Introduction
Cardiac arrest is a common event in clinical
practice and is caused by a number of different factors (1). Cardiac arrest can occur within and
external to the hospital. According to statistics, the yearly
incidence of out-of-hospital cardiac arrest is ~38/10 million,
while the incidence of in-hospital cardiac arrest is ~1–5/1,000
(2).
Ischemic heart disease resulting from coronary heart
disease is the most common cause of cardiac arrest (3). Cardiopulmonary resuscitation (CPR) is
an efficient method to improve the survival rate of patients with
cardiac arrest. At present, the success rate of cardiopulmonary
resuscitation is ~23.8% (4).
However, many patients admitted to hospital following successful
resuscitation, die of post-cardiac arrest syndrome prior to
discharge (5).
The incidence of clinical brain death following
cardiac arrest and the sustained return of spontaneous circulation
(ROSC) ranges from 8–16% (6). Only a
minority of patients experience optimal neurological and functional
recovery following treatment. The primary reason for this outcome
is the development of sustained brain injury. Cardiac arrest and
subsequent cardiopulmonary resuscitation is a complex process of
ischemia-reperfusion. Brain damage can occur during ischemic and
reperfusion periods, leading to severe neurological dysfunction in
patients following ROSC (7).
Patients with brain injury exhibit coma, epilepsy, muscle spasms,
varying degrees of recognition dysfunction and brain death
(8–10). These symptoms often occur within h to
a days following ROSC (11,12). Recovery of brain function is an
indicator of the success rate of CPR and therefore methods of
evaluating this and the degree of brain damage following CPR are
important for critical care practitioners. Injury and mitochondrial
ATP-sensitive potassium channels (mitoKATPs) have received
increasing attention due to advancements into understanding the
effects of ischemia and hypoxia in the heart and brain. Nicorandil
is a nitrate ester capable of opening mitoKATPs, which is currently
used to treat angina (13).
MitoKATPs are able to protect against myocardial ischemia and
reperfusion injury by reducing oxidative stress, preventing calcium
overload, maintaining mitochondrial function and structural
integrity, and inhibiting apoptosis (14–16).
Previous studies have revealed that neuronal cells express 6- to
7-fold more mitoKATPs as the myocardium and it has been
demonstrated that mitoKATPs exist in the brain tissue (17,18).
Studies assessing the protective effects of nicorandil in the brain
have demonstrated that its protective function is mediated by the
activation of mitoKATPs (19,20). It
has also been determined that premedication with nicorandil induces
a cerebroprotective effect in patients receiving liver transplants
(21). However, the protective
effect of nicorandil in brain tissue following CPR remains unknown.
Therefore, the present study assessed whether nicorandil exhibits a
protective effect against cerebral injury in a swine model of
cardiac arrest.
Materials and methods
Ethical approval
All trials were conducted with the approval of the
Animal Care and Use Committee of Shandong Province Hospital
Affiliated to Shandong University (Shandong, China). All animals
received humane care in compliance with the Guide for the Care and
Use of Laboratory Animals published by the National Institutes of
Health (22).
Animal preparation
Healthy male inbred landrace domestic pigs were
obtained from Shandong laboratory animal center (Jinan, China). A
total of 20 pigs, (age, ~2 months; weight, 25±2 kg) were divided
into three groups as follows: The sham group (n=4), the control
group (n=8) and the nicorandil group (n=8). All animals were housed
in the same environment for 1 week in which the room temperature
was set to 26°C with a relative humidity of 50±10% and a 12 h
light/dark cycle and all allowed free access to food and water.
The pigs were fasted overnight with ad
libitum access to water prior to surgery. Pigs then received an
intramuscular injection of midazolam (0.5 mg/kg, Jiangsu Nhwa
Pharmaceutical Co., Ltd., Jiangsu, China.) followed by an
intravenous (i.v.) injection of 3% pentobarbital sodium (8 mg/kg,
cat. no. P3761; Sigma Chemical Co.; Sigma-Aldrich, Darmstadt,
Germany) in the ear vein. Anesthesia was maintained with
pentobarbital (8 mg/kg/h; i.v.), which was also administered into
the ear vein.
A cuffed 7 mm endotracheal tube was inserted into
the trachea and animals were mechanically ventilated using a
volume-controlled ventilator (8417801–22; Dräger Medical GmbH,
Lübeck, Germany) at a tidal volume of 12 ml/kg, with the apparatus
set for synchronized intermittent mandatory and pressure support
ventilation. Pressure support ventilation included 10 cm
H2O and 21% FiO2. End-tidal CO2
partial pressure was monitored continuously using an infrared
capnograph. Respiratory frequency was adjusted to maintain an
end-tidal CO2 pressure of 35–40 mmHg. Lead II of the
surface electrocardiograph was monitored continuously throughout
the present study using a Philips monitor (M8003A; Philips Medizin
Systeme Böeblingen GmbH, Böeblingen, Germany).
The right femoral artery was dissected to insert a
fluid-filled catheter to measure mean arterial blood pressure using
a pressure transducer. Cardiac output was measured by
thermodilution using a pulse contour cardiac output monitor. The
right external jugular vein was dissected to insert a 5F catheter
for the insertion of bipolar pacing electrodes into the right
ventricle to induce ventricular fibrillation (VF).
Experimental procedure
Following surgery, animals were allowed to stabilize
for 30 min to achieve constant resting levels. Bipolar pacing
electrodes were inserted into the right ventricle and set at the
esophageal output S1S2 mode (300/200 ms), 8:1 ratio and 10-ms step
continuous electrical stimulation until VF was induced using an
external programmable electrical stimulator (DF-5A; KaiFeng
Qingtianweiye Flow Instrument Co., Ltd., Kaifeng, Henan, China). VF
was identified by an abrupt drop in arterial blood pressure and
from the appearance of a VF waveform on the electrocardiograph. VF
was maintained for 4 min and mechanical ventilation was attenuated
during VF.
Following 4 min untreated VF, manual chest
compressions were performed for at least 2 min at a frequency of
100 beats/min. Compression and relaxation times were divided evenly
and the compression depth was 25% of the anterior/posterior
diameter of the chest. Following 2 min compressions, electric
defibrillation was performed (150-J biphasic shocks) using a
defibrillator (LIFEPAK20; Medtronic, Inc., Minneapolis, MN, USA).
