Introduction
With the aged tendency of population and
industrialization in China, the proportion of complications like
osteoporosis is increasing. In addition to the risk factors in
traffic and work, the proportion in thoracolumbar vertebral
fracture is also increasing (1).
Thoracolumbar vertebral fracture patients are usually complicated
with severe and persistent acute pains in waist and back,
dysfunction in nerve system (2), or
even progressive deformity in waist and back with the progression
of disease (3). In clinical
practices, surgical treatment is preferred (4). However, open surgery is more suitable
for patients complicated with spinal cord dysfunction due to the
massive trauma (5), poor tolerance
and slow postoperative recovery of patients, while the
micro-invasive surgery can recover the spinal cord function rapidly
with less pain and correction of deformity (6). Among these methods, percutaneous
kyphoplasty is a more frequent micro-invasive surgical method in
clinical practices so far (7).
Alendronate sodium, as one of the most common
regulators in bone metabolism in clinical practices (8), manifests a strong affinity with the
intraosseous hydroxyapatite, which enables it to inhibit the
activity of osteoclast, thereby inducing the physiological effect
of osteoblast to suppress the bone absorption (9) and facilitating the bone mineralization
and deposition (10). Recurrence
rate of fracture remains high in some patients who undergo the
percutaneous kyphoplasty, especially those complicated with
osteoporosis, despite of its various advantages, which should be
focused on in clinical research and treatment (11). In this study, the analysis was
carried out mainly for the efficacy of percutaneous kyphoplasty in
combination with alendronate sodium on thoracolumbar vertebral
fracture, as well as the risk factors leading to the recurrence of
fracture after surgery.
Patients and methods
General data
A total of 80 patients with thoracolumbar vertebral
fracture who were admitted to were admitted to General Hospital of
The Yangtze River Shipping and Wuhan Brain Hospital and The
Affiliated Jiangyin Hospital of Southeast University Medical
College (Wuxi, China) between January 2014 and March 2016 for
combination treatment of percutaneous kyphoplasty and alendronate
sodium were enrolled. Before operation, all patients aged below 60
years old were required to undergo computed tomography (CT) and
magnetic resonance imaging (MRI) (Fig.
1A and B) for diagnosis to rule out those complicated with
tuberculosis of thoracolumbar spine, tumors in thoracolumbar and
vertebra, coagulation disorders, dysfunctions in lumbar vertebra,
heart, lung, liver or kidney, diseases in spine or nervous system,
mental diseases, diseases in consuming system, lateral displacement
or rotation in fracture site, complete spinal cord injury after
fracture or cauda equina syndrome. In addition, all patients had
signed the written informed consent, and the protocols of this
study had been approved by the Ethic's Committee of General
Hospital of The Yangtze River Shipping and Wuhan Brain Hospital and
The Affiliated Jiangyin Hospital of Southeast University Medical
College.
According to the recurrence of fracture, all
patients were divided into two groups, observation group (patients
with fracture recurrence, n=40) and control group (patients with no
fracture recurrence, n=40). In the observation group, there were 30
males and 10 females aged between 18 and 60 years old with an
average age of 43.2±2.1 years old; as for the fracture causes,
there were 25 cases caused by traffic accident, 13 by high-altitude
falling accident and 2 by bruise; in terms of the Frankel
classification of damage to spinal cord, there were 5 of class B,
15 of class C, 10 of class D and 10 of class E; for the site of
fracture, there were 13 in thoracic vertebra, 19 in lumbar vertebra
and 8 in thoracolumbar vertebra; the time from onset of fracture to
surgery ranged from 8 to 48 h with an average of 18.3±2.1 h. In the
control group, there were 31 males and 9 females aged between 18
and 60 years old with an average age of 44.1±2.0 years old; as for
the fracture causes, there were 26 cases caused by traffic
accident, 12 by high-altitude falling accident and 2 by bruise; in
terms of the Frankel classification of damage to spinal cord, there
were 6 of class B, 16 of class C, 9 of class D and 9 of class E;
for the site of fracture, there were 12 in thoracic vertebra, 15 in
lumbar vertebra and 10 in thoracolumbar vertebra; the time from
onset of fracture to surgery ranged from 8 to 48 h with an average
of 18.4±2.0 h. Comparisons of the gender, age, causes of fracture,
degree of damage to spinal cord, site of fracture and the time from
onset of fracture to surgery showed that the differences had no
statistical significance (P>0.05).
