Introduction
Upon lowering the head, the spinous process (SP) of
the seventh cervical vertebra (C7) of humans bulges to the skin and
forms a significant eminence on the back of the neck. The C7 is
usually identified by a long, club-shaped and unbranched SP
(1–3), referred to as vertebra prominens
(4). The C7 represents the bottom of
the cervical spine and connects with the top of the thoracic spine,
T1, to form the cervicothoracic junction, also referred to as
C7-T1. Thus, the C7 marks the level of transition from the dynamic
cervical segment to the relatively inflexible thoracic segment of
the vertebral column (1).
Furthermore, it is the point where cervical lordosis reverses into
thoracic kyphosis, making C7 anatomically unique (5). Of all cervical injuries, 9% occur at
the C7 segment, and the morphology of C7, which displays
inter-regional, inter-ethnic and individual variations, may affect
surgical approaches (6). Thus, the
morphology of the C7 is a clinically significant area of interest
in clinical practice (1).
In addition, C7-SP is of vital importance for
clinical examinations, diagnostic and therapeutic interventions and
various types of surgery involving the neck. For instance, C7-SP is
used as a point of reference for determining the level to insert
epidural catheters by anesthesiologists, and a C7-T1 level of entry
is recommended for cervical interlaminar epidural steroid injection
(7). In addition, owing to the
complex attachment of nuchal muscles to the spinous process, the SP
should be preserved to reduce the incidence of postoperative axial
pain (8). For the most part,
decisions regarding surgical treatment made by the physician are
affected by the anatomic characteristics of C7-SP. For instance,
when performing posterior cervical surgeries, surgeons often rely
on the morphology of C7-SP if the operation only involves the lower
cervical area. However, if the patient has a bifid C7-SP, this may
mislead the surgeons, which may result in undesired outcomes
(2). In addition, due to the
inter-individual deviation of C7-SP, the identification of suitable
approaches for inserting the screws when performing a posterior
fixation of the neck is challenging. Certain studies stressed that
a new pedicle screw should be inserted based on the
three-dimensional (3D) reconstruction as well as individualization
(9). Although numerous studies have
assessed the structures of C7-SP, most of them focused on the
dimensions and angulations of the pedicle, bifid condition and the
accurate ways to locate C7 (10–13).
However, the detailed anatomic characteristics of C7-SP have
remained to be elucidated.
Only a few reports have assessed the
inter-individual variation of C7-SP. In the present study, the
anatomic characteristics of the C7-SP were preliminarily measured
based on 3D computed tomography (CT) reconstruction, an imaging
tool that has been validated in a variety of applications for the
practice of spine surgery (14). The
objective of the present study was to explore the anatomical
features of C7-SP, which may facilitate the diagnosis and treatment
of conditions involving the cervical spine.
Patients and methods
Subjects
A total of 245 subjects were enrolled from January
2016 to August 2017 at the Affiliated Traditional Chinese Medicine
Hospital of Southwest Medical University (Luzhou, China). Prior to
the start of the study, approval was obtained from the Ethical
Inspection Committee of the Affiliated Traditional Chinese Medicine
Hospital of Southwest Medical University, which waived the
requirement for informed consent due to the retrospective nature.
The CT data of the C7 were collected at the Radiology Department of
the Affiliated Traditional Chinese Medicine Hospital of Southwest
Medical University. All patients were Han Chinese and >18 years
of age at the time of the CT scan. The majority of the patients had
been given a health examination, and the rest were given a special
examination the spine, as they had fallen prior to recruitment or
suffered accidental impacts, which may detrimentally affect the
spine. Individuals with congenital spinal malformation, spinal
pathology (including spondylolisthesis, retrolisthesis or disc
space collapse), spinal variation and those who had undergone
spinal surgeries were excluded.
3D reconstruction CT
A spiral CT scanner (Somatom Emotion; Siemens AG,
Munich, Germany) was used with the following scan conditions:
Voltage, 130 kV; current, 180 mA; thickness, 0.75 mm; and matrix
size, 512×512. In addition, the CARE Dose 4D technique was used in
the examination. All patients were kept in the supine position
during scanning. The 3D images were stored on the Picture Archiving
Communication System (PACS version 4.0; DJ HealthUnion Systems
Corporation, Shanghai, China). This was a system for recording and
storing radiographic images, permitting storage of large numbers of
images and allowing access from any networked station. In addition
to these storage facilities, PACS also incorporated a sensitive
measuring tool. After 3D reconstruction, the C7 was individually
analyzed. Typical C7 images were acquired by adjusting the position
and size, increasing the contrast and making other image
adjustments on the CT workstation prior to measuring.