If VF waves persisted, CPR was continued for a further 2 min,
followed by a second electrical defibrillation (200-J biphasic
shocks). This continued until ROSC was observed, which was defined
as a mean systolic arterial pressure >60 mmHg lasting for ≥10
min without pharmacological support or manual chest compressions.
Pig mortality was determined if no observable ROSC was measured
following 15 min.
Groups and drug delivery methods
After successful resuscitation, animals underwent
intensive care for 6 h and mechanical ventilation was resumed using
pre-cardiac arrest settings. Following successful resuscitation, 16
pigs achieved ROSC and were divided randomly into nicorandil and
control treatment groups (n=8 per group). Pigs in the nicorandil
group received an i.v. infusion of nicorandil (150 µg/kg; Beijing
Pharmaceutical Co., Ltd., Beijing, China) at the onset of ROSC,
followed by a second 3 µg/kg/min infusion until reperfusion was
achieved. While pigs in the control group received an equivalent
volume of 0.9% physiological saline solution following ROSC. A
total of 4 pigs were placed into a sham group and received surgery
without VF induction. All experimental animals were euthanized with
i.v. pentobarbital (150 mg/kg) 6 h following ROSC.
Biochemical assay
Venous blood samples were collected at 0, 5 min,
0.5, 3 and 6 h following ROSC. Clotted blood was centrifuged at 4°C
for 10 min at a speed of 1,760 × g. The resulting serum was removed
and stored at −80°C for subsequent analysis. ELISA kits were
utilized at room temperature to determine the serum concentrations
of neuron-specific enolase (NSE; cat. no. EIA06130P), S100β (cat.
no. EIA06308P), tumor necrosis factor α (TNF-α; cat. no. EIA06460P)
and interleukin 6 (IL-6; cat. no. EIA05884P) in 96-well plates. All
ELISA kits were sourced from Bio-swamp Life Science Lab (Shanghai,
China). The results were calibrated with hemoglobin values as
follows: Calibrated value=(analytic result ×100)/hemoglobin value
(g/l).
Histopathological and ultrastructural
observations of cerebral cortex
Following the euthanasia of pigs, the cerebral
cortex was immediately removed. Samples (~1.5×1.5×0.3
cm3) were removed and quickly fixed in 4%
paraformaldehyde for 24 h at room temperature. After being
processed by routine histological procedures, the samples were cut
into 4 µm sections. Sections were then stained using hematoxylin
for 5 min at 40°C and eosin solution for 1 min at room temperature.
The slides were then observed using an optical microscope at a
magnification of 100×. Additionally, Brain tissue was sliced into a
tissue block of 1 mm3. Samples were then placed in 2%
glutaraldehyde overnight for fixation at 4°C, rinsed 3 times with
0.2 mol/l phosphate buffer and fixed with 2% osmium acid for 2 h,
Samples were further rinsed with 0.2 mol/l phosphate buffer 3
times. Degradation using a gradient of ethanol and embedded in
epoxy resin. The tissues were then cut into 50 nm slices. Sliced
sections were double stained with uranium lead (3% uranyl acetate
for 15 min and lead lemon solution for 10 min) at room temperature
and then observed and photographed using a transmission electron
microscope (JEM-1200EX; JEOL Ltd., Tokyo, Japan). Western
blotting determination of aquaporin-4 (AQP-4) content. Segments
of brain tissue were homogenized in 10 µl/mg lysis solution and
centrifuged at 4°C at a speed of 12,000 × g for 30 min. A small
quantity of supernatant was removed for protein quantification
using a BCA protein assay kit (P0012 BCA; Beyotime Institute of
Biotechnology, Haimen, China). A total of 100 µg protein was loaded
per lane and separated using 10% sodium dodecyl
sulfate-polyacrylamide gel electrophoresis. Proteins were
electrically transferred to a polyvinylidene fluoride membrane. The
membranes were then blocked with 5% skimmed milk with Tris-buffered
saline containing Tween-20 (TBST) for 2 h at room temperature.
These were then incubated with primary antibodies (AQP-4; 1:1,000;
cat. no. ab46182; Abcam, Cambridge, UK and GAPDH; 1:1,000; cat. no.
ab22555; Abcam) at 4°C for 13 h and washed three times in
Tris-buffered saline with Tween 20. Proteins were then incubated
with a secondary antibody (horseradish peroxidase-labeled goat
anti-rabbit; 1:5,000; cat. no. ZB-2301; OriGene Technologies, Inc.,
Beijing, China) at room temperature for 1 h. The membranes were
then washed and signals were detected using an enhanced
chemiluminescence (ECL-Plus) reagent (EMD Millipore, Billerica, MA,
USA). Band images were scanned and densitometric analysis of the
western blots was performed (Tanon-5200; Tanon Science &
Technology Co., Ltd., Shanghai, China). Quantitative analysis of
western blotting was performed using ImageJ 1.41 software (National
Institutes of Health, Bethesda, MD, USA).
Determination of malondialdehyde (MDA)
and glutathione (GSH) levels in brain tissue
Animals were euthanized 6 h post-ROSC and the
cerebral cortex was immediately removed. MDA levels were
subsequently determined using the thiobarbituric acid colorimetric
method (MDA assay kit; Nanjing Jiancheng Bioengineering Institute,
Nanjing, China) and GSH content was determined using the
thiobenzoic acid colorimetric method (GSH peroxidase assay kit;
Nanjing Jiancheng Bioengineering Institute).
Statistical analysis
Data were analyzed using SPSS 21.0 (IBM Corp.,
Armonk, NY, USA). All data are expressed as the mean ± standard
deviation. Comparisons between multiple groups and times were made
using one-way analysis of variance, followed by post-hoc least
significant difference tests. P<0.05 was considered to indicate
a statistically significant result.
Results
CPR and basic characteristics
The baseline characteristics of the 3 groups prior
to ROSC were compared (Table I).
There were no significant differences in body weight, heart rate,
mean aortic blood pressure, cardiac output or body temperature
among the 3 groups. Additionally, there were no significant
differences in the number of electrical defibrillations or doses of
epinephrine administered during CPR prior to ROSC between the
nicorandil and control groups (Table
II).
 | Table I.Baseline characteristics. |
Table I.