Treatment methods
Under local anesthesia, all patients underwent
percutaneous kyphoplasty, and during the surgery, patients were
required to keep in prone with the hip and anterior superior spine
being lifted to keep the abdomen suspended for identify the
fracture site of vertebra under X-ray. From the pedicle of
vertebral arch in the affected vertebra under local anesthesia,
locating pin was guided into the 1/3 site of vertebra, and, after
the pathway was expanded manually by a drill, reached to the site 1
cm to the anterior edge of vertebra; again, X-ray examination was
then performed to guarantee that the tip of pin was in the midline
of vertebra. Thereafter, a saccule was inserted with the pressure
being adjusted to 160 to 180 psi, and the vertebra was then slowly
opened for injection of about 1 ml of bone cement under X-ray,
after which the distribution of bone cement should be closely
monitored. At 60 sec later, approximately 1 ml of bone cement was
again injected, and the distribution range of bone cement should
also be closely monitored to avoid the exosmosis of bone cement to
the posterior edge veins of vertebra. In this surgery, the amount
of bone cement injection was recorded until the bone cement was
coagulated, and surgery was completed after patients kept the prone
position for 20 min. After surgery, 10 mg alendronate sodium (SFDA
approval no. H10980108; CSPC Huasheng Pharmaceutical Co., Ltd.,
Shijiazhuang, China) was administrated orally in the morning before
meal once per day. Additionally, post-operation X-ray of all
patients were done to observe the effections of the operation
(Fig. 1C and D). All patients
underwent 1-year follow-up. Recurrence of fracture and the site
were identified through the clinical symptoms and the results of
MRI of spine cord.
Observation indexes and evaluation
methods
The alleviation time of numbness in lower limbs and
pains in waist and legs in two groups were compared. Statistics on
the adverse reaction during intervention in two groups were
collected. visual analogue scale (VAS) and Oswestry Disability
Index (ODI) scores of pains at different time points in two groups
were compared, and comparisons of age, section of fracture and
surgery, preoperative bone density, preoperative kyphotic angle,
preoperative height of anterior edge of affected vertebra and
amount of bone cement in operation were also performed. One-way and
multivariate analyses were performed for data above to identify the
relevant risk factors. As for the pain evaluation, VAS scale was
adopted, (10 points for intolerable pains, and 0 point for no
pain), and a higher score meant that the pain was more acute. For
ODI, the score was set from 0 to 45 points, and a higher score
meant that the dysfunction was more evident.
Statistical analysis
SPSS 21.0 software (IBM Corp., Armonk, NY, USA) was
adopted in this study. Measurement data were presented as mean ±
standard deviation, and t-test was carried out for mean
comparison between two groups. Chi-square test was performed for
rate comparison between two groups. As for the factors of patients,
like age, sections of fracture and surgery, preoperative bone
density, preoperative kyphotic angle, preoperative height of
anterior edge of affected vertebra and amount of bone cement in
operation, one-way ANOVA test followed by post hoc test (Least
Significant Difference) was firstly performed, and for those with
statistical significance, non-conditional multivariate Logistic
regression analysis was adopted. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of the alleviation time of
numbness in lower limbs and pains in waist and legs between two
groups after surgery
The alleviation time in numbness of lower limbs in
patients of the control group was earlier than that in the
observation group (P<0.05), and the differences are
statistically significant. The alleviation time in the waist and
legs of patients in the control group was also earlier than that in
the observation group, and the differences are statistically
significant (P<0.05; Table I). It
suggested that among patients in the observation group after the
first time of surgery, the alleviation time of numbness in lower
limbs and pains in waist and legs after the first time of surgery
is more significantly retarded than those in the control group.
 | Table I.Comparison of the alleviation time of
numbness in lower limbs and pains in waist and legs between two
groups after surgery (d, mean ± standard deviation). |
Table I.
Comparison of the alleviation time of
numbness in lower limbs and pains in waist and legs between two
groups after surgery (d, mean ± standard deviation).
| Variable | Alleviation time in
numbness of lower limbs | Alleviation time in
pains in waist and legs |
|---|
| Control group | 1.3±0.1 | 1.6±0.3 |
| Observation
group | 3.6±0.3 | 2.7±0.5 |
| t | 46.000 | 11.931 |
| P-value | <0.001 | <0.001 |
Comparisons of the adverse reactions
during intervention between two groups
The incidence rates of abdominal pain, diarrhea,
constipation and hypocalcemia in the control group were also lower
than those in the observation group, and the differences are
statistically significant (P<0.05; Table II). It suggested that complications
like abdominal pains, diarrhea, constipation and hypocalcemia occur
seldom in patients without fracture recurrence.
 | Table II.Comparisons of the adverse reactions
during intervention between two groups (n, %). |
Table II.