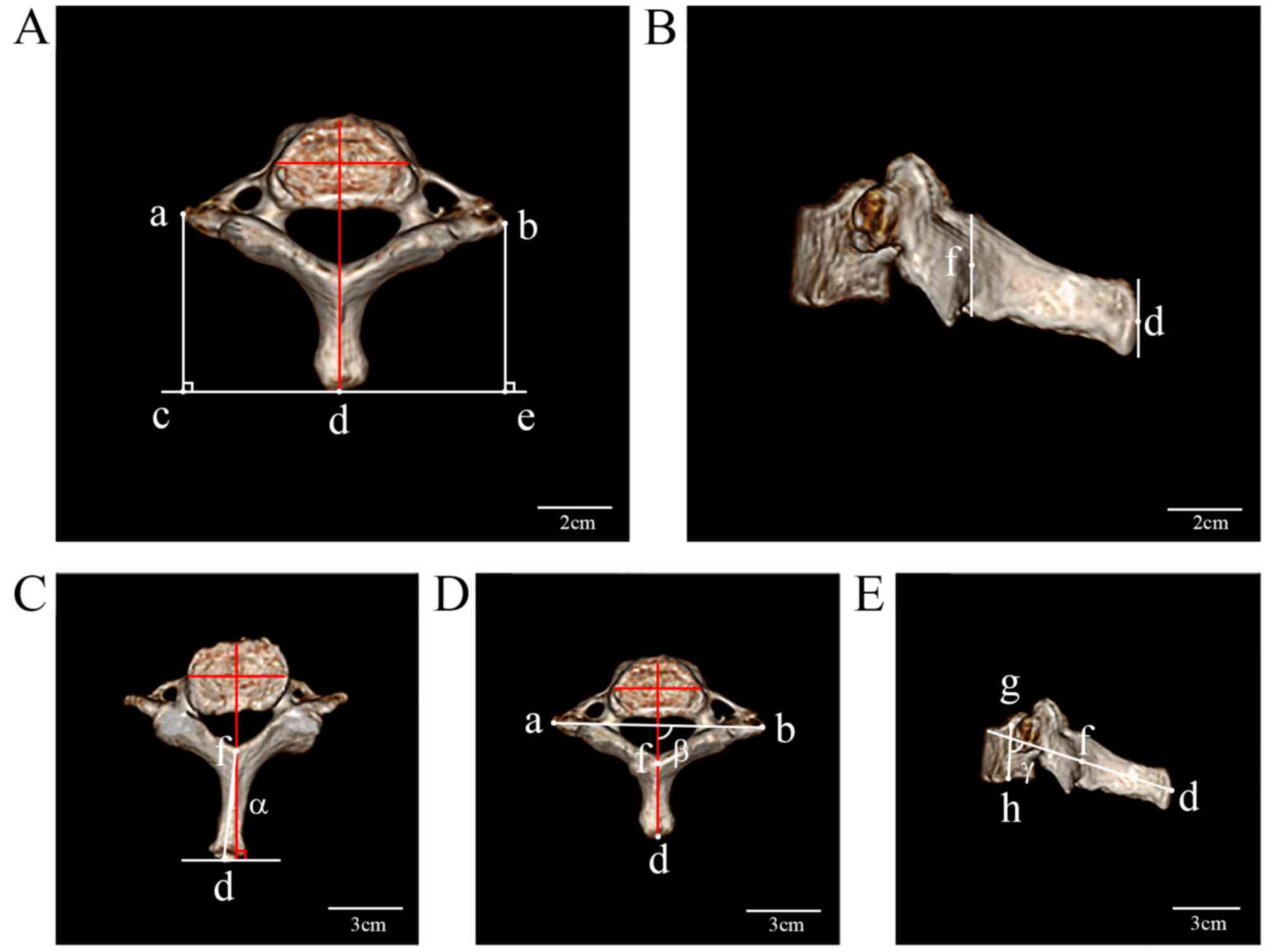
Measurement of C7-SP parameters
All measurements were performed by three
radiologists who had performed in CT-associated work for >5
years at the Radiology Department of the Affiliated Traditional
Chinese Medicine Hospital of Southwest Medical University. The
lateral, superior and posterior aspects of C7 images were saved
separately in the PACS. Prior to measurement, the C7 was placed in
different planes for each parameter. The minimal distance was 0.01
cm and the minimal angle was 1°. The distance between the borders
of the left or right transverse process and the tip of SP in the
superior aspect (DLTS or DRTS), and the distance between the tip of
C7-SP and the medial point of the rear of spinal canal in lateral
aspect, termed the length of SP (LSP), were determined. The angle
of the SP deviation (∠α) was measured as the angle between the long
axis of SP and the median line of the vertebra in the superior
