Introduction
Rats are used widely in experimental studies due to
their small size, low cost, high vitality and short breeding cycle
(1). In experimental research, rats
are used to construct models of biliary obstruction and are
subjected to external drainage of the orbiliary enterostomy
(2–4). There are two primary ways to construct
a biliary obstruction model: Opening the common bile duct and
performing silk ligation and simple silk ligation alone (5,6). The
former requires tissue area separation, which is comprised of a
large area and is time-consuming to perform (7). However, the surgery is thorough and the
latter tissue separation area is relatively small (7). The surgical method, is simple owing to
the fact that the common bile duct does not to be cut, only tied;
however, loose ligating lines may cause the bile duct obstruction
model to function less efficiently (8). At present, regardless of the surgical
method used to establish the model of biliary obstruction, jaundice
eliminating surgery is performed at the onset of jaundice (7), in order to establish the relevant
indicative changes of jaundice prior to and following surgery
(9,10). Previous studies have not assessed
whether obstructive jaundice subsides naturally (7). However, it has been observed that when
creating a rat model of biliary obstruction, jaundice is corrected
spontaneously, without the remission of biliary obstruction through
surgery (11). In a considerable
number of rats, if surgery for jaundice reduction is performed at
this time, the results are likely to be compromised due to the
condition naturally subsiding. Previous studies have demonstrated
that natural jaundice may subside; however the causes of this
spontaneous remission remain unknown (11–13). To
the best of our knowledge, no previous studies exist that have
elucidated this mechanism. Therefore, the aim of the current study
was to investigate the prevalence and causes of spontaneous
remission of obstructive jaundice. To the best of our knowledge,
the present study revealed for the first time the incidence, timing
and major types of jaundice that spontaneously dissipate in biliary
obstruction modeled rats. Three causes of spontaneous regression of
jaundice (microcirculation, adventitia of the adherent omental
canal and loosening of the ligation) were analyzed. In particular,
it was demonstrated by angiography that the small bile ducts of
rats can be opened and that the small ducts present in the
adhesions of the porta hepatic can communicate with the intestine.
This discovery has not been previously described in animal
experiments. This innovative discovery not only fills in the gaps
in animal experiments, but also enriches the content of teaching
materials. At the same time, it may exist as an important reference
value for the selection of animal experiment models for clinical
jaundice analysis and treatment application.
Materials and methods
Ethical approval
All researchers participating in this study were
experts and graduate students from Hainan Provincial People's
Hospital (Hainan, China). The study protocol was approved by the
Hainan Provincial Science and Technology Commission of China
(approval no. ZDYF2016158).
Groupings
A total of 108 healthy (54 male, 54 female), 8 month
old, Wistar rats (180–220 g) were obtained from the Hainan
Provincial Animal Laboratory and assigned randomly to receive
common bile duct ligation (CBDL) and transection (group A), CBDL
only (group B), or CBD dissected free without ligation or
transection (control group C; n=36 in each group). Rats were housed
at a temperature of 20–25°C and a humidity of 50–65% with a 12 h
light/dark cycle. Rats also received ad libitum access to
rat-specific grain and water.
Model creation
Rats were fasted without water for 12 h prior to
surgery. The rats were anesthetized (sodium pentobarbital, 40–45
mg/kg, i.p.) and the fur at the incision area was removed or cut
flat. All the fur on the abdomen was cleaned and disinfected with
75% alcohol prior to surgery. The upper abdomen was opened by a
median incision. The CBD was located along the hepatoduodenal
ligament and dissected free. For group A, the CBD was doubly
ligated near the duodenum with 4-0 silk sutures and transected
between the two ligatures. For group B, the CBD was doubly ligated
near the duodenum without transection. For group C, the CBD was
dissected free without ligation or transection.
Determination of indices
Blood was collected under anesthesia from the tail
vein of six rats from each group at 1, 3, 7, 14, 21 and 28 days
after surgery to determine the levels of total bilirubin (TB; Total
Billirubin kit; cat. no. 0617071; Maccura Biotechnology Co., Ltd.,
Chengdu, China), direct bilirubin (DB; Direct Bilirubin Assay kit;
Maccura Biotechnology Co., Ltd.; cat. no. 0817081), total bile acid
(TBA assay kit; Maccura Biotechnology Co., Ltd.; cat. no. 0611031)
and alanine aminotransferase (ALT assay kit; Maccura Biotechnology
Co., Ltd. Cat. no. 0617031). Following opening of the abdomen
(conducted after surgery), the CBD diameter was measured and a
small piece of liver tissue was collected for histopathology.
At day 21 after surgery, rats with spontaneous
remission of jaundice underwent cholangiography by injection of 38%
meglumine diatrizoate (MD) into the left or right hepatic duct
using a size-7 needle and MD distribution was observed via X-rays
21 days following surgery to ascertain the cause of jaundice
remission.
At day 28 after surgery, 0.2 ml of technetium-99m
iminodiacetic acid (99mTC-IDA) was injected into the
tail vein and its distribution in the bile ducts was observed using
an isotope scanner (ecom; Siemens AG, Munich, Germany). Rats were
anesthetized using 40 mg/kg intraperitoneal 1% sodium pentobarbital
and then sacrificed via exsanguination. Tissues of equal size were
removed from bile ducts above and below the ligature. The
distribution of rat 99mTC-IDA was assessed whilst rats were exposed
to low-dose anesthesia using a single-photon emission computerized
tomography isotope scanner (Siemens AG) with radiocolloid method
software included. The omentum was adhered to the porta hepatis,
jejunum and ileum to determine 99mTC-IDA levels
pot-sacrifice.
Statistical analysis
Data were analyzed using SPSS 18.0 (SPSS, Inc.,
Chicago, IL, USA). Levels of TB, DB, TBA and ALT were compared
among and within groups using one-way analysis of variance,
followed by a post hoc LSD test, and presented as the mean ±
standard deviation. Radionuclide quantitation was compared using a
paired Student's t-test. P<0.05 was considered to indicate a
statistically significant difference.
Results
General observations
At day 3 after surgery, rats in groups A and B were
listless and had poor appetite, with slightly yellow eyes and
tails. Slightly yellow abdominal organs, omental adhesions to the
porta hepatis and slight dilatation of proximal bile ducts were
also observed.
