Introduction
Vitiligo, an acquired, idiopathic disorder, is a
long-term skin disease featuring melanocytic destruction and
depigmented maculae and/or patches in the skin. The patches of
affected skin become white and usually have sharp margins (1,2). The
incidence of vitiligo is 0.1–2% worldwide (3) and may be as high as 2–3% in certain
populations, while females and males are equally affected (4,5). The
pathogenesis of vitiligo has remained to be fully elucidated but
appears to be associated with the interaction of genetic
susceptibility as well as neurological and immunological risk
factors (6,7). The course of vitiligo is unpredictable
but is often progressive, which may have a severe impact on the
quality of life of patients and result in marked emotional stress
(8,9). Several treatments are available for
vitiligo patients, including applied steroids, ultraviolet light
and phototherapy (10,11). Due to the large body surface area
affected, patients with extensive depigmentation may receive
treatment with phototherapy, including ultraviolet A radiation,
narrowband ultra-violet B radiation (NBUVB) and excimer laser
(12–14).
The 308-nm excimer laser is a relatively novel
treatment option, which has been reported to increase the precision
and the capability of delivering higher-energy fluencies to the
lesions in less time without affecting uninvolved skin (15,16). Of
note, the wavelengths of the excimer laser and NBUVB are in close
proximity (308 and 311 nm, respectively), indicating similar
therapeutic effects (17); however,
several studies demonstrated that in adult as well as in pediatric
vitiligo patients, the effectiveness and safety of 308-nm excimer
laser phototherapy are well established, with safety likely
superior to that of NBUVB phototherapy (18–20),
which may be explained by the ability of the excimer laser to emit
coherent short pulses, as well as differences in phototherapeutic
parameters, such as impulse frequency and intensity, thereby
stimulating a deeper reservoir of melanocytes in hair follicles
(17). Tacrolimus, a macrolide
immunosuppressant from the fungus Streptomyces tsukubaensis,
is a novel treatment for vitiligo (21). Recent studies have demonstrated that
combination therapy with the 308-nm excimer laser and topical
tacrolimus is more effective than either treatment alone (22,23).
As is known, digital imaging is a useful method for
assessing vitiligo (24). Compared
with conventional clinical digital imaging, dermoscopy, a
non-invasive skin imaging technique, facilitates the visualization
of the subsurface structures of the skin using optical
magnification, liquid immersion or cross-polarized lighting
(25). In addition, dermoscopy
allows for visualization of morphological structures of the
epidermis, which may improve the analysis of the
clinicopathological features of pigmented skin lesions (26). A previous study indicated that
dermoscopy had 89.6% sensitivity for malignant lesions (tested on
68 melanomas and 9 pigmented basal cell carcinomas) compared with
69.7% sensitivity by the observation using the naked eye (27). However, due to the complexity of
patterns and interpretation, dermoscopy examination results also
have limitations (25). In the
present study, an analysis to assess the effectiveness of
dermoscopy in evaluating the therapeutic efficacy of combination
therapy with tacrolimus ointment and 308-nm excimer laser in
vitiligo patients was performed.
Materials and methods
Study subjects
Between October 2015 and October 2016, 147 eligible
patients treated at Dong Guan People's Hospital (Dongguan, China)
were enrolled as study subjects. All patients were diagnosed with
localized vitiligo based on the diagnostic criteria of chloasma and
vitiligo established by the Pigmented Dermatosis Group of the
Dermatosis Committee of the China Society of Integrated Traditional
Chinese and Western Medicine in 2010 (28). Of the 147 patients, 87 were male and
60 were female; the age of the patients ranged from 4 to 58 years
(average age, 32.11±16.26 years), and the course of the disease
ranged from 2 weeks to 10 years. A total of 92 vitiligo patients
were in the progressive stage (57 males and 35 females; age range,
4–56 years; average age, 29.34±12.07 years), and the vitiliginous
areas covered 0.6–10% of the body surface (average, 5.37±2.08%).
The other 55 vitiligo patients were in the stable stage (30 males
and 25 females; age range, 7–58 years; average age, 31.98±16.77
years), and the vitiliginous areas covered 2.7–9% of the body
surface (average, 5.25±1.73%). Vitiliginous areas were mainly
present on the face, neck and torso. Among the 92 progressive-stage
patients, vitiliginous areas were present on the face in 33, on the
neck in 18 and on the torso in 41. Among the 55 stable-stage
patients, vitiliginous areas were present on the face in 18, on the
neck in 13 and on the torso in 24. No significant differences in
age, sex, proportion of vitiliginous area or the location of
vitiliginous areas were observed between the progressive-stage and
stable-stage patients (all P>0.05; Table I). Stable vitiligo was defined as
static lesions of vitiligo without any new lesions or extension of
previously existing lesions occurring over the past six months. By
contrast, progressive vitiligo was defined as the recent appearance
of new lesions or enlargement of existing lesions. Patients
selected for inclusion had localized vitiligo and a vitiliginous
area of <10% of the body surface. Patients were excluded if they
had: i) Segmental or generalized vitiligo; ii) skin lesions
combined with other skin diseases, or scar diathesis; iii) poor
compliance or a history of allergy to ultraviolet rays or
tacrolimus; iv) heart, liver or kidney photosensitization, or
autoimmune diseases; v) a history of cataract or glaucoma; vi) had
received any systemic or local therapy over the past 2 months; or
vii) were pregnant or lactating if females. All subjects or their
family members signed an informed consent form including
publication of the data and figures, and the experiment was
performed with the approval of the ethics committee of Dong Guan
People's Hospital (Dongguan, China).
 | Table I.Comparison of general data between
patients with progressive-stage and stable-period vitiligo at
baseline. |
Table I.