aspect. ∠β was defined as the angle between the long axis of the SP
and the line that crossed the tips of bilateral transverse
processes. ∠γ was measured as the angle between the vertical axis
and the long axis of the SP in the lateral aspect. All of the
abovementioned measurements are indicated in Fig. 1. All subjects of the present study
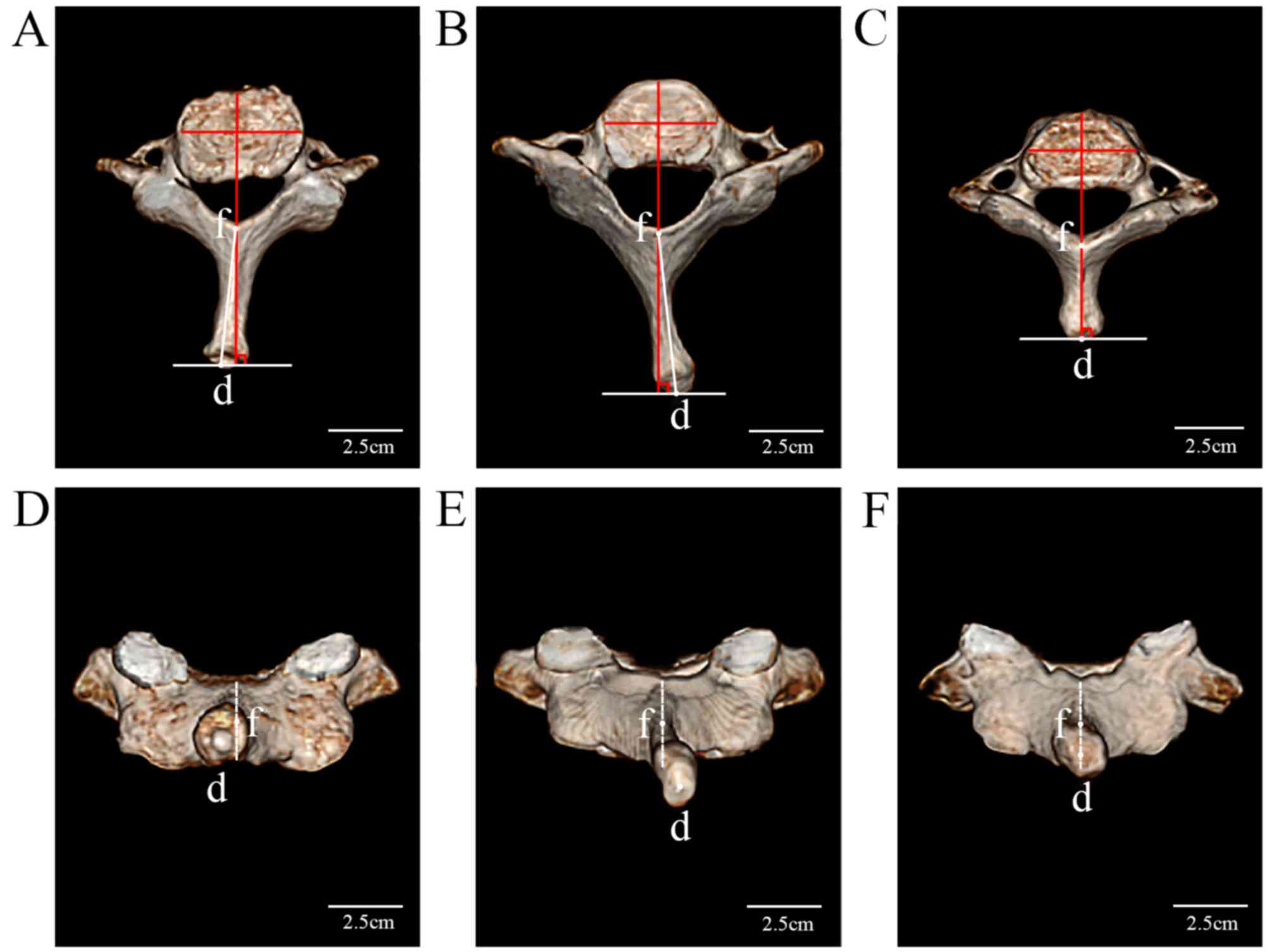
were grouped according to the deviational direction of C7-SP:
Deviating to the right (DR group), deviating to the left (DL group)
and no deviation (ND group) (Fig.
2).
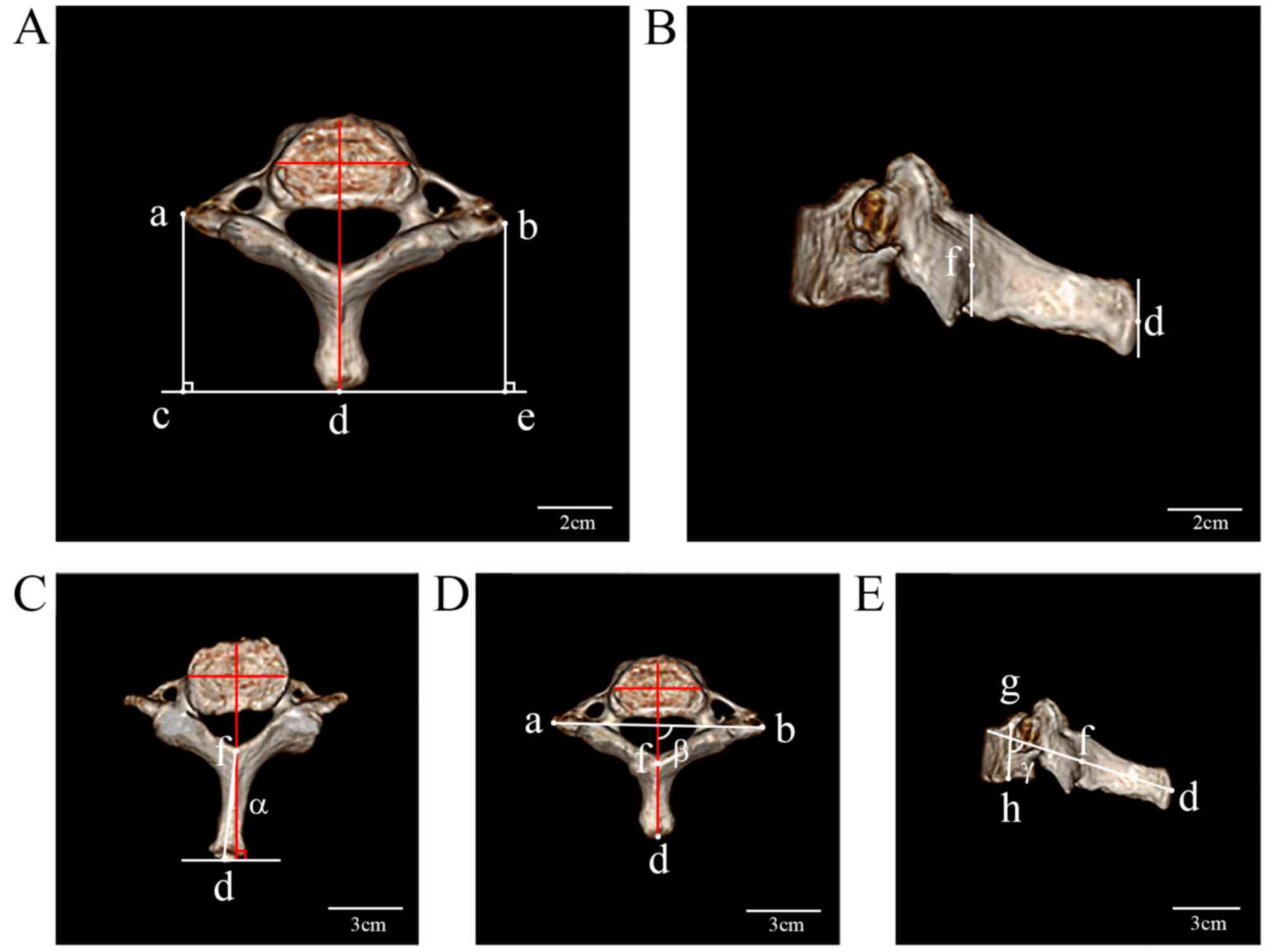 | Figure 1.Measurement of the three parameters
and three angles of the spinous process of the seventh cervical
vertebra in the superior and lateral views. Representative images
in the superior view of the (A and D) ND group and (C) DL group,
and (B and E) in the lateral view of the DR group. DL, C7-SP
deviating to left; DR, C7-SP deviating to right; ND, no deviation