Comparisons of the adverse reactions
during intervention between two groups (n, %).
| Variable | Abdominal pains and
diarrhea | Constipation | Hypocalcemia | Total incidence
rate |
|---|
| Control group | 1 | 0 | 1 | 2 (5.0%) |
| Observation
group | 3 | 4 | 3 | 10 (25.0%) |
| χ2 | – |
| 4.804 |
|
| P-value | – |
| 0.028 |
|
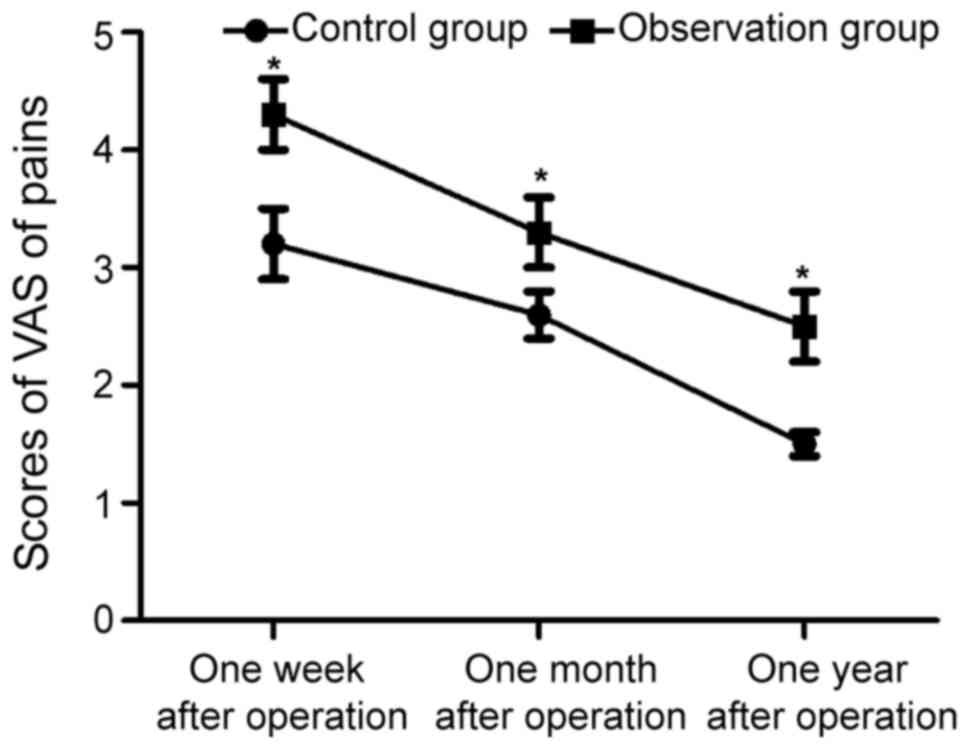
Comparison of the changes in VAS
scores of pains at different time points between two groups
One week, one month and even one year after
operation, the scores of VAS of pains in the control group were
3.2±0.3 points, 2.6±0.2 points and 1.5±0.1 points, significantly
lower than those of the recurrence patients (4.3±0.3 points,
3.3±0.3 points and 2.5±0.3 points) in the observation group in the
same period (t=16.398, 12.279 and 20.000; P<0.05;
Fig. 2). It revealed that patients
with fracture recurrence after percutaneous kyphoplasty have a much
higher pain score.
