Introduction
Owing to the social and economic development of
China, patients in need of surgery are currently on the increase.
Improved control in intensity and depth has led to use of
inhalation anesthesia having advantages over intravenous anesthesia
in surgery. Due to its mild irritation, rapid induction, stable
maintenance, and rapid revival, sevoflurane has replaced other
inhalational anesthetics in surgery and has become a first-line
drug (1). However, previous findings
have indicated that sevoflurane can lead to postoperative cognitive
dysfunction (2), although the
evidence for this effect is anecdotal.
Postoperative cognitive dysfunction or delirium
refers to changes in cognitive function affecting orientation,
thinking, attention, and insight (3), and is one of the most common
postoperative complications. Postoperative cognitive dysfunction
seriously affects the life of patients, prolongs hospitalization,
and increases the costs for medical care, thus bringing additional
burden to the patients and their families (4). Therefore, the relationship between
postoperative cognitive dysfunction, anesthesia administration, and
surgical trauma has increasingly attracted the attention of
anesthesia experts and clinicians. Present research has not fully
elucidated the specific mechanism by which sevoflurane affects
cognitive dysfunction.
Sevoflurane inhalation was utilized in the present
study to determine its effects on cognitive function in rats. We
analyzed changes in the expression of tumour necrosis factor-α
(TNF-α), interleukin (IL) −6, −8, and apoptosis in the hippocampus
of rats treated with sevoflurane, providing experimental data for
future clinical applications.
Materials and methods
Animals and grouping
We obtained 100 male Sprague-Dawley rats, 2 months
old with an average weight of 250–350 g (Nanjing Junke Biological
Engineering Co., Ltd., Nanjing, China). The rats were fed ad
libitum and kept in a 12 h light/dark cycle at 22–24°C. The
rats were randomly divided into 4 groups: i) Control (air
inhalation), ii) low-dose (1.5% sevoflurane inhalation for 2 h),
iii) high-dose (3% sevoflurane inhalation for 2 h), and iv)
nimodipine (3.0% sevoflurane inhalation for 2 h + nimodipine
treatment). Nimodipine is a calcium channel blocker that lowers
blood pressure and reduces brain damage from a burst blood vessel
(5).
Major instruments
The instruments used in the present study were:
Anesthesia machine (Shanghai Yuyan Instruments Co., Ltd., Shanghai,
China), anesthesia gas monitor (Harvard Apparatus, Holliston, MA,
USA), electronic balance (BS200S; Sartorius AG, Göttingen,
Germany), centrifuge (54178; Eppendorf, Hamburg, Germany),
electrophoresis apparatus DYY-2C and shaker WD-9405B both from
(Beijing Liuyi Instrument Factory, Beijing, China), refrigerator
(BCD256KFB; Haier Group, China), MightySmall Transphor (Amersham
Biosciences Corp., Piscataway, NJ, USA), and Morris water maze
(Beijing Shuolinyuan Science and Technology, Beijing, China).
Major reagents
The major reagents used in the present study were:
Sevoflurane (lot no. 11122231; Shanghai Hengrui Medicine Co., Ltd.,
Shanghai, China), BCA protein assay kit (PC0020; Beijing Suolaibao
Science and Technology Co., Ltd., Beijing, China), skim milk powder
(LP0031; Shanghai Chuanxiang Biotechnology Ltd., Shanghai, China),
protein marker (801-01; Shanghai Puxin Biological Technology Co.,
Ltd., Henan, China), RIPA lysis buffer (C1053, Beijing Pulilai Gene
Technology Co., Ltd., Beijing, China), acrylamide (AB1032; Bio
Basic Inc., Ontario, Canada), glycine (GT2065; Shanghai Biological
Engineering Technology Ltd., Shanghai, China), tris (hydroxymethyl)
aminomethane (TB0194; Bio Basic Inc.), 4% paraformaldehyde in
phosphate-buffered saline (PBS) solution (Shanghai Biological
Engineering Company, Shanghai, China), ELISA kit for quantitative
assay of mouse TNF-α (MTA00B), IL-6 (M6000B), and mouse IL-8
(M8000B) all from R&D Systems, Inc., (Minneapolis, MN, USA),
and Caspase 3 antibody (cat. no. ab9665; Cell Signaling Technology,
Inc., Danvers, MA, USA).
