteria
of primary hyperhidrosis; ii) patients with main clinical symptoms
of much palmar and foot sweating, lasting more than six months,
over more than once every week; iii) patients with hyperhidrosis
affecting daily activities; and iv) patients signed the inform
consent. Exclusion criteria: i) Patients with severe heart, brain,
liver or psychiatric disorders; and ii) patients with severe
coagulation disorders and drug allergy to the drug. The differences
in general data of patients in two groups were not statistically
significant (P>0.05) (Table I).
The study was approved by the Ethics Committee of Sun Yat-Sen
University (Guangdong, China).
 | Table I.General data of objects of study. |
Table I.
General data of objects of study.
| Characteristics | Control group
(n=38) | Observation group
(n=38) | t/χ2
value | P-value |
|---|
| Sex
(male/female) | 24/14 | 26/12 | 0.234 | 0.629 |
| Age (year old) | 18–40 | 18–45 |
|
|
| Average age (year
old) | 25.36±5.63 | 25.85±5.73 | 0.376 | 0.708 |
| Duration of illness
(year) | 11.62±2.46 | 11.25±2.37 | 0.668 | 0.506 |
| BMI
(kg/m2) | 23.43±3.27 | 22.87±3.58 | 0.712 | 0.479 |
| Severe degree (n,
%) |
|
|
|
|
| Mild | 4
(10.52) | 3 (7.89) | 0.001 | 0.999 |
|
Moderate | 16 (42.11) | 19 (50.00) | 0.211 | 0.645 |
|
Severe | 18 (47.37) | 16 (42.11) | 0.053 | 0.818 |
Drug therapy
Drug therapy was used in the control group. Before
treatment, patients underwent a general physical examination.
Patients with a history of drug allergy were excluded, and the
range of sweating was measured by the iodine-starch test. Twenty
injection sites were designed at each side of the hands and feet
(1.0 cm apart). Botulinum toxin type A (100 units) was diluted
using 3 ml sodium chloride solution, and subcutaneous injection was
conducted according to the designed injection sites (the amount of
injection at each injection site was approximately 2.5 units).
Attention was paid that the needle was not too deep to prevent the
weakening of muscle strength during injection. The condition of
patients was closely observed for approximately 30 min after
injection to prevent the occurrence of drug allergy.
Surgical therapy
Patients in the observation group underwent
laparoscopic thoracic-4 sympathetic chain combined with thoracic-3
branch amputation. Before operation, chest X-ray, electrocardiogram
and blood test and urine routine examination were performed to
confirm the indication of operation. General anesthesia was
performed with intravenous compound single-lumen endotracheal
intubation. The patient was in a semi-supine position, with the
upper arms reaching approximately 90 degrees to fully expose the
bilateral armpits. The sequence of operation was followed by first
right and then left. The incision was performed through the third
intercostal space (approximately 1 cm length of incision), followed
by placement of needle sleeve (Trocar). By adopting single-hole
double-channel video thoracoscope, electric coagulation hook was
placed. Through the observation by thoracoscope, the location of R3
(the third rib surface sympathetic ganglia) and R4 (the fourth rib
surfaces) were determined. An electric coagulation hook was used to
cut off the R4 trunk and perform repeated cauterization to ensure
complete separation of the nerve stoma; subsequently, approximately
2 cm length was cut along the rib surface to the outside, so as to
observe the existence of collateral fibers, and to ensure the
amputation. R3 trunk outside was observed for any collateral
fibers. If existing, the electric coagulation would break it, and
the incision approximately 1.5 cm in length was foreseeingly made
to outside, and if it was completely burned was observed, avoiding
the damage to the trunk of R3. At the end of the operation, whether
active bleeding was observed, and whether the bilateral hands were
dry and warm was determined. After the observation by thoracoscope
displayed the swell of lungs, endoscope was withdrawn, annular
tubes were extracted and the incision was sutured. If the hands and
feet were still cold and damp, the complete disconnection of broken
ends and collateral branches of sympathetic nerve should be
examined again before the withdrawal of the endoscope.