Baseline characteristics.
| Characteristic | Nicorandil
(n=8) | Control (n=8) | Sham (n=4) | F | P-value |
|---|
| Heart rate
(BPM) | 125.60±6.54 | 124.80±6.42 | 120.67±7.02 | 0.564 | 0.586 |
| Weight (kg) | 25.80±0.84 | 25.00±1.41 | 25.00±1.00 | 0.048 | 0.953 |
| Temperature
(°C) | 37.96±0.29 | 38.06±0.31 | 37.90±0.30 | 0.293 | 0.752 |
| Cardiac output
(l/min) | 4.49±0.20 | 4.48±0.09 | 4.52±0.09 | 0.057 | 0.944 |
| MAP (mmHg) | 115.20±5.45 | 115.80±5.31 | 111.33±4.16 | 0.769 | 0.489 |
 | Table II.Resuscitation outcomes. |
Table II.
Resuscitation outcomes.
| Characteristic | Nicorandil
(n=8) | Control (n=8) |
|---|
| Total adrenaline
dose (mg) | 0.40±0.042 | 0.30±0.045 |
| Time to ROSC
(min) | 2.40±1.41 | 2.20±1.30 |
| Energy of
defibrillation (J) | 185.00±78.26 | 220.00±95.85 |
| Number of
defibrillations | 1.20±0.45 | 1.40±0.55 |
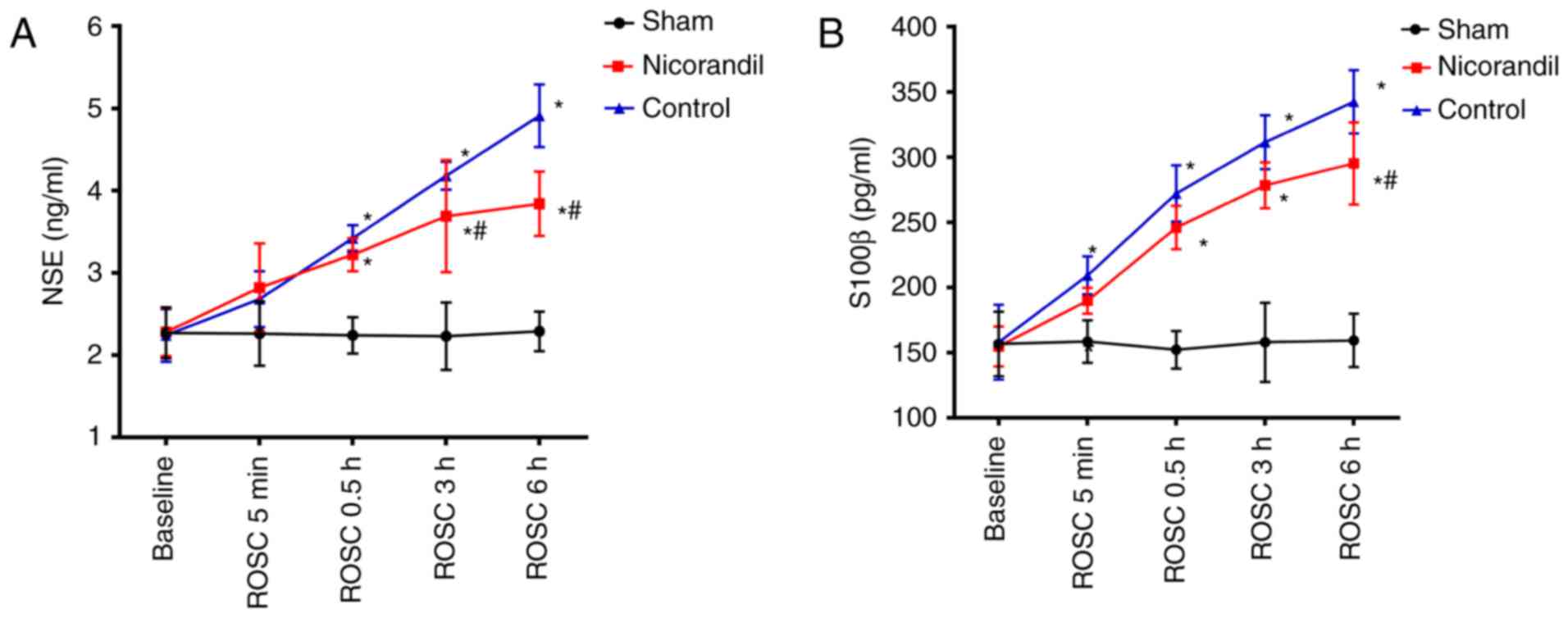
Serum NSE and S100β levels
The serum levels of NSE and S100β were compared
among the 3 groups at different times to determine the effects of
nicorandil on brain injury (Fig. 1).
There were no significant differences in the serum levels of NSE or
S100β among the three groups at baseline. However, NSE and S100β
levels in the nicorandil and control group significantly increased
at 0.5, 3 and 6 h following ROSC, compared with the sham group
(P<0.05). Control groups were significantly increased compared
with the sham group at 5 min 0.5, 3 and 6 h following ROSC
(P<0.05). Serum NSE levels in the nicorandil group were
significantly lower than that of the control group (P<0.05) at 3
and 6 h following ROSC. Furthermore, serum levels of S100β were
significantly decreased in the nicorandil group compared with the
control group 6 h following ROSC (P<0.05).