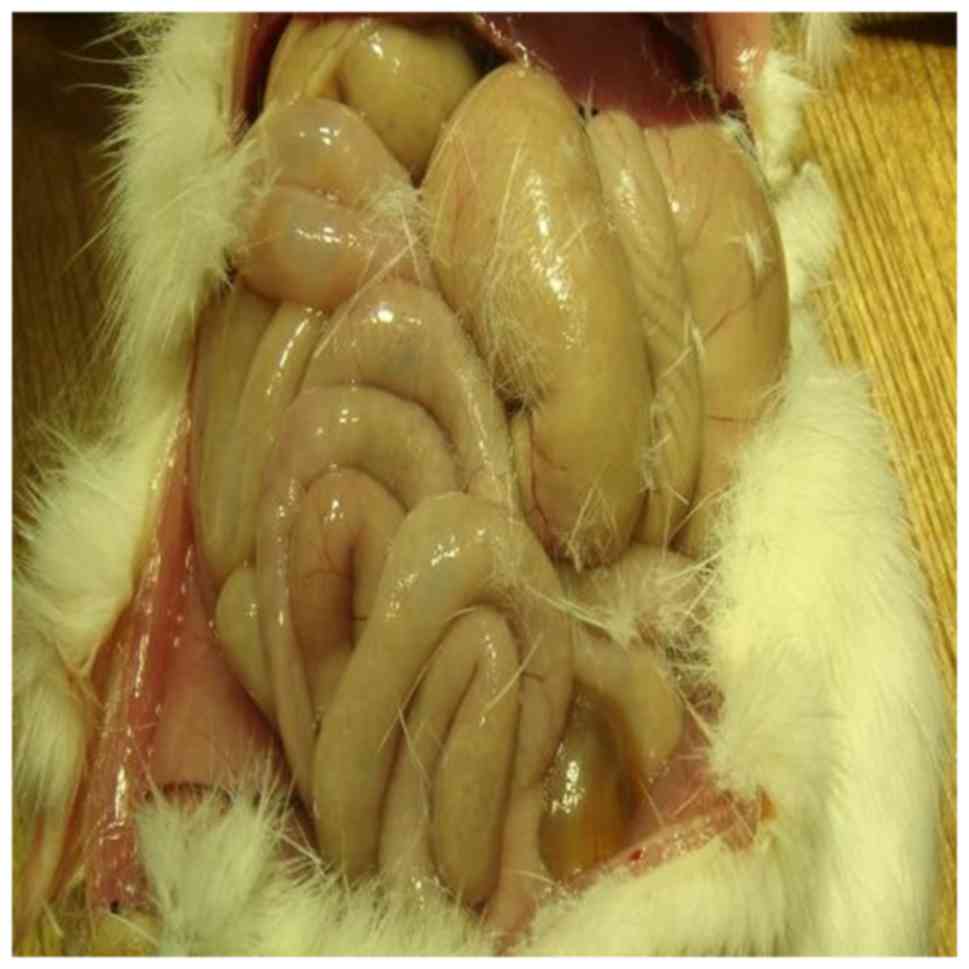
At day 7 after surgery, obviously yellow ears, eyes,
tails and internal organs were observed (Fig. 1), as well as dense hilar adhesions,
dilatation of proximal bile ducts and a moderate liver hardness in
the majority of the rats in groups A and B. In each group, there
was 1 rat in which jaundice was not observed.
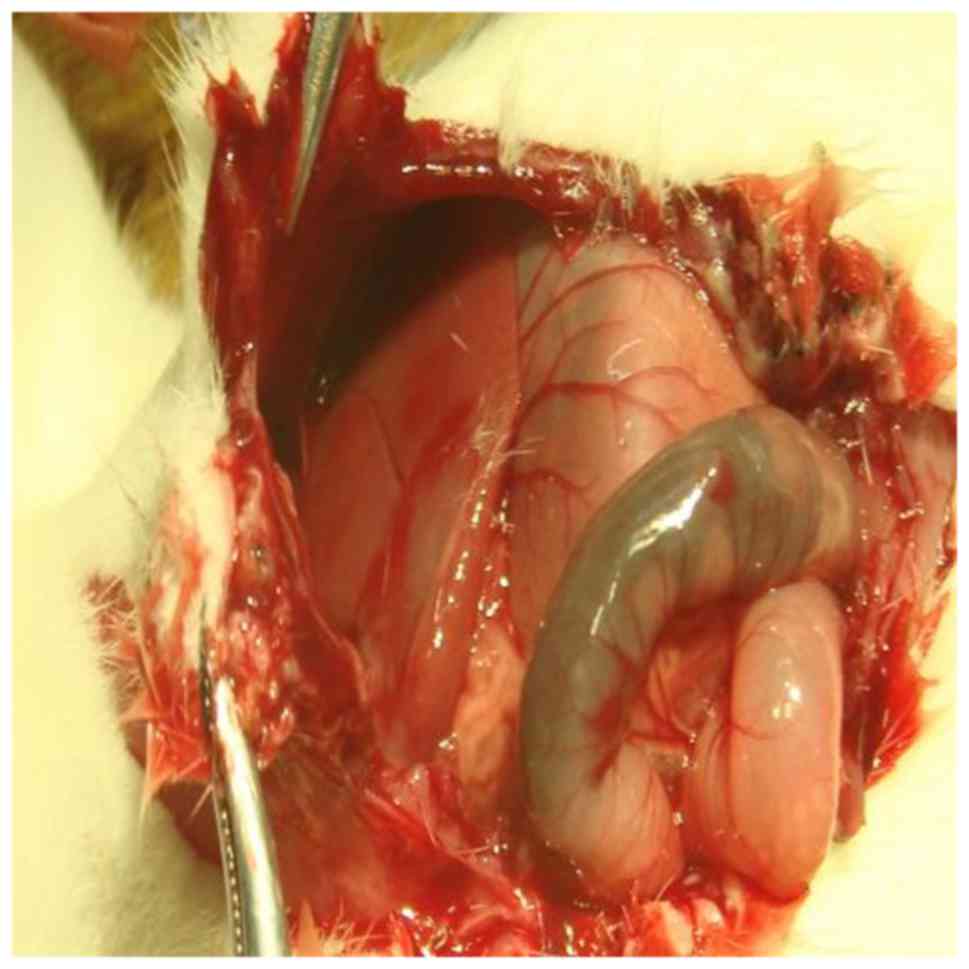
At day 14 after surgery, a more intense yellow color
of the ears, eyes and tail was noted, as were ascites, a hard
liver, orange abdominal organs and marked dilatation of the
proximal CBD (maximum diameter, 20 mm) in 15 of the 18 rats
(Fig. 2; from 14–28 days following
surgery; n=6 per group) in group A. Slightly less yellow ears, eyes
and tail, along with an improved activity and appetite, less yellow
abdominal organs, no significant ascites, a softened liver,
undetached bile duct ligatures, non-significant dilatation of
proximal bile ducts, and severe omental adhesions to the porta
hepatis were observed in 3 rats (16.7%) in group A and 14 rats
(77.8%) in group B. Increased jaundice was observed in an
additional 4 rats in group B, with abdominal findings similar to
the aforementioned 15 rats in group A.
