Introduction
Coronary artery disease (CAD) is one of the most
common complicated cardiovascular diseases and may be caused by
atherosclerosis, vascular cavity stenosis and/or occlusion
(1–3). It has previously been reported that
acute CAD may contribute to the pathogenesis of occlusive
thrombosis (4–6). Notably, multifactorial microvascular
dysfunction in patients with acute CAD may result in blunted
responses to adenosine and false-negative readings for fractional
flow reserve (7). It is therefore
important to develop more accurate diagnostic methods to confirm
whether patients have CAD. In recent years, a number of diagnostic
methods have been developed for coronary atherosclerotic heart
diseases (8–10). Notably, cardiac computed tomography
(CT) was reported to be more efficient compared with
electrocardiogram and intravascular ultrasound in the diagnosis of
coronary atherosclerotic heart diseases (11).
Currently, three-dimensional CT angiography (3D-CTA)
is widely used to diagnose human tumors, heart diseases and other
pathologic changes (12–15). It has been reported that 3D-CTA is an
effective technique for imaging microvascular anatomy (16). 3D-CTA is able to identify vascular
injuries to increase the diagnostic accuracy and improve treatment
(17). Furthermore, 3D-CTA is
essential for preoperative planning to decide on the best surgical
approach to treat arteriovenous malformations (18). 3D-CTA diagnosis has been used as an
initial screening tool in lieu of digital subtraction angiography
to rule out vascular diseases in idiopathic spontaneous
subarachnoid hemorrhage (19).
Furthermore, a randomized controlled trial demonstrated that 3D-CTA
is advantageous compared with conventional coronary angiography
(CCA) when performing laparoscopic colorectal resection for
patient's mesenteric vascular anatomy (20). However, the efficacy of 3D-CTA as a
diagnostic tool for CAD remains to be elucidated.
The aim of the present study was to investigate the
diagnostic efficacy of 3D-CTA and coronary CTA (CCTA), as well as
the accuracy of CCTA in measuring calcifying plaques and the ratio
of calcified plaque volume to vessel circumference (RVTC) in 136
patients with suspicious with acute CAD. The results demonstrated
that 3D-CTA has a superior diagnostic performance compared with CCA
in patients with acute CAD.
Materials and methods
Study population
A total of 136 patients with suspected acute CAD
were recruited from the Affiliated Hospital of Changchun University
of Chinese Medicine (Changchun, China) between February 2014 and
May 2015 and all patients underwent CCA and 3D-CTA (Discovery CT750
HD; GE Healthcare Life Sciences, Little Chalfont, UK) between May
2013 and October 2016. The exclusion criteria included renal
insufficiency (serum creatinine level, >1.5 mg/dl), diabetes
mellitus and a history of allergic reaction to contrast medium. The
Ethical Committee of the Affiliated Hospital of Changchun
University of Chinese Medicine approved this prospective study.
Written informed consent was obtained from all the patients.
CCA
All patients were diagnosed using CCA. Calcified
plaques were analyzed using quantitative CAA (AXIOM Artis dB;
Siemens AG, Munich, Germany) (21).
CCA was performed in all evaluable coronary segments to identify
coronary stenosis and plaques by an experienced cardiologist, who
was blinded to the conditions of the present study. The severity of
stenosis was defined when lesions of the coronary artery were ≥50%
in diameter.
3D-CTA analysis
3D-CTA was performed to evaluate the lesions as
previously described (22). All
images were acquired using an MDCT scanner (Philips Healthcare,
Amsterdam, The Netherlands) with 16 detectors and a tiltable
gantry. The parameters negative predictive value (NPV), positive
predictive value (PPV), CCTA and RVTC were recorded and analyzed
using a dedicated cardiac workstation (TeraRecon GmbH, Frankfurt,
Germany). The lesions were analyzed on an OsiriX workstation
(OsiriX Imaging Software 2.0; Pixmeo SARL, Bernex, Switzerland) and
target-to-background ratio (TBR) was defined as the ratio of
maximum activity values in the manually defined lesion to the mean
background value. The plaque was confirmed by obvious presence of
plaque or napkin ring signs and spotty calcium.