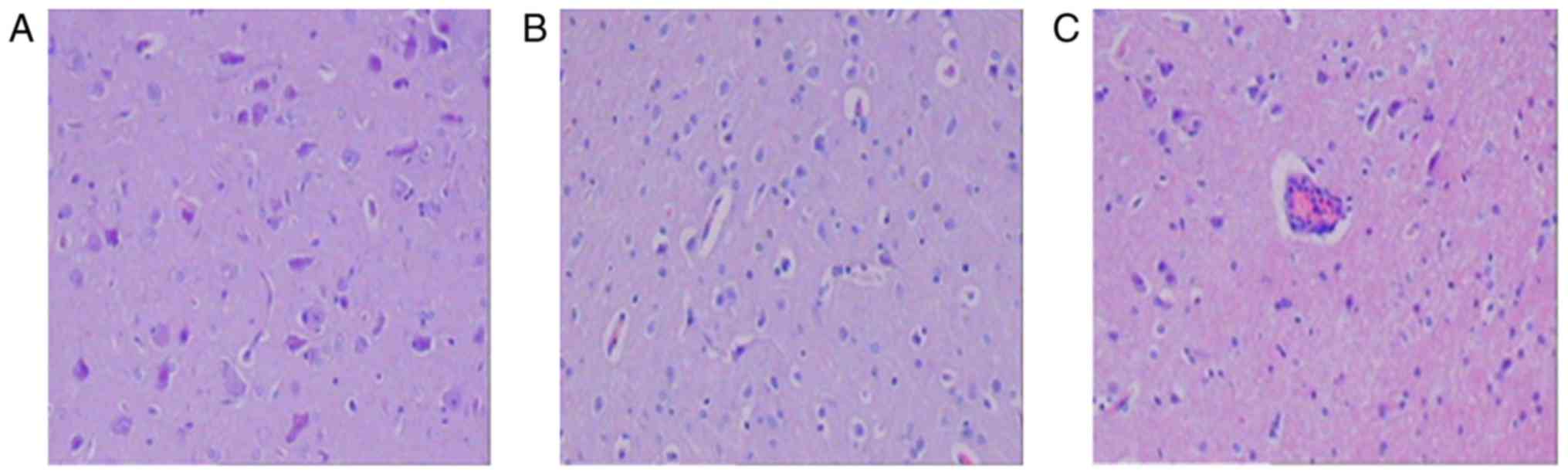
H&E staining and brain
ultramicrostructure
Pathological changes in brain structures were
examined by performing H&E staining (Fig. 2). At 6 h following ROSC, neuronal
structures in the sham group were normal (Fig. 2A); however, cells from the control
group exhibited lymphocyte infiltration around the blood vessels
and swelling (Fig. 2C). Cells from
the nicrorandil group also exhibited swelling but to a lesser
extent than cells from the control group (Fig. 2B).
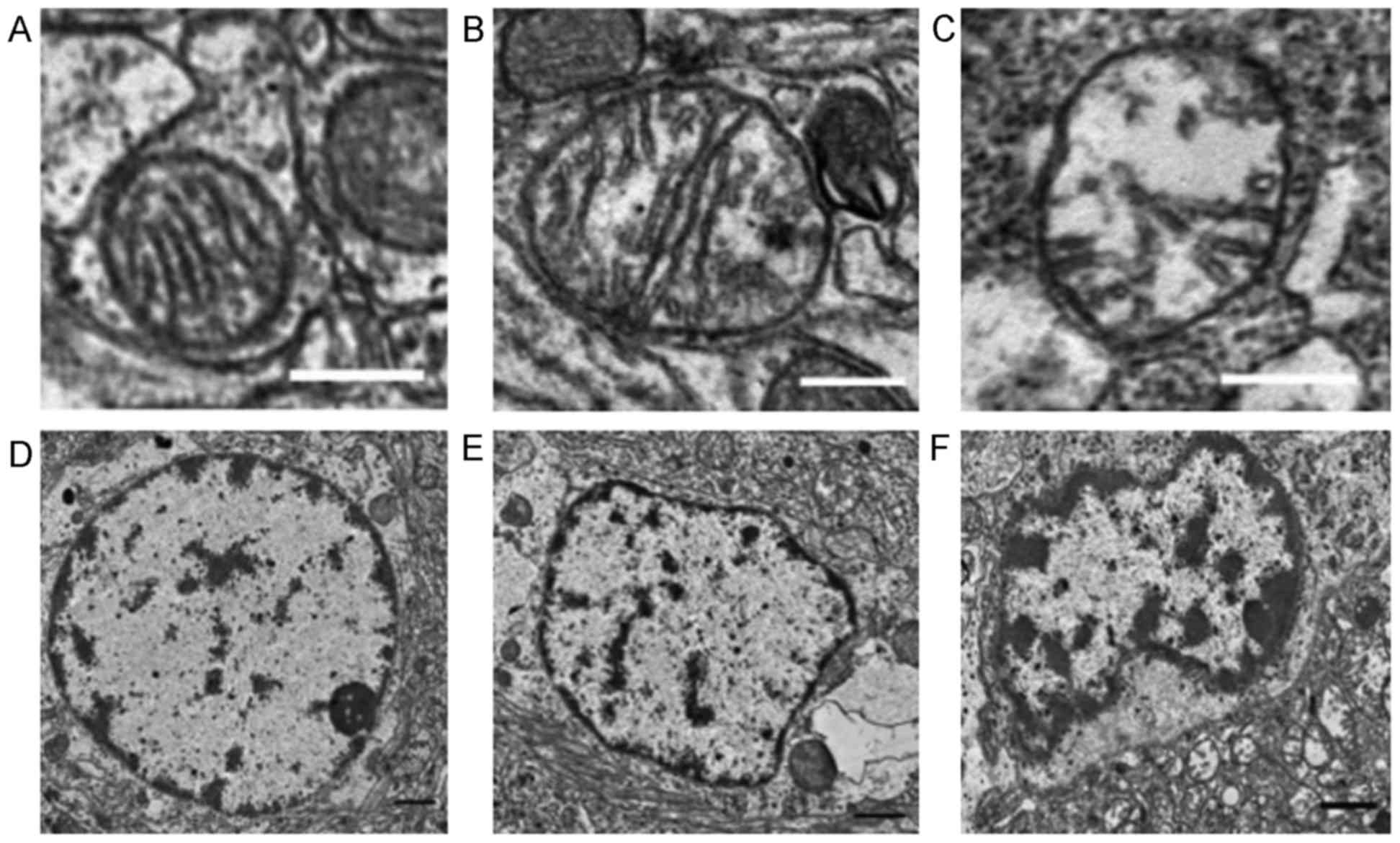
The ultrastructure of the cerebral cortex was normal
in the sham group 6 h following ROSC, as determined by electron
transmission microscopy (Fig. 3).
Nuclei in the nicorandil and control groups exhibited partial
dissolution, condensation and nuclear membrane depression, although
this was exhibited to a greater extent in the control group. The
nicorandil group also exhibited mild mitochondrial edema, with
clear, visible cristae ridges that were less characteristic of
necrosis. The control group exhibited a greater severity of
mitochondrial edema than the nicorandil group; this included the
loss of the mitochondrial bilayer and cristae ridges, as well as
evidence of vacuolar changes.