Comparison of general data between
patients with progressive-stage and stable-period vitiligo at
baseline.
| Parameter | Progressive stage
(n=92) | Stable period
(n=55) |
χ2/t | P-value |
|---|
| Sex |
|
| 0.783 | 0.376 |
|
Male | 57 (61.96) | 30 (54.55) |
|
|
|
Female | 35 (38.04) | 25 (45.45) |
|
|
| Age (years) | 32.18±16.05
(3–56) | 31.98±16.77
(5–58) | 0.072 | 0.943 |
| Vitiliginous area
(%) | 5.37±2.08
(0.5–10) | 5.25±1.73
(2.5–9) | 0.569 | 0.572 |
| Location of
vitiliginous areas |
|
| 0.375 | 0.829 |
|
Face | 33 (35.86) | 18 (32.73) |
|
|
|
Neck | 18 (19.57) | 13 (23.64) |
|
|
|
Torso | 41 (44.57) | 24 (43.63) |
|
|
Treatment schedule
All patients received laser therapy twice weekly
combined with external tacrolimus ointment twice daily for 12
weeks. The laser used was a 308-nm xenon chloride excimer laser
(HONKON-308VAL; Beijing Honkon Technologies Co., Ltd., Beijing,
China). The fixed technical variables were as follows: Laser wave
length, 308±2 nm; wave crest, 308 nm; single pulse energy, 3
mJ/cm2; pulse frequency, 200 Hz; power density, 50
mw/cm2; light output window of therapy area, 50×60,
30×50, 30×40 and 20×30 mm2; diameter of the spot sizes,
10 mm; and time of therapy, 1–99 sec. First, the minimal erythema
dose (MED) of each subject was assessed and a suitable light output
window was selected based on the lesion condition, with an initial
dose of 1–2 times the MED. Care was taken to avoid exposing normal
skin to the light output window. The initial dose was decreased by
1 MED for lesions in wrinkled skin and the area around the ankle
joint but increased by 1 MED for patients with normal, darker and
thicker skin. Each dose was increased by 15–25% of the previous
dose until the maximum safe dose for treatment was reached (3
J/cm2 for the head, face and neck and 4.5
J/cm2 for the torso). If local erythema persisted, the
dose was reduced 10–20% from the previous dose; if a painful
erythematous skin lesion or blister appeared, laser treatment was
discontinued one or two times. Tacrolimus ointment (0.1% for adults
or 0.03% for children; Astellas Pharma Tech, Toyama, Japan) was
applied and patients returned for visits once a week.
Dermoscopy monitoring
Dermoscopy was performed using an electron
microscope (Dr Camscope; Sometech Inc., Seoul, Korea) with a ×30
lens via the immersion dermoscopy method. Dermoscopy of skin
lesions of all patients was performed by skilled professional
personnel. For each patient, one vitiliginous area was selected to
observe the condition of the lesion and fully exposed lesions
underwent dermoscopy at the initial visit. To avoid omitting
detailed information on the lesions, the physician carefully
scanned and observed the lesions of the patients from top to bottom
and from left to right. After 4, 8 and 12 weeks of treatment,
dermoscopy of the same skin lesions was performed by the same
physician. The information on the observed lesions at the initial
visit of each patient was carefully recorded to ensure that
follow-up dermoscopy monitoring was performed in the same
vitiliginous area.
Assessment of efficacy and adverse
reactions
The therapeutic effect index was determined as
follows: i) Residual perifollicular pigmentation: The pilosebaceous
orifice in the vitiliginous areas and the surrounding
non-interrupted pigmentation had a homogeneous appearance with a
single diffuse distribution usually seen in peripheral lesions
compared with central lesions. Observation of one or multi-residual
perifollicular pigmentation areas by dermoscopy was evaluated as
‘yes’; by contrast, absence of residual perifollicular pigmentation
or observation of typical pigment residue was rated as ‘no’. ii)
Angiotelectasis: Punctate, linear or mesh angiotelectasis was
identified in skin lesions. iii) Early formation of pigmentation
islands: The occurrence of black and hair follicle pigmentary units
is difficult to observe with the naked eye, and mutual integration
of the two residual perifollicular pigmentations may indicate early
signs of recovery. Pigmentation islands contain two main forms, the
marginal type and the central type, which refer to the occurrence
of pigmentation islands in the normal skin at the edge of white
spots and at the center of white spots, respectively. iv)
Perilesional hyperpigmentation: Darker pigmentation was observed
around the skin lesions. The evaluation criteria for dermoscopy
efficacy were as follows: Dermoscopy images from the initial visit
were compared with those obtained after 4, 8 and 12 weeks of
treatment to evaluate the efficacy by referring to standards of
clinical efficacy with the naked eye. The standards of clinical
efficacy were examined by the naked eye (28): i) Fading away of all vitiligo and
return to normal skin color was regarded as a ‘cure’; ii) partial
fading or reduction of vitiliginous areas and return of >50% of
skin lesions to normal skin color was regarded as ‘effective’; iii)
partial fading or reduction of vitiliginous areas was regarded as
an ‘improvement’; iv) no pigment regeneration in vitiliginous areas
or larger vitiliginous areas was regarded as ‘ineffective’. The
effective rate was determined as follows: Effective
rate=[(ncure+neffective)/ntotal]×100%,
and the efficacy was calculated as follows:
Efficacy=[(ncure+neffective+nimprovement)/ntotal]×100%.