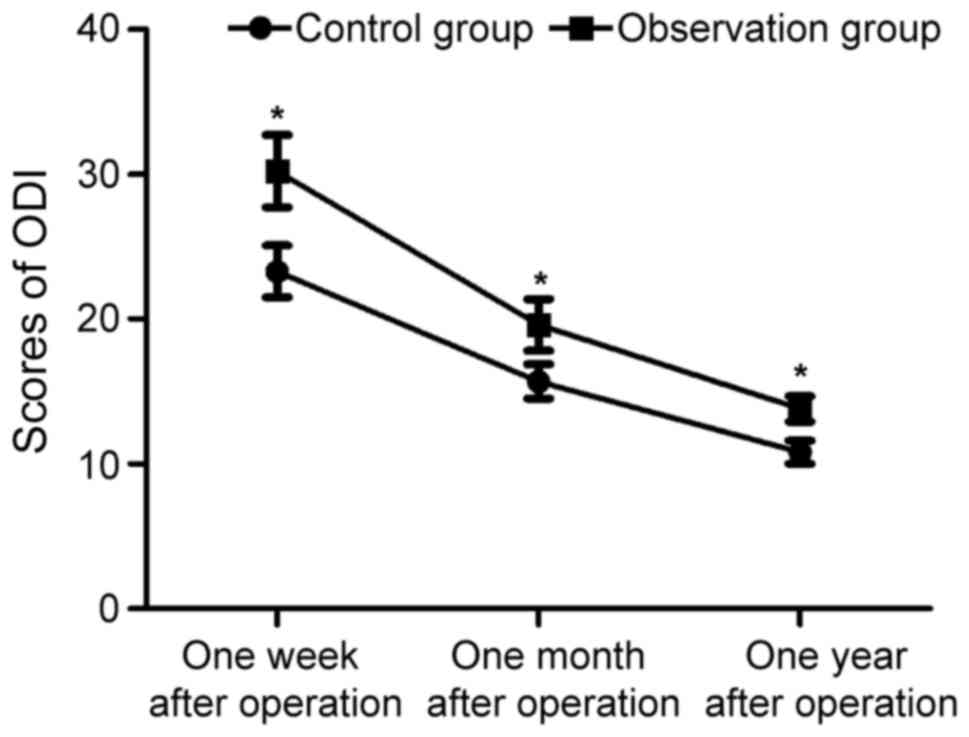
Comparison of the changes in ODI
scores of pains at different time points between two groups
One week, one month and even one year after
operation, the scores of ODI in the control group were 23.3±1.8
points, 15.7±1.2 points and 10.8±0.8 points, significantly lower
than those (30.2±2.5 points, 19.6±1.8 points and 13.7±0.9 points)
in the observation group in the same period (t=14.166, 11.402 and
15.232; P<0.05; Fig. 3). It
revealed that patients with fracture recurrence after percutaneous
kyphoplasty have a relatively lower score of ODI.
Comparisons of the results of one-way
analysis of measurement data between two groups
Through one-way analysis, it was found that the
amount of fracture and surgery sections, preoperative bone density,
preoperative kyphotic angle, preoperative height of anterior edge
of affected vertebra, amount of bone cement in operation, onset
time and exosmosis of bone cement were the relevant risk factors
for the recurrence of fracture after the percutaneous kyphoplasty
in combination with alendronate sodium for patients with
thoracolumbar vertebral fracture (Tables III and IV).
 | Table III.Comparisons of the results of one-way
analysis of measurement data between two groups (mean ± standard
deviation). |
Table III.
Comparisons of the results of one-way
analysis of measurement data between two groups (mean ± standard
deviation).
| Variable | Observation
group | Control group | t | P-value |
|---|
| Age (years old) |
65.7±2.1 |
66.0±2.1 | 0.639 | 0.525 |
| Section of fracture
(n) |
2.15±0.03 |
1.36±0.02 | 138.575 | <0.001 |
| Section of surgery
(n) |
2.03±0.03 |
1.12±0.02 | 159.625 | <0.001 |
| Preoperative bone
density (standard deviation) |
−3.24±0.12 |
−2.79±0.09 | 18.974 | <0.001 |
| Preoperative kyphotic
angle (°) |
23.56±0.21 |
19.50±0.18 | 92.838 | <0.001 |
| Preoperative height
of anterior edge of affected vertebra (mm) |
0.59±0.03 |
0.65±0.04 | 7.589 | <0.001 |
| Amount of bone cement
in operation (ml) |
3.21±0.08 |
3.56±0.09 | 18.383 | <0.001 |
 | Table IV.Comparisons of the results of one-way
analysis of enumeration data between two groups (n). |
Table IV.