in C7-SP; a, the border of the left transverse process; b, the
border of the right transverse process; d, the tip of the SP; a-c,
the vertical distance between the left transverse process to the
tip of the SP; b-e, the vertical distance between the border of the
right transverse process and the tip of the SP; f, the medial point
of the rear of spinal canal; d-f, the distance between the tip of
the C7-SP and the medial point of the rear of the spinal canal in
the lateral aspect; g-h, the axis of the vertebral body. ∠α, the
angle between the long axis of the SP and the median line of the
vertebra in the superior aspect; ∠β, the angle between the long
axis of the SP and the line which crossed the tips of the bilateral
transverse processes in the superior aspect; ∠γ, the angle between
the vertical body axis and the SP axis in the lateral aspect. |
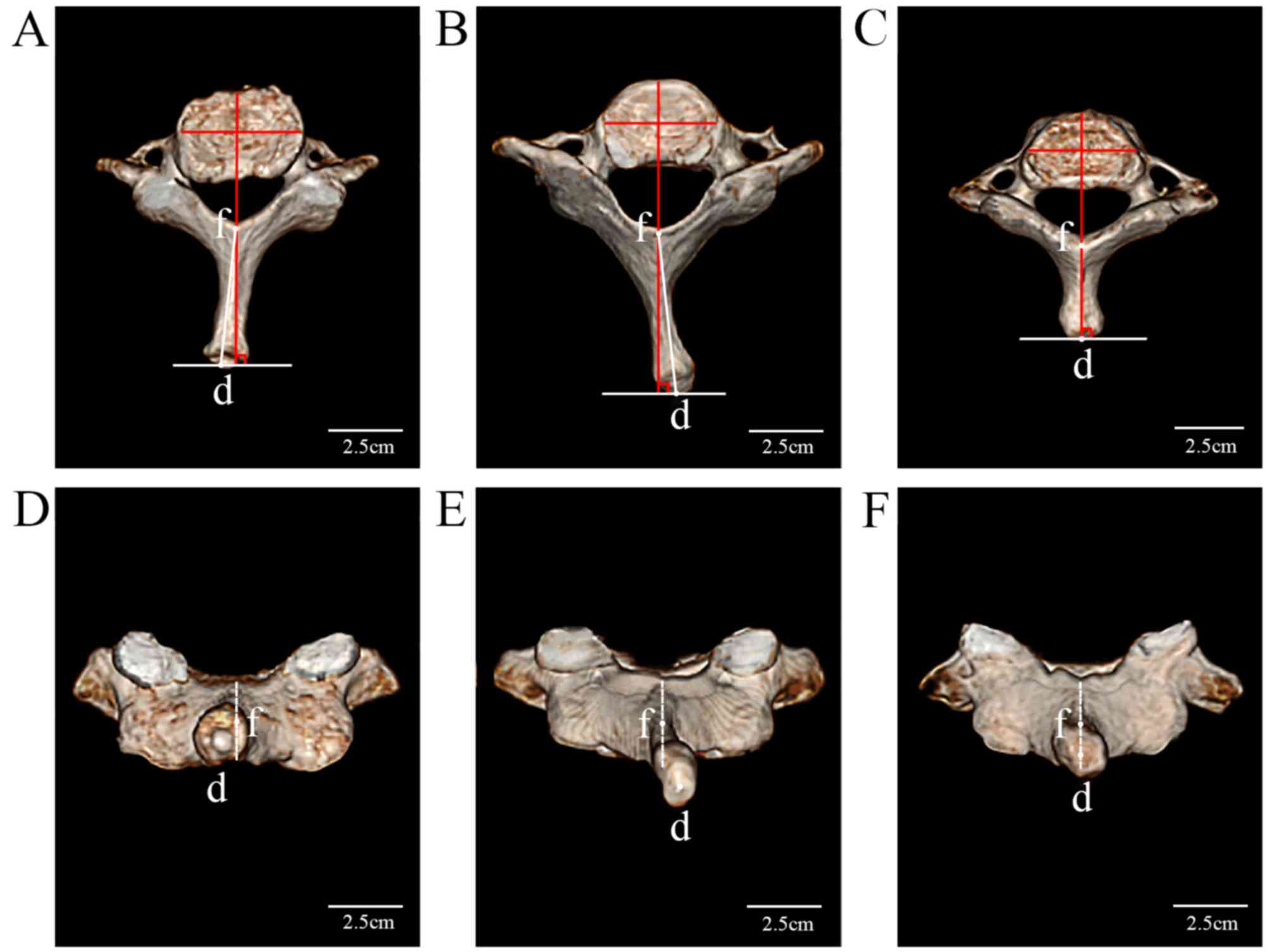 | Figure 2.Different deviations of the C7-SP in
the three groups in superior and posterior view, respectively.