At day 21 after surgery, persistent jaundice and
poor mental status were observed in 15 rats in group A; however,
the other 3 rats in group A and 14 rats in group B exhibited
complete remission of jaundice of the ears, eyes, tail and
abdominal organs, and a soft liver texture (Fig. 3), as well as no dilatation of
proximal bile ducts, weight gain and a normal appetite.
At day 28 after surgery, 2 rats with jaundice in
group A died; persistent jaundice, poor mental status and low
levels of activity were observed in the 4 remaining rats in group A
and 4 rats with jaundice in group B. The remaining 14 rats in group
B and 3 rats in group A exhibited no jaundice and had normal hair
color, good mental status, normal appetite and weight gain. Group C
indicators, including skin, coat, color, mental status and degree
of activity were normal. Incision infection or abdominal infection
did not occur in any rats.
Serum level of bilirubin
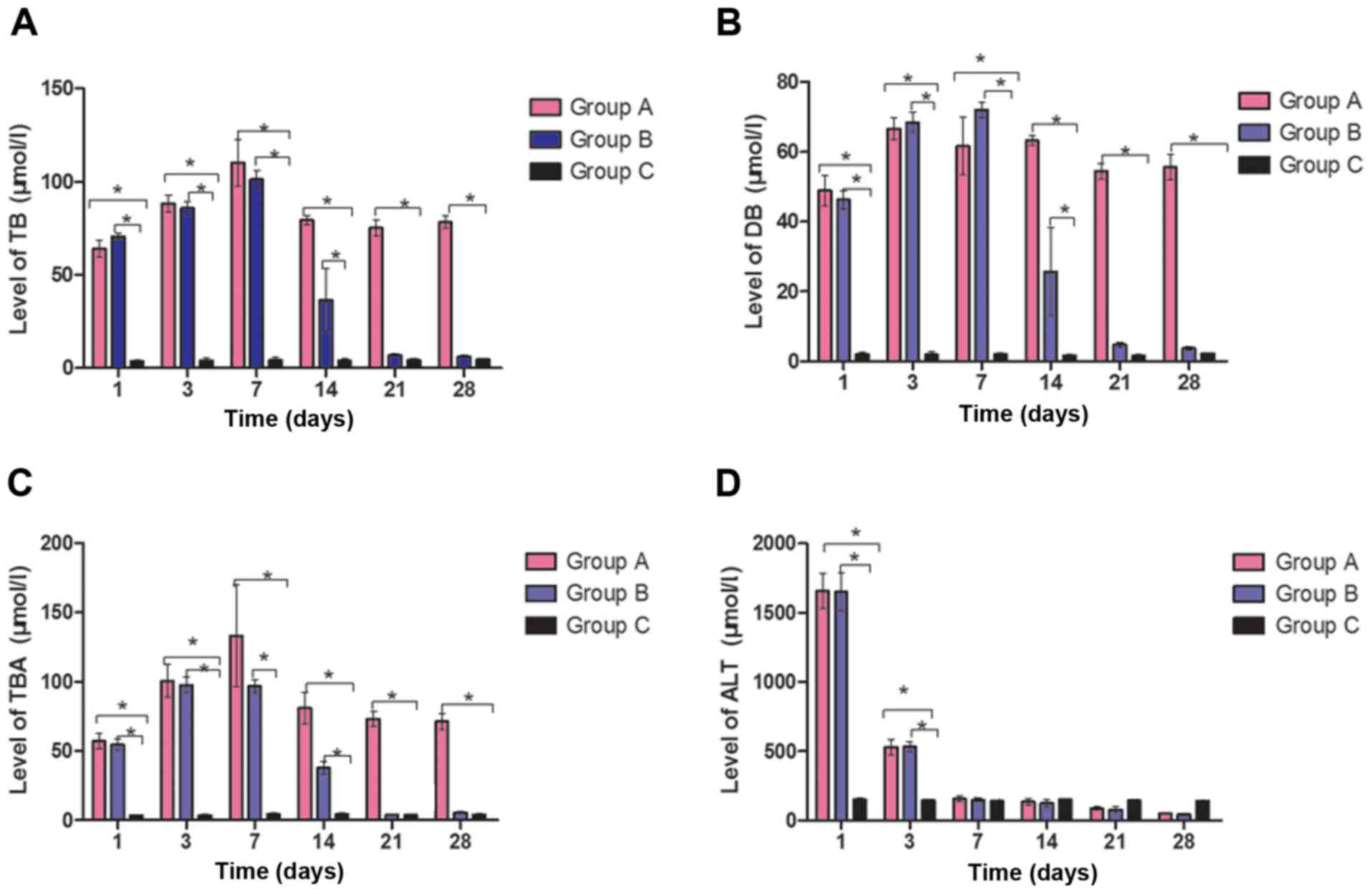
There were significant differences in TB level among
the three groups (P<0.05). The TB level was significantly
different among days 1, 3 and 7 in groups A and B (P<0.05). A
significant increase in TB level was noted in group A compared with
group C at all time points (P<0.05). A significant increase in
TB was observed in group B compared with group C at 1, 3, 7 and 14
days (P<0.05), but not at 21 or 28 days (Fig. 4A).
No significant difference was identified in the DB
level at 14, 21 and 28 days in group A, but a significant
difference was observed at the same time points in group B
(P<0.05). There was a significant increase in DB level in group
A compared with group C at all time points (P<0.05). There was a
significant increased in DB level in group B compared with group C
at 1, 3, 7 and 14 days (P<0.05), but not at 21 or 28 days
(Fig. 4B). The TBA level at 1, 3 and
7 days were significantly different from that at 14, 21 and 28 days
comparing groups A and C, and B and C (P<0.05); however no
significant difference was observed in group B when compared with
group C at 21 and 28 days (Fig.
4C).