Anesthesia administration
The rats were placed in the prepared anesthesia box
and anaesthetized with an inhalation machine. Oxygen concentration
and anesthesia doses were continuously monitored. The anesthesia
time commenced when the sevoflurane concentration reached the
maximum for each group. The gas flow in the anesthesia chamber was
maintained at 4 l/min.
Water maze test
The Morris water maze was used to test the cognitive
function of the rats in each group. Since its invention in 1984,
the Morris water maze has been used to evaluate the spatial
learning ability and behavior of animals (6). Therefore, the Morris water maze can be
used to examine the cognitive competence of animals after any
intervention (7,8). The rats were placed into the water at
the midpoint of the pool wall in a quadrant. A platform was set in
the southwest quadrant, approximately 25 cm from the wall. The
distance from the platform to the wall was equal to that from the
platform to the pool center. The temperature and light of the water
maze were kept constant. The rats were trained for 1 week, 8 times
a day. Each time a rat was placed into the water maze, the latent
period was recorded before finding the platform for a total of 90
sec. The total length of the swimming route was recorded.
Harvest of the hippocampal tissue
After the end of the experiments, the rats were
sacrificed by cervical dislocation and the whole brain was isolated
and placed on tin foil paper. The cortical tissue was removed with
ophthalmological forceps and the hippocampi harvested. Total
protein was extracted from the hippocampus and quantified.
Western blot analysis
The total protein homogenates from hippocampal
tissue were resolved in an 8–10% gradient SDS-PAGE and transferred
onto nitrocellulose membranes by semi-dry method. The membrane was
blocked using blocking solution (5% skim milk powder) and incubated
at 4°C for 1 h. The rabbit anti-rat caspase-3 polyclonal primary
antibody (1:5,000, cat. no. 9662; Cell Signaling Technology, Inc.)
was added onto the membrane, followed by overnight incubation at
4°C. After 4 washes in PBS, the secondary goat anti-rabbit IgG
polyclonal antibody (1:10,000; cat. no. 7074; Cell Signaling
Technology, Inc.) was added for 2 h. The membrane was rinsed three
times using sterile 4% paraformaldehyde in PBS, followed by
chromogenic reaction, exposure, development, and documentation.
Finally, optical density of the bands was determined by using a gel
imaging system, and the protein expression quantitatively
analyzed.
Statistical analysis
SPSS 19.0 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. Measurement data were presented
as means ± SD, and inter-group data were compared using single
factor ANOVA. P<0.05 was considered to indicate a statistically
significant difference.
Results
Effect of sevoflurane on cognitive
function of rats after inhalation anesthesia
After treating rats with sevoflurane, the latent
period in the Morris water maze was examined. Sevoflurane
anesthesia significantly prolonged the latent period and
significantly shortened the total length of the swimming route of
the rats in a dose-dependent manner (Table I). After high-dose sevoflurane and
nimodipine, the latent period was significantly shorter and the
total length of swimming route was longer than that of the
high-dose sevoflurane group (Table
I). These results suggested a decreased cognitive function for
rats treated with sevoflurane.
 | Table I.Effects of sevoflurane on cognitive
function of rats after anesthesia. |
Table I.