Index detection
Fasting venous blood (3–5 ml) was collected from
patients in the two groups before and at one week after treatment,
followed by separation and extraction of serum. The levels of serum
C-reactive protein (CRP), interleukin-6 (IL-6), IL-10 and tumor
necrosis factor-α (TNF-α) in patients were measured by
enzyme-linked immunosorbent assay (ELISA), and related kits were
provided by Zhejiang Ikon Co., Ltd., Zhejiang, China. The
operations were performed strictly according to the instructions.
The optical density (OD) value was read at 450 nm of wavelength by
a microplate reader (Jiangsu Potebio Co., Ltd., Jiangsu, China),
followed by calculation of levels of CRP, IL-6, IL-10 and TNF-α.
The levels of immunoglobulin G (IgG), IgA and IgM in patients were
detected by immunoturbidimetry, and related kits were provided by
Shanghai Yanjin Biotechnology Co., Ltd., Shanghai, China. The
operations were strictly performed according to the instructions.
The contents of IgG, IgA and IgM in the sample were calculated by
measuring turbidity of reaction liquid and comparing with standard
samples.
Follow-up
After treatment, follow-up was conducted by
outpatient, telephone, network and other methods for 6 months, so
as to understand the improvement and recurrence of the primary
sweating site and assess the quality of life.
Evaluation criteria
Criteria for judging the severity of palmar and foot
hyperhidrosis: a) mild, it was moist when sweating; b) moderate,
sweating soaked a handkerchief; c) severe, sweat dropped as beads
of sweat.
The curative effect was evaluated, and the criteria
were as follows: a) cured, after 3 months of treatment, hands and
feet were warm and dry, with no moisture and sweat in the quiet
state and suitable room temperature; b) effective, after treatment,
the wet and sweating conditions of hand and foot were improved
significantly, with slight sweating under normal conditions; c)
ineffective, after 3 months of treatment, severe sweating occurred
in patients or sweating did not improve significantly compared with
that before treatment. Therapeutic total effective rate = cure rate
+ effective rate.
Fasting venous blood (5 ml) was collected from
patients in the morning before and at one week after treatment,
followed by separation and extraction of serum and stored at −20°C.
The levels of serum CRP, IL-6, IL-10 and TNF-α in patients were
measured by ELISA before treatment and at one week after treatment.
The levels of immunoglobulin IgG, IgA and IgM were detected by
immunoturbidimetry.
The quality-of-life index (iQOL) was used to assess
the quality of life in patients before and after treatment
(6). According to the impact of
disease on the quality of life in patients, the severity was
divided into 0–3 points (0 point indicates no impact on quality of
life; 3 points indicate a serious impact on quality of life), and
the score was negatively related to the quality of life of
patients.
Statistical analysis
Data were processed by SPSS 19.0 (SPSS Inc.,
Chicago, IL, USA) software. Measurement data were expressed by mean
± standard deviation, and t-test was adopted. Count data were
expressed by percentage, and Chi-square test was utilized. The rank
sum test was used for curative effect. P<0.05 was considered to
indicate a statistically significant difference.
Results
Three months later, the therapeutic effective rate
in the observation group was 94.74%, which was significantly higher
than 73.23% in the control group, and the difference was
statistically significant (P<0.05) (Table II).
 | Table II.Comparison of curative effect in
patients of the two groups (n, %). |
Table II.
Comparison of curative effect in
patients of the two groups (n, %).