ALT level
ALT levels increased, 1 day following surgery. Then,
the ALT level decreased, with the sharpest decrease from days 2 to
3 and a slightly smaller decrease from days 4 to 7. The ALT level
decreased to a normal level after day 14. When comparing groups A
and C, and B and C, the ALT level significantly decreased between
days 1 and 3 (P<0.05). There was no significant difference
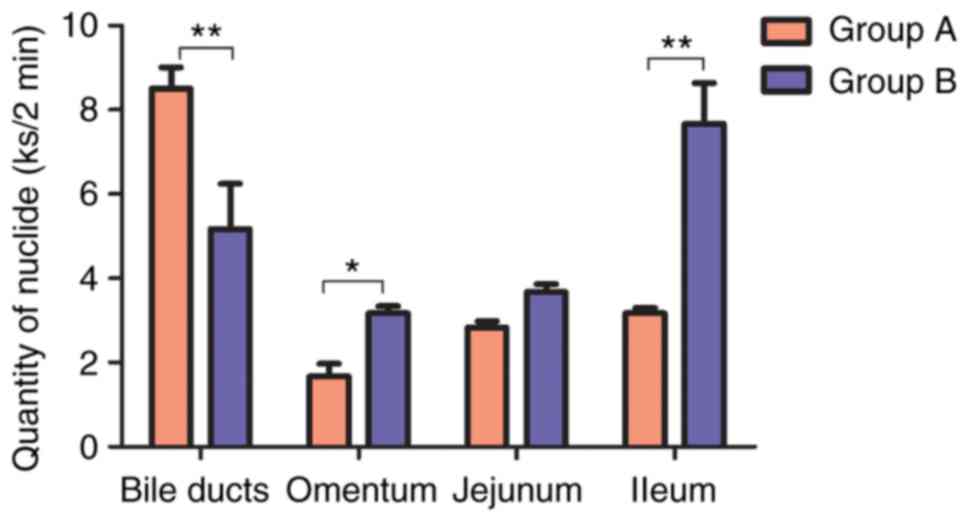
between days 7 and 14 (P>0.05). The radionuclide level from the
bile ducts above the ligature was significantly different from
those at sites with the omentum was adhered to the porta hepatis
and ileum in group A and B when compared with group C (P<0.05).
The ALT level was significantly higher in groups A and B compared
with group C at days 1 and 3 (P<0.05), but no significant
differences were observed from day 7 onwards (Fig. 4D).
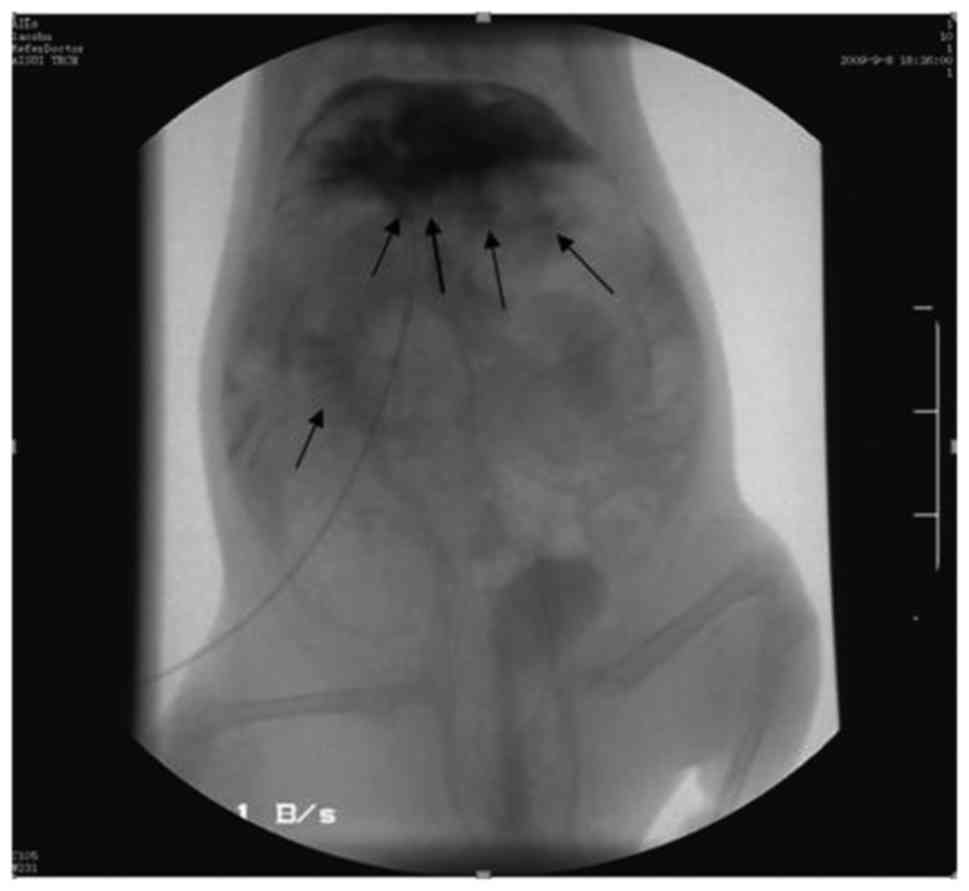
Cholangiography
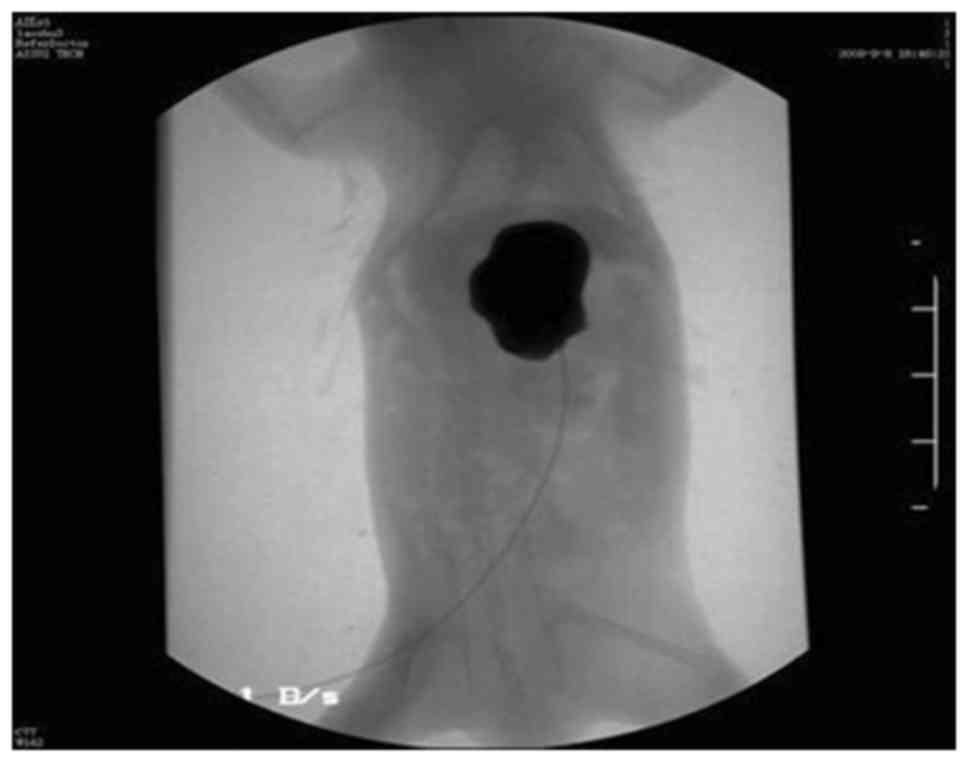
Groups A and B underwent cholangiography with MD