Comparisons of the results of one-way
analysis of enumeration data between two groups (n).
| Variable | Observation
group | Control group | χ2 | P-value |
|---|
| Sex |
|
|
| 0.805 |
| Male | 11 | 12 | 0.061 |
|
|
Female | 29 | 28 |
|
|
| Time of fracture |
|
|
| 0.008 |
| Within 1
month | 28 | 38 | 7.013 |
|
| Over 1
month | 12 | 2 |
|
|
| Hormone
administration |
|
|
| 0.302 |
| Yes | 12 | 8 | 1.067 |
|
| No | 28 | 32 |
|
|
| Exosmosis of bone
cement |
|
|
| <0.001 |
| Yes | 20 | 2 | 18.119 |
|
| No | 20 | 38 |
|
|
Multivariate logistic regression
analysis of the recurrence of fracture
With the recurrence of fracture as the dependent
variable, the multivariate logistic regression analysis was
performed and the results revealed that a lower preoperative bone
density and the exosmosis of bone cement during surgery were the
independent risk factors in the recurrence of fracture (Table V).
 | Table V.Multivariate logistic regression
analysis of fracture recurrence. |
Table V.
Multivariate logistic regression
analysis of fracture recurrence.
| Variable | β | Standard error | Weight | P-value | Odds ratio | 95% confident
interval |
|---|
| Fracture section
(n) | 0.786 | 0.613 | 1.645 | 0.201 | 2.193 | 0.661–7.729 |
| Surgery section
(n) | 0.045 | 0.060 | 0.579 | 0.448 | 1.047 | 0.933–1.173 |
| Preoperative bone
density (SD) | −1.835 | 0.777 | 5.595 | 0.018 | 0.159 | 0.035–0.731 |
| Preoperative
kyphotic angle (°) | 0.035 | 0.044 | 0.601 | 0.439 | 1.035 | 0.951–1.127 |
| Preoperative height
of anterior edge of affected vertebra (mm) | 0.223 | 0.343 | 0.425 | 0.516 | 1.251 | 0.640–2.446 |
| Intraoperative
amount of bone cement (ml) | 0.938 | 3.207 | 0.086 | 0.771 | 2.553 | 0.005–1368.589 |
| Onset of
fracture | 0.073 | 0.053 | 0.031 | 0.856 | 2.693 | 0.491–2.361 |
| Bone cement
exosmosis | 1.873 | 0.834 | 5.050 | 0.025 | 6.503 | 1.272–33.273 |
Discussion
After treatment of percutaneous kyphoplasty in
combination with alendronate sodium for thoracolumbar vertebral
fracture, some patients may suffer from the recurrence of fracture
(12), which usually leads to the
severe pains in waist and back, progressive collapse of spinal
cord, kyphosis osteotomy of vertebral laminae or even dysfunction
in spinal cord, thereby affecting the normal motor function
(13). Recurrence not only decreases
the life quality of patients, but also brings heavy burden for the
society and the family of patients (14). A previous study (15) believed that osteoporosis is the most
common cause for recurrence of fracture in percutaneous
kyphoplasty. But, there remain few studies currently focusing on
the causes responsible for the recurrence of fracture after
administration of alendronate sodium for symptomatic treatment. We
suspected that there were important relationships between the
recurrence of fracture and quantity of fracture, surgery sections,
preoperative bone density, preoperative kyphotic angle,
preoperative height of anterior edge of affected vertebra,
intraoperative usage amount of bone cement, onset time of fracture
and exosmosis of bone cement after administration of alendronate
sodium.