| Group | N | Cured | Effective | Ineffective | Totally
effective |
|---|
| Observation | 38 | 27 (71.05) | 9
(23.68) | 2 (5.26) | 6
(94.74) |
| Control | 38 | 12 (31.58) | 16 (42.11) | 10 (26.32) | 18 (73.23) |
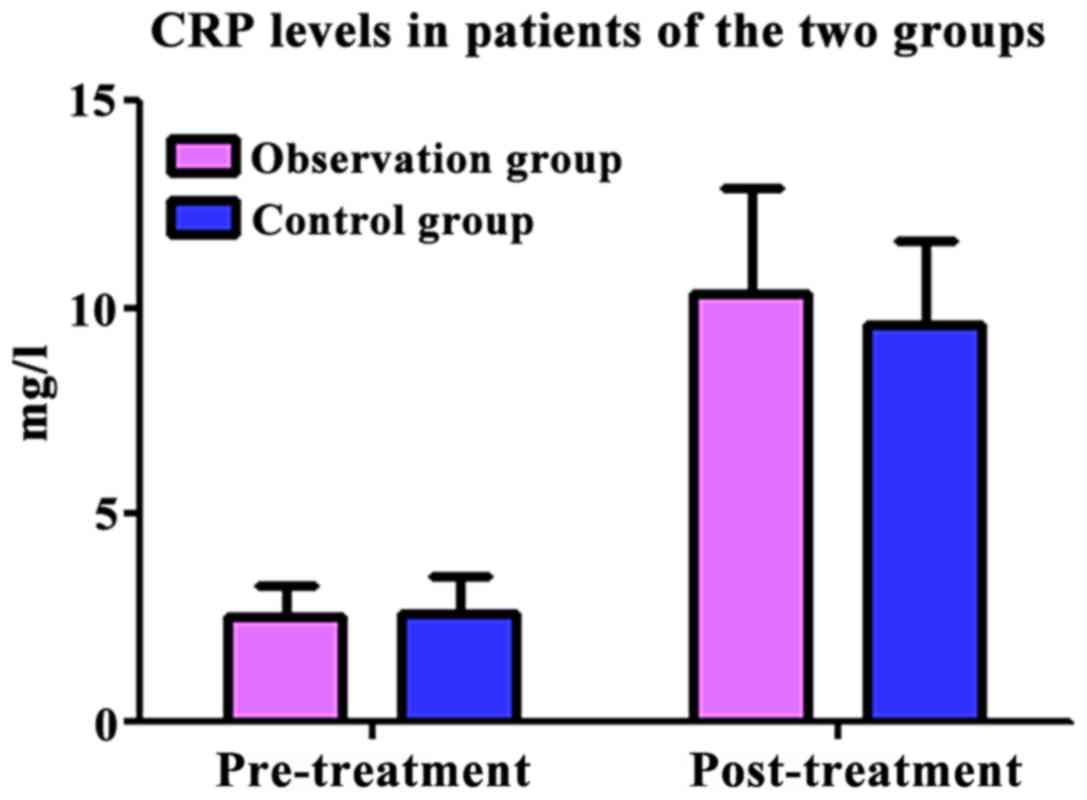
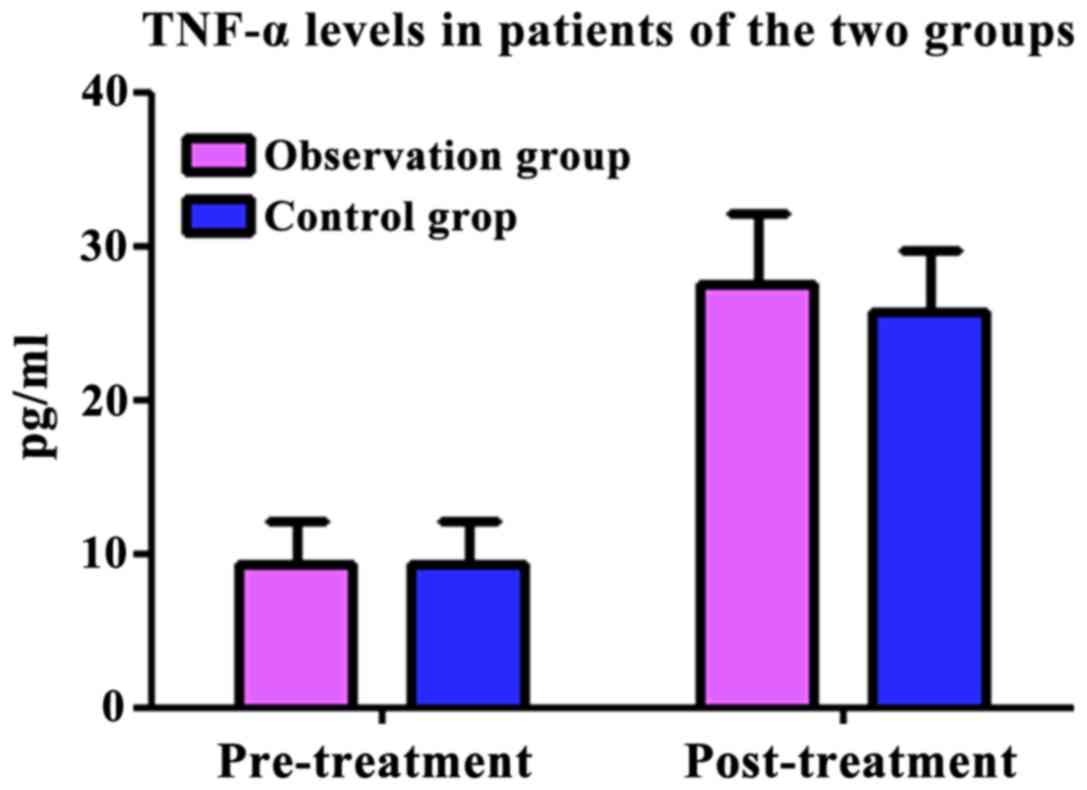
Comparisons of levels of CRP, IL-6,
IL-10 and TNF-α in the patients of the two groups
Before treatment and at one week after treatment,
CRP levels in observation group were 2.57±0.24, 10.37±1.23 mg/l;
IL-6 levels were 6.43±4.24, 31.67±3.23 pg/ml; IL-10 levels were
8.43±2.24, 15.37±3.23 pg/ml; and TNF-α levels were 9.43±5.24,
27.67±3.23 pg/ml. Before treatment and at one week after treatment,
CRP levels in observation group were 2.65±0.35, 9.63±2.15 mg/l;
IL-6 levels were 17.24±4.36, 29.58±3.74 pg/ml; IL-10 levels were
8.68±2.58, 13.67±3.23 pg/ml; TNF-α levels were 9.36±5.17,
25.85±4.43 pg/ml. The serum levels of CRP, IL-6, IL-10 and TNF-α in
the patients of the two groups after treatment were increased
compared with those before treatment (P<0.05). There were no
statistically significant differences in patients between two
groups (P>0.05) (Figs. 1–4).
Comparisons of immunological indexes
in patients of the two groups
After treatment for one week, IgG, IgM and IgA in
patients of the two groups were obviously increased (P<0.05).