Statistical analysis
All statistical analyses were performed using SPSS
19.0 (IBM Corp., Armonk, NY, USA). Comparisons between groups were
made using one-way analysis of variance for continuous variables
followed by Tukey's post hoc test. Categorical variables were
analyzed using Fisher's exact test and the sensitivity,
specificity, NPV and PPV values were analyzed using exact binomial
confidence intervals. For the CCTA assessment, the test was
considered positive if ≥50% stenosis or plaque was identified. RVTC
was analyzed using the receiver operating characteristics curve and
the area under curve (AUC) was compared between groups using the
DeLong algorithm. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
A total of 136 patients with suspected acute CAD
were recruited and diagnosed using 3D-CTA and CCA. Patients'
baseline characteristics are summarized in Table I. No significant differences were
observed in baseline demographics or risk factors for male and
female patients. All patients underwent both 3D-CTA and CCA
diagnosis.
 | Table I.Baseline patient characteristics. |
Table I.
Baseline patient characteristics.
|
| Male | Female |
|---|
| Characteristic | (n=80) | (n=56) |
|---|
| Mean age (years) | 53.4±13.3 | 56.0±9.4 |
| Cardiovascular risk
factors (%) |
|
Hypertension | 13 (16.25) | 5 (8.93) |
|
Dyslipidemia | 10 (12.5) | 6 (10.71) |
| Former or current
smoker, n (%) | 22 (27.5) | 3 (5.36) |
| Family history of
premature coronary artery disease, n (%) | 14 (17.5) | 7 (12.5) |
| Acute coronary
syndrome, n (%) |
|
Myocardial infarction | 10 (12.5) | 5 (8.93) |
| Unstable
angina pectoris | 8 (10.0) | 5 (8.93) |