In this study, patients with thoracolumbar vertebral
fracture who received the percutaneous kyphoplasty in combination
with alendronate sodium were enrolled to figure out the recurrence
of fracture. It was found that in comparison of the alleviation
time of numbness in lower limbs and pains in waist and legs between
two groups after treatment, the alleviation time of numbness in
lower limbs in the control group was significantly earlier than
that in the observation group, and the alleviation time of pains in
waist and legs in the control group was also earlier than that in
the observation group, suggesting that among patients in the
observation group after the first time of surgery, the alleviation
time of numbness in lower limbs and pains in waist and legs after
the first time of surgery is more significantly retarded than those
in the control group. Meanwhile, comparison of incidence rate of
adverse reaction during intervention between two groups also showed
that the total incidence rates of abdominal pains, diarrhea,
constipation and hypocalcemia in the patients of the control group
were significantly lower than those in the observation group,
suggesting that complications like abdominal pains, diarrhea,
constipation and hypocalcemia occur seldom in patients without
fracture recurrence, which may be correlated with the absorption
after treatment of alendronate sodium. In addition, the analyses in
changes of VAS scores of pains and ODI scores at different time
points in two groups showed that one week, one month and even one
year after operation, the scores of VAS of pains and ODI in the
control group were significantly lower than those in the
observation group in the same period, revealing that patients with
fracture recurrence after percutaneous kyphoplasty have a much
higher pain score and a relatively lower score of ODI. Finally,
one-way analysis and multivariate analysis for relevant risk
factors leading to the fracture recurrence after percutaneous
kyphoplasty in combination with alendronate sodium showed that a
large quantity of fracture and surgery sections, preoperative bone
density, preoperative kyphotic angle, preoperative height of
anterior edge of affected vertebra, intraoperative usage amount of
bone cement, onset time of fracture and exosmosis of bone cement
are the relevant risk factors leading to the fracture recurrence
after percutaneous kyphoplasty in combination with alendronate
sodium, and the low preoperative bone density and exosmosis of bone
cement in surgery are also the independent risk factors of fracture
recurrence.
Among the patients with fracture recurrence after
percutaneous kyphoplasty in combination with alendronate sodium for
thoracolumbar vertebral fracture, elder patients with a relatively
low bone density are the dominant population (16). The reason may be that bone mineral
density decreased significantly with the growth of the age,
especially in older postmenopausal women. In the present study,
bone density is an independent risk factor affecting the fracture
recurrence after surgery, suggesting that bone density is a major
factor affecting the surgical efficacy, especially the recurrence
of fracture (17,18). In addition, exosmosis of bone cement
is the most common complication in percutaneous kyphoplasty
(19), and also the independent risk
factor leading to the postoperative recurrence of fracture
(20). In this study, it was found
that for patients who undergo percutaneous kyphoplasty with or
without administration of alendronate sodium for thoracolumbar
vertebral fracture, the incidence rate of postoperative recurrence
of fracture was significantly increased in patients complicated
with the exosmosis of bone cement in surgery.
There are still some limitations in this study.
Classifying the recurrence rate of fracture and the exosmosis of
bone cement as ‘Yes/No’, we did not consider the type, severity and
site of exosmosis, which could warrant the conclusions. Thus,
further studies will be needed to clarify the relations of
refracture types and severity and site of exosmosis. Additionally,
the efficacy of alendronate sodium with PTH in treatment of
Thoracolumbar Vertebral Fracture will also be explored in
future.
In conclusion, our study indicated that percutaneous
kyphoplasty combined with alendronate sodium was a superior
treatment option of thoracolumbar vertebral fracture when compared
with percutaneous kyphoplasty alone. Additionally, there underlies
an important correlation between the recurrence rate of fracture
and the preoperative bone density as well as the exosmosis of bone
cement in operation for patients with thoracolumbar vertebral
fracture who receive percutaneous kyphoplasty in combination with
alendronate sodium.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
PL and WT designed the study, BC, KW, KZ and ZJ
collected the data, FZ and YZ analyzed the data, PL and YZ prepared
the manuscript, WT and KZ made the revisions, YZ and PL performed
the operations. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethic Committee of
General Hospital of The Yangtze River Shipping and Wuhan Brain
Hospital and The Affiliated Jiangyin Hospital of Southeast
University Medical College (Wuhan, China). Signed written informed
consents were obtained from the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Semaan H, Obri T, Bazerbashi M, Paull D,
Liu X, Sarrouj M and Elgafy H: Clinical outcome and subsequent
sequelae of cement extravasation after percutaneous kyphoplasty and
vertebroplasty: A comparative review. Acta Radiol. Jan 1. 2017,
(Epub ahead of print). PubMed/NCBI
|
|
2
|
Niu J, Song D, Zhou H, Meng Q, Meng B and
Yang H: Percutaneous kyphoplasty for the treatment of osteoporotic
vertebral fractures with intravertebral fluid or air: A comparative
study. Clin Spine Surg. 30:367–373. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Filippiadis DK, Marcia S, Masala S,
Deschamps F and Kelekis A: Percutaneous vertebroplasty and
kyphoplasty: Current status, new developments and old
controversies. Cardiovasc Intervent Radiol. 40:1815–1823. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rajasekaran S, Kanna RM, Schnake KJ,
Vaccaro AR, Schroeder GD, Sadiqi S and Oner C: Osteoporotic
thoracolumbar Fractures-How are they different?-Classification and
treatment algorithm. J Orthop Trauma. 31(Suppl 4): S49–S56. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu T, Li Z, Su Q and Hai Y: Cement
leakage in osteoporotic vertebral compression fractures with
cortical defect using high-viscosity bone cement during unilateral
percutaneous kyphoplasty surgery. Medicine (Baltimore).