The differences were not statistically significant in patients
between two groups (P>0.05) (Table
III).
 | Table III.Comparisons of immunological indexes
in patients of the two groups (g/l). |
Table III.
Comparisons of immunological indexes
in patients of the two groups (g/l).
|
| IgA |
|
| IgG |
|
| IgM |
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Group | Before treatment | After treatment | t-value | P-value | Before treatment | After treatment | t-value | P-value | Before treatment | After treatment | t-value | P-value |
|---|
| Observation | 1.03±0.26 | 1.69±0.45 | 7.828 | <0.001 | 5.15±1.63 | 9.05±2.67 | 7.685 | <0.001 | 1.15±0.43 | 1.83±0.36 | 7.475 | <0.001 |
| Control | 1.04±0.27 | 1.67±0.34 | 8.945 | <0.001 | 5.17±1.45 | 9.07±2.42 | 8.522 | <0.001 | 1.17±0.35 | 1.88±0.47 | 7.469 | <0.001 |
| t-value | 0.164 | 0.219 |
|
| 0.057 | 0.034 |
|
| 0.222 | 0.521 |
|
|
|---|
| P-value | 0.870 | 0.827 |
|
| 0.955 | 0.973 |
|
| 0.825 | 0.604 |
|
|
|---|
Comparisons of quality of life in
patients of the two groups
Through the follow-up for six months, it could be
seen that iQOL scores in patients of the two groups were remarkably
decreased, which was more significant in observation group
(P<0.05) (Table IV).
 | Table IV.iQOL in patients of the two
groups. |
Table IV.
iQOL in patients of the two
groups.