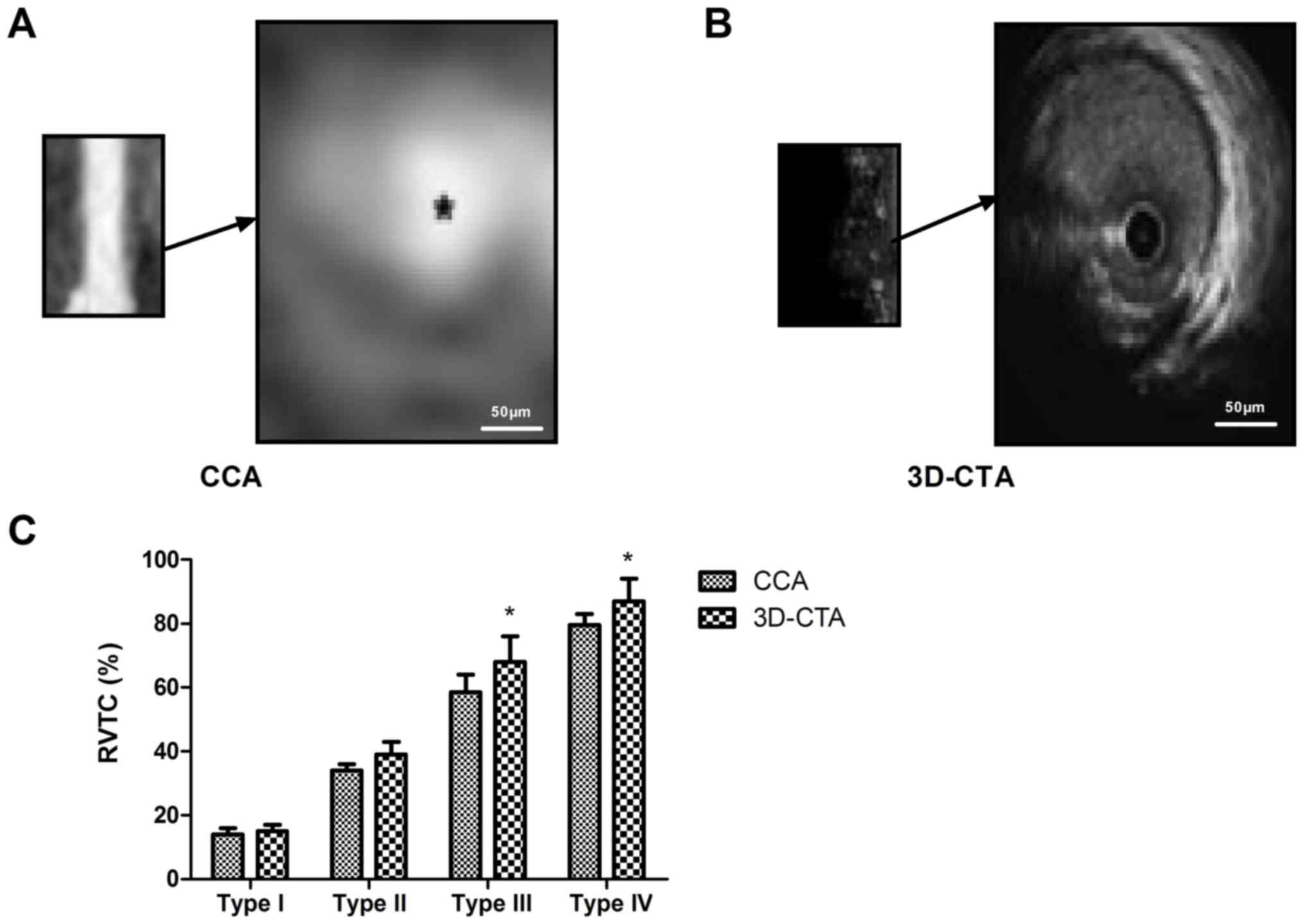
Analysis of the calcified plaque and
RVTC
The calcified plaques and RVTC were investigated in
the present study. The results revealed that 3D-CTA was able to
identify calcified plaques more clearly in patients with acute CAD
compared with CCA (Fig. 1A and B).
The calculated RVTC was higher using 3D-CTA compared with CCA for
types III and IV (P<0.05; Fig.
1C). These results suggest that 3D-CTA is an effective method
for identifying calcified plaques and RVTC in patients with acute
CAD.
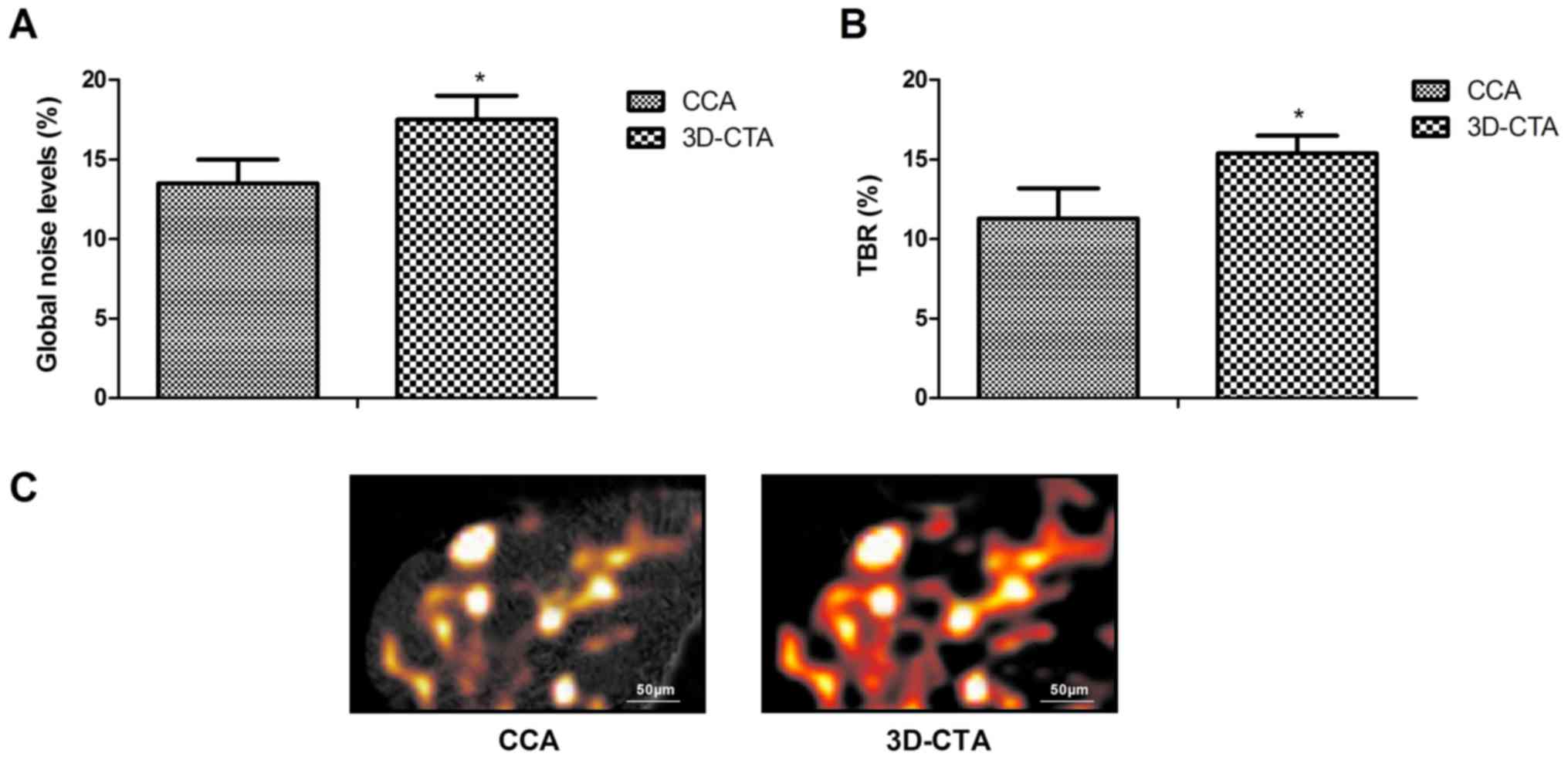
3D-CTA for identifying risk events in
patients with acute CAD
The efficacy of 3D-CTA for identifying risk events
(TBR and ischemia) was evaluated in patients with acute CAD. The
results indicate that 3D-CTA diagnosis significantly improved the
AUC, specificity, PPV and NPV compared with CCA diagnosis
(P<0.05; Table II). Global noise
levels and TBR were significantly decreased using 3D-CTA compared
with CCA (P<0.05; Fig. 2A and B).
It was also demonstrated that ischemia may be more easily
discriminated using 3D-CTA compared with CCA (Fig. 2C). These outcomes indicate that
3D-CTA could efficiently evaluate the risk events for patients with
acute CAD.
 | Table II.Diagnostic accuracy of 3D-CTA and CCA
for patients with coronary artery disease. |
Table II.
Diagnostic accuracy of 3D-CTA and CCA
for patients with coronary artery disease.
| Variable | CCA | 3D-CTA | P-value |
|---|
| Area under curve | 78.8 | 97.2 | 0.0385 |
| Positive predictive
value (%) | 71.2 | 94.3 | 0.0263 |
| Negative predictive
value (%) | 70.8 | 40.3 | 0.00170 |
| Specificity (%) | 82.3 | 94.8 | 0.0478 |