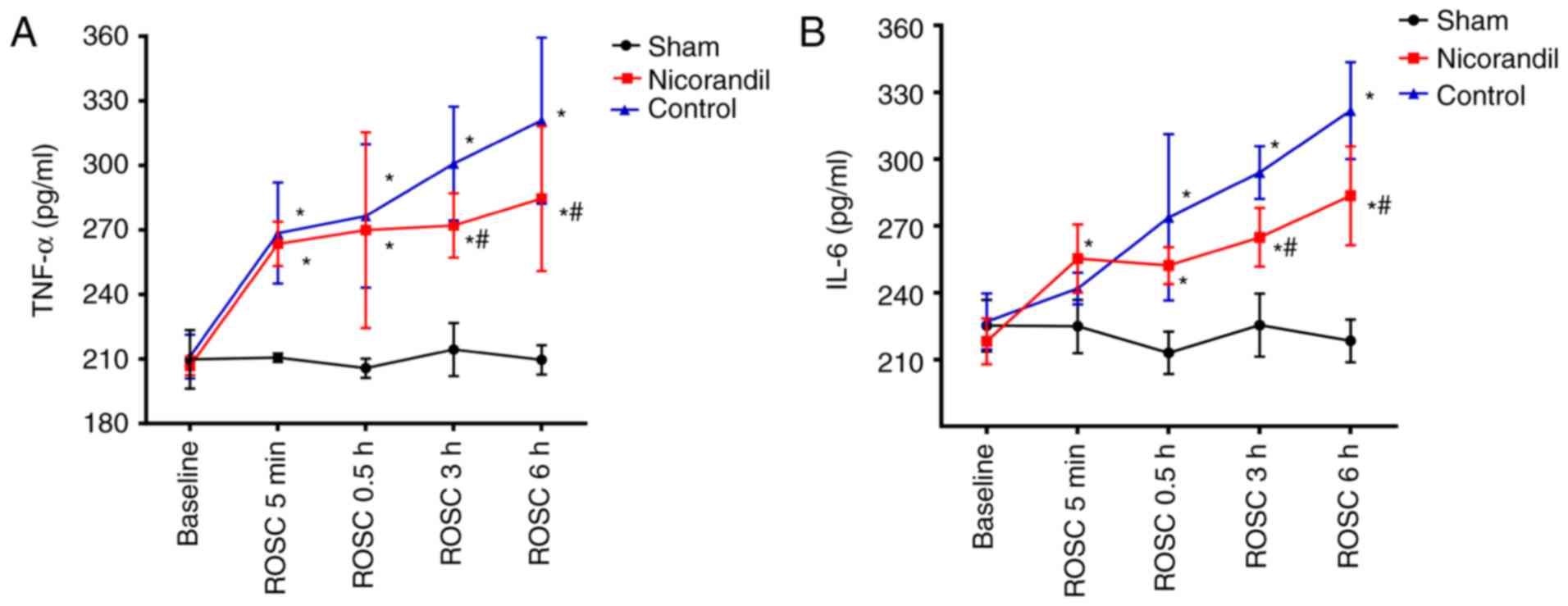
Serum TNF-α and IL-6
concentrations
There were no significant differences in TNF-α and
IL-6 levels in the cerebral cortex among the 3 groups at baseline
(Fig. 4). Levels of TNF-α were
significantly higher in the nicorandil and control groups, compared
with the sham group (P<0.05) at 5 min and 0.5, 3 and 6 h
following ROSC (Fig. 4A). IL-6
levels were significantly higher in the control and nicorandil
groups 0.5, 3 and 6 h following ROSC compared with the sham group
(Fig. 4B). However, TNF-α and IL-6
levels in the nicorandil group were significantly lower than those
in the control group 3 and 6 h post-ROSC (P<0.05).
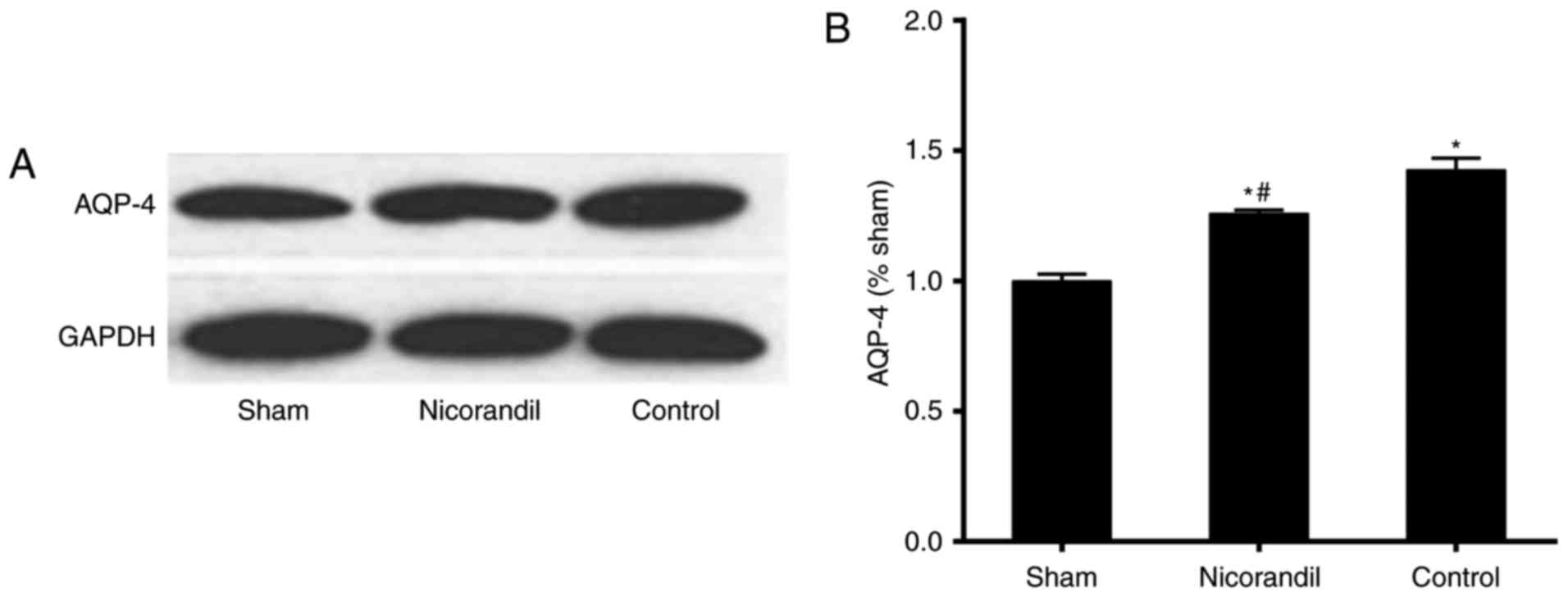
AQP-4 levels in brain tissue
Levels of AQP-4 in brain tissue were significantly
higher in the nicorandil and control groups compared with the sham
group 6 h following ROSC (Fig. 5).