treatment at day 21 after surgery. Marked dilatation of the bile
ducts above the ligature was observed in group A, with a maximum
diameter of 20 mm and the contrast agent did not spread to other
sites (Fig. 5). Slight dilatation of
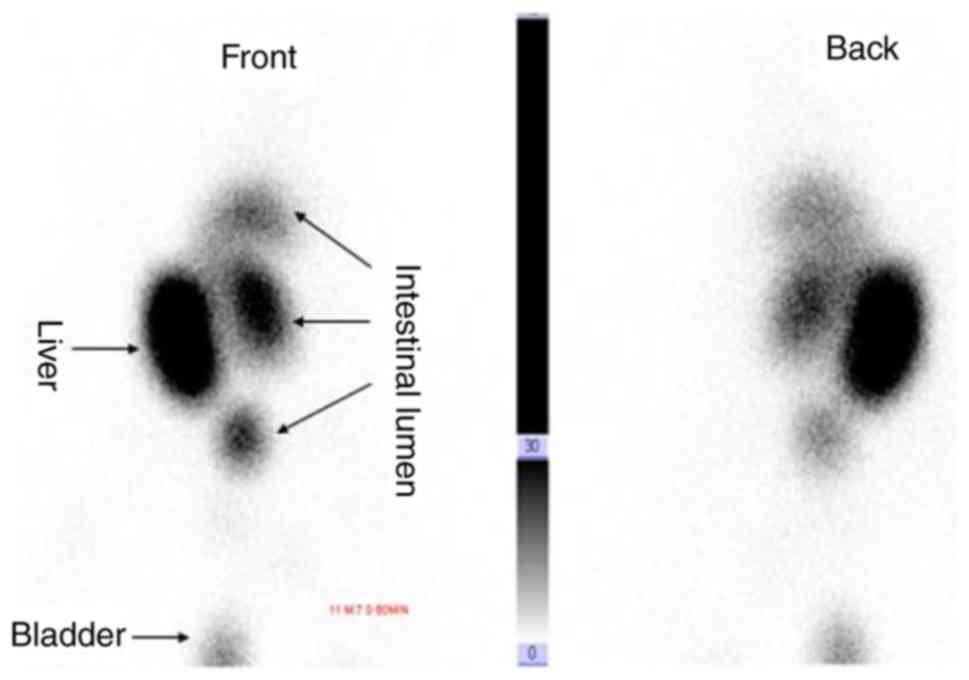
the bile ducts was observed in group B and the contrast agent
entered the small intestinal lumen through the omentum adhering to
the porta hepatis (Fig. 6).
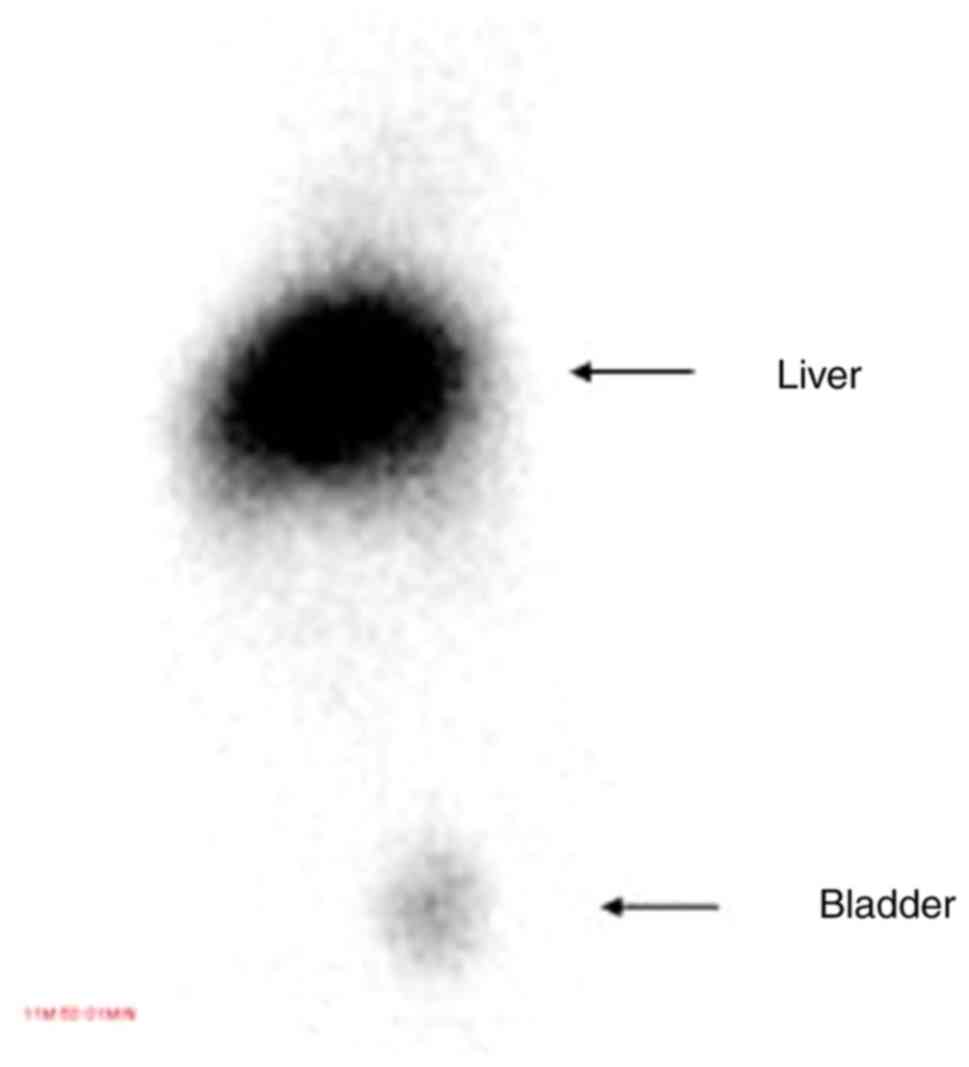
Radionuclide imaging and
quantification
At day 28 after surgery, 99mTC-IDA was
injected into the tail vein of 6 rats with significant jaundice in
group A and 6 rats with remission of jaundice in group B. The
radionuclide accumulated first in the liver. In group A, it did not
enter the intestine and images of the bladder were obtained in a
small number of rats (Fig. 7).
However, in group B, 99mTC-IDA started to enter the
intestine from the liver through the omentum adhering to the porta
hepatis 5 min after administration to produce radionuclide images.