Effects of sevoflurane on cognitive
function of rats after anesthesia.
| Groups | Latent period
(sec) | Total route length
(cm) |
|---|
| Control | 9.41±1.23 | 972±85 |
| Low-dose |
10.86±1.34a | 854±98a |
| High-dose |
16.52±3.29b | 339±101b |
| Nimodipine |
12.04±3.46c | 536±127c |
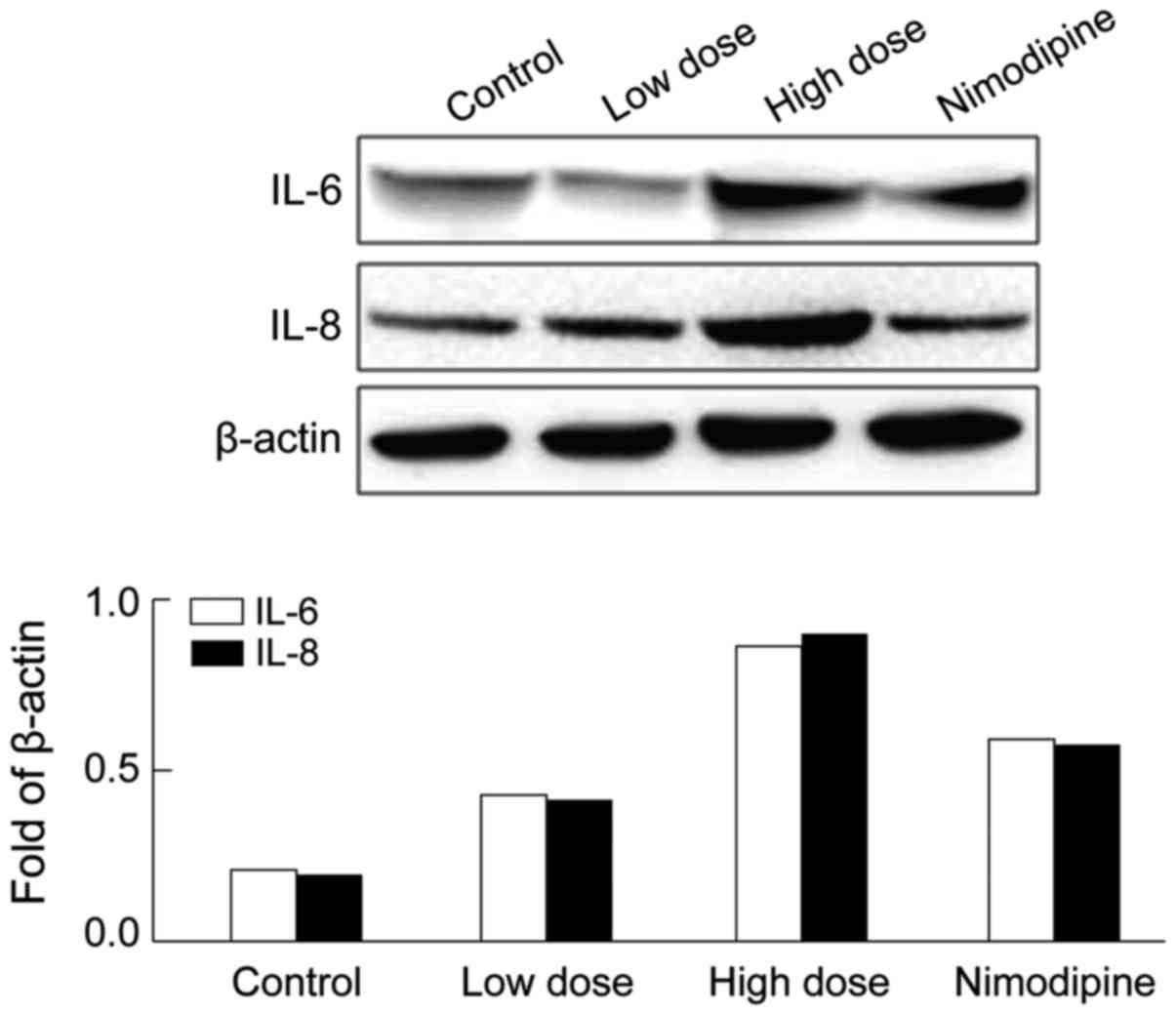
Effect of sevoflurane on IL-6/IL-8
expression
The expression of IL-6/IL-8 in hippocampus after
anesthesia was examined to determine the potential mechanisms
mediating the effects of sevoflurane on cognition. The western blot
analysis showed that IL-6 and IL-8 were significantly upregulated
in hippocampus after sevoflurane anesthesia compared with that of
the control group (Fig. 1),
indicating hippocampus inflammation. After nimodipine intervention
the abnormal expression of IL-6 and IL-8 in rats was partially
reversed compared with the high-dose group (Fig. 1).