|
|
| iQQL score |
|
|
|---|
|
|
|
|
|
|
|---|
| Group | Case | Before treatment | After treatment | t-value | P-value |
|---|
| Observation | 38 | 2.36±0.32 | 0.41±0.12 | 35.173 | <0.001 |
| Control | 38 | 2.35±0.33 | 1.18±0.87 |
7.751 | <0.001 |
| t-value |
| 0.134 | 5.405 |
|
|
| P-value |
| 0.894 | <0.001 |
|
|
Discussion
The pathogenesis of palmar and foot hyperhidrosis is
not yet entirely clear, and anxiety, stress and hot weather all
contribute to this disease. Most studies suggest that it is closely
related to the overactivity of sympathetic nerve (7). The secretion of sweat glands in the
human body is governed by sympathetic nerves, and the sympathetic
nerve chain belongs to the autonomic nervous system, which consists
of sympathetic ganglia and intersegmental branches, and is
symmetrically distributed on both sides of the human spine
(8). The sympathetic nerve, which
usually controls the sweat glands of hands and feet, is located at
the levels of thoracic-2 to the thoracic-6 spinal segments and
controls the sweat glands by releasing acetylcholine (9). Studies have revealed that sympathetic
nerve fiber myelin sheath is thickened in patients with palmar and
foot hyperhidrosis than that in normal people, thus accelerating
the speed of sympathetic nerve conduction, so the excitability in
patients stimulated by nervousness, excitement, stress and fever in
the waking state will be enlarged, thereby increasing the sweat
secreted by sweat glands; palmar and foot hyperhidrosis usually
occurs during the young period or adolescence, which will continue
to exist for life; it has a strong heredity with genetic
probability in 30–40% (10,11).
Palmar and foot hyperhidrosis can be treated by
medication and surgery; therein, medication includes topical
medication, oral medication, direct current, iontophoresis and
botulinum toxin injection (12).
Commonly used drugs are anticholinergic agents that inhibit the
action of sweat glands by competing against acetylcholine
muscarinic receptors, reducing the amount of perspiration thus
treating them. However, it has many side effects such as intestinal
reaction, elevated intraocular pressure, dry mouth, blood pressure
drop and tachycardia. Surgical treatment is usually performed by
sympathectomy currently, thus inhibiting the excessive secretion of
sweat glands (13). The results of
this study displayed that the therapeutic effective rate in the
observation group was 94.74%, which was significantly higher than
73.23% in the control group, and the difference was statistically
significant (P<0.05). The reason is that botulinum toxin type A
can inhibit acetylcholine releasing from presynaptic nerve
terminals through acting on cholinergic nerve endings, thus
inhibiting the secretion of sweat gland; however, long-term
injection is prone to induce immune tolerance, pain of injection
site and amyasthenia in patients; although they can be treated in
the short-term, the disease easily relapses, which shows an
uncertain long-term curative effect (14). The conduction of sympathetic nerve
can be effectively blocked through burning corresponding
sympathetic segment and extending to the outside, namely
thoracoscopic thoracic-4 sympathetic nerve chain combined with
thoracic-3 branch amputation, thus inhibiting sweat glands; once
treated, it is difficult to relapse, and it has certain long-term
curative effect, smaller incision of minimally invasive surgery,
not obvious postoperative scar and higher satisfaction in patients
(15).
Surgical trauma, combined with anesthesia and other
stress reactions will inhibit the immune function and easily
induces immune dysfunction, accompanied by inflammatory responses,
thus leading to postoperative infection, which is not conducive to
postoperative recovery of patients. CRP is an acute-phase reactive
protein with high sensitivity. It can play a regulatory role by
stimulating cell activation, which is commonly utilized as a marker
of trauma and inflammation in the clinical practice. When the
organism is damaged or has a bacterial infection, the concentration
of CRP increases obviously (16–18).