Images of the bladder were obtained in a small number of rats
(Fig. 8).
The radionuclide level at site from the bile ducts
above the ligature was significantly different from those at sites
where the omentum was adhered to the porta hepatis, jejunum, and
ileum in group A (all P<0.05) but not in group B. The
radionuclide level at site bile ducts above the ligature in group A
was significantly higher compared with group B (P<0.01). At
these sites, the isotopic abundance of group B was significantly
higher than that of group A as 99mTC-IDA had entered group B
tissue. (P<0.05; Fig. 9).
Histopathology of the liver
On day 1 after surgery, cholestasis, hepatocyte
swelling, translucent cytoplasm, steatosis and eosinophilic
changes, as well as punctate and focal necrosis were observed in
groups A and B.
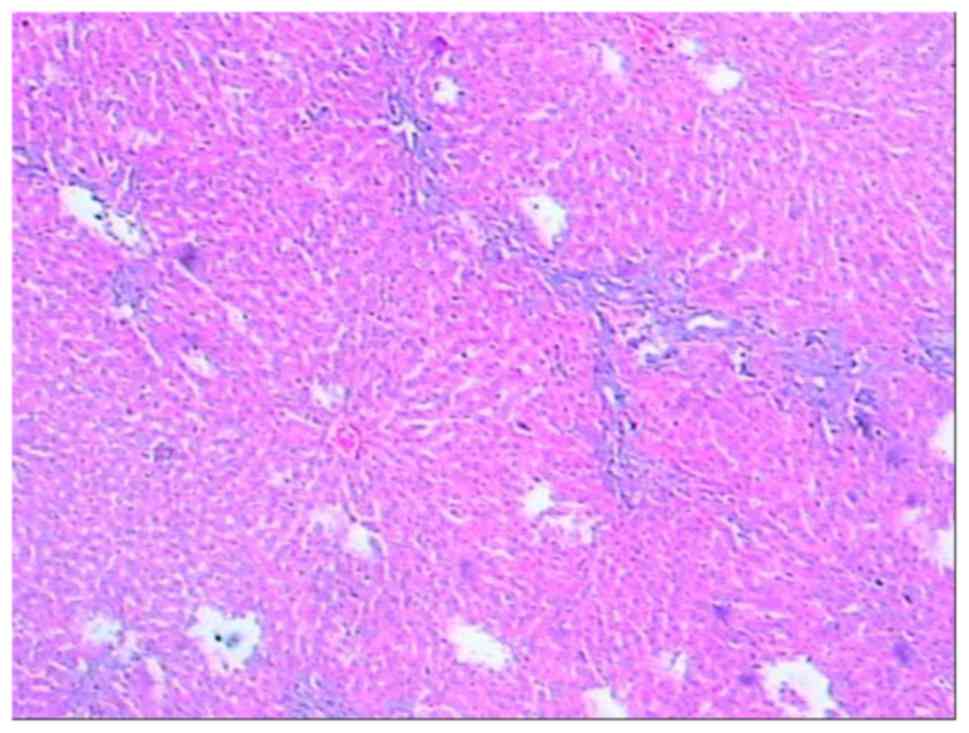
In groups A and B, 7–14 days after surgery,
dilatation and hyperplasia of the small bile ducts in the portal
area, marked hepatic necrosis, marked collagen deposition,
compression of hepatic sinusoids, and dilatation and congestion of
interlobular vessels were observed (Fig. 10).
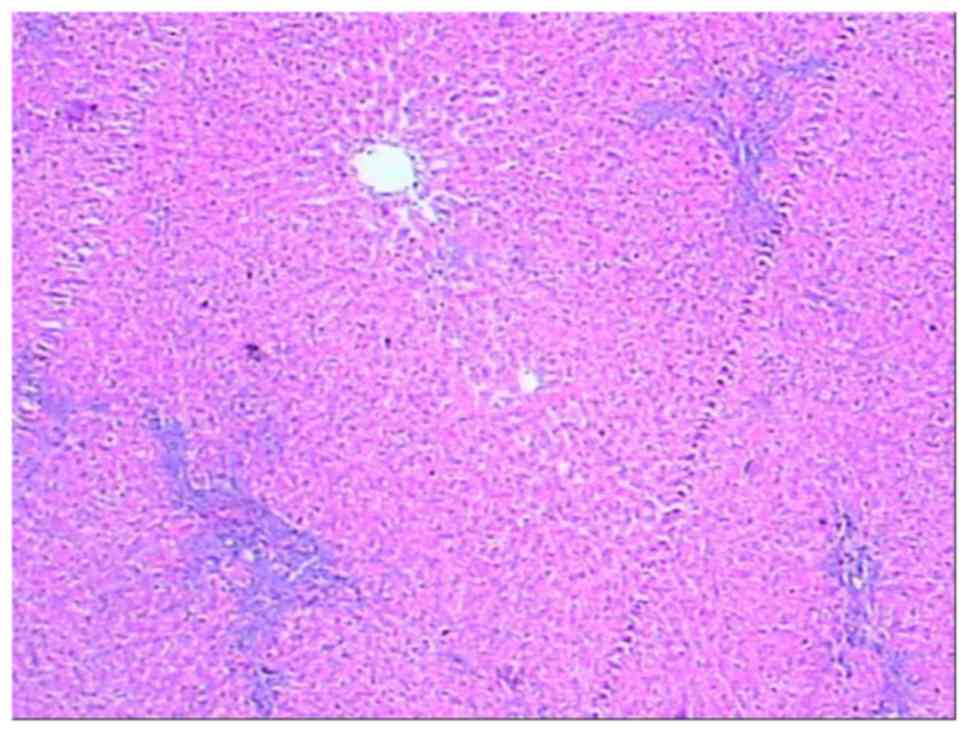
At ≥21 days after surgery, continued hyperplasia of
bile ducts and liver fibrosis were observed in group A. Reduced
hyperplasia of bile ducts, relatively reduced collagen deposition,
non-marked dilatation and congestion of interlobular vessels were
observed in group B (Fig. 11),
which suggested markedly reduced liver fibrosis. These findings
were consistent with the changes observed in serum indices.
Discussion
Serum levels of TB and DB increased progressively
from 1 day after common bile duct ligation and peaked at 7 days.
The serum level of bilirubin continued to increase in most rats in
group A 7 days after surgery, whereas it began to decrease 14 days
after surgery and decreased substantially to normal levels 21 days
after surgery in most rats in group B. This is similar to the
time-to-reduction of the serum level of bilirubin reported by Huang
et al (14). McIntyre and
Rosalki (15) reported that the
serum level of bilirubin generally increases up to 170–500 µmol/l
after complete biliary obstruction, and does not continue to
increase.