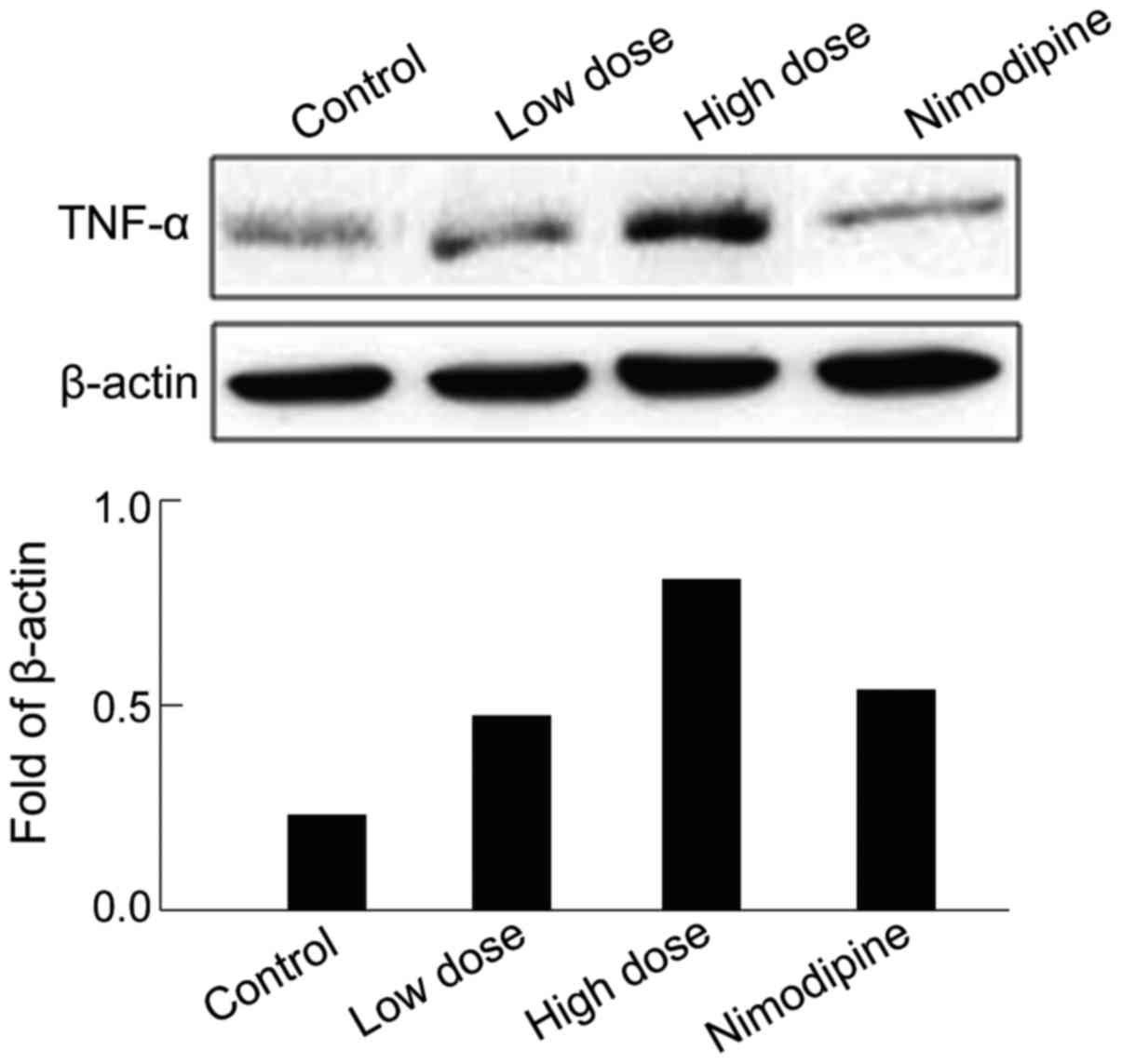
Effect of sevoflurane on TNF-α
expression
The activation of other inflammatory pathways were
studied by examining the expression of TNF-α. TNF-α was
significantly upregulated in hippocampus after sevoflurane
anesthesia compared with that of the control group (Fig. 2), supporting the inflammation of
hippocampus. After nimodipine intervention, the TNF-α expression
was partially restored compared with the high-dose group (Fig. 2).
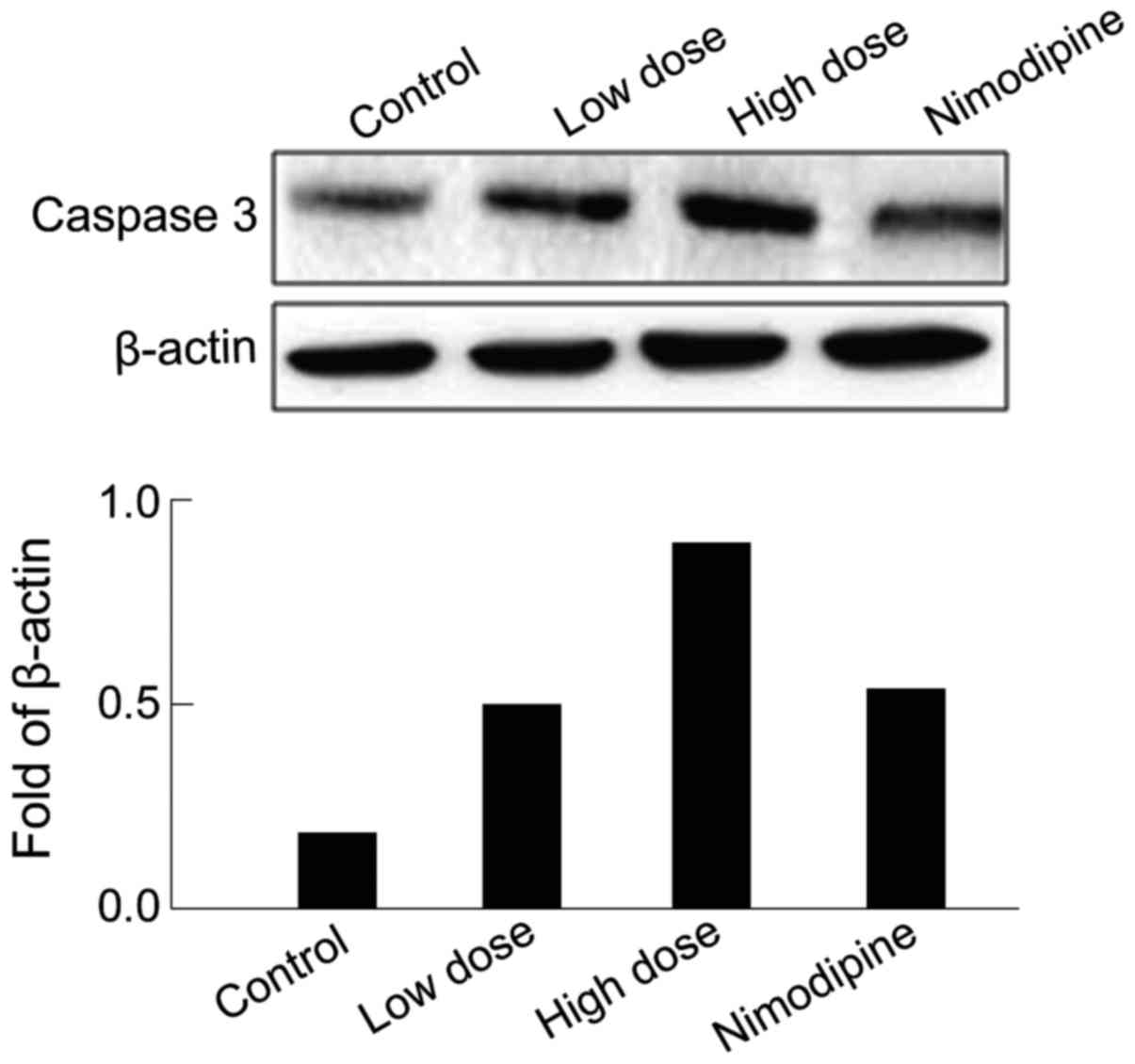
Effects of sevoflurane on Caspase-3
expression
Activation of apoptosis markers after anesthesia
were also examined. The results showed that Caspase-3 expression
was upregulated in rat hippocampus after sevoflurane anesthesia
compared with that of the control group (Fig. 3), indicating significant neuronal
death in the hippocampus. After nimodipine intervention, Caspase-3
expression was partially restored compared with that of the
high-dose group (Fig. 3).
Discussion
Postoperative cognitive dysfunction causes
personality disorder, decrease of social ability, loss of
interpersonal skills, and seriously affects the quality of life
because of severe hypomnesis, inattention, and other mental issues