However, AQP-4 levels were significantly lower in the nicorandil
group than in the control group 6 h following ROSC (P<0.05).
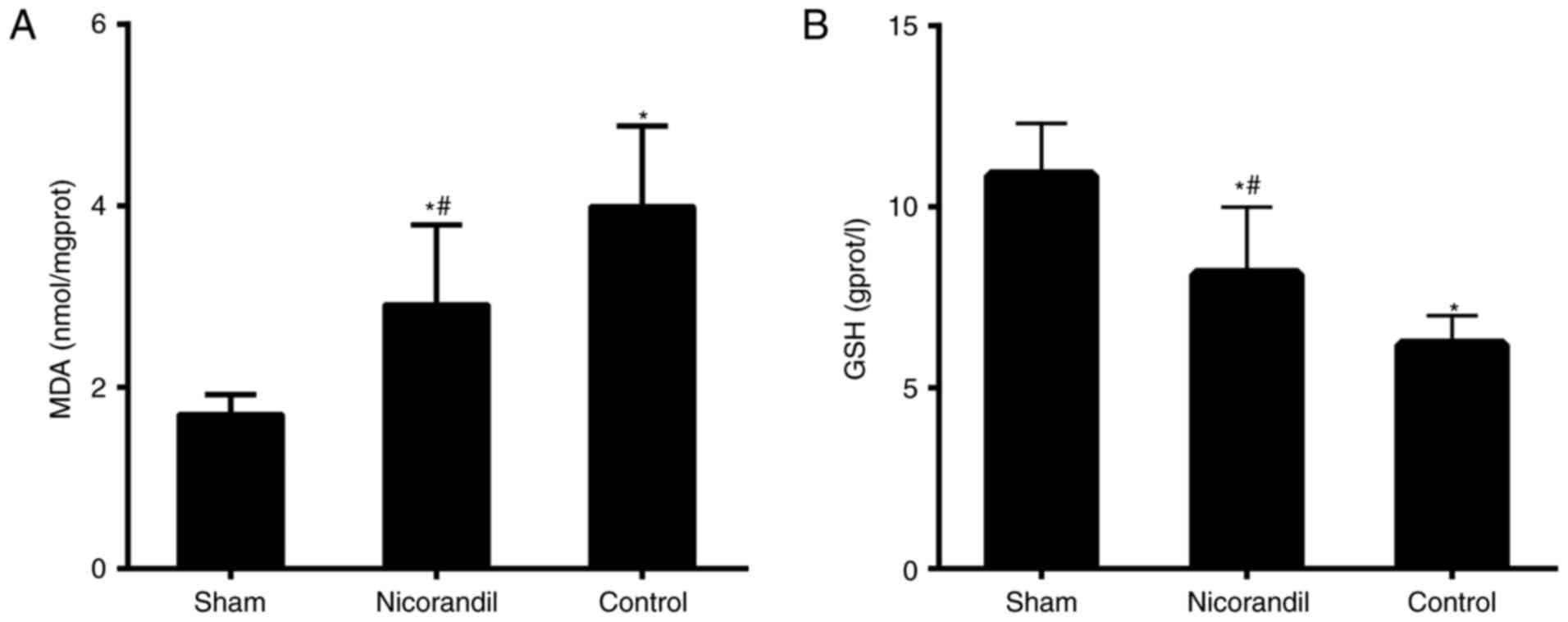
MDA and GSH levels in the cerebral
cortex
MDA levels in the cerebral cortex were significantly
higher in the nicorandil and control groups compared with the sham
group 6 h following ROSC (P<0.05; Fig. 6A). However, MDA levels were
significantly lower in the nicorandil group compared with the
control group. GSH levels were significantly lower in the control
and nicorandil groups, compared with the sham group (P<0.05;
Fig. 6B). Furthermore, GSH levels in
the nicorandil group were significantly higher than in the control
group (P<0.05).
Discussion
The results of the present study demonstrated that
cardiac arrest followed by CPR causes significant damage to swine
brain tissue. Electron microscopy and pathological examinations of
the cerebral cortex and cellular ultrastructure revealed that nerve
cell mitochondria were damaged and that NSE and S100β levels were
significantly increased. However, treatment with nicorandil
attenuated the increase in NSE and S100β following CPR and reduced
the degree of mitochondrial swelling, indicating that nicorandil
induces a protective effect following brain injury.
Serum NSE and S100β levels were assessed to
determine their potential as neurobiochemical markers of brain
damage. NSE is localized in the neuronal and neuroendocrine cell
cytoplasm; however, it is also present in small quantities in serum
and cerebrospinal fluid. In the event of neuronal necrosis, cells
become leaky, leading to an increase in NSE serum levels (23). S100β is an EF-hand-type
calcium-binding protein with a low molecular weight and is abundant
in brain tissue (24). In certain
types of brain injury involving damage to the blood-brain barrier,
S100β may enter the cerebrospinal fluid and bloodstream. Various
microproteins, including S100β and NSE can therefore be detected in
the blood (25,26). Rundgren et al (27) identified that NSE and S100β predict
the severity of brain injury following CPR. The results of the
current study demonstrated that nicorandil reduces serum levels of
NSE and S100β following CPR, indicating that it serves a protective
role against brain damage.
Cardiac arrest affects the central nervous system
and results in whole-brain structural injury and functional damage,
the severity of which directly affects patient prognosis. Despite
the implementation of CPR, further brain damage may occur in the
reperfusion phase of cardiac arrest, due to the accumulation of
free radicals, the systemic inflammatory response and mitochondrial
damage (28,29).
The results of the present study demonstrated that
TNF-α and IL-6 levels in pigs increased rapidly following
resuscitation in VF cardiac arrest and remained elevated during the
initial 6 h following ROSC. TNF-α and IL-6 are upregulated
following cerebral ischemia and it has been demonstrated that
transient global ischemia, induced by cardiac arrest, increases
IL-6 and TNF-α levels in rat hippocampi (30). In the current study, the serum levels
of these pro-inflammatory cytokines were significantly reduced
following treatment with nicorandil, indicating that it exhibits
protective effects against brain injury.
AQPs are channels located in the cell membrane that
transport water to regulate intra- and extracellular environments.