The change in TBA level was different from that of
bilirubin. It Significantly increased 1 day after surgery in groups
A and B. The TBA level did not decrease and remained high in group
A 14 days after surgery. Increased levels of DB and TBA reflected
bile obstruction (16,17). The TBA level decreased in group B 14
days after surgery and decreased to a normal level at 21–28 days,
but did not fall below the normal level.
The causes of spontaneous remission of obstructive
jaundice in rats are not known. Wu et al (11) proposed that it may be caused by
increased pressure within the bile duct, which leads to compression
of the portal vein and hepatic artery. This phenomenon leads to
reduced blood flow in the liver, severe liver dysfunction, impaired
ability of hepatocytes to secrete bile, and reduced regurgitation
of bile into blood.
Numerous animal and clinical studies have
investigated the mechanism of liver injury and pathophysiological
changes during obstruction of the bile duct (18,19).
These studies have confirmed pathological liver injury in rats with
obstructive jaundice. The changes in enzyme levels and liver
histology observed in the present study also confirmed pathological
liver injury following biliary obstruction, but do not explain the
causes of remission of spontaneous jaundice.
There are three possible causes of remission of
spontaneous jaundice. The first possible cause is compensatory
opening of very small bile ducts (VSBDs). The hepatoduodenal
ligament of the rat contains the CBD and potentially numerous VSBDs
(20). Following CBDL, the VSBDs may
open to compensate, thereby restoring bile flow. This phenomenon
may explain the complete absence of jaundice following CBDL in 2
rats in the present study. The basic premise of the Kasai procedure
(21) to treat biliary atresia is
that there may be VSBDs in the vicinity of the porta hepatis even
with extrahepatic biliary atresia, and appropriate resection of the
fibers in the porta hepatis that compresses the VSBDs may allow
bile discharge and patient survival. Kordzaia and Jangavadze
(22) injected ink into dilated
proximal bile ducts, and identified that previously unknown VSBDs
were distributed along the veins in the adventitia.
The second possible cause of remission of
spontaneous jaundice is passage into the intestine via omental
ducts adhering to the liver edge. MD injected into dilated proximal
bile ducts was observed to enter the small intestine via the
omentum adhering to the liver edge. The image was unlike that of a
hidden CBD with a clear linear contour, and instead exhibited
several vessels that seemed to adhere to the omentum, via which the
contrast agent had passed into the intestine. Furthermore, in rats
with remission of jaundice, the radionuclide was discharged from
the liver into the intestine via extensive omental ducts in the
porta hepatis to gradually produce radionuclide images 5 min after
99mTC-IDA injection via the tail vein. Comparison of
radionuclide levels among different sites revealed no significant
difference among bile in bile ducts above the CBD ligatures, in
blood vessels adhering to the omentum in the porta hepatis, or in
the intestines of rats with remission of jaundice, whereas the
opposite was true for rats with persistent jaundice. These findings
suggested that bile above the ligatures may pass into the intestine
through omental ducts adhering to the porta hepatis in rats with
remission of jaundice, although this has not been supported by
pathological evidence. The spontaneous remission of jaundice began
14 days after establishment of the model, when omental adhesions to
the porta hepatis were likely to have been relatively stable, which
would have been conducive to the shunting of bile. The mechanism of
action sustaining the passage of bile into the intestine via ducts
adhering to the omentum is not known and requires further
research.
The third possible cause of remission of spontaneous
jaundice is loose ligatures. Spontaneous remission of jaundice
occurred predominantly in rats that received ligation only.
Therefore, loose ligatures, for example due to untightened knots or
short silk suture ends, may have been the cause. However, the
ligatures were intact in the two groups. If the ligatures were
loose in rats that received ligation only, cholangiography with MD
should have exhibited images of the CBD with clear, broad lines.
Loose ligatures in rats that underwent ligation and transection
were associated with biliary peritonitis (23). The rats, in general, would not
survive biliary peritonitis, and bile would be seen within the
abdominal cavity of survivors. However, no bile was observed in the
abdominal cavity of the rats that underwent ligation and
transection in the present study. Loose ligatures theoretically
exist, but should be evaluated specifically.
Overall, 47.2% (17/36) of rats experienced
spontaneous remission of jaundice (A group), 82.4% (14/17) of which
underwent ligation only (B group). The separation area may have
been relatively small in rats that received ligation only, so VSBDs
or hidden CBDs could not be transected or ligated readily, which
was conducive to compensatory opening. Furthermore, the numerous
blood vessels in the hepatoduodenal ligament could lead to
adhesions. Therefore, 77.8% of rats experienced spontaneous
remission of jaundice 14 days after surgery without external
drainage or biliary enterostomy. In this case, the use of internal
or external drainage to reduce jaundice will most likely provide
inaccurate results. A total of 16.7% of rats that underwent
ligation and transection also experienced spontaneous remission of
jaundice, but the majority of rats did not experience spontaneous
remission. This observation may have been because such rats had
large separation areas, and VSBDs or hidden CBDs were likely to be
transected and could not adhere to the greater omentum with ease.
Therefore, CBD transection is the preferred model of biliary
obstruction, and surgery may be undertaken to reduce jaundice 14
days after establishment of the model. If a ligation model is
selected, to reflect the actual effects following jaundice
reduction and restoration of normal morphology and physiological
functions of the liver (24),
jaundice-reduction surgery should be postponed by 1 week until 21
days after establishment of the model and performed in rats with
persistent jaundice. This approach should be adopted since there is
a 1-week period of jaundice reduction 14 days after establishment
of the model, in addition to the high prevalence of spontaneous
remission of jaundice. In conclusion, the establishment of a
biliary obstruction model should be considered as the first choice
for choledocholithotomy + ligation procedures. Yellow reduction
surgery is a procedure in which jaundice is eliminated through
internal and external drainage. The present study demonstrated that
jaundice may spontaneously dissipate following 14 days, thus
eliminating the necessity for surgery.
Acknowledgements
The authors would like to thank the Animal
Experiment Center of Hainan Medical College (Hainan, China) for
providing the experimental location and assisting in completing the
experiments. The authors would also like to thank Professor
Chenghui Luo (Teaching and Research Office of Statistics, Hainan
Provincial Health School, Hainan, China) for completing statistical
analyses for this study.
Funding
The study was supported by the Hainan Provincial Key
Scientific and Technological Research and Development Projects
(grant no. ZDYF2016158), and the Hainan Provincial Government for
providing financial assistance (grant no. 288).
Availability of data and materials
All data generated or analyzed during this study is
included in this published article and can be used as a reference
by other scholars.