96:e72162017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Masoudi MS, Haghnegahdar A, Ghaffarpasand
F and Ilami G: Functional recovery following early kyphoplasty
versus conservative management in stable thoracuolumbar fractures
in parachute jumpers: A randomized clinical trial. Clin Spine Surg.
30:E1066–E1073. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang P, Lin J, Liu H, Shen H and Yang HL:
Primary bone mantle cell lymphomas with multiple vertebral
compression fractures: A case report. Oncol Lett. 13:1288–1292.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sun ZY, Li XF, Zhao H, Lin J, Qian ZL,
Zhang ZM and Yang HL: Percutaneous balloon kyphoplasty in treatment
of painful osteoporotic occult vertebral fracture: A retrospective
study of 89 cases. Med Sci Monit. 23:1682–1690. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rosenbaum BP, Kshettry VR, Kelly ML, Mroz
TE and Weil RJ: Trends in inpatient vertebroplasty and kyphoplasty
volume in the united states, 2005–2011: Assessing the impact of
randomized controlled trials. Clin Spine Surg. 30:E276–E282. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lin D, Hao J, Li L, Wang L, Zhang H, Zou W
and Lian K: Effect of bone cement volume fraction on adjacent
vertebral fractures after unilateral percutaneous kyphoplasty. Clin
Spine Surg. 30:E270–E275. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pesenti S, Graillon T, Mansouri N,
Adetchessi T, Tropiano P, Blondel B and Fuentes S: Use of pedicle
percutaneous cemented screws in the management of patients with
poor bone stock. Neurochirurgie. 62:306–311. 2016.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wu YS, Zhang H, Zheng WH, Feng ZH, Chen ZX
and Lin Y: Hidden blood loss and the influential factors after
percutaneous kyphoplasty surgery. Eur Spine J. 26:1878–1883. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gonschorek O, Hauck S, Weiss T and Buhren
V: Percutaneous vertebral augmentation in fragility
fractures-indications and limitations. Eur J Trauma Emerg Surg.
43:9–17. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Beall DP, Parsons B and Burner S:
Technical strategies and anatomic considerations for an
extrapedicular modified inferior endplate access to thoracic and
lumbar vertebral bodies. Pain Physician. 19:593–601.
2016.PubMed/NCBI
|
|
15
|
Dmytriw AA, Talla K and Smith R:
Percutaneous sacroplasty for the management of painful pathologic
fracture in a multiple myeloma patient: Case report and review of
the literature. Neuroradiol J. 30:80–83. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cheng X, Long HQ, Xu JH, Huang YL and Li
FB: Comparison of unilateral versus bilateral percutaneous
kyphoplasty for the treatment of patients with osteoporosis
vertebral compression fracture (OVCF): A systematic review and
meta-analysis. Eur Spine J. 25:3439–3449. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Riva A, Togni S, Giacomelli L, Franceschi
F, Eggenhoffner R, Feragalli B, Belcaro G, Cacchio M, Shu H and
Dugall M: Effects of a curcumin-based supplementation in
asymptomatic subjects with low bone density: A preliminary 24-week
supplement study. Eur Rev Med Pharmacol Sci. 21:1684–1689.
2017.PubMed/NCBI
|
|
18
|
Yang H, Liu H, Wang S, Wu K, Meng B and
Liu T: Review of percutaneous kyphoplasty in china. Spine (Phila Pa
1976). 41(Suppl 19): B52–B58. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yaltirik K, Ashour AM, Reis CR, Ozdogan S
and Atalay B: Vertebral augmentation by kyphoplasty and
vertebroplasty: 8 years experience outcomes and complications. J
Craniovertebr Junction Spine. 7:153–160. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Korovessis P, Mpountogianni E and
Syrimpeis V: Percutaneous pedicle screw fixation plus kyphoplasty
for thoracolumbar fractures A2, A3 and B2. Eur Spine J.
26:1492–1498. 2017. View Article : Google Scholar : PubMed/NCBI
|