(9). The International Study of
Post-Operative Cognitive Dysfunction (ISPOCD) specializes in the
largest multicenter study currently to define the relationship
between anesthesia and postoperative cognitive dysfunction. The
ISPOCD study concluded that the incidence rate of postoperative
cognitive dysfunction was 26% one week after surgery, 10% three
months after surgery, and 1% two years after surgery (except for
cardiac surgery) (10). During
cardiac surgery when a cardiopulmonary bypass device was used, the
incidence of postoperative cognitive dysfunction was 53% one week
after surgery and 42% in the intervening five years. Based on these
results, scholars now pay more attention to the occurrence of
postoperative cognitive dysfunction.
The specific mechanisms of cognitive dysfunction
caused by anesthesia remain unclear. Based on the existing
theories, some possible mechanisms include: i) Anesthesia causes
direct toxic effects on calcium homeostasis in neurons (11); ii) the neuroinflammation system is
aggravated by surgical injury (12);
iii) the physiological functions of neural stem cells in the brain
are inhibited by anesthesia (13);
and iv) anesthesia exacerbates the endogenous neurodegeneration
processes (14). Our study confirmed
that the cognitive function of rats decreased after sevoflurane
anesthesia. Previous findings have suggested that sevoflurane can
activate specific enzymes and cause protein denaturation (15). Additionally, sevoflurane can induce
ER stress, induce apoptosis, and lead to cognitive dysfunction
(16). We confirmed that sevoflurane
upregulated Caspase-3 in hippocampal tissue.
Neurodegenerative diseases can cause damage to the
cognitive function and inflammation plays an important role in
these pathologies (17,18). During surgical intervention, the
stress response can lead to the production of several inflammatory
factors such as TNF-α, IL-6, and IL-8. These inflammatory factors
promote the release of other inflammatory factors, thus aggravating
the inflammatory response. Sevoflurane is known to increase the
expression level of IL-6 and TNF-α, thereby causing
neuroinflammation (19). In the
present study, we confirmed that sevoflurane upregulated the levels
of TNF-α, IL-6, and IL-8 in anesthetized rats, supporting the role
of neuroinflammation to the occurrence of postoperative cognitive
dysfunction (20,21).