Authors' contributions
YLv designed the study, organized and implemented
the experiment, observed the experimental results, collected and
analyzed relevant information, and prepared and submitted the
manuscript. JD and YLi conducted statistical analyses and prepared
the figures. JY, XG XH and HW performed the experiments.
Ethics approval and consent to
participate
The study protocol was approved by the Hainan
Provincial Science and Technology Commission, China (approval no.
ZDYF2016158).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing financial
interests.
References
|
1
|
Bulte JW, Schmieder AH, Keupp J, Caruthers
SD, Wickline SA and Lanza GM: MR cholangiography demonstrates
unsuspected rapid biliary clearance of nanoparticles in rodents:
Implications for clinical translation. Nanomedicine. 10:1385–1388.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ferreira MA, Santos JS, Dutra RA, Salgado
W Jr, Kemp R, Domiciano C, Ramalho LN, Sankarankutty AK and
Castro-e-Silva Od: Bilioduodenal anastomosis in rats with
extra-hepatic biliary obstruction is followed by lesions ischemia
and reperfusion-induced. Acta Cir Bras. 23 Suppl 1:S47–S52. 2008.
View Article : Google Scholar
|
|
3
|
Kemp R, de Araújo WM, de Castro AA,
Ardengh JC, Neder L and dos Santos JS: Influence of biliary
drainage on the repair of hepatic lesions in biliary fibrosis. J
Surg Res. 169:e127–e136. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang ZK, Xiao JG, Huang XF, Gong YC and Li
W: Effect of biliary drainage on inducible nitric oxide synthase,
CD14 and TGR5 expression in obstructive jaundice rats. World J
Gastroenterol. 19:2319–2330. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li JY, Zhu X and Fu ZM: Experimental study
of postoperative obstructive jaundice and postoperative care.
Jiangxi Yixueyuan Xuebao. 31:73–76. 1991.(In Chinese).
|
|
6
|
Saiki S, Chijiiwa K, Komura M, Yamaguchi
K, Kuroki S and Tanaka M: Preoperative internal biliary drainage is
inferior to external biliary drainage in liver regeneration and
function after hepatecctomy in obstruction jaundice rats. Ann Surg.
230:655–662. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Su X, Luo KF, Wu L, Wu LL and Li Wen: The
correlation study of the plasma diamine oxidase activities and the
intestinal barrier function in rats with obstructive jaundice after
internal and external biliary drainages. Xian Dai Sheng Wu Yi Xue
Jin Zhan. 17:3216–3219. 2014.(In Chinese).
|
|
8
|
Gong YH and Li W: The different effects of
internal and external biliary drainages on the blood levels of
endotoxin, interleukin-2 and interleukin-6 in rats with obstructive
jaundice. Weichangbingxue He Ganbingxue Zazhi. 4:329–331. 2008.(In
Chinese).
|
|
9
|
Zeng Y, Zhang Y, Zheng S and Dong J:
Establishment of model of selective external biliary drainage in
rats with obstructive jaundice. Zhonghua Xiao Hua Wai Ke Za Zhi.
6:209–212. 2007.(In Chinese).
|
|
10
|
Zhang SH, Liao CX, Zhang CX, Deng H, Zhu
H, Lei L and Yao C: Establishment of a mouse model of biliary
obstruction and its dynamic observations. Nan Fang Yi Ke Da Xue Xue
Bao. 28:1579–1581. 2008.(In Chinese). PubMed/NCBI
|
|
11
|
Wu W, Yang Y and Huang Q: Bilirubin
metabolism after obstructive jaundice in rats. Zhonghua Gan Dan Wai
Ke Za Zhi. 5:288–291. 2001.(In Chinese).
|
|
12
|
Ni Y, Marchal G, Lukito G, Yu J, Mühler A
and Baert AL: MR imaging evaluation of liver enhancement by
Gd-EOB-DTPA in selective and total bile duct obstruction in rats:
Correlation with serologic, microcholangiographic, and histologic
findings. Radiology. 190:753–758. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kountouras J, Scheuer PJ and Billing BH:
Effect of prolonged bile duct obstruction in the rat on hepatic
transport of bilirubin. Clin Sci (Lond). 68:341–347. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huang Q, Liu C, Zhu C, Xie F and Hu S:
Postoperative anastomotic bile duct stricture is affected by the
experience of surgeons and the choice of surgical procedures but
not the timing of repair after obstructive bile duct injury. Int J
Clin Exp Pathol. 7:6635–6643. 2014.PubMed/NCBI
|
|
15
|
McIntyre N and Rosalki S: Biochemical
investigations in the management of liver diseaseHepatobiliary
Diseases. Springer; Berlin: pp. 39–71. 1992, View Article : Google Scholar
|
|
16
|
Nehéz L and Andersson R: Compromise of
immune function in obstructive jaundice. Eur J Surg. 168:315–328.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Scopa CD, Koureleas S, Tsamandas AC,
Spiliopoulou I, Alexandrides T, Filos KS and Vagianos CE:
Beneficial effects of growth hormone and insulin-like growth factor
I on intestinal bacterial translocation, endotoxemia, and apoptosis
in experimentally jaundiced rats. J Am Coll Surg. 190:423–431.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sinenchenko GI, Kabanov Mlu and Tikhonchuk
SV: Perspectives of using ozonized solutions in complex treatment
of patients with mechanical jaundice. Vestn Khir Im I I Grek.
163:91–94. 2003.(In Russian).
|
|
19
|
Shibayama Y: Endotoxaemia and hepatic
injury in obstructive jaundice. J Pathol. 159:335–339. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang Z and Zou S: Extrahepatic biliary
ductBiliary Surgery. Beijing: People's Medical Publishing House;
pp. 23–26. 2010, (In Chinese).
|
|
21
|
Lv Y, Han X, Gong X, Wu H, Liu N, Hu Y,
Deng J, Li Y and Li Q: Etiological classification of bile duct
dilatation and proportion of each cause in 1430 patients. Int J New
Technol Res. 1:51–54. 2015.
|
|
22
|
Kordzaia D and Jangavadze M: Unknown bile
ductuli accompanying hepatic vein tributaries (experimental study).
Georgian Med News. 234:121–129. 2014.
|
|
23
|
Lv Y and Dang J: Diagnostics and
therapeutics of intra-extrahepatic cholangiectasis (Chinese
edition). Science Press. 1:319–321. 2014.
|
|
24
|
Tag CG, Weiskirchen S, Hittatiya K, Tacke
F, Tolba RH and Weiskirchen R: Induction of experimental
obstructive cholestasis in mice. Lab Anim. 49 1 Suppl:70–80. 2015.
View Article : Google Scholar : PubMed/NCBI
|