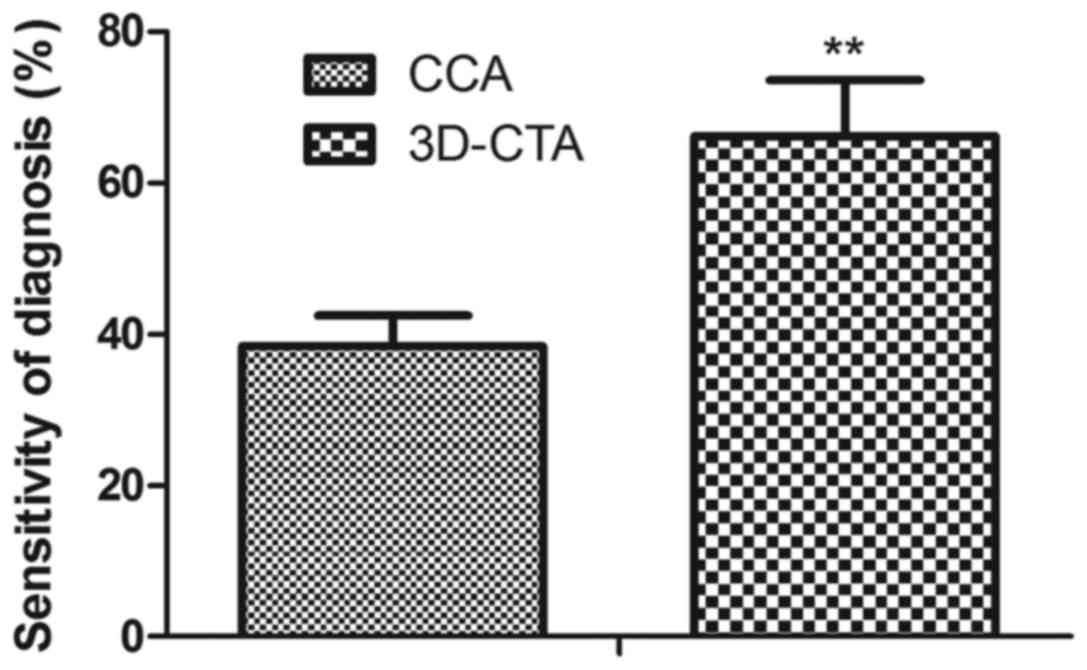
3D-CTA for the diagnosis of patients
with acute CAD
The accuracy of 3D-CTA as a diagnostic tool for
patients with acute CAD was investigated. 3D-CTA was used to
successfully diagnose 86 patients with acute CAD, 34 patients with
myocardial infarction and 16 patients with stable angina. CCA
successfully diagnosed 72 patients with acute CAD, 26 with
myocardial infarction and 8 with stable angina (Table III). As such, 3D-CTA had a
significantly higher sensitivity for the diagnosis of acute CAD
compared with CCA in the present study (P<0.01; Fig. 3). Taken together, these results
suggest that 3D-CTA may be used in place of CCA to improve the
diagnostic accuracy for patients with acute CAD.
 | Table III.Diagnostic outcomes between 3D-CTA and
CCA for patients with acute coronary artery disease. |
Table III.
Diagnostic outcomes between 3D-CTA and
CCA for patients with acute coronary artery disease.
| Disease | CCA | 3D-CTA | P-value |
|---|
| Acute coronary artery
disease | 72 | 86 | 0.0372 |
| Myocardial
infarction | 26 | 34 | 0.0460 |
| Stable angina | 8 | 16 | 0.0174 |
Discussion
Currently, acute CAD has high mortality and is
associated with metabolic disorders of myocardial cells (23). Early diagnosis of acute CAD is
important to improve treatment (24). It has been reported that 3D-CTA is a
useful tool for aiding doctors in recognizing the morphology of
coronary arteries and plaques in patients with CAD (25). In the present study, the diagnostic
efficacy of 3D-CTA for acute CAD was assessed, using CCA diagnosis
as a control. The results revealed that 3D-CTA had a significantly
greater diagnostic accuracy than CCA for patients with acute