Elevated intracellular calcium is a common pathway
associated with nerve impairment that can be caused by multiple
factors. Calcium overload is a pathological state that can induce
metabolic disequilibrium, which eventually leads to cognitive
dysfunction (22). Calcium overload
in the brain can trigger harmful processes such as inflammation,
injury, and neuronal death (23).
Moreover, calcium overload in the hippocampus affects
neurotransmitter release by decreased synaptic conductivity. This
disturbance of synaptic transmission ultimately aggravates learning
and memory dysfunction (24).
Nimodipine is a dihydropyridine calcium channel blocker whose
targets are the brain vessels and neurons. In the present study, we
have shown that nimodipine restored neuronal function in the
hippocampus after anesthesia and partially recovered the cognitive
dysfunction caused by sevoflurane inhalation. Thus, the
neuroprotective activity of nimodipine suggest that sevoflurane
causes neuronal dysfunction, at least in part, by disrupting
calcium transport (25).
Furthermore, nimodipine partially restored the abnormal expression
of TNF-α, IL-6, IL-8, and Caspase-3, suggesting that
neuroinflammation and cell death are pathways activated downstream
of the calcium dysfunction.
In conclusion, the sevoflurane-induced cognitive
dysfunction may be related to the activation of TNF-α, IL-6, IL-8,
and Caspase-3 and other inflammatory and apoptotic factors. The
administration of nimodipine can partially restore the damage
caused by sevoflurane, suggesting altered calcium transport.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tang L, Liu H, Wu Y, Li M, Li W, Jiang M,
Hou J, Jiang Y, Xia Z and Meng Q: Sevoflurane may be more
beneficial than propofol in patients receiving endoscopic variceal
ligation and endoscopic variceal sclerotherapy: A randomized,
double-blind study. Exp Ther Med. 14:3145–3152. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Peng S, Zhang Y, Li GJ, Zhang DX, Sun DP
and Fang Q: The effect of sevoflurane on the expression of M1
acetylcholine receptor in the hippocampus and cognitive function of
aged rats. Mol Cell Biochem. 361:229–233. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Monk TG, Weldon BC, Garvan CW, Dede DE,
van der Aa MT, Heilman KM and Gravenstein JS: Predictors of
cognitive dysfunction after major noncardiac surgery.
Anesthesiology. 108:18–30. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Feng X, Liu JJ, Zhou X, Song FH, Yang XY,
Chen XS, Huang WQ, Zhou LH and Ye JH: Single sevoflurane exposure
decreases neuronal nitric oxide synthase levels in the hippocampus
of developing rats. Br J Anaesth. 109:225–233. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bork K, Wurm F, Haller H, Strauss C,
Scheller C, Gnanapragassam VS and Horstkorte R: Neuroprotective and
neuroregenerative effects of nimodipine in a model system of
neuronal differentiation and neurite outgrowth. Molecules.