Statistical analysis
Data were evaluated by SPSS 22.0 software (IBM
Corp., Armonk, NY, USA). Differences in measurement data between
groups were compared with Student's t-test, and comparison of the
effective rate and further parameters between the two groups was
performed using the χ2 test. Binary logistic regression
analysis identified risk factors associated with the combination
therapy of tacrolimus ointment with 308-nm excimer laser for
vitiligo patients. P<0.05 was considered to indicate a
statistically significant difference.
Results
Observation results for dermoscopy on
vitiligo patients in different stages
The observation results by dermoscopy revealed
characteristics of vitiligo skin lesions in 61 patients in the
progressive-stage group and 19 patients in the stable-stage group.
More progressive-stage patients than stable-stage patients had
residual perifollicular pigmentation (χ2=23.180,
P<0.001), while the presence of perilesional hyperpigmentation
was obviously lower in patients with progressive vitiligo than in
those with stable vitiligo (χ2=32.780, P<0.001). No
significant differences were observed in angiotelectasis or the
early formation of pigmentation islands between the progressive-
and stable-stage vitiligo patients (both P>0.05; Table II).
 | Table II.Dermoscopy observation results of
patients with progressive-stage and stable-period vitiligo at
baseline. |
Table II.
Dermoscopy observation results of
patients with progressive-stage and stable-period vitiligo at
baseline.
| Description of skin
lesions | Progressive stage
(n=92) | Stable period
(n=55) | χ2 | P-value |
|---|
| Residual
perifollicular pigmentation |
|
|
|
|
|
Yes | 56 (60.87) | 11 (20.00) | 23.180 | <0.001 |
| No | 36 (39.13) | 44 (80.00) |
|
|
|
Angiotelectasis |
|
|
|
|
|
Yes | 5 (5.43) | 2 (3.64) |
0.246 | 0.620 |
| No | 87 (94.57) | 53 (96.36) |
|
|
| Early formation of
pigmentation islands |
|
|
|
|
|
Yes | 2 (2.17) | 1 (1.82) |
0.022 | 0.883 |
| No | 90 (97.83) | 54 (98.18) |
|
|
| Perilesional
hyperpigmentation |
|
|
|
|
|
Yes | 1 (1.09) | 19 (34.55) | 32.780 | <0.001 |
| No | 91 (98.91) | 36 (65.45) |
|
|
Dermoscopy observation results of skin
lesions after combination therapy with tacrolimus ointment and
308-nm excimer laser
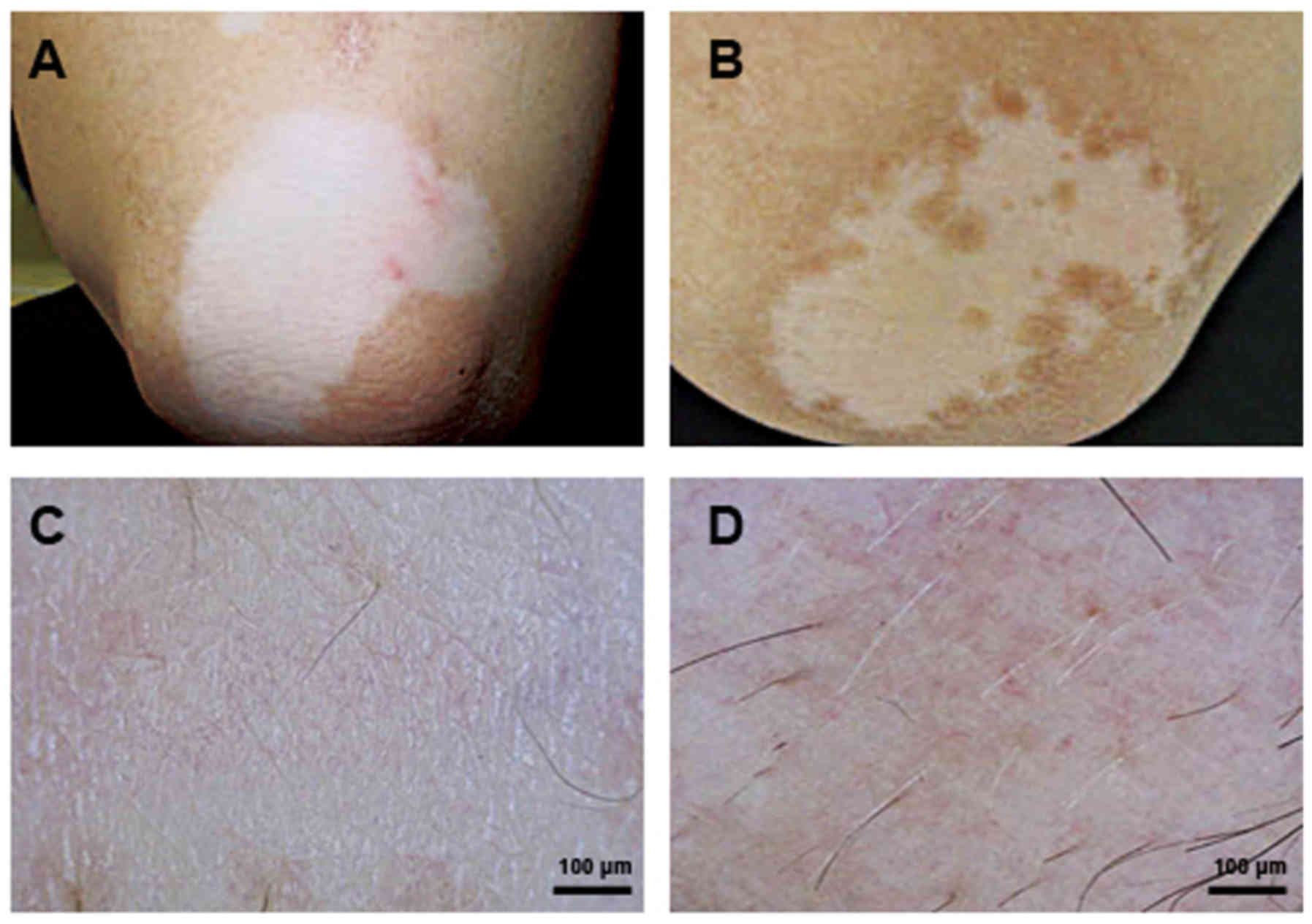
Fig. 1A and B display
representative the visual observation results for skin lesions in a
vitiligo patient at the initial visit and after 12 weeks of
combination therapy with tacrolimus ointment and 308-nm excimer
laser, and the dermoscopy results at the same time-points are
presented in Fig. 1C and D.