Representative images in the superior view of the (A) DL group, (B)
DR group and (C) ND group, and in the posterior view of the (D) DL
group, (E) DR group and (F) ND group. DL, C7-SP deviating to left;
DR, C7-SP deviating to right; ND, no deviation in C7-SP; d, tip of
the SP; f, medial point of the rear of the spinal canal; d-f,
distance between the tip of the C7-SP and the medial point of the
rear of the spinal canal in the lateral aspect; C7-SP, spinous
process of the seventh cervical vertebra. |
Statistical analysis
A statistical analysis was performed using SPSS,
version 20.0 (IBM Corp., Armonk, NY, USA). The amounts of males and
females in each group were expressed as frequencies and percentages
and were analyzed by the χ2 test. The age and parameters of C7 were
expressed as the mean ± standard deviation. In order to determine
the normal distribution, the Kolmogorov-Smirnov and Shapiro-Wilk
tests were performed. One-way analysis of variance was used to
compare the age and parameters of C7 among the three groups, and
the Student-Newman-Keuls test was the post hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
A total of 245 subjects were enrolled in the present
study, and the number of patients in the DL group was 94, which
comprised 43 males (17.55%) and 51 females (20.82%), and the
average age was 47.23±12.78 years (range, 21–80 years). The DR
group consisted of 133 patients with an average age of 47.95±14.27
years (range, 19–89 years), and included 64 males (26.12%) and 69
females (28.16%). The ND group included 18 subjects, comprising 5
males (2.04%) and 13 females (5.31%) with an average age of
47.95±14.27 years (range, 25–86 years). No statistically
significant difference in the age and the male-to-female ratio
among the three groups was determined (Table I).
 | Table I.Number of males and females, and their
age in the three groups. |
Table I.
Number of males and females, and their
age in the three groups.
| Group | Male | Female | Age (years) |
|---|
| DL | 43 (17.55) | 51 (20.82) | 47.23±12.78 |
| DR | 64 (26.12) | 69 (28.16) | 47.95±14.27 |
| ND | 5 (2.04%) | 13 (5.31) | 47.95±14.27 |
A statistically significant difference in the DLTS
between the DL and ND groups was observed (4.69±0.53 vs. 4.41±0.54
cm; P<0.05). In addition, the DRTS in the DR group was
significantly different from that in the ND group (4.72±0.47 vs.
4.44±0.45 cm; P<0.05). Compared with that in the ND group, the
∠α in the DL and DR groups was significantly different (0 vs.
4.30±2.96 and −5.17±3.35°; P<0.05); furthermore, the ∠α in the
DL group was significantly different from that in the DR group
(P<0.05). More importantly, ∠β was significantly different among
the DL, DR and ND groups (93.09±3.39, 86.30±3.70 and 89.72±2.02°,
respectively; P<0.05). The differences in the LSP and ∠γ among
the three groups were not significant (P>0.05; Table II).
 | Table II.Measurements in the three groups. |
Table II.
Measurements in the three groups.
| Group | DLTS (cm) | DRTS (cm) | LSP (cm) | ∠α (°) | ∠β (°) | ∠γ (°) |
|---|
| DL |
4.69±0.53b | 4.59±0.51 | 3.03±0.37 |
4.30±2.96a,b | 93.09±3.39a,b | 70.95±7.96 |
| DR | 4.57±0.50 |
4.72±0.47b | 3.08±0.36 |
−5.17±3.35b |
86.30±3.70b | 69.33±10.04 |
| ND | 4.41±0.54 | 4.44±0.45 | 2.98±0.28 | 0.00±0.00 | 89.72±2.02 | 70.64±8.13 |
Discussion
The accuracy in identifying C7 using manual
palpation by clinicians is limited due to the inter-individual
variation in the morphology of C7-SP (15–19).
While several studies have assessed the anatomic structures of
C7-SP, most of them focus on the mechanisms of diseases affecting
it (8,20,21). The
SP extends from the posterior of the vertebral arch to provide
connection points for the muscles that extend from the neck,
including the trapezius and spinalis muscles. The end of the nuchal
ligament, which supports the muscles of the neck and connects the
occipital bone of the skull to the C7 vertebra, attaches at the tip
of the spinous process. According to various studies, the
preservation of C7-SP has a crucial role in preventing axial
symptoms (22–25). This is a form of pain around the neck
and shoulders and often remains a major concern for several years
postoperatively, even in patients with excellent neurologic
recovery (26,27). In addition, protection of the C7-SP
and anatomical structures around the cervical spine, including the
muscles attached to the spinous process, as well as the
supraspinous and interspinous ligaments, provides better results
regarding the range of movement and cervical axial pain (28). In addition, it was reported that
adequate knowledge of C7 morphology is necessary for the spinal
surgeon in order to avoid damage to the vertebral arteries, spinal
cord or nerve roots during fixation interventions involving the
posterior cervical spine (29). The
cervicothoracic junction is a challenging anatomical transition in
spine surgery. Compared with all other cervical vertebrae, C7 has
relatively broader laminae, larger pedicles, smaller lateral masses
and a long non-bifid spinous process. These characteristics allow
for a variety of surgical methods to be performed to apply
posterior rigid instrumentation in the form of different types of
screw, including lateral mass, pedicle, transfacet and intralaminar
screws (1).