IL-6 is an important member of the interleukin family and plays a
diverse role in the body's immune response and apoptosis (19). IL-10 can inhibit the secretion of a
variety of proinflammatory cytokines, and the upregulation of its
level can make the body into a highly reactive state of humoral
immunity (20). As a polypeptide
cytokine, TNF-α can synergistically interact with inflammatory
mediators such as IL-6 and IL-10, which is an important cytokine
mediating injury and infection; it is closely related to host
defense function (21). The results
of this study displayed that the serum levels of CRP, IL-6, IL-10
and TNF-α in patients of the two groups were higher at one week
after treatment than those before treatment (P<0.05), and there
were no significant differences between the two groups (P>0.05).
The reason is that multi point injection therapy makes stronger
sense of pain in patients, and the stress reaction can lead to
abnormally increased secretion of serum cytokines; especially, the
surgical treatment is more likely to cause inflammatory reaction
after operation, so CRP, IL-6, IL-10 and TNF-α levels were
increased compared with those before treatment. Minimally invasive
surgery utilized in observation group can reduce the use of
surgical instruments, plus the reduction of surgical incision
length, so that the trauma is less. During the operation, the nerve
was cut off by electric coagulation under direct vision using
thoracoscope, and no drainage was performed after the operation, so
as to reduce the stress reaction compared with routine surgery in
patients and effectively decrease the occurrence of infection.
Patients recovered usually at approximately one week after
operation, fully demonstrating the concept of minimally invasive
surgery.
After treatment for one week, IgG, IgM and IgA in
patients of the two groups were obviously increased (P<0.05),
and the differences in patients between two groups were not
statistically significant (P>0.05). The reason is that humoral
immunity in normal human will remain at a low level; the body
affected by trauma will produce slight infection, while self-immune
regulation occurs in the body, thus increasing the immunoglobulin
IgG, IgM and IgA levels and enhancing the ability of resistance.
Thoracoscopic sympathectomy has advantages of more accurate
positioning, minimally invasive processing and safety, which causes
less injury to normal immune function of the body, and it has
little influence on the normal increase of postoperative
immunoglobulin IgG, IgM and IgA levels in patients, which is
conducive to the rapid recovery in patients after operation.
In summary, minimally invasive surgery adopted to
treat palmar and foot hyperhidrosis has more significant effect
compared with drug therapy. It causes slight postoperative
inflammatory reaction and has less influence on the immune function
of patients, and it can also improve the quality of life in
patients. Thus, it is the ideal method for the treatment of palmar
and foot hyperhidrosis, which is worthy of clinical
application.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WXL collected, analyzed and interpreted the patients
data. YKL contributed to the conception and design of the study.
HTL wrote, revised the manuscript for important intellectual
content. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Sun Yat-Sen University (Guangzhou, China). Patients provided
written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siah TW and Hampton PJ: The effectiveness
of tap water iontophoresis for palmoplantar hyperhidrosis using a
Monday, Wednesday, and Friday treatment regime. Dermatol Online J.
19:142013.PubMed/NCBI
|
|
2
|
Hougaard MG and Thyssen JP: Treatment of
hand eczema caused by hyperhidrosisTextbook of Hand Eczema. Alikhan
A, Lachapelle JM and Maibach H: Springer; Berlin, Heidelberg: pp.
361–370. 2014, View Article : Google Scholar
|
|
3
|
Ak M, Dinçer D, Haciomeroglu B, Akarsu S,
Lapsekili N and Ada S: The evaluation of primary idiopathic focal
hyperhidrosis patients in terms of alexithymia. J Health Psychol.
18:704–710. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yanagishita T, Tamada Y, Ohshima Y, Ito K,
Akita Y and Watanabe D: Histological localization of aluminum in
topical aluminum chloride treatment for palmar hyperhidrosis. J
Dermatol Sci. 67:69–71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rieger R, Loureiro MP, Pedevilla S and de
Oliveira RA: Endoscopic lumbar sympathectomy following thoracic
sympathectomy in patients with palmoplantar hyperhidrosis. World J
Surg. 35:49–53. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Inoue M, Yokoyama T, Ishii A, Watanabe T,
Yamato T and Kumon H: The effect of hochuekkito on female stress
urinary incontinence. Kampo Med. 61:853–855. 2010. View Article : Google Scholar
|
|
7
|
Inukai YS, Iwase S, Shimizu Y and Sato M,
Nishimura N, Onizuka C, Kuwahara Y, Sugenoya J and Sato M:
Pathogenesis of the hemifacial hyperhidrosis. J Neurol Sci.