Perilesional hyperpigmentation, angiotelectasis and early
reservoirs of pigmentation may be considered as the most important
dermoscopic features of vitiligo.
In terms of patients treated with topical
tacrolimus, angiotelectasis was not observed on the face, but on
the body. After 4, 8 and 12 weeks of combination therapy, skin
lesions were found in 57, 36 and 26 patients with the progressive
vitiligo, and in 18, 12 and 11 cases with stable vitiligo,
respectively (Table III). After 4
weeks of combination therapy, the occurrence of residual
perifollicular pigmentation, angiotelectasis and early reservoirs
of pigmentation were significantly higher in the progressive-stage
vitiligo patients than in those in the stable stage (all
P<0.001). In addition, more patients in the progressive-stage
group had residual perifollicular pigmentation and angiotelectasis
than those in the stable-stage group after 8 weeks (all P<0.05).
Furthermore, at 12 weeks, a significant difference in the presence
of residual perifollicular pigmentation between the progressive-
and stable-stage patients was observed (P=0.025).
 | Table III.Dermoscopy observation results of
skin lesions after combination therapy with tacrolimus ointment and
308-nm excimer laser. |
Table III.
Dermoscopy observation results of
skin lesions after combination therapy with tacrolimus ointment and
308-nm excimer laser.
|
|
| 4 weeks | 8 weeks | 12 weeks |
|---|
|
|
|
|
|
|
|---|
| Description of skin
lesions | Results | Progressive
stage | Stable period | χ2 | P-value | Progressive
stage | Stable period | χ2 | P-value | Progressive
stage | Stable period | χ2 | P-value |
|---|
| Residual
perifollicular pigmentation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
| 55 (59.78) | 11 (20.00) | 22.020 | <0.001 | 33 (35.87) | 8 (14.55) | 7.783 | 0.005 | 22 (23.91) | 5 (9.09) | 5.044 | 0.025 |
| No |
| 37 (40.22) | 44 (80.00) |
|
| 59 (64.13) | 47 (85.45) |
|
| 70 (76.09) | 50 (90.91) |
|
|
|
Angiotelectasis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
| 57 (61.96) | 18 (32.73) | 11.770 | <0.001 | 36 (39.13) | 12 (21.82) | 4.691 | 0.030 | 26 (28.26) | 11 (20.00) | 1.247 | 0.264 |
| No |
| 35 (38.04) | 37 (67.27) |
|
| 56 (60.87) | 43 (78.18) |
|
| 66 (71.74) | 44 (80.00) |
|
|
| Early formation of
pigmentation islands |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
| 38 (41.30) | 7 (12.73) | 13.230 | <0.001 | 16 (17.39) | 5 (9.09) | 1.937 | 0.164 | 15 (16.30) | 5 (9.09) | 1.524 | 0.217 |
| No |
| 54 (58.70) | 48 (87.27) |
|
| 76 (82.61) | 50 (90.91) |
|
| 77 (83.70) | 50 (90.91) |
|
|
| Perilesional