CAD.
Visualization techniques utilizing multislice
CT-coronary angiography of the heart are beneficial for identifying
correlations between axial, multiplanar, 3D and virtual endoscopic
imaging (26). In the present study,
3D-CTA data was used to diagnose 86 patients with acute CAD, 34
with myocardial infarction and 16 with stable angina with
significantly greater accuracy than CCA. 3D-CTA also presented a
direct role during the surgery for patients with CAD (20). The results demonstrate that 3D-CTA is
able to accurately identify the calcified plaque and RVTC for
patients with acute CAD, which may be an efficient method for the
diagnosis of acute CAD patients.
Acute coronary syndrome is a kind of cardiovascular
disease caused by the rupture of coronary atherosclerosis plaques
(27). It has previously been
reported that 3D-CTA produces high quality 3D cardiac images that
can be used to predict the contrast injection rate for patients
with congenital heart disease (28).
It the present study it was revealed that the diagnostic accuracy
and specificity of 3D-CTA is significantly higher for acute CAD
patients compared with CCA. 3D-CTA clearly identified global noise
levels, TBR and ischemia in patients with acute CAD. Notably,
3D-CTA had a greater diagnostic sensitivity for acute CAD compared
with CCA. However, further research should be conducted to
authenticate the diagnostic efficacy of 3D-CTA for patients with
acute CAD. Additionally, receiver operator characteristic curves
should be plotted to compare the sensitivity and specificity of CCA
and 3D-CTA using a larger sample size of patients with suspected
acute CAD.