In the present study, all subjects were grouped
according to the angle of SP deviation. Compared with that in the
ND group, the ∠α of the DL and DR groups was significantly
different. It was indicated that a deviation of the C7-SP existed,
and that it was possible to preliminarily group all C7s according
to their ∠α. Furthermore, as the age and male-to-female ratio did
not significantly differ between the groups, the grouping was not
affected by the age and the male-to-female ratio.
After the grouping, no significant differences were
noted in ∠γ and LSP among the three groups (P>0.05). Numerous
other studies had been performed to measure the LSP. Bazaldua et
al (30), studied the
morphometry of the cervical vertebrae C3-7 in a population from
Northeastern Mexico and measured the distance from the superior
border to the tip of the SP in the sagittal plane to determine a
mean value of 29.12±5.86 mm, which was in accordance with the
results of the present study. However other studies obtained
measures of 22.19±2.02 and 22.78±2.03 mm (31,32),
which was smaller than the result of the present study. These
discrepancies may be the result of the various measuring criteria,
inter-regional or -ethnic differences and statistical errors.
Furthermore, in the present study, the difference in
the DLTS between the DL and ND groups was statistically significant
(4.69±0.53 vs. 4.41±0.54 cm; P<0.05). A statistically
significant difference in the DRTS between the DR and ND groups was
also observed (4.72±0.47 vs. 4.44±0.45 cm; P<0.05). This
indicated that the orientation that SP deviated to had a longer
distance between the transverse process and SP. This may be due to
the rotation of the vertebral body. Stricter measuring methods are
required to be formulated to reduce these errors. More importantly,
statistically significant differences were also observed in ∠β
among the three groups (P<0.05). This parameter reflects the
angle between the transverse process and SP, and it is of vital
importance for surgeries involving the exposure of the
posterolateral part of C7. In addition, it was reported that the
most effective type of posterior fixation at the cervicothoracic
junction was a pedicle screw fixation due to the specific
characteristics of the C7 (7,33–36).
Kajino et al (37), studied
the surgical anatomy for pedicle screw placement in the cervical
spine. They confirmed that the ideal posterior entrance for screw
insertion was 2.5 mm medial to the lateral margin of the lateral
masses, the correct insertion angle was ~45° and the critical value
of depth of insertion was 13–14 mm. Lee et al (38), studied the anatomic feasibility of
posterior cervical pedicle screw placement in children with CT
analysis, arguing that the possibility of subaxial lateral mass
screw fixation must be investigated with a more tailored method. In
this study, before the measurement, all the objectives accepted CT
scan. The value of CT in detecting spinal fractures is well known.
Unlike conventional X-ray analysis, CT scanning provides detailed
images of numerous types of tissue as well as the bones and blood
vessels. Thus, CT has been used in clinical fields including
diagnosis of diseases and anatomical analysis (39–41).
According to the Food and Drug Administration, CT scanning is a
rapid procedure and offers accurate evaluation of bone and most
soft tissues. Using the latest equipment, the spine may be
displayed in multiple planes and 3D images may be reconstructed. In
the present study, the scan images were reconstructed in 3D models.
Compared with conventional 2D images, 3D images may provide more
advancement in the clinic. In addition, these CT images were taken
from helical CTs, which provided adequate data for creating 3D
images.
The present study had certain limitations. First,
the parameters of the C7-SP were measured on the PACS, in which the
tips or medial parts of the structures were determined by three
radiologists. A more advanced measuring tool is required to provide
accurate results. In addition, only the C7-SP of Chinese patients
from the Affiliated Traditional Chinese Medicine Hospital of
Southwest Medical University were assessed, and patients aged
<18 years were excluded; further studies may be performed at
other hospitals for other populations/ethnicities and underage
subjects. Furthermore, no cadaveric study of the C7-SP was
performed in the present study, which may be the aim of a future
study.
In conclusion, based on the 3D CT, several
parameters of the C7-SP were precisely measured. It was identified
that despite of the different age and gender of the patients, it
was possible to preliminarily group all of them according to the
deviation of C7-SP. These results may support future diagnoses and
treatments, and reduce the incidence of misdiagnosis. In addition,
the present study may provide a basis for further studies on C7.
Apart from the deviation of C7-SP, it remains to be determined
whether there is an association with any other parameters.
Therefore, more study is required for assessing the association
between C7-SP, the bony structures and tissues surrounding it.
Acknowledgements
Not applicable.
Funding
This work was supported by Academician Workstation
Construction Project of Luzhou (Luzhou, China; grant no.
20180101).
Availability of data and materials
The analysed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
The study was designed by LZ. Patients were
recruited by ZL, HW, LR, FY, TG and SF. The imaging measurements
were made by ZL, LR and FY. The statistical analysis was conducted
by LZ and HW. LZ, ZL, TG and SF wrote the manuscript.