hyperpigmentation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
| 38 (41.30) | 18 (32.73) | 1.074 | 0.300 | 15 (16.30) | 13 (23.64) | 1.200 | 0.273 | 17 (18.48) | 11 (20.00) | 0.052 | 0.820 |
| No |
| 54 (58.70) | 37 (67.27) |
|
| 77 (83.70) | 42 (76.36) |
|
| 75 (81.52) | 44 (80.00) |
|
|
Evaluation of the efficiency of
combination therapy with tacrolimus ointment and 308-nm excimer
laser by dermoscopy
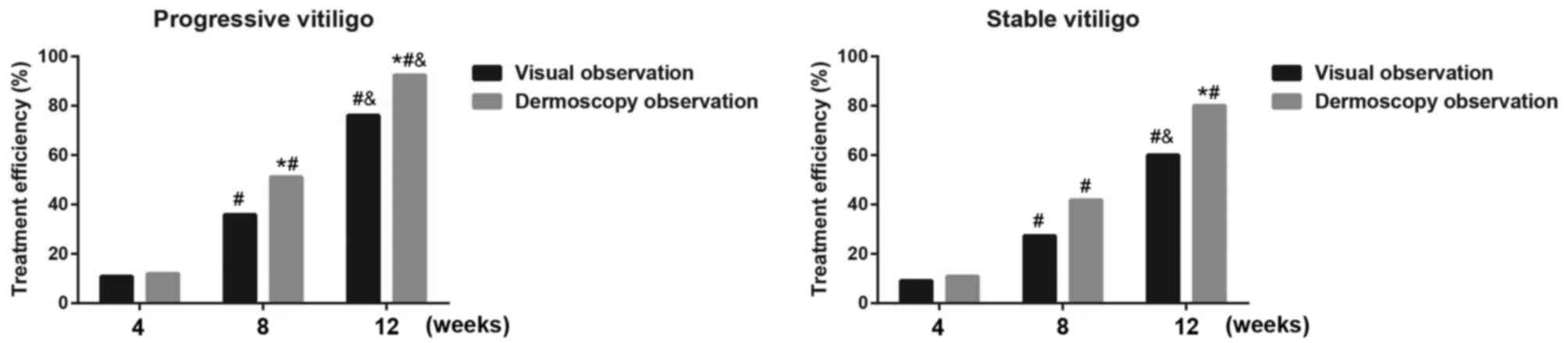
Eight patients presented with erythema and a burning
sensation, but these symptoms did not affect the combination
therapy, and no medical treatments were administered. The
efficiency of the combination therapy at 4 and 8 weeks did not
significantly differ between the progressive-stage and stable-stage
groups when assessed by either visual observation or dermoscopy
(all P>0.05). At 12 weeks, the efficiency of combination therapy
in the progressive-stage group was markedly higher than that in the
stable-stage group as assessed by direct visual and dermoscopy
observation (dermoscopy, 92.39 vs. 80.00%; visual, 76.09 vs.
60.00%; both P<0.05). After 8 and 12 weeks of combination
therapy, the efficiencies in progressive-stage patients assessed by
dermoscopy observation were significantly higher than those
determined by visual observation (8 weeks, 51.09 vs. 35.87%; 12
weeks, 92.39 vs. 76.09%; both P<0.05), and the efficiencies in
stable-stage patients assessed by dermoscopy observation were
significantly higher than those determined by visual observation at
12 weeks (80.00 vs. 60.00%, P<0.05), as illustrated in Fig. 2.
Multivariate binary logistic
regression analysis
Multivariate binary logistic regression analysis was
performed with the efficiency of dermoscopy observation (effective
or non-effecitve) as a dependent variable, and with the disease
stage, age, sex as well as other parameters that affect efficiency
as independent variables (Table
IV). The results demonstrated that the disease stage,
vitiliginous area and course of disease were risk factors
associated with the treatment efficacy of tacrolimus ointment with
308-nm excimer laser (all P<0.05).
 | Table IV.Multivariate logistic regression
analysis of the influencing factors for the treatment efficacy of
tacrolimus ointment with a 308-nm excimer laser. |
Table IV.
Multivariate logistic regression
analysis of the influencing factors for the treatment efficacy of
tacrolimus ointment with a 308-nm excimer laser.
| Variable | B | SE | Wald | df | P-value | Exp (B) | 95% CI |
|---|
| Group (Stable vs.
Progressive) | −3.075 | 1.087 | 8.004 | 1 | 0.005 | 0.046 | 0.005–0.389 |
| Sex (Female vs.