In summary, 3D-CTA may be used to clinically
diagnosis patients with acute CAD. 3D-CTA may improve the overall
diagnostic accuracy and contribute to treatment for acute patients
with CAD, However, further studies should be performed to confirm
this.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LL performed the experiments. JH and SQ analyzed
data. YF designed the study.
Ethics approval and consent to
participate
The Ethical Committee of the Affiliated Hospital of
Changchun University of Chinese Medicine approved this prospective
study. Written informed consent was obtained from all the
patients.
Consent for publication
Written informed consent was obtained from all the
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dickens C, Cherrington A and McGowan L:
Depression and health-related quality of life in people with
coronary heart disease: A systematic review. Eur J Cardiovasc Nurs.
11:265–275. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zwadlo C, Meyer GP, Schieffer B and
Westhoff-Bleck M: Anomalous intramural course of coronary arteries
in congenital heart disease-three case reports and review of the
literature. Congenit Heart Dis. 7:139–144. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mehra M, Somohano T and Choi M: Mandibular
fibular graft reconstruction with CAD/CAM technology: A clinical
report and literature review. J Prosthet Dent. 115:123–128. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Haasenritter J, Aerts M, Bösner S, Buntinx
F, Burnand B, Herzig L, Knottnerus JA, Minalu G, Nilsson S, Renier
W, et al: Coronary heart disease in primary care: Accuracy of
medical history and physical findings in patients with chest pain-a
study protocol for a systematic review with individual patient
data. BMC Fam Pract. 13:812012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fan J, Song Y, Wang Y, Hui R and Zhang W:
Dietary glycemic index, glycemic load, and risk of coronary heart
disease, stroke, and stroke mortality: A systematic review with
meta-analysis. PLoS one. 7:e521822012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ciatto S, Del Turco Rosselli M, Burke P,
Visioli C, Paci E and Zappa M: Comparison of standard and double
reading and computer-aided detection (CAD) of interval cancers at
prior negative screening mammograms: Blind review. Br J Cancer.
89:1645–1649. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Janssen V, De Gucht V, Dusseldorp E and
Maes S: Lifestyle modification programmes for patients with
coronary heart disease: A systematic review and meta-analysis of
randomized controlled trials. Eur J Prev Cardiol. 20:620–640. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Maddahi J and Packard RR: PET should
replace SPECT in cardiac imaging for diagnosis and risk assessment
of patients with known or suspected CAD: Pro. J Nucl Cardiol.
24:1955–1959. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schelbert H: Measurement of MBF by PET is
ready for prime time as an integral part of clinical reports in
diagnosis and risk assessment of patients with known or suspected
CAD: For prime time not yet: Need impact and certainty. J Nucl
Cardiol. 25:153–156. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dolatabadi Davari A, Khadem SEZ and Asl
BM: Automated diagnosis of coronary artery disease (CAD) patients
using optimized SVM. Comput Methods Programs Biomed. 138:117–126.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ni J and Wang P: Reasonable application of
cardiac CT in the diagnosis of coronary atherosclerotic heart
disease. Zhonghua Yi Xue Za Zhi. 95:801–802. 2015.(In Chinese).
PubMed/NCBI
|
|
12
|
Perkins JA, Sidhu M, Manning SC, Ghioni V
and Sze R: Three-dimensional CT angiography imaging of vascular
tumors of the head and neck. Int J Pediatr Otorhinolaryngol.
69:319–325. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Murai S, Hamada S, Yamamoto S, Khankan AA,
Sumikawa H, Inoue A, Tsubamoto M, Honda O, Tomiyama N, Johkoh T and
Nakamura H: Evaluation of major aortopulmonary collateral arteries
(MAPCAs) using three-dimensional CT angiography: Two case reports.