Ethical approval and consent to
participate
All of the procedures were approved by the Ethical
Committee of the Affiliated Traditional Chinese Medicine Hospital
of Southwest Medical University (Luzhou, China; no.
SWMCTCM2017-0810) and registered as a clinical trial
(ChiCTR-BOC-17012270), and were performed in accordance with the
1964 Helsinki declaration and its later amendments or comparable
ethical standards. Informed consent was obtained from all
individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
C7
|
seventh cervical vertebra
|
|
SP
|
spinous process
|
|
3D CT
|
three dimensional computed
tomography
|
|
DL
|
deviating to left
|
|
DR
|
deviating to right
|
|
ND
|
no deviation
|
|
DLTS
|
distance between the left transverse
process and spinous process
|
|
DRTS
|
distance between the right transverse
process and spinous process
|
|
LSP
|
length of SP
|
|
PACS
|
picture archiving communication
system
|
References
|
1
|
Bayoumi AB, Efe IE, Berk S, Kasper EM,
Toktas ZO and Konya D: Posterior rigid instrumentation of C7:
Surgical considerations and biomechanics at the cervicothoracic
junction. A Review of the literature. World Neurosurg. 111:216–226.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cho W, Maeda T, Park Y, Buchowski JM, Nabb
CE and Riew D: The incidence of bifid C7 spinous processes. Global
Spine J. 2:99–104. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Greiner TM: Shape analysis of the cervical
spinous process. Clin Anat. 30:894–900. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Asvat R: The configuration of cervical
spinous processes in black and white South African skeletal
samples. J Forensic Sci. 57:176–181. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hong JT, Yi JS, Kim JT, Ji C, Ryu KS and
Park CK: Clinical and radiologic outcome of laminar screw at C2 and
C7 for posterior instrumentation-review of 25 cases and comparison
of C2 and C7 intralaminar screw fixation. World Neurosurg.
73:112–118. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tse MS, Chan CH, Wong KK and Wong WC:
Quantitative anatomy of C7 vetebra in southern chinese for
insertion of lateral mass screwsand pedicle screw. Asian Spine J.
10:705–710. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kothe R, Ruther W, Schneider E and Linkeet
B: Biomechanical analysis of transpedicular screw fixation in the
subaxial cervical spine. Spine (Phila Pa 1976). 29:1869–1875. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ono A, Tonosaki Y, Yokoyama T, Aburakawa
S, Takeuchi K, Numasawa T, Wada K, Kachi T and Toh S: Surgical
anatomy of the nuchal muscles in the posterior cervicothoracic
junction: Significance of the preservation of the C7 spinous
process in cervical laminoplasty. Spine (Phila Pa 1976).
33:E349–E354. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liao W, Guo L, Bao H and Wanget L:
Morphometric analysis of the seventh cervical vertebra for pedicle
screw insertion. Indian J Orthop. 49:272–277. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Barrey C, Cotton F, Jund J, Mertens P and
Perrin G: Transpedicular screwing of the seventh cervical vertebra:
Anatomical considerations and surgical technique. Surg Radiol Anat.
25:354–360. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tomasino A, Parikh K, Koller H, Zink W,
Tsiouris AJ, Steinberger J and Härtl R: The vertebral artery and
the cervical pedicle: Morphometric analysis of a critical
neighborhood. J Neurosurg Spine. 13:52–60. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bruneau M, Cornelius JF, Marneffe V,
Triffaux M and George B: Anatomical variations of the V2 segment of
the vertebral artery. Neurosurgery. 59:ONS20–ONS24. 2006.PubMed/NCBI
|
|
13
|
Jovanoviic MS: A comparative study of the
foramen transversarium of the sixth and seventh cervical vertebrae.
Surg Radiol Anart. 12:167–172. 1990. View Article : Google Scholar
|
|
14
|
Schell A, Rhee JM, Holbrook J, Lenehan E
and Park KY: Assessing foraminal stenosis in the cervical spine: A
comparison of three-dimensional computed tomographic surface
reconstruction to two-dimensional modalities. Global Spine J.
7:266–271. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shin S, Yoon DM and Yoon KB:
Identification of the correct cervical level by palpation of
spinous processes. Anesth Analg. 112:1232–1235. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ingram LA, Snodgrass SJ and Rivett DA:
Comparison of cervical spine stiffness in individuals with chronic
nonspecific neck pain and asymptomatic individuals. J Orthop Sports
Phys Ther. 45:162–169. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Robinson R, Robinson HS, Bjorke G and
Kvaleet A: Reliability and validity of a palpation technique for
identifying the spinous processes of C7 and L5. Man Ther.
14:409–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hogan Q: Anatomy of the neuraxis. Cousins
MJ, Carr DB, Horlocker TT and Bridenbaugh TH: Cousins and
Bridenbaugh's Neural Blockade in Clinical Anesthesia and Pain
Medicine. 4th edition. Philadelphia: Lippincott Williams &
Wilkins; pp. 181–212. 2009
|
|
19
|
Cooperstein R and Haneline MT: Spinous
process palpation using the scapular tip as a landmark vs. a
radiographic criterion standard. J Chiropr Med. 6:87–93. 2007.
View Article : Google Scholar
|
|
20
|
Zenmyo M, Komiya S, Hamada T and Inouee A:
A solitary bone cyst in the spinous process of the cervical spine:
A case report. Spine (Phila Pa 1976). 25:641–642. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang P, Shen Y, Zhang YZ, Ding WY, Xu JX
and Cao JM: Preserving the C7 spinous process in laminectomy
combined with lateral mass screw to prevent axial symptom. J Orthop
Sci. 16:492–497. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Takeuchi T and Shono Y: Importance of
preserving the C7 spinous process and attached nuchal ligament in
French-door laminoplasty to reduce postoperative axial symptoms.