Male) | −1.614 | 1.044 | 2.390 | 1 | 0.122 | 0.199 | 0.026–1.541 |
| Age | 0.053 | 0.028 | 3.445 | 1 | 0.063 | 1.054 | 0.997–1.115 |
| Vitiliginous
area | −1.370 | 0.398 | 11.866 | 1 | 0.001 | 0.254 | 0.117–0.554 |
| Course of
disease | −0.010 | 0.005 | 3.971 | 1 | 0.046 | 0.990 | 0.980–1.000 |
| Location of
vitiliginous areas |
|
| 2.778 | 2 | 0.249 |
|
|
| Face
vs. torso | 1.043 | 1.084 | 0.926 | 1 | 0.336 | 2.838 | 0.339–23.762 |
| Neck
vs. torso | −0.937 | 1.118 | 0.703 | 1 | 0.402 | 0.392 | 0.044–3.503 |
Discussion
Vitiligo is a common depigmentation disorder; its
pathogenesis has remained to be fully elucidated, while the major
theories include autoimmunity and toxicity in melanocytes mediated
by oxidative stress (29,30). The efficacy of previous treatment
options for vitiligo is not significant, particularly for
leukoplakia on the exposed parts of the face and neck, which may
induce great psychological stress in vitiligo patients (8). Kim et al (31) demonstrated that excimer laser
treatment of vitiligo patients with leukotrichia had a poor
clinical outcome of compared with those without leukotrichia. In
this regard, early diagnosis and treatment as well as timely
monitoring of affected patients may help prevent the development
and progression of the disease. However, in clinical practice, it
is difficult to distinguish evolving vitiligo lesions from
hypopigmentation or depigmentation induced by other causes. The
present study performed an analysis to evaluate the function of
dermoscopy in the evaluation of the therapeutic efficacy of
combination therapy with tacrolimus ointment and 308-nm excimer
laser in vitiligo patients. It was determined that dermoscopy may
be used as an effective means of vitiligo therapy outcome
assessment to provide an accurate and scientific evaluation of the
treatment efficacy. As a noninvasive observation method, dermoscopy
may detect subtle changes in the structure of the skin surface and
lower epidermis as well as skin changes that cannot be observed by
the naked eye (32). At present,
dermoscopic examination is widely used in the diagnosis and
differentiation of depigmentation disorders. Previous studies have
demonstrated that examination by dermoscopy may effectively detect
subtle changes in pigmentation, which may be helpful in the early
diagnosis of vitiligo patients (33,34). In
the present study, dermoscopy to was applied detect the recovery of
pigmentation after combination therapy in vitiligo patients at
different stages under continuous observation. The most important
result was that, compared with the stable-stage patients, more
progressive-stage patients had residual perifollicular
pigmentation, while fewer patients had perilesional
hyperpigmentation. In accordance with the present findings, a
previous study by Meng et al (35) reported that 91.9% of progressive and
62.9% of stable vitiligo patients presented with residual
perifollicular pigmentation. Furthermore, to the best of our
knowledge, the present study was the first to demonstrate that
after 12 weeks of combination therapy, marked differences in the
frequency of residual perifollicular pigmentation were present
between the progressive- and stable-stage patients. A previous
study indicated that, compared with stable patients,
progressive-stage vitiligo patients had increased CD4+ T
cells and decreased CD8+ T cells, which indicated that a
greater T-cell imbalance may be present in vitiligo patients in the
progressive stage (36), leading to
disorders of the functional immune response (17). As is known, tacrolimus ointment and
308-nm excimer laser therapies are associated with significant
changes in immune cells. Cather et al (37) reported that tacrolimus had the
ability to inhibit T-lymphocyte activation, and a study by Yang and
Huang (38) revealed that 308-nm
excimer laser treatment induced apoptosis of T lymphocytes,
suggesting that combination therapy of tacrolimus ointment and
308-nm excimer laser may enhance these immunosuppressive effects
for the treatment of vitiligo, particularly in progressive vitiligo
patients. Furthermore, a previous study reported that melanocyte
damage and local inflammation are important in the induction of
CD8+ cytotoxic T lymphocyte-recognizing peptides derived
from melanocyte protein, thus leading to the immune destruction of
melanocytes (39). Of note,
melanocytes were incompletely destroyed in lesions of progressive
vitiligo patients, whereas stable vitiligo patients, who often have
a long-term disease course, had a complete depigmentation disorder
(24); therefore, the present study
hypothesized that destruction of melanocytes may affect the immune
imbalance, leading to differential sensitivity of combination
treatments in different stages of vitiligo. Furthermore, Kang et
al (40) demonstrated that
during repigmentation, the melanocytes are mainly located on the
edge of the leukoplakia and around the follicle and may represent
early reservoirs of pigmentation. In the present study, dermoscopy
revealed perifollicular repigmentation in several patients and
early reservoirs of pigmentation on the edge of the leukoplakia in
certain patients, consistent with this previous study.
As the second major novel finding of the present
study, the efficiencies assessed by dermoscopy observation were
significantly higher than those determined by visual observation in
progressive-stage as well as stable-stage patients after 12 weeks
of combination therapy. Thatte and Khopkar (33) reported that dermoscopy is able to
effectively detect the presence of pigmentary changes,
perifollicular hyperpigmentation and perilesional
hyperpigmentation, and Kim et al (31) revealed that skin lesions confirmed by
dermoscopy in patients with vitiligo prior to excimer laser
treatment may be helpful in predicting the response to treatment,
indicating that dermoscopy is better than routine histopathology in
the diagnosis of vitiligo. Therefore, it may be concluded that
dermoscopy, as a specific optical amplification method, allows for
early detection of repigmentation conditions in patients with
vitiligo more effectively than observation with the naked eye. This
superior performance may be associated with the advantages of
dermoscopy, which include a wide observation range, unlimited
positions of observation and ease of changing the view. Tacrolimus
ointment has been proven to be an effective and helpful alternative
therapy for vitiligo patients, particularly those with lesions
involving the head and neck (21,41–43). In
the present study, no occurrence of angiotelectasis was observed on
the faces of patients treated with topical tacrolimus, which was
consistent with previous studies. During the course of treatment,
dermoscopic examination facilitates the observation of the
occurrence of angiotelectasis, which is helpful for clinicians to
readjust medications and implement other necessary measures. The
present study had certain limitations, as more clinical data should
have been collected, the sample size should be have been expanded
and a more comprehensive evaluation of the efficacy of therapy for
vitiligo should have been performed.