20:1003–1013. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Choeiri C, Hewitt K, Durkin J, Simard CJ,
Renaud JM and Messier C: Longitudinal evaluation of memory
performance and peripheral neuropathy in the Ins2C96Y
Akita mice. Behav Brain Res. 157:31–38. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fitsanakis VA, Thompson KN, Deery SE,
Milatovic D, Shihabi ZK, Erikson KM, Brown RW and Aschner M: A
chronic iron-deficient/high-manganese diet in rodents results in
increased brain oxidative stress and behavioral deficits in the
morris water maze. Neurotox Res. 15:167–178. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kumar A, Seghal N, Padi SV and Naidu PS:
Differential effects of cyclooxygenase inhibitors on
intracerebroventricular colchicine-induced dysfunction and
oxidative stress in rats. Eur J Pharmacol. 551:58–66. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Umholtz M and Nader ND: Anesthetic
immunomodulation of the neuroinflammation in postoperative
cognitive dysfunction. Immunol Invest. 46:805–815. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jungwirth B, Zieglgänsberger W, Kochs E
and Rammes G: Anesthesia and postoperative cognitive dysfunction
(POCD). Mini Rev Med Chem. 9:1568–1579. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wei H and Xie Z: Anesthesia, calcium
homeostasis and Alzheimer's disease. Curr Alzheimer Res. 6:30–35.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wan Y, Xu J, Ma D, Zeng Y, Cibelli M and
Maze M: Postoperative impairment of cognitive function in rats: A
possible role for cytokine-mediated inflammation in the
hippocampus. Anesthesiology. 106:436–443. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sall JW, Stratmann G, Leong J, McKleroy W,
Mason D, Shenoy S, Pleasure SJ and Bickler PE: Isoflurane inhibits
growth but does not cause cell death in hippocampal neural
precursor cells grown in culture. Anesthesiology. 110:826–833.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bohnen NI, Warner MA, Kokmen E, Beard CM
and Kurland LT: Alzheimer's disease and cumulative exposure to
anesthesia: A case-control study. J Am Geriatr Soc. 42:198–201.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Le Freche H, Brouillette J,
Fernandez-Gomez FJ, Patin P, Caillierez R, Zommer N, Sergeant N,
Buée-Scherrer V, Lebuffe G, Blum D and Buée L: Tau phosphorylation
and sevoflurane anesthesia: An association to postoperative
cognitive. Impairment Anesthesiology,. 116(4): 779–787. 2012.
View Article : Google Scholar
|
|
16
|
Chen G, Gong M, Yan M and Zhang X:
Sevoflurane induces endoplasmic reticulum stress mediated apoptosis
in hippocampal neurons of aging rats. PLoS One. 8:e578702013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shih J, May LD, Gonzalez HE, Lee EW, Alvi
RS, Sall JW, Rau V, Bickler PE, Lalchandani GR, Yusupova M, et al:
Delayed environmental enrichment reverses sevoflurane-induced
memory impairment in rats. Anesthesiology. 116:586–602. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang HK, Chungh DS and Hwang JM: The
effect of general anesthesia and strabismus surgery on the
intellectual abilities of children: A pilot study. Am J Ophthalmol.
153:609–613. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang L, Zhang J, Yang L, Dong Y, Zhang Y
and Xie Z: Isoflurane and sevoflurane increase interleukin-6 levels
through the nuclear factor-kappa B pathway in neuroglioma cells. Br
J Anaesth. 110 Suppl 1:82–91. 2013. View Article : Google Scholar
|
|
20
|
Kronfol Z and Remick DG: Cytokines and the
brain: Implications for clinical psychiatry. Am J Psychiatry.
157:683–694. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Akiyama H, Barger S, Barnum S, Bradt B,
Bauer J, Cole GM, Cooper NR, Eikelenboom P, Emmerling M, Fiebich
BL, et al: Inflammation and Alzheimer's disease. Neurobiol Aging.
21:383–421. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kandel ER, Schwartz JH and Jessell TM:
Principles of neuronal science (4th Edition). McGraw-Hill; New
York, NY: pp. 386–409. 2001
|
|
23
|
Vannucci RC, Brucklacher RM and Vannucci
SJ: Intracellular calcium accumulation during the evolution of
hypoxic-ischemic brain damage in the immature rat. Brain Res Dev
Brain Res. 126:117–120. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Foster TC and Norris CM: Age-associated
changes in Ca(2+)-dependent processes: Relation to
hippocampal synaptic plasticity. Hippocampus. 7:602–612. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Macdonald RL and Kelly KM: Antiepileptic
drug mechanisms of action. Epilepsia. 36 Suppl 2:2–12. 1995.
View Article : Google Scholar
|