Intracerebral AQP-4 is primarily expressed in capillary endothelial
cells and in the foot process of astrocytes located on the
blood-brain barrier (BBB). Previous studies have therefore
speculated that AQP-4 may serve an important role in mediating the
transport of water across the BBB (31,32). It
has been demonstrated that AQP-4 expression is upregulated
following cardiac arrest and CPR in rats (33). Furthermore, a positive association
between cerebral edema and AQP-4 expression has been identified,
indicating that AQP-4 is involved in ischemic brain damage and
edema formation (34). The results
of the present study demonstrated that nicorandil reduces AQP-4
expression in brain tissue, which may have protected the brain by
reducing the degree of edema following CPR.
The brain is a lipid-rich organ, in which oxidation
and antioxidation are maintained in a balanced state. However,
ischemia, hypoxia or ischemia-reperfusion brain injury produces
large quantities of oxygen free radicals, which induce oxidative
stress and brain damage (35). MDA
is a major metabolite of lipid peroxidation that is induced by
reactive oxygen species and therefore may indicate the degree of
oxidative stress present. GSH is also an important antioxidant and
scavenger of free radicals (36). In
the present study, levels of GSH and MDA in the 3 experimental
groups were assessed. It was demonstrated that nicorandil increases
GSH and decreases MDA levels, indicating that it reduces oxidative
damage and thus exerts a protective effect in the brain.
Neurons contain two types of ATP-sensitive potassium
channels: MitoKATPs and intima-ATP-sensitive potassium channels
(18,37). MitoKATPs maintain the mitochondrial
K+ balance, thus controlling volume changes in the
mitochondrial matrix (18). It is
also involved in K+ reuptake, compensating for the
charge transfer in oxidative phosphorylation generated by proton
pumps, thus maintaining the stability of the pH gradient and
transmissive potential difference (38). Nicorandil is a selective mitoKATP
agonist (13). It has been
demonstrated in vitro that nicorandil protects the brain
from oxidative stress by activating mitoKATPs (19). In addition, nicorandil has been
revealed to function as a nitrate ester (39). Therefore, its protective effects may
be associated with its vasodilator activity in the brain.
The present study demonstrated that nicorandil
exerts a protective effect against brain injury by reducing
oxidative damage, the inflammatory response and brain edema in a
swine model of cardiac arrest. However, there were several
limitations of the present study. There are numerous physiological
differences between healthy experimental animals and human
patients, making it difficult to extrapolate the results of this
swine model to the relevant clinical situations. Furthermore, the
results of the present study were limited by the small quantity of
animals utilized. Therefore, large-scale studies in animal models
and human subjects are required for future studies.
In conclusion, the results of the present study
demonstrated that nicorandil exerts a protective effect against
brain injury following cardiac arrest by reducing the oxidative
damage, the inflammatory response and brain edema that occur
post-ROSC.
Acknowledgements
The authors of the present study give thanks to Mr.
Jinsen Huang and Mr Bao Zhao (Shandong Provincial Hospital
Affiliated to Shandong University, China) for technical
assistance.
Funding
The present study was supported by the Chinese
National Natural Science Foundation (grant no. 81471833) and the
2012 Jinan Science and Technology Development Plan (grant no.
201219007).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DS and XJ designed and directed the experiment. FZ,
YZ, ZH, HH, LL, JC and QC performed the experiments. XZ performed
the statistical analysis. FZ and XZ wrote the manuscript. DS and XJ
reviewed and edited the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
All trials were conducted with the approval of the
Animal Care and Use Committee of Shandong Province Hospital
Affiliated to Shandong University (Shandong, China). All animals
received humane care in compliance with the Guide for the Care and
Use of Laboratory Animals published by the National Institutes of
Health.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sadaka F, Doerr D, Hindia J, Lee KP and
Logan W: Continuous electroencephalogram in comatose postcardiac
arrest syndrome patients treated with therapeutic hypothermia:
Outcome prediction study. J intensive care med. 30:292–296. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Deakin CD, Nolan JP, Soar J, Sunde K,
Koster RW, Smith GB and Perkins GD: European resuscitation council
guideline for resuscitation 2010 section 4. Adult advanced life
support. Resuscitation. 81:1305–1352. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pell JP, Sirel JM, Marsden AK, Ford I,
Walker NL and Cobbe SM: Presentation, management and outcome of out
of hospital cardiopulmonary arrest: Comparison by underlying
aetiology. Heart. 89:839–842. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nolan JP, Soar J, Wenzel V and Paal P:
Cardiopulmonary resuscitation andmanagement of cardiac arrest. Nat
Rev Cardiol. 9:499–511. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Neumar RW, Nolan JP, Adrie C, Aibiki M,
Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC,
et al: Post-cardiac arrest syndrome: Epidemiology, pathophysiology,
treatment and prognostication. A consensus statement from the
international liaison committee on resuscitation (American Heart
Association, Australian and New Zealand Council on Resuscitation,
European Resuscitation Council, Heart and Stroke Foundation of
Canada, Inter American Heart Foundation, Resuscitation Council of
Asia and the Resuscitation Council of Southern Africa); the
American Heart Association Emergency Cardiovascular Care Committee;
the Council on Cardiovascular Surgery and Anesthesia; the Council
on Cardiopulmonary, Perioperative and Critical Care; the Council on
Clinical Cardiology; and the Stroke Council. Circulation.
118:2452–2483. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Adrie C, Haouache H, Saleh M, Memain N,
Laurent I, Thuong M, Dargues L, Geurrini P and Monchi M: An
underrecognized source of organ donors: Patients with brain death
after successfully resuscitated cardiac arrest. Intensive Care Med.
34:132–137. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Safar P, Behringer W, Bottiger BW and
Sterz F: Cerebral resuscitation potentials for cardiac arrest. Crit
Care Med. 30 4 Suppl:S140–S144. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Krumholz A, Stern BJ and Weiss HD: Outcome
from coma after cardiopulmonary resuscitation: Relation to seizures
and myoclonus. Neurology. 38:401–405. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pusswald G, Fertl E, Faltl M and Auff E:
Neurological rehabilitation of severely disabled cardiac arrest
survivors, part II: life situation of patients and families after
treatment. Resuscitation. 47:241–248. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Groswasser Z, Cohen M and Costeff H:
Rehabilitation outcome after anoxic brain damage. Arch Phys Med
Rehabil. 70:186–188. 1989.PubMed/NCBI
|
|
11
|
Taraszewska A, Zelman IB, Ogonowska W and
Chrzanowska H: The pattern of irreversible brain changes after
cardiac arrest in humans. Folia Neuropathol. 40:133–141.