In summary, the present results supported that
dermoscopy is advantageous in monitoring the recovery of patients
with vitiligo, and compared with observation by the naked eye,
dermoscopy is more effective for evaluating the therapeutic
efficacy of combination therapy with tacrolimus ointment and 308-nm
excimer laser in vitiligo patients. Dermoscopy may be used as an
effective means of vitiligo therapy outcome assessment to provide
an accurate and scientific evaluation of the effects of vitiligo
treatment.
Acknowledgements
The authors would like to thank all subjects who
participated in the present study.
References
|
1
|
Shahmoradi Z, Najafian J, Naeini FF and
Fahimipour F: Vitiligo and autoantibodies of celiac disease. Int J
Prev Med. 4:200–203. 2013.PubMed/NCBI
|
|
2
|
Dertlioğlu SB, Oğuz H, Çiçek D and Yücel
H: Prevalence of glaucoma in patients with vitiligo. Cutis.
97:E21–E25. 2016.PubMed/NCBI
|
|
3
|
Yaghoobi R, Omidian M and Bagherani N:
Vitiligo: A review of the published work. J Dermatol. 38:419–431.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Krüger C and Schallreuter KU: A review of
the worldwide prevalence of vitiligo in children/adolescents and
adults. Int J Dermatol. 51:1206–1212. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Whitton M, Pinart M, Batchelor JM,
Leonardi-Bee J, Gonzalez U, Jiyad Z, Eleftheriadou V and Ezzedine
K: Evidence-based management of vitiligo: Summary of a Cochrane
systematic review. Br J Dermatol. 174:962–969. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Malhotra N and Dytoc M: The pathogenesis
of vitiligo. J Cutan Med Surg. 17:153–172. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mohammed GF, Gomaa AH and Al-Dhubaibi MS:
Highlights in pathogenesis of vitiligo. World J Clin Cases.
3:221–230. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ezzedine K, Eleftheriadou V, Whitton M and
van Geel N: Vitiligo. Lancet. 386:74–84. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zuo RC, Naik HB, Steinberg SM, Baird K,
Mitchell SA, Kuzmina Z, Pavletic SZ and Cowen EW: Risk factors and
characterization of vitiligo and alopecia areata in patients with
chronic graft-vs-host disease. JAMA Dermatol. 151:23–32. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Whitton ME, Ashcroft DM and González U:
Therapeutic interventions for vitiligo. J Am Acad Dermatol.
59:713–717. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Whitton ME, Pinart M, Batchelor J,
Leonardi-Bee J, González U, Jiyad Z, Eleftheriadou V and Ezzedine
K: Interventions for vitiligo. Cochrane Database Syst Rev.
CD003263:2015.
|
|
12
|
Adauwiyah J and Suraiya HH: A
retrospective study of narrowband-UVB phototherapy for treatment of
vitiligo in Malaysian patients. Med J Malaysia. 65:297–299.
2010.PubMed/NCBI
|
|
13
|
Hamzavi IH, Lim HW and Syed ZU:
Ultraviolet-based therapy for vitiligo: What's new? Indian J
Dermatol Venereol Leprol. 78:42–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shenoi SD and Prabhu S: Indian Association
of Dermatologists V and Leprologists: Photochemotherapy (PUVA) in
psoriasis and vitiligo. Indian J Dermatol Venereol Leprol.
80:497–504. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Spencer JM, Nossa R and Ajmeri J:
Treatment of vitiligo with the 308-nm excimer laser: A pilot study.
J Am Acad Dermatol. 46:727–731. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Esposito M, Soda R, Costanzo A and
Chimenti S: Treatment of vitiligo with the 308 nm excimer laser.
Clin Exp Dermatol. 29:133–137. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yang YS, Cho HR, Ryou JH and Lee MH:
Clinical study of repigmentation patterns with either narrow-band
ultraviolet B (NBUVB) or 308 nm excimer laser treatment in Korean
vitiligo patients. Int J Dermatol. 49:317–323. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang XY, He YL, Dong J, Xu JZ and Wang J:
Clinical efficacy of a 308 nm excimer laser in the treatment of
vitiligo. Photodermatol Photoimmunol Photomed. 26:138–142. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Le Duff F, Fontas E, Giacchero D, Sillard
L, Lacour JP, Ortonne JP and Passeron T: 308-nm excimer lamp vs.
308-nm excimer laser for treating vitiligo: A randomized study. Br
J Dermatol. 163:188–192. 2010.
|
|
20
|
Do JE, Shin JY, Kim DY, Hann SK and Oh SH:
The effect of 308 nm excimer laser on segmental vitiligo: A
retrospective study of 80 patients with segmental vitiligo.
Photodermatol Photoimmunol Photomed. 27:147–151. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Travis LB, Weinberg JM and Silverberg NB:
Successful treatment of vitiligo with 0.1% tacrolimus ointment.