Eur Spine J. 16:1417–1422. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Umeda M, Sasai K, Kushida T, Wakabayashi
E, Maruyama T, Ikeura A and Iida H: A less-invasive cervical
laminoplasty for spondylotic myelopathy that preserves the
semispinalis cervicis muscles and nuchal ligament. J Neurosurg
Spine. 18:545–552. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mori E, Ueta T, Maeda T, Yugué I, Kawano O
and Shiba K: Effect of preservation of the C-6 spinous process and
its paraspinal muscular attachment on the prevention of
postoperative axial neck pain in C3-6 laminoplasty. J Neurosurg
Spine. 22:221–229. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kato M, Nakamura H, Konishi S, Dohzono S,
Toyoda H, Fukushima W, Kondo K and Matsuda H: Effect of preserving
paraspinal muscles on postoperative axial pain in the selective
cervical laminoplasty. Spine (Phila Pa 1976). 33:E455–E459. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang P, Shen Y, Zhang YZ, Ding WY, Xu JX
and Cao JM: Preserving the C7 spinous process in laminectomy
combined with lateral mass screw to preventaxial symptom. J Orthop
Sci. 16:492–497. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hosono N, Sakaura H, Mukai Y, Fujii R and
Yoshikawa H: C3-6 laminoplasty takes over C3-7 laminoplasty with
significantly lower incidence of axial neck pain. Eur Spine J.
15:1375–1379. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Secer HI, Harman F, Aytar MH and Kahraman
S: Open-door laminoplasty with preservation of muscle attachments
of C2 and C7 for cervical spondylotic myelopathy, retrospective
study. Turk Neurosurg. 28:257–262. 2018.PubMed/NCBI
|
|
29
|
Karaikovic EE, Kunakornsawat S, Daubs MD,
Madsen TW and Gaines RW Jr: Surgical anatomy of the cervical
pedicles: Landmarks for posterior cervical pedicle entrance
localization. J Spine Disord. 13:63–72. 2000. View Article : Google Scholar
|
|
30
|
Bazaldúa CJJ, González LA, Gómez SA,
Villarreal SE, Velázquez GSE, Sánchez UA, Elizondo-Omaña RE and
Guznán LS: Morphometric study of cervical vertebrae C3-C7 in a
population from Northeastern Mexico. Int J Morphol. 29:325–330.
2011. View Article : Google Scholar
|
|
31
|
Parashar R, Saxena D, Chauhan S, Arora R
and Abhijeet J: A morphometric study of pedicle, lamina and spinous
process of C3-C7 vertebrae in Rajasthan population. Int J Res Med.
3:140–145. 2014.
|
|
32
|
Prabavathy G, Philip XC, Arthi G and
Sadeesh T: Morphometric study of cervical vertebrae C3-C7 in South
Indian population-A clinicoanatomical approach. Italian J Anat
Embryol. 122:49–57. 2017.
|
|
33
|
Rhee JM, Kraiwattanapong C and Hutton WC:
A comparison of pedicle and lateral mass screw construct
stiffnesses at the cervicothoracic junction: A biomechanical study.
Spine (Phila Pa 1976). 30:E636–E640. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ramos-Peek J: Alarm criteria for cervical,
thoracic and lumbar pedicle crews. Clini Neurophysiol.
127:e304–e305. 2016. View Article : Google Scholar
|
|
35
|
Wu C, Chen C, Wu W, Zhao W, Sun P, Fan J,
Bi Z, Zhang J and Ouyang J: Biomechanical analysis of differential
pull-out strengths of bone screws using cervical anterior
transpedicular technique in normal and osteoporotic cervical
cadaveric spines. Spine (Phila Pa 1976). 40:E1–E8. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Fan D, Song R, Zhang M, Bai R, Li Y, Zhang
Z, Wu H, Wang Y, Zhao L, Gao W, et al: Guideline for C1 lateral
mass and C2 pedicle screw choices in children younger than 6 years.
Spine (Phila Pa 1976). 42:E949–E955. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kajino T, Taneichi H, Suda K and Kaneda K:
Surgical Anatomy for Pedicle Screw Placement in the Cervical Spine.
J Japan Spine Res Soc. 15:141–142. 2004.
|
|
38
|
Lee H, Hong JT, Kim IS, Kim MS, Sung JH
and Lee SW: Anatomic feasibility of posterior cervical pedicle
screw placement in children: Computerized tomographic analysis of
children under 10 years old. J Korean Neurosurg Soc. 56:475–481.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Melamed KH, Abtin F, Barjaktarevic I and
Cooper CB: Diagnostic value of quantitative chest CT scan in a case
of spontaneous pneumothorax. Chest. 152:e109–e114. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Feng ST, Zhu H, Peng Z, Huang L, Dong Z,
Xu L, Huang K, Yang X, Lin Z and Li ZP: An individually optimized
protocol of contrast medium injection in enhanced CT scan for liver
imaging. Contrast Media Mol Imaging. 2017:73504292017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Riaz S, Naz F, Bashir H and Niazi IK:
‘Bottle Brush Sign’-spinal meningeal disease on 18F-FDG PET-CT
scan. Clin Nucl Med. 41:726–727. 2016. View Article : Google Scholar : PubMed/NCBI
|