Radiat Med. 22:186–189. 2004.PubMed/NCBI
|
|
14
|
Kato Y, Hayakawa M and Katada K:
Three-dimensional multislice helical CT angiography of cerebral
aneurysms. Nihon Rinsho. 62:715–721. 2004.(In Japanese). PubMed/NCBI
|
|
15
|
Jeong Y, Lim C, Oh S, Jung J, Chang J,
Yoon J and Choi M: Three-dimensional CT angiography of the canine
hepatic vasculature. J Vet Sci. 9:407–413. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rozen WM, Stella DL, Ashton MW, Phillips
TJ and Taylor GI: Three-dimensional CT angiography: A new technique
for imaging microvascular anatomy. Clin Anat. 20:1001–1003. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fishman EK, Horton KM and Johnson PT:
Multidetector CT and three-dimensional CT angiography for suspected
vascular trauma of the extremities. Radiographics. 28:653–665.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tanabe S, Uede T, Nonaka T, Ohtaki M and
Hashi K: Diagnosis of cerebral arteriovenous malformations with
three-dimensional CT angiography. J Clin Neurosci. 5 Suppl:S33–S38.
1998. View Article : Google Scholar
|
|
19
|
Prestigiacomo CJ, Sabit A, He W, Jethwa P,
Gandhi C and Russin J: Three dimensional CT angiography versus
digital subtraction angiography in the detection of intracranial
aneurysms in subarachnoid hemorrhage. J Neurointerv Surg.
2:385–389. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mari FS, Nigri G, Pancaldi A, De Cecco CN,
Gasparrini M, Dall'Oglio A, Pindozzi F, Laghi A and Brescia A: Role
of CT angiography with three-dimensional reconstruction of
mesenteric vessels in laparoscopic colorectal resections: A
randomized controlled trial. Surg Endosc. 27:2058–2067. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hoffmann MH, Shi H, Schmid FT, Gelman H,
Brambs HJ and Aschoff AJ: Noninvasive coronary imaging with MDCT in
comparison to invasive conventional coronary angiography: A
fast-developing technology. AJR Am J Roentgenol. 182:601–608. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Matsumoto M, Kodama N, Sakuma J, Sato S,
Oinuma M, Konno Y, Suzuki K, Sasaki T, Suzuki K, Katakura T and
Shishido F: 3D-CT arteriography and 3D-CT venography: The separate
demonstration of arterial-phase and venous-phase on 3D-CT
angiography in a single procedure. AJNR. Am J Neuroradiol.
26:635–641. 2005.PubMed/NCBI
|
|
23
|
Wang Z, Zhang J, Ren T and Dong Z:
Targeted metabolomic profiling of cardioprotective effect of
Ginkgo biloba L. extract on myocardial ischemia in rats.
Phytomedicine. 23:621–631. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hashoul S, Gaspar T, Halon DA, Lewis BS,
Shenkar Y, Jaffe R, Peled N and Rubinshtein R: Automated
computer-assisted diagnosis of obstructive coronary artery disease
in emergency department patients undergoing 256-slice coronary
computed tomography angiography for acute chest pain. Am J Cardiol.
116:1017–1021. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Athanasiou LS, Rigas GA, Sakellarios AI,
Exarchos TP, Siogkas PK, Michalis LK, Parodi O, Vozzi F and
Fotiadis DI: Three-dimensional reconstruction of coronary arteries
and plaque morphology using CT angiography-comparison and
registration using IVUS. Conf Proc IEEE Eng Med Biol Soc.
2015:5638–5641. 2015.PubMed/NCBI
|
|
26
|
Herzog C, Ay M, Engelmann K, Abolmaali N,
Dogani S, Diebold T and Vogl TJ: Visualization techniques in
multislice CT-coronary angiography of the heart. Correlations of
axial, multiplanar, three-dimensional and virtual endoscopic
imaging with the invasive diagnosis. Rofo. 173:341–349.
2001.(Article in German). View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Thompson KA, Philip KJ, Barbagelata A and
Schwarz ER: Review article: The new concept of interventional heart
failure therapy-part 1: Electrical therapy, treatment of CAD, fluid
removal, and ventricular support. J Cardiovasc Pharmacol Ther.
15:102–111. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jelnin V, Co J, Muneer B, Swaminathan B,
Toska S and Ruiz CE: Three dimensional CT angiography for patients
with congenital heart disease: Scanning protocol for pediatric
patients. Catheter Cardiovasc Interv. 67:120–126. 2006. View Article : Google Scholar : PubMed/NCBI
|