2002.PubMed/NCBI
|
|
12
|
Lipton P: Ischemic cell death in brain
neurons. Physiol Rev. 79:1431–1568. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Horinaka S: Use of nicorandil in
cardiovascular disease and its optimization. Drugs. 71:1105–1119.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu H, Ye M, Yang J, Ding J, Yang J, Dong W
and Wang X: Nicorandil protects the heart from ischemia/reperfusion
injury by attenuating endoplasmic reticulum response-induced
apoptosis through PI3K/Akt signaling pathway. Cell Physiol Biochem.
35:2320–2332. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nagata K, Obata K, Odashima M, Yamada A,
Somura F, Nishizawa T, Ichihara S, Izawa H, Iwase M, Hayakawa A, et
al: Nicorandil inhibits oxidative stress-induced apoptosis in
cardiac myocytes through activation of mitochondrial ATP-sensitive
potassium channels and a nitrate-like effect. J Mol Cell Cardiol.
35:1505–1512. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Raveaud S, Verdetti J and Faury G:
Nicorandil protects ATP-sensitive potassium channels against
oxidation-induced dysfunction in cardiomyocytes of aging rats.
Biogerontology. 10:537–547. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lacza Z, Snipes JA, Kis B, Szabó C, Grover
G and Busija DW: Investigation of the subunit composition and the
pharmacology of the mitochondrial ATP-dependent K+ channel in the
brain. Brain Res. 994:27–36. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bajgar R, Seetharaman S, Kowaltowski AJ,
Garlid KD and Paucek P: Identification and properties of a novel
intracellular (mitochondrial) ATP-sensitive potassium channel in
brain. J Biol Chem. 276:33369–33374. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Teshima Y, Akao M, Baumgartner WA and
Marbán E: Nicorandil prevents oxidative stress-induced apoptosis in
neurons by activating mitochondrial ATP-sensitive potassium
channels. Brain Res. 990:45–50. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kurihara J, Ochiai N and Kato H:
Protection by nicorandil against the dysfunction of the central
vagal baroreflex system following transient global cerebral
ischemia in dogs. Br J Pharmacol. 109:1263–1267. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xia YF, Wang ZP, Zhou YC, Yan T and Li ST:
Cerebral protective effect of nicorandil premedication on patients
undergoing liver transplantation. Hepatobiliary Pancreat Dis Int.
11:132–136. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
National Research Council of The National
Academies: Guide for the Care and Use of Laboratory Animals. 8th
edition. The National Academies Press; Washington, DC: 2010
|
|
23
|
Marangos PJ, Schmechel DE, Parma AM and
Goodwin FK: Developmental profile of neuron-specific (NSE) and
non-neuronal (NNE) enolase. Brain Res. 190:185–193. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Heizmann CW, Fritz G and Schäfer BW: S100
proteins: Structure, functions and pathology. Front Biosci.
7:d1356–d1368. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cavus E, Bein B, Dörges V, Stadlbauer KH,
Wenzel V, Steinfath M, Hanss R and Scholz J: Brain tissue oxygen
pressure and cerebral metabolism in an animal model of cardiac
arrest and cardiopulmonary resuscitation. Resuscitation. 71:97–106.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ekmektzoglou KA, Xanthos T and
Papadimitriou L: Biochemical markers (NSE, S-100, IL-8) as
predictors of neurological outcome in patients after cardiac arrest
and return of spontaneous circulation. Resuscitation. 75:219–228.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rundgren M, Karlsson T, Nielsen N,
Cronberg T, Johnsson P and Friberg H: Neuron specific enolase and
S-100B as predictors of outcome after cardiac arrest and induced
hypothermia. Resuscitation. 80:784–789. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vereczki V, Martin E, Rosenthal RE, Hof
PR, Hoffman GE and Fiskum G: Normoxic resuscitation after cardiac
arrest protects against hippocampal oxidative stress, metabolic
dysfunction and neuronal death. J Cereb Blood Flow Metab.
26:821–835. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Richards EM, Fiskum G, Rosenthal RE,
Hopkins I and McKenna MC: Hyperoxic reperfusion after global
ischemia decreases hippocampal energy metabolism. Stroke.
38:1578–1584. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Xing J and Lu J: HIF-1α activation
attenuates IL-6 and TNF-α pathways in hippocampus of rats following
transient global ischemia. Cell Physiol Biochem. 39:511–520. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kleffner I, Bungeroth M, Schiffbauer H,
Schäbitz WR, Ringelstein EB and Kuhlenbäumer G: The role of
aquaporin-4 polymorphisms in the development of brain edema after
middle cerebral artery occlusion. Stroke. 39:1333–1335. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ho JD, Yeh R, Sandstrom A, Chorny I,
Harries WE, Robbins RA, Miercke LJ and Stroud RM: Crystal structure
of human aquaporin 4 at 1.8 Å and its mechanism of conductance.
Proc Natl Acad Sci. 106:7437–7442. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xiao F, Arnold TC, Zhang S, Brown C,
Alexander JS, Carden DL and Conrad SA: Cerebral cortical
aquaporin-4 expression in brain edema following cardiac arrest in
rats. Acad Emerg Med. 11:1001–1007. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wang H, Wang X and Guo Q: The correlation
between DTI parameters and levels of AQP-4 in the early phases of
cerebral edema after hypoxic-ischemic/reperfusion injury in
piglets. Pediatr Radiol. 42:992–999. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nunes C, Barbosa RM, Almeida L and
Laranjinha J: Nitric oxide and DOPAC-induced cell death: from GSH
depletion to mitochondrial energy crisis. Mol Cell Neurosci.
48:94–103. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Radak D, Resanovic I and Isenovic ER: Link
between oxidative stress and acute brain ischemia. Angiology.
65:667–676. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Dunn-Meynell AA and Rawson NE:
Distribution and phenotype of neurons containing the ATP-sensitive
K+ channel in rat brain. Brain Res. 814:41–54. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Garlid KD: Mitochondrial potassium
transport: The K(+) cycle. Biochim Biophys Acta. 1606:23–41. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tarkin J M and Kaski JC: Vasodilator
therapy: Nitrates and nicorandil. Cardiovasc Drugs Ther.
30:367–378. 2016. View Article : Google Scholar : PubMed/NCBI
|