333:e712–e713. 2013. View Article : Google Scholar
|
|
8
|
Weitz G, Elam M, Born J, Fehm HL and Dodt
C: Postmenopausal estrogen administration suppresses muscle
sympathetic nerve activity. J Clin Endocrinol Metab. 86:344–348.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nedvetsky PI, Emmerson E, Finley JK,
Ettinger A, Cruz-Pacheco N, Prochazka J, Haddox CL, Northrup E,
Hodges C, Mostov KE, et al: Parasympathetic innervation regulates
tubulogenesis in the developing salivary gland. Dev Cell.
30:449–462. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cerfolio RJ, De Campos JR, Bryant AS,
Connery CP, Miller DL, DeCamp MM, McKenna RJ and Krasna MJ: The
Society of Thoracic Surgeons expert consensus for the surgical
treatment of hyperhidrosis. Ann Thorac Surg. 91:1642–1648. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wolosker N, Schvartsman C, Krutman M,
Campbell TP, Kauffman P, de Campos JR and Puech-Leão P: Efficacy
and quality of life outcomes of oxybutynin for treating palmar
hyperhidrosis in children younger than 14 years old. Pediatr
Dermatol. 31:48–53. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bovell DL, MacDonald A, Meyer BA, Corbett
AD, MacLaren WM, Holmes SL and Harker M: The secretory clear cell
of the eccrine sweat gland as the probable source of excess sweat
production in hyperhidrosis. Exp Dermatol. 20:1017–1020. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yuncu G, Turk F, Ozturk G and Atinkaya C:
Comparison of only T3 and T3-T4 sympathectomy for axillary
hyperhidrosis regarding treatment effect and compensatory sweating.
Interact Cardiovasc Thorac Surg. 17:263–267. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mazzocchio R and Caleo M: More than at the
neuromuscular synapse: Actions of botulinum neurotoxin A in the
central nervous system. Neuroscientist. 21:44–61. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang Y, Zeng L, An Z, Wang L and Hu J:
Minimally invasive thoracic sympathectomy for palmar hyperhidrosis
via a single unilateral incision approach by the pleura videoscope.
J Laparoendosc Adv Surg Tech A. 24:328–332. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nishiofuku H, Tanaka T, Marugami N, Sho M,
Akahori T, Nakajima Y and Kichikawa K: Increased tumour ADC value
during chemotherapy predicts improved survival in unresectable
pancreatic cancer. Eur Radiol. 26:1835–1842. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Qin CF and Zhao FL: Long non-coding RNA
TUG1 can promote proliferation and migration of pancreatic cancer
via EMT pathway. Eur Rev Med Pharmacol Sci. 21:2377–2384.
2017.PubMed/NCBI
|
|
18
|
Christensen MB, Eriksen T and
Kjelgaard-Hansen M: C-reactive protein: quantitative marker of
surgical trauma and post-surgical complications in dogs: a
systematic review. Acta Vet Scand. 57:712015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mauer J, Chaurasia B, Goldau J, Vogt MC,
Ruud J, Nguyen KD, Theurich S, Hausen AC, Schmitz J, Brönneke HS,
et al: Signaling by IL-6 promotes alternative activation of
macrophages to limit endotoxemia and obesity-associated resistance
to insulin. Nat Immunol. 15:423–430. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zigmond E, Bernshtein B, Friedlander G,
Walker CR, Yona S, Kim KW, Brenner O, Krauthgamer R, Varol C,
Müller W, et al: Macrophage-restricted interleukin-10 receptor
deficiency, but not IL-10 deficiency, causes severe spontaneous
colitis. Immunity. 40:720–733. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
DeBerge MP, Ely KH and Enelow RI: Soluble,
but not transmembrane, TNF-α is required during influenza infection
to limit the magnitude of immune responses and the extent of
immunopathology. J Immunol. 192:5839–5851. 2014. View Article : Google Scholar : PubMed/NCBI
|