Arch Dermatol. 139:571–574. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Matin M, Latifi S, Zoufan N, Koushki D,
Mirjafari Daryasari SA and Rahdari F: The effectiveness of excimer
laser on vitiligo treatment in comparison with a combination
therapy of Excimer laser and tacrolimus in an Iranian population. J
Cosmet Laser Ther. 16:241–245. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Park OJ, Park GH, Choi JR, Jung HJ, Oh ES,
Choi JH, Lee MW and Chang SE: A combination of excimer laser
treatment and topical tacrolimus is more effective in treating
vitiligo than either therapy alone for the initial 6 months, but
not thereafter. Clin Exp Dermatol. 41:236–241. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Oh TS, Lee O, Kim JE, Son SW and Oh CH:
Quantitative method for measuring therapeutic efficacy of the 308
nm excimer laser for vitiligo. Skin Res Technol. 18:347–355. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Baldi A, Quartulli M, Murace R, Dragonetti
E, Manganaro M, Guerra O and Bizzi S: Automated dermoscopy image
analysis of pigmented skin lesions. Cancers (Basel). 2:262–273.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Celebi ME, Mendonca T and Marques JS:
Dermoscopy Image Analysis. 141. 1st. Boca Raton, Florida, USA: pp.
200–210. 2015, PubMed/NCBI
|
|
27
|
Soyer HP, Argenziano G, Zalaudek I, Corona
R, Sera F, Talamini R, Barbato F, Baroni A, Cicale L, Di Stefani A,
et al: Three-point checklist of dermoscopy. A new screening method
for early detection of melanoma. Dermatology. 208:27–31. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Xiaolan D, Juan Du and Jianzhong Z: The
epidemiology and treatment of vitiligo: A chinese perspective. J
Pigmentary Disord. 1:62014.
|
|
29
|
Awad SS: Depigmentation during vitiligo
activity spares epithelial grafted areas. J Cosmet Dermatol.
15:383–386. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Laddha NC, Dwivedi M, Mansuri MS, Singh M,
Gani AR, Yeola AP, Panchal VN, Khan F, Dave DJ, Patel A, et al:
Role of oxidative stress and autoimmunity in onset and progression
of vitiligo. Exp Dermatol. 23:352–353. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim MS, Cho EB, Park EJ, Kim KH and Kim
KJ: Effect of excimer laser treatment on vitiliginous areas with
leukotrichia after confirmation by dermoscopy. Int J Dermatol.
55:886–892. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Thatte SS, Dongre AM and Khopkar US:
‘Reversed pigmentary network pattern’ in evolving lesions of
vitiligo. Indian Dermatol Online J. 6:222–223. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Thatte SS and Khopkar US: The utility of
dermoscopy in the diagnosis of evolving lesions of vitiligo. Indian
J Dermatol Venereol Leprol. 80:505–508. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chandrashekar L: Dermatoscopy of blue
vitiligo. Clin Exp Dermatol. 34:e125–e126. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Meng RS, Zhao G, Cai RK, Meng X and Jiang
ZG: Application of polarized light dermoscopy in the early
diagnosis of vitiligo and its differential diagnosis from other
depigmented diseases. Zhonghua Pi Fu Ke Za Zhi. 810–813. 2009.
|
|
36
|
Song LX, Yan-Zhu XU and Zhang SF:
Expression levels of T-lymphocyte subsets in peripheral blood of
patients with vitiligo in different staging. Lin Chuang Wu Zhen Wu
Zhi. 49:931–951. 2013.(In Chinese).
|
|
37
|
Cather JC, Abramovits W and Menter A:
Cyclosporine and tacrolimus in dermatology. Dermatol Clin.
19:119–137, ix. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yang HL and Huang XY: 308 nm excimer laser
triggers two different apoptotic pathways of T lymphocytes. J Clin
Dermatol. 37:639–641. 2008.
|
|
39
|
Steitz J, Wenzel J, Gaffal E and Tüting T:
Initiation and regulation of CD8+T cells recognizing melanocytic
antigens in the epidermis: Implications for the pathophysiology of
vitiligo. Eur J Cell Biol. 83:797–803. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kang HY, le Duff F, Passeron T, Lacour JP,
Ortonne JP and Bahadoran P: A noninvasive technique, reflectance
confocal microscopy, for the characterization of melanocyte loss in
untreated and treated vitiligo lesions. J Am Acad Dermatol.
63:e97–e100. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Silverberg NB, Lin P, Travis L, Farley-Li
J, Mancini AJ, Wagner AM, Chamlin SL and Paller AS: Tacrolimus
ointment promotes repigmentation of vitiligo in children: A review
of 57 cases. J Am Acad Dermatol. 51:760–766. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Majid I: Does topical tacrolimus ointment
enhance the efficacy of narrowband ultraviolet B therapy in
vitiligo? A left-right comparison study. Photodermatol Photoimmunol
Photomed. 26:230–234. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Nordal EJ, Guleng GE and Rönnevig JR:
Treatment of vitiligo with narrowband-UVB (TL01) combined with
tacrolimus ointment (0.1%) vs. placebo ointment, a randomized
right/left double-blind comparative study. J Eur Acad Dermatol
Venereol. 25:1440–1443. 2011. View Article : Google Scholar : PubMed/NCBI
|